Abstract
Donor CD8+ T cells capable of host reactivity inhibit marrow graft rejection, but also generate graft-versus-host disease (GVHD). To evaluate whether the Tc1- and Tc2-type subsets of CD8 cells might inhibit rejection without host reactivity, we established an F1 into-parent murine bone marrow transplant model. Donor Tc1 and Tc2 cells were generated that preferentially secreted type I or type II cytokines; both subsets possessed potent cytolytic function, and clonally deleted host-type allospecific precursor CTL in vitro. B6 hosts receiving 950 cGy irradiation did not reject the donor marrow (F1 chimerism of 78.6%; n = 10), whereas hosts receiving 650 cGy rejected the donor marrow (3.8% chimerism; n = 8). At 650 cGy irradiation, the addition of Tc2 cells to the F1 marrow resulted in extensive F1 chimerism (70.8%) in 8 of 8 recipients; in contrast, alloengraftment was not consistently observed in mice receiving Tc1 cells or unmanipulated CD8 cells. Furthermore, when the preparative regimen was further reduced to 600 cGy, only hosts receiving the Tc2-type cells did not reject the F1 marrow. We conclude that Tc2 cells potently inhibit marrow graft rejection without inducing an alloaggressive response and that non–host-reactive Tc2 cells therefore facilitate engraftment across genetic barriers with reduced GVHD.
THE HOST-VERSUS-GRAFT immune response, which results in graft rejection, is a primary limitation to the transfer of marrow across genetic barriers. The observation that recipients of T-cell–depleted transplants have a high rate of marrow failure1 has led to the realization that donor T cells abrogate graft rejection; indeed, the presence of donor T cells in the marrow appears to be one of the primary determinants of whether alloengraftment occurs.2 As such, administration of T-cell–enriched marrow is one approach to the facilitation of alloengraftment. However, in addition to preventing graft rejection, donor T cells generate an alloaggressive response against host antigens, which can result in graft-versus-host disease (GVHD). The donor CD8+ T-cell subset appears to be particularly capable of abrogating rejection3; however, CD8+ T cells also contribute significantly to the generation of GVHD.4 5 Given this limitation, we have evaluated whether functional subsets of donor CD8 cells might prevent graft rejection with reduced GVHD.
Recently, the existence of cytokine-secreting subsets of cytotoxic CD8+ T cells has been demonstrated6,7: the Tc1 subset secretes the type I cytokines interleukin-2 (IL-2) and interferon-γ (IFN-γ), whereas the Tc2 subset secretes the type II cytokines IL-4, IL-5, and IL-10. Both cytokine-secreting subsets of CD8 cells possess cytolytic function, which has led to the Tc1/Tc2 terminology.7 Such CD8 functional subsets appear to differentially mediate allogeneic responses; eg, we and others have observed that the Tc2 subset results in reduced GVHD.8,9Importantly, the Tc2 subset can also mediate a graft-versus-leukemia (GVL) effect.8 10 These results suggest that Tc2 cells might represent a CD8 population capable of mediating beneficial allogeneic responses (such as the mediation of GVL effects or the abrogation of graft rejection) with reduced detrimental effects (less severe GVHD). In light of these observations, we have compared the Tc1 and Tc2 subsets of CD8+ T cells for their ability to prevent marrow rejection.
To study the engraftment effects of the Tc1 and Tc2 subsets of donor CD8 cells independent of their GVHD effects, we have established an F1 into-parent model of graft rejection (B6C3F1 bone marrow into sublethally irradiated B6 hosts). In this type of rejection model, donor CD8 cells share the haplotype of the parental host and thus do not induce an alloaggressive reaction against the host; T-cell–mediated facilitation of engraftment in such models has been attributed to a veto effect.11 In the veto effect, host-type precursor CTL capable of mediating rejection are clonally deleted by cytotoxic donor cells that express the alloantigens present on the marrow graft12; in addition, the donor cells mediating the clonal deletion are nonreactive to host antigens. The definition of veto cells is therefore a functional one, and multiple cell types have been observed to possess veto-type activity in the setting of murine allogeneic bone marrow transplantation, including bone marrow-derived natural killer cells13 and CD4+14 and CD8+3,14 T cells. Previous experiments have demonstrated that the perforin/granzyme pathway of cytolysis is important in the mediation of the veto effect.12 Thus, in light of studies that indicate that the Tc2 subset of CD8+ T cells preferentially uses the perforin/granzyme pathway,15 we hypothesized that non–host-reactive Tc2 cells would prevent marrow rejection.
