Abstract
The leukemic B lymphocytes from chronic lymphocytic leukemic (CLL) patients have a long survival in vivo, although ex vivo they rapidly die by apoptosis. To further investigate the mechanism of this, we have studied the influence of bone marrow stromal cells from normal subjects on apoptosis of B-CLL cells and normal umbilical cord blood (UCB) B lymphocytes. After 48 hours of incubation in medium alone, leukemic and normal B cells showed, respectively, 22 ± 3% and 31 ± 5% of apoptosis. Cocultures with stromal cells reduced the percentage of leukemic cells undergoing apoptosis (8 ± 2%, P< .0005) and prevented the loss of bcl-2 protein expression. In contrast, stromal cells slightly increased normal B-cell apoptosis (37 ± 6%). Direct contact between leukemic cells and stromal cells was found to be essential for inhibition of leukemic cell apoptosis; indeed, separation of leukemic cells from stromal cells by microporous membrane increased spontaneous apoptosis, and comparable results were obtained with stromal cell conditioned medium. The difference in behavior observed between normal and leukemic B cells plated on stromal cells can be explained by the fact that only a few normal B cells adhere to stromal cells in comparison with B-CLL cells. B-CLL cell adhesion to stromal cells is mediated by β1 and β2 integrins acting simultaneously. Contact between B-CLL cells and bone marrow stromal cells seems to play a major role in the accumulation and survival of B-CLL cells in the bone marrow.
B-CHRONIC LYMPHOCYTIC leukemia (B-CLL) is a malignant disease characterized by the accumulation of mature monoclonal CD5+ B cells.1 The majority of circulating cells appear to be nondividing, and it has been suggested that a prolonged life span could be responsible for the accumulation of the malignant B cells in vivo.2
The longevity of B cells is controlled by programmed cell death or apoptosis, an active process involving activation of an internally coded suicidal program and characterized by specific morphologic and biochemical changes leading to endonucleolytic degradation of the DNA at nucleosomal intervals.3,4 Apoptosis can be influenced by various factors that may be the appearance or disappearance of a stimulus, such as the withdrawal of growth factors for growth factor–dependant cells.5
Despite an apparent long half-life in vivo, B-CLL cells die in vitro during short-term culture in media supplemented by either autologous or fetal bovine serum.6,7 This fact suggest that the prolonged survival of B-CLL cells may be attributed to humoral or cellular factors capable of protecting these cells from apoptotic cell death. A variety of cytokines, such as interleukin-4 (IL-4), interferon α (IFN-α), IFN-γ, and IL-10, have been shown to be involved with the process of apoptosis in B-CLL cells, many exerting their effects by way of bcl-2 expression.8-11 In addition to cytokines, cell-cell and cell-matrix interactions have been shown to be critical in preventing apoptosis of malignant lymphocytes.12
Recently, Long et al13 reported that apoptosis of B-CLL cells can be prevented by contact with endothelial cell hybrids by way of integrins expressed on the malignant B lymphocytes. Given that B-cell proliferation and death involve interactions with stromal cells and their products,14 15 we have evaluated whether interactions with bone marrow (BM) stromal cells could play a major role in maintaining the malignant clone in this disease.
Examination of the factors and mechanisms involved in the process of apoptosis could be of value in the development of new therapeutic strategies for B-CLL.
This study provides evidence that BM stromal cells produce soluble factors inducing apoptosis of B-CLL cells, but that adhesion of these B-CLL cells to stromal cells rescues them from apoptosis and extends their life span in vitro.
MATERIAL AND METHODS
Patients.
Twenty B-CLL patients, 6 women and 14 men, with a median age of 61 (47 to 84) years were included in this study. Diagnosis was based on clinical examination, peripheral blood count, and immunophenotyping (Table 1). These patients were either untreated or had not received treatment for the previous 6 months.
Purification of CLL B-lymphocytes.
