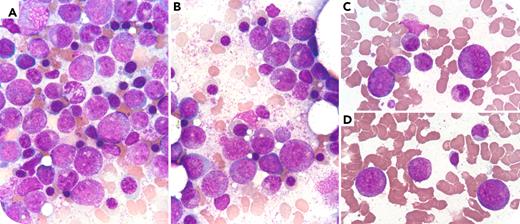
A 58-year-old woman with chronic lymphocytic leukemia completed 4 cycles of fludarabine, cyclophosphamide, and rituximab. Four weeks after her last infusion, she presented with fever, fatigue, and severe neutropenia (absolute neutrophil count, 0.28 × 109/L). No recent infections, viral reactivation, or other drug exposures were identified. A bone marrow aspirate and biopsy demonstrated marked hypercellularity with an inverted myeloid-to-erythroid ratio and a striking maturation arrest predominately at the promyelocyte stage and near absence of mature neutrophils (panels A-D, Wright-Giemsa stain, 100× objective). Given the morphological overlap with acute promyelocytic leukemia (APL), urgent PML-RARA fusion gene testing was performed and returned a negative result. No Auer rods or faggot cells were observed, flow cytometry confirmed the absence of a clonal promyelocytic population, and the coagulation parameters were normal. The patient received broad-spectrum antibiotics and granulocyte–colony stimulating factor (G-CSF) after which gradual neutrophil recovery and symptom resolution were achieved within 4 weeks.
Rituximab-associated late-onset neutropenia (LON) is an uncommon complication that typically arises weeks to months following therapy. Despite profound peripheral neutropenia, bone marrow findings often demonstrate preserved cellularity with granulocytic maturation arrest. The mechanism remains incompletely understood but likely involves immune-mediated suppression of granulopoiesis. The clinical course is generally benign with prompt response to G-CSF in most patients. This case highlights a diagnostic pitfall, because LON closely mimics APL morphologically and should be considered in the differential diagnosis of postrituximab neutropenia with promyelocyte-predominant bone marrow findings.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.