In this study, we compared the Tc1 and Tc2 subsets of donor CD8+ T cells for their ability to facilitate alloengraftment and have determined that the Tc2 subset potently inhibits marrow graft rejection. By using an F1 into-parent model, we have shown that Tc2-mediated abrogation of rejection can occur independent of an alloaggressive response. The administration of non–host-reactive Tc2 cells therefore represents a strategy for abrogating rejection with reduced GVHD and thus may allow for the transfer of marrow across genetic barriers.
MATERIALS AND METHODS
In vitro generation of donor CD8+ T cells of Tc1 and Tc2 phenotype.
Spleen cells from donor B6D2F1 mice (C57BL/6 × DBA/2, H-2b/d; obtained from Frederick Cancer Research Facility [Frederick, MD] and used at 8 to 16 weeks of age) were harvested, lysed in Tris-ammonium chloride buffer (Biofluids, Rockville, MD), and brought to a concentration of 4 × 107 cells/mL in RPMI 1640 (Life Technologies, Grand Island, NY) containing 10% fetal calf serum (FCS; HyClone, Logan, UT). This splenic single-cell suspension was enriched for T cells (goat antimouse H and L bioparticles; PerSeptive Diagnostics, Cambridge, MA) and then enriched for CD8 cells by complement treatment (rabbit low-tox; Cedarlane, Hornby, Ontario, Candada) after incubation with anti-CD4 (supernatant from clone RL172/416). The CD8-enriched spleen cells were then resuspended at 1 × 106/mL and cocultured at a ratio of 1:4 with irradiated (3,000 cGy) whole spleen cells from B6C3F1 mice (C57Bl/6 × C3H/HeN, H-2b/k).
The coculture was performed in 75-cm2 flasks (Costar, Cambridge, MA) in 40 mL of RPMI 1640 supplemented with 10% FCS, sodium pyruvate (1%), nonessential amino acids (1%), L-glutamine (0.5%), 2-ME (5 × 10−5 mol/L), penicillin (0.5%), streptomycin (0.5%), and N-acetyl cysteine (Sigma Chemical Co, St Louis, MO; 10 mmol/L, pH adjusted to 7.2). All cocultures received recombinant human IL-2 at 40 Cetus units (CU)/mL (kindly provided by Dr Martin Giedlin, Chiron Therapeutics, Emeryville, CA) and recombinant human IL-7 (20 ng/mL; Peprotech, Rocky Hill, NJ) on days 0 and 2. Tc1 cultures were supplemented (day 0) with recombinant murine IL-12 (20 U/mL; kindly provided by Dr Stan Wolf, Genetics Institute, Cambridge, MA) and recombinant human transforming growth factor β-one (TGF-β; 10 ng/mL; R&D Systems, Minneapolis, MN), whereas Tc2 cultures were supplemented (day 0) with recombinant murine IL-4 (1,000 U/mL; Peprotech). On day 5 of culture, Tc1 and Tc2 flasks were harvested, brought to a final concentration of 0. 5 × 106/mL in 40 mL of fresh media, and restimulated with irradiated (3,000 cGy) B6C3F1 spleen cells at a ratio of 1:4. At the time of restimulation, IL-2 (40 U/mL) and IL-7 (20 ng/mL) were added to both Tc1 and Tc2 cultures.
Flow cytometric (FCM) evaluation of Tc1/Tc2 surface phenotype.
To evaluate the Tc1 and Tc2 populations for cell surface phenotype, aliquots from the CD8 cultures were harvested on day 7, washed, and resuspended in FCM media consisting of Hanks' balanced salt solution (HBSS; Life Technologies) supplemented with 0.5% bovine serum albumin (BSA; Sigma) and 0.1% azide. Cells were first incubated with unlabeled anti-Fc receptor (2.4G2; PharMingen, San Diego, CA) and then stained with anti-CD4 fluorescein isothiocyanate (FITC) and anti-CD8 phycoerythrin (PE) (Becton Dickinson Immunocytometry Systems [BDIS], Mountain View, CA); negative control stains consisted of Leu8 FITC and Leu4 PE. Cells were also stained with anti-CD69 PE (PharMingen). Two-color flow cytometry was performed on a FACSort (BDIS) using LYSIS II software. Five thousand to 10,000 live events were acquired for analysis; dead cells were gated out on the basis of propidium iodide staining.