Heparinized venous blood from all patients was centrifugated over Ficoll-Hypaque (Lymphocyte Separation Medium, International Medical Products, Brussels, Belgium), and mononuclear cells were depleted from monocytes and T cells as previously described.16 After purification, the samples were stained with selected monoclonal antibodies and contained greater than 98% of CD19+ cells of which 67 ± 6% coexpressed CD5.
Purification of normal B lymphocytes.
CD19+ cells were purified from umbilical cord blood (UCB) on Ceprate LC CD19 affinity columns (CellPro, Bothell, WA) according to the manufacturer's instructions. Mononuclear cells were incubated 25 minutes at 4°C with a biotinylated mouse monoclonal Ig antihuman CD19. The cells were then washed and loaded onto an avidin-immunoaffinity column. Nonadsorbed cells were removed by washing the column with phosphate-buffered saline (PBS), and adsorbed cells were gathered by squeezing and eluting off the column. Cell numbers before and after separation were measured using Trypan blue staining.
The ratio of CD19+ cells in the mononuclear cell population obtained from 11 UCB samples varied from sample to sample (range 4% to 52%, mean 23 ± 5%), and 14 ± 5% of CD19+coexpressed the CD5 antigen. The Ceprate LC separation of UCB cells resulted in a population containing 89 ± 2% CD19+cells of which 57 ± 6% coexpressed CD5.
Phenotypic analysis.
Peripheral blood mononuclear cells or purified B lymphocytes were resuspended in PBS and washed and stained by direct immunofluorescence. The cells were incubated at room temperature for 30 minutes with specific monoclonal antibodies.
Double-labeling fluorescence staining was performed using fluorescein isothiocyanate (FITC)–conjugated CD5 and phycoerythrin (PE)–conjugated CD19 antibodies (Dakopatts, Glostrup, Denmark). Anti-CD25 (IL-2R1), CD3, CD14, and antibodies against surface Ig anti-κ, anti-λ, anti-α, anti-μ, and anti-δ were also purchased from Dakopatts.
The cells were analyzed with an EPICS-XL flowcytometer (Coulter, Hialeah, FL). The percentage of positive cells was determined by reference to nonspecific staining with antibodies of the same isotype.
BM stromal cell cultures.
After informed consent, BM from normal volunteer donors and B-CLL patients were collected by sternal aspiration and BM-mononuclear cells (BM-MNC) were isolated by layering on a Ficoll-Hypaque density gradient (International Medical Product). BM stromal layers were established as previously described.16
In brief, 5 × 105 BM-MNC were plated in 35-mm petri dishes containing 1 mL α-minimal essential medium (α-MEM; GIBCO, Grand Island, NY) supplemented with 15% fetal calf serum (FCS; Seralab, Sussex, UK) and 2 × 10−6 M methyl prednisolone (Pharmacia and Upjohn, Kalamazoo, MI) at 37°C, 7.5% CO2 in humidified air.
The adhering cells were fed at weekly intervals by complete replacement of the medium until a confluent layer of fibroblasts, macrophages, and fat cells had formed in each dish. Confluence was usually achieved after 4 to 6 weeks of culture.
Preparation of stromal cell–conditioned medium (stroma CM).
Conditioned media were prepared from 6-week-old stromal cell layers established from normal subjects when these cells had grown to form a confluent layer. Stromal cells were washed three times to remove methyl prednisolone, fed with fresh medium, and cultured for 48 hours.
The stromal cell supernatants were then collected after centrifugation and stored at −80°C until use.
Measurement of cytokines.
