Abstract
The influence of immunodeficiency on the course of hepatitis C virus (HCV) infection is still debated, although a worsening effect has been suggested. We compared the characteristics of hepatitis C in two groups of hematologic patients with different levels of immunocompetence who acquired the same virus strain after treatment with contaminated intravenous immunoglobulins (IVIG). Indications for IVIG therapy were idiopathic thrombocytopenic purpura (ITP) in six patients and hypogammaglobulinemia in 7 patients with various hematologic disorders, who were defined immunodeficient (ID). Infection rate was 100%. Five ID patients never developed HCV antibodies despite serum HCV-RNA positivity. The same HCV genotype was shown in 10 patients tested. Moreover, E1-E2 gene partial nucleotide sequencing, performed in four patients, showed identical or closely related amino acid sequences, thus strongly supporting the hypothesis of a common source of infection. Clinical acute infection did not differ significantly between the two groups, but subsequent liver failure developed in five of the seven ID patients and in none of the ITP patients (P = .04). Liver biopsy, performed in three cases, documented HCV as the only cause of liver damage. Six ID patients died, with liver disease being the primary cause of death in four cases and a contributory cause in two cases. Their median survival after IVIG was 12 months, significantly worse than that of ITP patients (P = .0028). We conclude that immunodeficiency markedly worsens the course of IVIG-acquired HCV infection in hematologic patients.
HEPATITIS C VIRUS (HCV) infection is a known complication of transfusions of blood products, including intravenous immunoglobulins (IVIG). The clinical course and the prognosis of posttransfusion HCV hepatitis, as well as the pathogenetic mechanisms of hepatocellular damage, including the role of the immune system, are still debated.1-4 Several reports have suggested a worsening effect of immunodeficiency, either congenital, human immunodeficiency virus (HIV)-linked, or pharmacologically mediated,5-8 on the severity of hepatitis C.
We had the opportunity of observing a group of patients with different hematologic disorders, in which infection with the same strain of HCV was accidentally transmitted through the administration of a preparation of anti-HCV antibody-screened IVIG that was associated with reports of acute hepatitis C outbreak.9
Because our patients had different degrees of immunocompetence, we could comparatively analyze the effects of an impaired immune system on the clinical course of hepatitis C. We found that in hematologic patients with coexisting immunodeficiency, IVIG-induced HCV infection can frequently lead to irreversible liver failure, which markedly worsens their prognosis.
PATIENTS AND METHODS
During January and February 1994, a preparation of commercially available IVIG (Gammagard; Baxter Hyland Division, Rome, Italy) was available for use in our hematologic unit. The preparation was withdrawn worldwide on February 21, 1994 after reports of acute hepatitis C outbreaks both in Europe and the United States. Fourteen of the the 310 patients admitted to the unit during that period were treated with IVIG. One had known serum anti-HCV antibody (Ab) positivity and was not further considered. The 13 patients with negative (no. 10) or unknown (no. 3) serum anti-HCV Ab status at the time of IVIG infusion are the subject of the present report.
Indications for IVIG therapy were idiopathic thrombocytopenic purpura (ITP) in six patients and hypogammaglobulinemia in seven patients, who were defined as immunodeficient (ID), being affected either by chronic lymphoproliferative disorders (no. 5), common variable immunodeficiency (no. 1), or graft-versus-host disease after allogeneic marrow transplantation (no.1). The clinical characteristics of the patients are detailed in Table 1. Because the original batches of IVIG suspected for HCV contamination were not available, virologic tests were performed only on the serum of patients treated with IVIG.
Serological tests.Anti-HCV Ab was assayed in duplicate by an enzyme-linked immunosorbent assay (ELISA) (Ortho Diagnostic Systems, Raritan, NJ). The determination of antibodies against specific viral antigens was carried out with second- or third-generation Recombinant Immunoblot Assay (RIBA) (Ortho Diagnostic Systems).