Cytokine secretion profiles of Tc1 and Tc2 populations by enzyme-linked immunosorbent assay (ELISA).
On day 7 of culture, aliquots from Tc1 and Tc2 cultures were harvested, brought to a final concentration of 0.5 × 106/mL, and stimulated in 24-well plates (Costar) with either syngeneic B6D2F1 or semiallogeneic B6C3F1 spleen cells (irradiated 3,000 cGy; 1:4 ratio). Supernatants were harvested after 24 hours and tested in two-site ELISAs using commercially available reagents (purified and biotinylated anti-cytokine antibody pairs; PharMingen). Cytokine levels were calculated by reference to standard curves constructed on supernatants containing known amounts of recombinant cytokine.
Evaluation of Tc1/Tc2 cytolytic function.
On day 7 of culture, aliquots from Tc1 and Tc2 cultures were harvested and tested for their ability to lyse the allogeneic tumor line P21017 (H-2k; myeloid line transfected with the bcr/abl oncogene; kindly provided by Dr James Griffin, Dana-Farber Cancer Institute, Boston, MA). The syngeneic control target EL-4 (H-2b; American Type Tissue Culture TIB 39) was used to determine allospecificity of cytolytic function; as a positive control for this syngeneic target, CD8+ T cells from DBA mice were stimulated under Tc1 and Tc2 conditions using spleen cells from B6 mice (H-2b) as stimulator cells. Standard chromium-release assays were performed, with calculation of the percentage of specific lysis.18
In vitro assay of Tc1- and Tc2-mediated deletion of precursor CTL.
Using a previously described in vitro model of veto cell function,12 we tested the Tc1 and Tc2 populations for their ability to clonally delete allospecific precursor CTL. In this model, a mixed lymphocyte reaction was established using a 10:1 mixture of responder spleen cells from C57Bl/6(H-2b) and C57Bl/6 transgenic mice (2C mice; CD8+ T cells transgenic at the TCR locus for Ld allospecificity19). Responder cells (4 × 106) were stimulated in 24-well plates (Costar) with irradiated spleen cells (2,500 cGy) from DBA/2 mice (H-2d). Expansion of the allospecific CD8+T cells was monitored by daily cell count determinations and flow cytometry (the transgenic TCR was identified by flow cytometry after staining with directly FITC-labeled 1B2 antibody specific for the transgenic TCR19). In this culture system, transgenic CD8+ T cells undergo an approximate 10-fold expansion between days 2 and 3 of the MLR. To evaluate the ability of CD8 functional T-cell subsets to mediate veto activity in vitro, Tc1 and Tc2 populations were generated (as described above) and added to the transgenic cultures on day 2; on day 3, cell counting and flow cytometry was performed to determine transgenic CTL yield. The Tc1 and Tc2 populations were generated from CD8+ T cells from B6D2F1 mice and thus shared the H-2b haplotype with the transgenic CTL and shared the H-2d haplotype with the irradiated stimulator cells. As such, Tc1- or Tc2-mediated deletion of the transgenic CTL may occur by a veto-type mechanism.
F1 into-parent transplantation model.
Parental B6 mice received total body irradiation (137Cs γ radiation source, 101 cGy/min; Gamma Cell 40; Atomic Energy of Canada, Ltd, Ottawa, Ontario, Canada); depending on the particular experiment, the radiation dose varied from 600 to 950 cGy. Four to 6 hours after irradiation, all mice received an intravenous injection of 1 × 107 T-cell–depleted (TCD) bone marrow cells from B6D2F1 mice (antibody/complement depletion using the anti–T-cell monoclonal HO-13-220). Control mice received only the TCD marrow, whereas recipients in other groups also received a separate intravenous injection of 1 × 107 CD8+ T cells of donor B6D2F1 origin; such CD8+ T cells consisted of either in vitro generated CD8+ T cells of Tc1 or Tc2 phenotype (harvested from flasks on day 7 of culture) or uncultured B6D2F1 CD8+ T cells (prepared by T-cell enrichment and anti-CD4/complement treatment, as described above).
Evaluation of donor chimerism posttransplant by flow cytometry.