Cytokines were measured in conditioned media using specific immunologic procedures (enzyme-linked immunosorbent assay [ELISA]): IL-6 (Eurogenetics, Tessenderlo, Belgium; sensitivity 5 pg/mL), leukemia-inhibiting factor (LIF; Eurogenetics; sensitivity 10 pg/mL), IL-7 (Eurogenetics; sensitivity 10 pg/mL), granulocyte colony-stimulating factor (G-CSF; Quantikine, R&D Systems, Minneapolis, MN; sensitivity 11 pg/mL), stem cell factor (SCF; Quantikine; sensitivity 3 pg/mL), granulocyte-macrophage colony-stimulating factor (GM-CSF; Medgenix, Fleurus, Belgium; sensitivity 3 pg/mL), IL-10 (DNAX, Palo Alto, CA; sensitivity 40 pg/mL), macrophage inhibitory protein-1α (MIP-1α; ImmunoSource, Halle, Belgium; sensitivity 195 pg/mL), and transforming growth factor β (TGF-β; Promega Corp, Madison, WI; sensitivity 25 pg/mL).
Source of neutralizing antibodies.
Neutralizing antibodies to IL-6 were a murine IgG antibody (Eurogenetics), antibody to IL-10 was a goat IgG (R&D Systems), and chicken anti-human TGF-β was purchased from R&D systems. These antibodies were used at 10 μg/mL.
Cell culture studies.
Before each experiment, the media from stromal cell cultures was removed and these cells were washed three times with α-MEM.
Purified leukemic and normal B lymphocytes were resuspended in α-MEM + 15% FCS at a final concentration of 106/mL. Then, 2 mL of this cell suspension was placed in the wells of a 6-well plate or seeded on BM stromal cells in identical plates. In parallel experiments, cells were seeded onto 24 mm transwell diffusion chambers (0.4 μm microporous filter; Costar, Catalog No. 3408) and placed into stroma-coated 6-well plates.
Leukemic and normal B lymphocytes were also cultured in α-MEM supplemented with 50% stroma CM. All cell cultures were incubated for 48 hours at 37°C in 5% CO2 with 100% humidity.
Determination of cell viability.
Viability was determined at various time intervals by Trypan blue exclusion in a Neubauer counting chamber (Vel, Leuven, Belgium). Stromal cells were identifiable by their large size and different morphology. In some cases, nonviable cells were stained with propidium iodide (20 μg/mL) in PBS and counted by flow cytometry.
Determination of DNA fragmentation by flow cytometry.
Quantification of cells with degraded DNA was performed using a method described by Nicoletti et al.17
Cells to be analyzed were collected, washed, permeabilized, and incubated with solution containing propidium iodide (PI) and RNAse (Coulter DNA-Prep Reagent). The tubes were placed at 4°C in the dark overnight before analysis by flow cytometry.
Data collection was gated using forward light scatter and side light scatter to exclude cell debris and aggregates.
The PI fluorescence of individual nuclei was measured using a Coulter EPIC XL. At least 5 × 103 cells of each sample were analyzed. Apoptotic cells are represented by a broad hypodiploid peak of cells that is easily discriminable from the peak of cells with diploid DNA content in the red fluorescence channel. All data were analysed using EPICS Elite 4.0 software.
When B-lymphocytes were cultured in the presence of stromal cells, cell cycle analysis was performed by labeling cells prestained with biotinylated anti-CD19 and streptavidin-FITC (Pharmingen, San Diego, CA) with PI and determining their DNA content by flow cytometry as previously described.
Tunel assay.
DNA fragmentation in apoptotic cells was detected according to the method described by Gavrieli.18 B cells were fixed in 4% buffered formaldehyde (pH 7.4) for 30 minutes at room temperature. Then, after washing in PBS, B cells were resuspended in permeabilization solution (0.1% Triton X-100 in 0.1% sodium citrate) for 2 minutes on ice. After washing, B cells were resuspended in TUNEL reaction mixture (dUTP-FITC) at 37°C for 1 hour according to the manufacturer's instruction (Boehringer Mannheim Biochemical, Indianapolis, IN). Cells were washed and analyzed by flow cytometry. Control staining was performed on aliquots of the same cells treated with the staining mixture without terminal deoxynucleotidyl transferase (TdT). As previously described, TUNEL assay was performed in cocultures with B cells prestained with biotinylated anti-CD19 and streptavidin-PE (Pharmingen).