RNA extraction and amplification by the polymerase chain reaction (PCR).Total RNA was isolated from 100 μL of serum with RNAzol B (Cinna-Biotecx, Houston, TX), following the manufacturer's instructions. Reverse transcription and nested PCR of the 5′ untranslated region (5′UTR) and E1-E2 region were performed as previously described.10 11
Determination of HCV genotypes.The determination of HCV genotypes was performed by differential hybridization of the 5′UTR PCR products on microtiter plates11 12 using probes specific for genotypes 1-4 located at nucleotides −171-−155: genotype 1 (5′-GAATTGCCAGGACGACC-3′ ), genotype 2 (5′-GAATTGCCGGGAAGACT-3′ ), genotype 3 (5′-GAATCGCTGGGGTGACC-3′ ), and genotype 4 (5′-GAATCGCCGGGATGACC-3′ ).
Cloning and nucleotide sequence analysis.The PCR products of the E1-E2 region, including the hypervariable region 1 (HVR1) (nucleotides 498-1671), were cloned in the Bluescript plasmid vector (Stratagene, La Jolla, CA). Six independent clones were isolated from each PCR product. Partial nucleotide sequence analysis was performed on single-stranded DNA using the Sequenase Images kit (United States Biochemical, Cleveland, OH). Sequence data were analyzed and compared with reference sequences13 using the computer program PC/GENE (Intelligenetics, Geel, Belgium).
RESULTS
Rate of HCV infection.Infection by HCV after IVIG therapy was documented in 100% (13 of 13) of patients. Among six ITP patients, five showed seroconversion from anti-HCV Ab negativity to anti-HCV Ab positivity 2 to 12 months after IVIG (Table 2). One patient had unknown anti-HCV Ab status before IVIG, but had evidence of acute hepatitis 5 months after IVIG, and of anti-HCV Ab positivity 10 months after IVIG, respectively (Table 3). Among seven ID patients, anti-HCV Ab negativity was shown in all cases, five before and two shortly after IVIG. Only two patients had evidence of seroconversion to anti-HCV Ab positivity, 2 and 5 months after IVIG, respectively. The other five patients, who remained anti-HCV Ab negative up to 12 months after IVIG, had evidence of acute hepatitis a median of 3 months after IVIG (Table 3) and serum HCV-RNA positivity was detected in all patients 1.5 to 12 months after IVIG (Table 2). In one case (FF ), HCV-RNA was also tested before IVIG and found negative. Moreover, in two (AA and BF ) of the remaining four ID patients, the demonstration of the same type of viral sequences by molecular studies of the HVR1 region (Fig 1) strongly supported their HCV-naive status before IVIG.
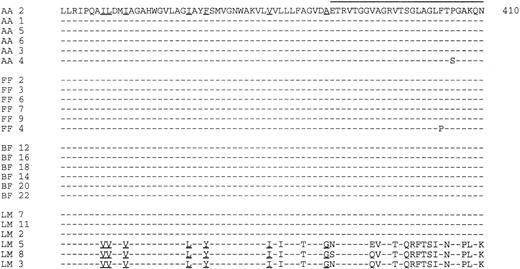
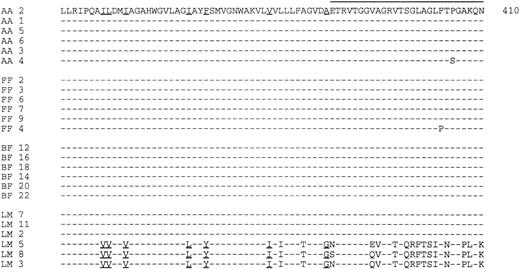
Deduced amino acid sequence of the E1-E2 region (residues 337-410). The initials of patients and the number of each clone are indicated on the left. The horizontal line indicates the HVR1 region. The residues specific for genotypes 1a or 1b (clones LM 5, LM 8, and LM 3)13 are underlined.