Donor cell chimerism of transplant recipients for each experiment was determined by flow cytometry at approximately 1 month posttransplant and again after 3 months posttransplant. Heparinized peripheral blood was obtained from the retro-orbital sinus, and lymphocytes were isolated by density centrifugation (Cellsep; 1.077 specific gravity; Larex, Inc, St Paul, MN) and subsequently washed in FCM media. Cells were incubated with unlabeled anti-Fc receptor antibody (2.4G2; PharMingen) and stained with anti-H-2kb FITC and anti-H-2kd PE (PharMingen); cells were also stained with isotype control antibodies to define background staining. Lymphocytes taken from untreated B6 and B6D2F1 mice were used to define postive and negative quadrants. Other stains used to evaluate lineages of engraftment were anti-CD19 FITC, anti-granulocyte FITC, and anti-Thy 1.2 FITC (all from PharMingen).
Statistical methodology.
P values were obtained using the two-sided matched-rank analysis of Wilcoxin; values less than .05 were considered statistically significant.
RESULTS
Phenotyping of in vitro-generated donor CD8+ T cells of Tc1 and Tc2 phenotype.
After 7 days, cells from the Tc1 and Tc2 cultures were phenotyped by flow cytometry. Both Tc1 and Tc2 culture conditions resulted in a population that was greater than 90% CD8+, with less than 2% contaminating CD4+ cells. Similar to results we have reported previously,8 cells from the Tc2 culture had lower surface CD8 expression relative to the Tc1 culture (mean fluorescence intensity of CD8 expression for Tc2 cells was 3,662, whereas Tc1 cell mean fluorescence intensity of CD8 expression was 5,131). Also, expression of surface CD69 was measured to compare the Tc1 and Tc2 cultures for their activation status21: the majority of cells (>85%) in both Tc1 and Tc2 cultures were positive for CD69, indicating that both populations were similarly activated at the time of their in vivo evaluation (day 7 of culture).
On day 7 of culture, cells from the Tc1 and Tc2 cultures were harvested and evaluated for cytokine phenotype. To evaluate the allospecific cytokine secretion pattern, cultured CD8 cells were restimulated with either syngeneic B6D2F1 spleen cells or semiallogeneic B6C3F1 cells; cytokine secretion was allospecific, because stimulation of Tc1 and Tc2 cells with syngeneic spleen cells did not result in significant cytokine production above the detection limits of the assays (IL-2 assay, 0.8 CU/mL; IFN-γ, 1.0 IU/mL; IL-4, 20 pg/mL; IL-5, 320 pg/mL; and IL-10, 40 pg/mL). In response to restimulation with the third-party alloantigen (H-2k), cells from the Tc1 culture secreted the type I cytokines IL-2 (10.9 CU/mL) and IFN-γ (152 IU/mL), but did not secrete the type II cytokines. In marked contrast, cells from the Tc2 culture secreted the type II cytokines IL-4 (204 pg/mL), IL-5 (3,193 pg/mL), and IL-10 (1,510 pg/mL) and secreted reduced levels of the type I cytokines IL-2 (1.2 CU/mL) and IFN-γ (19.9 IU/mL).
Cytolytic function of the Tc1 and Tc2 cultures was evaluated in chromium release assays using the allogeneic tumor target, P210; this target shares the alloantigen (H-2k) used for the in vitro CD8 generation. As Fig 1 shows, CD8+ T cells secreting either type I or type II cytokines were similarly effective in their lysis of the allogeneic P210 target. In contrast, the Tc1 and Tc2 populations mediated only nominal lysis of the syngeneic EL-4 target; the ability of the EL-4 control target to be lysed was confirmed by generating Tc1- and Tc2-type effector cells of anti-H-2b specificity (both populations showed greater than 65% specific lysis of the EL-4 target at a 30:1 E:T ratio). Thus, the Tc1 and Tc2 populations were allospecific both in their cytokine secretion and cytolytic function. As such, the in vitro culture methodology was effective in generating allospecific CD8+donor T cells of Tc1 and Tc2 phenotype.
Cytolytic function of the Tc1 and Tc2 populations. CD8+ T cells from B6D2F1 donor mice were stimulated in vitro with irradiated spleen cells from B6C3F1 mice under Tc1 or Tc2 conditions, harvested on day 7 of culture, and plated in a standard 4-hour chromium-release assay at the stated E:T ratios with the allogeneic tumor target, P210 (H-2k), or the syngeneic tumor target, EL-4 (H-2b). Each data point was performed in triplicate, with less than 5% standard deviation for each point.