Adhesion assay.
Normal and leukemic B cells were radiolabeled by incubating 1 to 5 × 106 cells with 100 μCi Na251CrO4 for 1 hour at 37°C.51Cr-labeled B cells were washed and plated into wells containing confluent BM stromal cells and incubated at 37°C for 2 hours. After two washes to remove nonadherent cells, the stromal cell–adherent B cells were quantitated on a γ-counter. All the experiments were performed in triplicate, and the percentage of adhesion was calculated as follows:
For inhibition studies, B-CLL cells were incubated for 1 hour with the following blocking antibodies at 10 μg/mL: anti-CD11a, anti-CD18, anti-CD29, and anti-CD49d (Immunotech, Marseille, France) before addition to wells. Stromal cells were incubated with anti-CD54 and anti-CD106 1 hour before the addition of labeled B-CLL cells. Results were compared with those of wells containing isotype-matched irrelevant antibody.
Bcl-2 expression.
Cells were permeabilized by treatment with Permeafix (Ortho Diagnostics Systems, Beerse, Belgium) for 40 minutes and then washed in cold PBS. The washed cells were then incubated with FITC-labeled mouse antihuman bcl-2 monoclonal antibody (MoAb; Dako, Glostrup, Denmark) for 30 minutes.
The cells were then washed in PBS, and cell-associated fluorescence analysis was performed on the flowcytometer. A mouse IgG1 MoAb was used as a negative control. In cell cocultures, bcl-2 expression was evaluated in B cells prestained with biotinylated anti-CD19 and streptavidin-PE.
To quantify bcl-2 expression, the cytometer was calibrated using FITC-labeled micro-beads (Immuno-Brite, Coulter). The set of four beads used titred, respectively, 31,500, 115,000, 460,000, and 1,115,000 mean equivalent of soluble fluorochrome (MESF) units.
A linear regression model was used to correlate mean values of the fluorescent bead peaks to the log10 of corresponding MESF units. This method allows quantification of mean bcl-2 expression of the tested population and direct comparison of samples analyzed at different times.
Statistical analysis.
The Wilcoxon's nonparametric test was used to analyze the statistical significance of the experimental results.
RESULTS
Spontaneous cell death of B lymphocytes in vitro.
B cells from 20 patients and 11 UCB samples were cultured in medium alone, and apoptotic cell death was evaluated by light microscopy and flow cytometry.
Purified normal and leukemic B lymphocytes rapidly initiated apoptosis when placed in culture as previously described.6 19
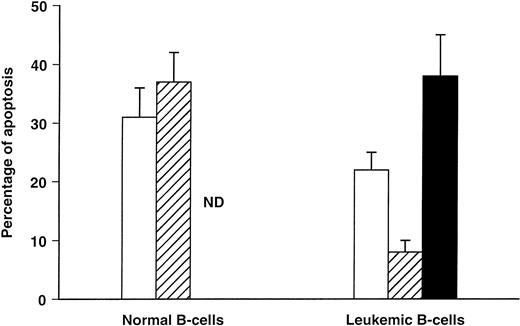
After 48 hours of culture, B cells showed morphologic evidence of apoptosis, such as nuclear fragmentation and loss of cell volume. As measured by flow cytometry, the mean percentage of apoptotic cells was 31 ± 5% and 22 ± 3%, respectively, for normal and leukemic B cells (Fig 1). These B cells were 80% to 100% dead after 7 days of culture, and the appearance of cells with degraded DNA was associated with the loss of viability through the culture period.
Percentage of apoptotic B cells after 48 hours of culture in medium alone (control MEM) or in the presence of stromal cells (with or without contact). DNA fragmentation was revealed by flow cytometry. Results are expressed as mean ± SEM of 11 experiments for normal B cells and 20 for B-CLL cells. (□), Control MEM; (▨), stromal cell contact; (▪), no stromal cell contact.