Deduced amino acid sequence of the E1-E2 region (residues 337-410). The initials of patients and the number of each clone are indicated on the left. The horizontal line indicates the HVR1 region. The residues specific for genotypes 1a or 1b (clones LM 5, LM 8, and LM 3)13 are underlined.
Source of HCV infection.The IVIG origin of HCV infection was supported by clinical follow-up as well as by virologic studies (Tables 2 and 3).
At the time of IVIG infusion, alanine aminotransferase (ALT) levels were normal in all patients except in one (VE), whose levels were less than 100 U/dL. A median of 3 months after IVIG therapy, a greater than fivefold ALT increase over baseline levels was detected in 11 of 11 evaluable patients. In two patients (GA, SG), ALT levels were not monitored shortly after IVIG, but abnormal ALT levels and seroconversion to HCV-Ab positivity were documented 5 and 10 months after IVIG treatment, respectively. Transfusions of packed red blood cells (RBCs) and/or platelet concentrates were given after IVIG therapy and before the onset of hepatitis to two ITP and four ID patients (Table 1). However, none of the patients was transfused from the same blood donor.
HCV genotype determination, performed on 10 patients (6 ID and 4 ITP), detected genotype 1 in all cases. The E1-E2 region was successfully amplified from 4 of 5 available samples obtained from ID patients 3 to 4 months after infusion of IVIG. The alignment of deduced amino acid sequences showed common features in all patients (Fig 1). In 3 cases all sequences were identical or closely related to each other, whereas in 1 patient (LM), two molecular species were detected, one of which was common to the remaining patients. Amino acid sequences of the C terminus of E1 region indicated that the HCV isolate detected in all patients belonged to genotype 1a. By contrast, the sequence isolated only from patient LM shared homology with genotype 1b. This patient was anti-HCV Ab–negative before IVIG and received 1 U of packed RBCs during splenectomy after IVIG. However, 2 of the 3 patients who showed complete homology of all HVR1 sequences of E2 gene also had received multiple transfusions. The clinical course of HCV hepatitis in the double-infected patient (LM) was mild.
Clinical course.Clinical or laboratory features of acute hepatitis developed in all 11 evaluable patients (Table 3). Liver failure, defined as a reduction of prothrombin activity below 50% and/or of albumin concentration below 2.5 g/dL and/or an irreversible elevation of bilirubin level greater than 10 mg/dL, developed in five patients, while ALT levels never exceeded 1,000 IU/mL. A liver biopsy was performed in three patients. Liver histology showed moderately aggressive chronic hepatitis in one ITP patient with chronic ALT elevation as well as in one ID patient with low-grade non-Hodgkin's lymphoma. In this patient hepatic infiltration by lymphoma was excluded by immunohistochemistry. In the single marrow transplanted ID patient histology showed acute HCV hepatitis excluding the possibility of hepatic graft-versus-host disease. Liver biopsy was not performed in four ID patients because of coagulation defects.
At the present time, seven patients, six ITP and one ID, are still alive 27 months after infected IVIG infusion. Six of them have mild chronic HCV hepatitis without showing signs of liver failure. Six ID patients died 4.5 to 17 months after IVIG, 1 to 14 months (median, 2.5 months) after the development of hepatitis. The primary cause of death was protracted acute hepatitis in two patients, and chronic hepatitis, causing irreversible liver failure, in two others. Liver disease was a significant contributory cause of death in the remaining two cases. HCV infection was considered the main cause of hepatic disease in all cases. Serologic studies excluded coinfection both with hepatitis B virus and human immunodeficiency virus in all cases. Cytomegalovirus and Epstein-Barr virus coinfection was excluded in five and three ID patients, respectively. After IVIG therapy, the clinical course of the underlying hematologic disorder did not accelerate in any of the cases studied, nor were there any major changes in hematologic treatment, and none of the patients received cytostatic or immunosuppressive agents, which they had not received before IVIG (Table 1).