Cytolytic function of the Tc1 and Tc2 populations. CD8+ T cells from B6D2F1 donor mice were stimulated in vitro with irradiated spleen cells from B6C3F1 mice under Tc1 or Tc2 conditions, harvested on day 7 of culture, and plated in a standard 4-hour chromium-release assay at the stated E:T ratios with the allogeneic tumor target, P210 (H-2k), or the syngeneic tumor target, EL-4 (H-2b). Each data point was performed in triplicate, with less than 5% standard deviation for each point.
Both Tc1- and Tc2-type populations effectively delete precursor CTL in vitro.
Graft rejection is mediated in part by radioresistant allospecific CTL22-25; the clonal deletion of such CTL may be one mechanism whereby donor T cells abrogate graft rejection. A model has been developed to evaluate the ability of cytotoxic cells to clonally delete allospecific CTL in vitro by a veto-type mechanism12; using this model, we compared the Tc1 and Tc2 populations for their ability to clonally delete precursor CTL. In this model, the fate of allospecific precursor CTL is determined by measuring the flow cytometric expression of the transgenic TCR expressed by these CTL. It is important to note that, similar to the in vivo graft rejection model, this in vitro model is a one-way alloreactive system; ie, the transgenic precursor CTL can recognize the stimulator cells and the Tc1 or Tc2 populations, but the Tc1 and Tc2 cells are syngeneic relative to the precursor CTL. Figure 2 shows that both Tc1 and Tc2 cells were similarly effective in their ability to delete the allospecific precursor CTL population: the addition of 1 × 106 Tc1 or Tc2 cells on day 2 of the MLR resulted in an approximate one log reduction in transgenic CTL number by day 3 of culture.
Both Tc1 and Tc2 populations clonally delete precursor CTL in vitro by a veto-type mechanism. A mixed lymphocyte reaction was established in 24-well plates using a 10:1 mixture of responder spleen cells from C57Bl/6(H-2b) and C57Bl/6 transgenic mice (2C mice; CD8+ T cells are transgenic at the TCR locus for Ld allospecificity) and stimulator spleen cells from DBA/2 mice (H-2d). The yield of transgenic CD8+ T cells in the MLR (tg responder MLR) was calculated by determination of cell counts and transgene percentage (transgenic TCR was identified by flow cytometry after staining with FITC-labeled 1B2 antibody); in this system, the transgenic CD8 population expands appoximately 10-fold between days 2 and 3 of the MLR. To evaluate the ability of Tc1- and Tc2-type cells to clonally delete this transgenic population by a veto mechanism, CD8+ T cells from B6D2F1 donor mice were stimulated in vitro with irradiated spleen cells from B6C3F1 mice under Tc1 or Tc2 conditions, harvested on day 7 of culture, and added to the transgenic MLR at the indicated numbers per well (tg + Tc1 and tg + Tc2) on day 2 of the MLR. The yield of transgenic CD8 cells was then determined on day 3 of the MLR.
Both Tc1 and Tc2 populations clonally delete precursor CTL in vitro by a veto-type mechanism. A mixed lymphocyte reaction was established in 24-well plates using a 10:1 mixture of responder spleen cells from C57Bl/6(H-2b) and C57Bl/6 transgenic mice (2C mice; CD8+ T cells are transgenic at the TCR locus for Ld allospecificity) and stimulator spleen cells from DBA/2 mice (H-2d). The yield of transgenic CD8+ T cells in the MLR (tg responder MLR) was calculated by determination of cell counts and transgene percentage (transgenic TCR was identified by flow cytometry after staining with FITC-labeled 1B2 antibody); in this system, the transgenic CD8 population expands appoximately 10-fold between days 2 and 3 of the MLR. To evaluate the ability of Tc1- and Tc2-type cells to clonally delete this transgenic population by a veto mechanism, CD8+ T cells from B6D2F1 donor mice were stimulated in vitro with irradiated spleen cells from B6C3F1 mice under Tc1 or Tc2 conditions, harvested on day 7 of culture, and added to the transgenic MLR at the indicated numbers per well (tg + Tc1 and tg + Tc2) on day 2 of the MLR. The yield of transgenic CD8 cells was then determined on day 3 of the MLR.
F1 CD8+ T cells of Tc2 phenotype potently inhibit marrow graft rejection.