Percentage of apoptotic B cells after 48 hours of culture in medium alone (control MEM) or in the presence of stromal cells (with or without contact). DNA fragmentation was revealed by flow cytometry. Results are expressed as mean ± SEM of 11 experiments for normal B cells and 20 for B-CLL cells. (□), Control MEM; (▨), stromal cell contact; (▪), no stromal cell contact.
BM stromal cells prevent apoptosis of B-CLL cells.
To determine whether the presence of normal stromal cells could influence cell viability, B cells were cultured for 48 hours on BM stromal cells. Quantification of the percentage of cells with degraded DNA was performed by PI staining of permeabilized cells prestained with CD19. As shown in Fig 1, apoptosis of leukemic B cells was significantly reduced by plating these cells on normal allogeneic stromal cells (8 ± 2 v 22 ± 3%, P < .0005). In contrast, when normal B cells were cocultured with stromal cells, the percentage of B cells undergoing apoptosis was slightly but not significantly increased (37 ± 6% v 31 ± 5%).
When a microporous membrane was inserted between stroma and leukemic B cells, the protective effect of stromal cells was lost and strikingly, the percentage of apoptotic cells was increased (38 ± 7% v22 ± 3%, P < .001; Fig 1).
These observations suggest that stromal cells secrete factors that diffuse through microporous membrane and are able to induce apoptosis of leukemic B cells. Moreover, intimate B-cell–stroma contact is essential to rescue leukemic cells from spontaneous apoptosis and apoptosis induced by soluble factors produced by stromal cells.
Stroma CM induces apoptosis of normal and leukemic B cells.
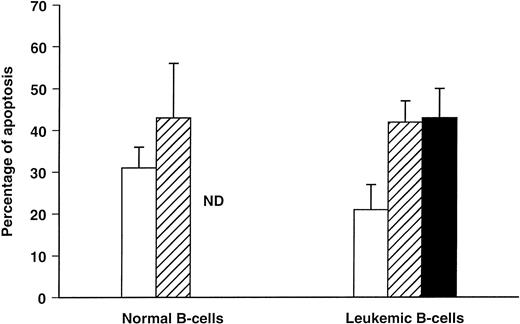
To confirm that stromal cells secrete factors inducing B-cell apoptosis, we have cultured normal and leukemic B cells in α-MEM supplemented with 50% stroma CM.
As shown in Fig 2, increased apoptosis of normal and leukemic B cells was obtained in the presence of stroma CM, confirming that stromal cells secrete factors responsible for B-cell apoptosis.
Effect of stroma CM on B cell apoptosis. Stroma CM was prepared as described in Materials and Methods. Results are expressed as the mean ± SEM of nine experiments and represent the percentage of apoptotic B cells after 48 hours of culture in the presence of α-MEM supplemented with stroma CM at 50% compared with cultures in α-MEM alone or in the presence of stromal cells but without contact. (□), Control MEM; (▨), stroma CM; (▪), no stromal cell contact.
Effect of stroma CM on B cell apoptosis. Stroma CM was prepared as described in Materials and Methods. Results are expressed as the mean ± SEM of nine experiments and represent the percentage of apoptotic B cells after 48 hours of culture in the presence of α-MEM supplemented with stroma CM at 50% compared with cultures in α-MEM alone or in the presence of stromal cells but without contact. (□), Control MEM; (▨), stroma CM; (▪), no stromal cell contact.
After 48 hours, in all CLL patients tested (n = 9), spontaneous and stroma CM–induced apoptosis mean percentages were, respectively, 21 ± 6% and 42 ± 5% (P < .012), and similar results were obtained when B cells were separated from stroma by filter (43 ± 7%, P < .008). Stroma CM also induced apoptosis of normal B cells (51 ±14% v 43 ± 13%, in medium alone, n = 4) but this difference was not significant.