Comparison between ITP and ID patients.The two subgroups of patients did not show significant differences in age, performance status at the time of IVIG infusion, and frequency of corticosteroid therapy before and after IVIG. In the subgroup of ID patients, there was a predominance of males and patients received more cytostatic and/or immunosuppressive agents other than corticosteroids both before and after IVIG. On the other hand, ITP patients were all females and three of them were splenectomized after IVIG (Table 1). The mean dose of IVIG received by the ITP patients was 88 g (SD ± 51), significantly higher than that of the ID patients (31.2 g; SD: ±9.8) (Student's t-test: P = .015). During acute infection, there were no significant differences in the duration of the incubation period as well as in ALT peak levels, although the highest levels were recorded among ITP patients whereas ALT never exceeded 1,000 U/dL in ID patients (Table 3). On the other hand, ID patients had more marked increases of bilirubin levels. A bilirubin level greater than 5 mg/dL occurred in 86% of ID patients compared with 33% of ITP patients. Chronic HCV hepatitis developed in all evaluable ID patients and in 5 of 6 ITP patients. Signs of liver failure developed in 71% of ID patients and in no ITP patient (Chi-square analysis with Yates's correction: P = .04).
Two years after IVIG, only one ID patient was alive (14%) whereas all ITP patients were alive. The median survival of ID patients was 12 months, significantly worse than that of ITP patients (Mantel-Cox analysis: P = .003).
DISCUSSION
The present study describes the development of HCV hepatitis in a small group of hematologic patients treated with a preparation of contaminated IVIG. Because both a common source of infection and a common etiologic agent were detected in different patients, the influence of the patients' characteristics, particularly of their immune status, on the clinical course and prognosis of HCV infection could be analyzed in detail.
Both epidemiological and clinical data closely linked the IVIG therapy received by all patients to subsequent development of HCV hepatitis. In addition, virologic studies strongly suggested that patients were infected by at least one identical strain of HCV, consistent with the hypothesis of a single infection source. The same HCV genotype 1 was shown in all the patients tested. More importantly, a high degree of homology was demonstrated among the HVR1 sequences derived from the four patients tested. Because the HVR1 region is extremely variable among different isolates, and because distinct sequences can be identified even in a single patient,14 sequence analysis further strengthens the possibility of a common infectious source. In one patient a second independent HVR1 sequence belonging to a different genotype was identified. Because the original batches of IVIG were not available for study, it was impossible to assess whether double infection derived from IVIG or from different sources.
Subdividing patients in two subgroups according to their underlying disease enabled us to analyze the relationship between HCV infection and the host's immune status. The six patients with ITP were considered immunocompetent, whereas the remaining seven patients were considered ID, since they had hypogammaglobulinemia, either primary or secondary to chronic lymphoid malignancies, or graft-versus-host disease after bone marrow transplantation, a condition in which immune reconstitution is markedly impaired.
The demonstration of the contact with HCV was difficult in ID patients. Serum anti-HCV Ab testing was not sufficient and had to be complemented with HCV-RNA detection by PCR, because only two of the seven patients developed antibodies to HCV after IVIG. Similarly, low rates (53% to 66%) of anti-HCV Ab positivity were reported in HCV-infected patients with immunodeficiency disorders and with malignant hematologic diseases,9,15 but when the search for HCV-RNA was performed, HCV infection could be documented in 85% to 100% of patients with primary hypogammaglobulinemia5 or after bone marrow transplants from HCV-RNA–positive donors.16 On the other hand, anti-HCV Ab positivity developed in all ITP patients.