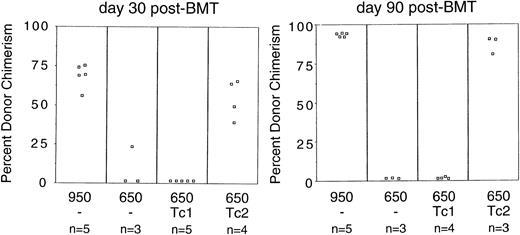
Having generated CD8+ T cells of both Tc1 and Tc2 phenotype from F1 donors, we next evaluated their effect on F1 marrow engraftment in an F1 into-parent model of graft rejection. B6 mice were sublethally irradiated and subsequently received marrow from B6D2F1 mice; control mice received only the F1 marrow, whereas other treatment groups received additional donor CD8+ T cells of Tc1 or Tc2 phenotype. Figure 3 shows the flow cytometry result for determination of F1 chimerism at both day 30 and day 90 posttransplant. Irradiation of the B6 hosts with a high dose of irradiation (950 cGy) resulted in F1 marrow engraftment (the range of F1 chimerism was 56% to 76% at day 30 and 92% to 95% at day 90). In contrast, B6 hosts that were irradiated at a lower dose (650 cGy) displayed nearly complete host-type chimerism by day 90 posttransplant (<2% F1 chimerism), thus indicating rejection of the F1 marrow. In this experiment, hosts prepared with 650 cGy irradiation that received marrow enriched with F1 CD8+ T cells of Tc1 phenotype also rejected the F1 marrow (<3% chimerism in all recipients). In marked contrast, hosts prepared with 650 cGy irradiation that received additional CD8+ T cells of Tc2 phenotype had predominately donor-type chimerism (the range of F1 chimerism was 51% to 66% at day 30 and 82% to 91% at day 90). Other flow cytometry data (not shown) indicated that the chimerism occurred in the T-cell, B-cell, and granulocyte lineages. This experiment therefore indicated that the Tc2-type cells had a marked ability to prevent acute marrow graft rejection and that Tc2-mediated facilitation of engraftment resulted in long-term, stable marrow engraftment.
Tc2-type donor CD8+ T cells abrogate marrow graft rejection. Host B6 (H-2b) mice were irradiated at 950 or 650 cGy; all mice received 1 × 107 TCD bone marrow cells from B6D2F1 (H-2b/d) donor mice. Engraftment control mice (950/−) and rejection control mice (650/−) received only the donor bone marrow at the time of transplant; other groups received additional donor CD8+ T cells (1 × 107cells) of Tc1-type (650/Tc1) or Tc2-type (650/Tc2). Peripheral blood lymphocytes were isolated on days 30 and 90 posttransplant and stained with H-2b FITC (common to both donor and host cells) and H-2d PE (specific for donor cells); the percentage of donor and host chimerism was then determined by flow cytometry. Each data point represents the donor chimerism result for an individual animal.
Tc2-type donor CD8+ T cells abrogate marrow graft rejection. Host B6 (H-2b) mice were irradiated at 950 or 650 cGy; all mice received 1 × 107 TCD bone marrow cells from B6D2F1 (H-2b/d) donor mice. Engraftment control mice (950/−) and rejection control mice (650/−) received only the donor bone marrow at the time of transplant; other groups received additional donor CD8+ T cells (1 × 107cells) of Tc1-type (650/Tc1) or Tc2-type (650/Tc2). Peripheral blood lymphocytes were isolated on days 30 and 90 posttransplant and stained with H-2b FITC (common to both donor and host cells) and H-2d PE (specific for donor cells); the percentage of donor and host chimerism was then determined by flow cytometry. Each data point represents the donor chimerism result for an individual animal.
To further evaluate the effect of the Tc1 and Tc2 populations on F1 marrow engraftment, B6 host mice were irradiated (950, 650, or 600 cGy) and received injections of either F1 marrow alone or marrow and F1 CD8 cells that were cultured in vitro under Tc1 or Tc2 conditions; a separate treatment group received F1 marrow and unmanipulated F1 CD8+ T cells (naive CD8). As Fig 4 shows (chimerism results on day 41 posttransplant), hosts receiving 950 cGy irradiation displayed nearly complete F1 engraftment, whereas hosts receiving 650 cGy irradiation uniformly rejected the F1 marrow. At 650 cGy of host irradiation, mice receiving the F1 marrow and CD8+ T cells of Tc1 phenotype displayed a variable level of F1 engraftment (F1 chimerism of 0.6%, 42%, 44%, 73%, and 76%); thus, in contrast to the experiment shown in Fig 3, donor CD8 cells of Tc1-type were capable of abrogating the marrow graft rejection response. The administration of unmanipulated F1 CD8 cells also did not result in consistent F1 engraftment (F1 chimerism of 0.7%, 3%, 8%, 71%, and 86%). Thus, at 650 cGy host irradiation, donor T cells of naive or Tc1 phenotype partially abrogated the graft rejection response. In contrast, mice receiving F1 marrow and Tc2-type CD8 cells had a high level of F1 chimerism in 5 of 5 recipients at the 650 cGy dose of irradiation (F1 chimerism of 78%, 82%, 83%, 84%, and 88%). When the results shown in Figs 3 and 4 are pooled (650 cGy host irradiation), the Tc2 population was found to abrogate the rejection of TCD marrow (+Tc2 > marrow alone; P = .01) and found to prevent marrow rejection more potently than Tc1-type cells (+Tc2 > +Tc1; P = .008).
Tc2-type donor CD8+ T cells are enriched in their ability to abrogate marrow graft rejection. Host B6 (H-2b) mice were irradiated at 950, 650, or 600 cGy; all mice received 1 × 107 TCD bone marrow cells from B6D2F1 (H-2b/d) donor mice. Engraftment control mice (950/−) and rejection control mice (650/−) received only the donor bone marrow at the time of transplantation; other groups received additional in vitro-generated donor CD8+ T cells (1 × 107cells) of Tc1-type (650/Tc1, 600/Tc1) or Tc2-type (650/Tc2, 600/Tc2) or additional unmanipulated donor CD8 cells (650/naive CD8). Each treatment group consisted of 5 mice. Peripheral blood lymphocytes were isolated on day 41 posttransplant and stained with H-2bFITC (common to both donor and host cells) and H-2d PE (specific for donor cells); the percentage of donor and host chimerism was then determined by flow cytometry.
Tc2-type donor CD8+ T cells are enriched in their ability to abrogate marrow graft rejection. Host B6 (H-2b) mice were irradiated at 950, 650, or 600 cGy; all mice received 1 × 107 TCD bone marrow cells from B6D2F1 (H-2b/d) donor mice. Engraftment control mice (950/−) and rejection control mice (650/−) received only the donor bone marrow at the time of transplantation; other groups received additional in vitro-generated donor CD8+ T cells (1 × 107cells) of Tc1-type (650/Tc1, 600/Tc1) or Tc2-type (650/Tc2, 600/Tc2) or additional unmanipulated donor CD8 cells (650/naive CD8). Each treatment group consisted of 5 mice. Peripheral blood lymphocytes were isolated on day 41 posttransplant and stained with H-2bFITC (common to both donor and host cells) and H-2d PE (specific for donor cells); the percentage of donor and host chimerism was then determined by flow cytometry.
As Fig 4 shows, mice irradiated at 600 cGy that received marrow supplemented with Tc2-type cells were uniformly engrafted with the F1 marrow (F1 chimerism in 5 of 5 recipients; 64%, 66%, 71%, 78%, and 84% F1 chimerism); in contrast, 5 of 5 Tc1 recipients (600 cGy irradiation) displayed less than 1% F1 chimerism. Similar chimerism results were also obtained in this experiment at 161 days posttransplant (not shown). This experiment confirms that donor CD8+ T cells of Tc2 phenotype are enriched for an ability to prevent marrow graft rejection and shows that Tc2 cells are capable of facilitating alloengraftment in the setting of less intensive host preparative regimens.
DISCUSSION
In this report, we have evaluated the effect of donor CD8+T cells of Tc1 and Tc2 phenotype on marrow graft rejection and have determined that the Tc2 subset is particularly potent in its ability to facilitate alloengraftment. The Tc2 subset, which possessed cytolytic function and secreted type II cytokines, prevented the rejection of MHC-disparate marrow in sublethally irradiated hosts and allowed for a significant reduction in intensity of the host preparative regimen. Because we used an F1 into-parent model in these studies, our results demonstrate that Tc2-mediated abrogation of rejection does not require an alloaggressive response against the host. These findings thus confirm that non–host-reactive donor CD8 cells can play an important role in the regulation of marrow rejection and identify the Tc2 subset of CD8 cells as a population particularly enriched in its ability to facilitate alloengraftment.