The rate of HCV infection after IVIG infusion was 100% in our patients, indicating that the efficiency of transmission might not be influenced by the immune status. An alternative explanation might be a high viral load in the infectious inoculum, or the high total doses of IVIG administered. Notably, ITP patients received a significantly higher dose of IVIG, which may partially account for their high infection rate. A high infection rate (82%) was recently documented also among patients in the United Kingdom who received a contaminated batch of anti-HCV antibody-screened IVIG.17
Neither the timing nor the severity of acute infection seemed to be influenced by the immune status of patients. The incubation period of acute hepatitis was similar in ITP and in ID patients. Peak ALT levels did not differ significantly between ITP and ID patients. Nevertheless, it should be noted that ID patients had particularly mild increases of ALT, whose peak levels never exceeded 1,000 IU/dL. In most reported studies, immunosuppression does not appear to worsen the severity of acute hepatitis. ALT levels decreased when corticosteroids or cytostatic drugs were given to patients with hepatitis,15,18,19 with some exceptions.20 However, during immunosuppressive therapy an increase in viremia has been reported by different investigators,19,21 even with no biochemical signs of hepatic necrosis. On suspending corticosteroid or cytostatic treatment, several cases of fulminant hepatitis C have been observed,16,22-25 as in patients infected with hepatitis B virus,26 suggesting a role of the immune system in the pathogenesis of acute hepatic necrosis.
In our study a trend toward a more marked elevation of bilirubin levels was shown in the subgroup of ID patients. Jaundice developed in the majority (86%) of ID patients compared with 33% of ITP patients, and was the main cause of hospital admission. In patients with hematologic disorders an elevation of bilirubin levels during acute HCV hepatitis has been reported in 24% of cases.15 Both the type of the underlying disorder and the drugs used for its treatment may have contributed to the differences in the incidence and severity of jaundice in ID patients. A severe cholestatic form of liver disease, which finally leads to death from liver failure, has also been observed in patients with heart and liver transplantation as well as in patients with hypogammaglobulinemia.3
The course of HCV hepatitis was strikingly different between ITP and ID patients and hepatic disease severely affected the overall prognosis of ID patients. Among ITP patients, resolution of HCV infection occurred in one case and chronicization occurred in five patients (83%), a rate that is only marginally higher than that of normal individuals after HCV infection.9,27 Moreover, chronic infection was clinically mild and no patients have shown signs of liver failure. Conversely, among ID patients, liver failure developed in 71% of cases and proved irreversible in 80% of them. It is noteworthy that this occurred in the absence of signs of hyperacute hepatic necrosis, as shown by only moderate ALT elevation, throughout the clinical course of the disease. Apoptosis has been recently identified as a mechanism of programmed cell death in many tissues, including the liver.28 As opposed to necrosis, apoptosis is not associated with inflammatory signs. It may be postulated that since apoptosis has been shown in hepatitis C, it may be one of the mechanisms involved in hepatocellular injury in patients with immunodeficiency.
Hepatic disease was the most important factor in determining the very poor outcome of ID patients, whose 2-year survival rate was only 12%. In addition to their immune status, other differences between ITP and ID patients, such as their underlying disorders, the possibility of coinfection with other unidentified viral agents, or the treatments received, may be advocated to explain the different course of hepatic disease. However, ID patients lacked signs of liver involvement by their underlying disorder before HCV infection and did not show a progressive course thereafter. Moreover, hepatic histology, in the cases analyzed, further confirmed that HCV infection was the only cause of hepatic disease, as recently observed in a patient with chronic lymphocytic leukemia treated with HCV-infected IVIG.17 Immunosuppressive therapy was given both to ITP and ID patients, but only ID patients also received cytostatic agents before and after HCV infection. Therefore, it cannot be excluded that preceding or concomitant chemotherapy may predispose patients to subacute or chronic HCV-mediated liver damage in the presence of immunodeficiency. Indeed, liver failure developed rapidly in the two ID patients who continued cytostatic treatment after IVIG, whereas the only surviving ID patient has never been treated with chemotherapy. However, because the type of drugs and the dosages used in our patients are unlikely to be associated with a significant drug-induced liver toxicity, it is possible that chemotherapy plays its negative role by further impairing the immune status of ID patients.
Address reprint requests to Giuseppe Rossi, MD, Sezione Ematologia, Spedali Civili, p.le Spedali Civili, 1, 25100 Brescia, Italy.