The marked ability of the Tc2 population to facilitate alloengraftment indicates that the process of graft rejection is quite susceptible to regulation by non–host-reactive donor T cells. Previous marrow rejection studies using unmanipulated donor CD8+ T cells indicated that non–host-reactive CD8 cells were less potent than donor CD8 cells capable of mediating an alloaggressive response against the host.14 In this study, we have demonstrated that the non–host-reactive mechanism for preventing graft rejection can be augmented by using in vitro-generated donor CD8 cells enriched for cytotoxic function and type II cytokine secretion. Because host-reactive T-cell responses result in GVHD, use of Tc2-type donor populations to abrogate rejection via a non–host-reactive pathway represents a new strategy for improving the balance between alloengraftment and GVHD. In previous studies, we have demonstrated that host-reactive CD8+ T cells of Tc2 phenotype can mediate a GVL effect with reduced GVHD relative to unmanipulated donor T cells8; given these results, we would predict that host-reactive Tc2 cells might also represent a strategy for preventing rejection with reduced GVHD.
Previous studies have indicated that cytolytic function and an ability to clonally delete allospecific precursor CTL might be two parameters predictive for an ability to prevent graft rejection by a non–host-reactive, veto-type mechanism.12 Given that the Tc1- and Tc2-type donor CD8+ T cells possessed similar cytolytic function and ability to clonally delete allospecific precursor CTL, we reasoned that these CD8 subsets would prevent marrow rejection in this F1 into-parent model with similar efficacy. However, because the Tc2 subset was clearly superior in preventing marrow graft rejection, we believe that other functional characteristics must contribute to the in vivo effectiveness of this population.
The mechanism for the enhanced ability of the Tc2 subset to abrogate rejection relative to the Tc1 population is currently not known, but likely involves a noncytolytic characteristic of the Tc2-type cells. One possibility is that the Tc2 subset has a longer in vivo half-life or a favorable in vivo homing pattern. A second possibility is that the dichotomous cytokine secretion pattern of the Tc1 and Tc2 subsets might exert differential effects on the graft rejection process in vivo; eg, a murine tumor model has demonstrated that the type II cytokine IL-10 can block an allogeneic rejection response.26 However, we do not favor this explanation in our experiments, because our previous pilot studies using CD4+ Th2 cells, which secreted the type II cytokines but were noncytolytic, did not abrogate marrow rejection in an F1 into-parent model.
It is also possible that the Tc2 cells might be more effective than the Tc1 population at preventing marrow rejection mediated by host CD4+ T cells. The graft rejection model used in these studies involves disparities at both MHC class I and class II alloantigens; as such, radioresistant host CD4+ and CD8+ T cells may both have contributed to the marrow rejection process. In contrast to human CD8+ T cells, which can express HLA class II antigens, murine CD8+T cells are not known to express class II antigens; the Tc1 and Tc2 populations used in these studies were negative for MHC class II expression by routine FCM analysis. Because the classical veto mechanism is driven by host recognition of donor antigens, if Tc2 cells are capable of preventing CD4-mediated rejection, an alternative (non-veto) mechanism would presumably be operative.
Clinical translation of the non–host-reactive Tc2 strategy would require the development of methodologies for the generation and characterization of human Tc2 cells that are rendered nonreactive to host alloantigens. Application of this strategy in the setting of transplantation for nonmalignant diseases would likely result in a favorable balance between engraftment and GVHD. However, because the GVL effect may require an alloaggressive T-cell reaction, the use of host-reactive Tc2 cells for the purpose of abrogating rejection might be advantageous in the setting of leukemic hosts.
In conclusion, we have identified the Tc2 subset of donor CD8+ T cells as a population particularly enriched in its ability to abrogate marrow graft rejection. Our observation that the Tc2 population abrogates rejection without inducing an alloaggressive response helps define the biology of T-cell regulation of marrow graft rejection and offers a new strategy for achieving alloengraftment with reduced GVHD. Combined with our previous findings that host-reactive Tc2 cells can mediate a GVL effect with reduced GVHD, the current results suggest that donor cells of Tc2 phenotype may be the optimal CD8+ T-cell subset for use in the setting of allogeneic bone marrow transplantation. Marrow supplemented with both host-reactive and non–host-reactive Tc2 cells might optimally mediate antileukemia effects and prevent marrow rejection. As such, both cytokine phenotype (type I v type II) and specificity (host-reactive v non–host-reactive) of donor CD8+T cells are important considerations in attempts to broaden the future clinical applicability of allogeneic bone marrow transplantation.
Supported in part by a Translational Research Grant from the Leukemia Society of America.
Address reprint requests to Daniel H. Fowler, MD, National Institutes of Health, 9000 Rockville Pike, Bldg 10, Room 12N226, Bethesda, MD 20892.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" is accordance with 18 U.S.C. section 1734 solely to indicate this fact.