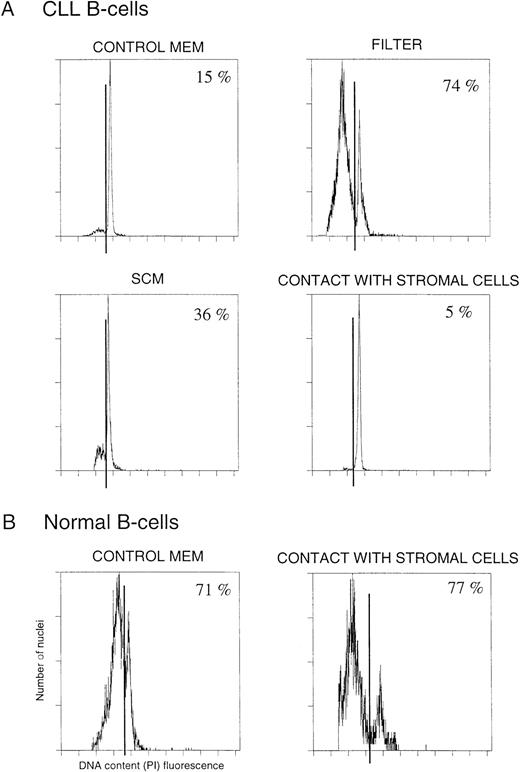
Profile of DNA fluorescence in CLL and UCB B cells cultured in these various conditions are shown in Fig 3. Some samples were labeled with biotinylated dUTP using the TUNEL assay as described previously and showed comparable results (data not shown).
DNA fluorescence (PI mediated) in CLL (A) and UCB (B) B cells cultured in various conditions.
DNA fluorescence (PI mediated) in CLL (A) and UCB (B) B cells cultured in various conditions.
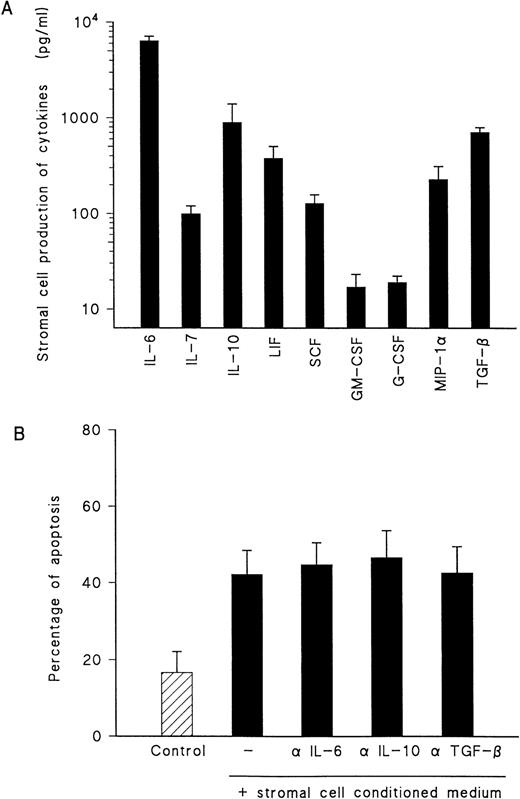
To establish the nature of soluble factors produced by stromal cells and inducing apoptosis, the cytokines present in conditioned medium and the effect of neutralizing antibodies to specific cytokines have been evaluated. BM stromal cells produce constitutively a wide variety of cytokines but at various levels (Fig 4A). Using neutralizing antibodies, we have determined the potential role of IL-6, IL-10, and TGF-β as inducers of apoptosis. Indeed, IL-6 represents the major cytokine constitutively released by stromal cells (>5 ng/mL), and IL-10 or TGF-β have been described as modulators of apoptosis in several cell types including B lymphocytes. Our observations, detailed in Fig 4B, showed that these cytokines are not involved in the induction of apoptosis by stroma CM.
(A) Cytokine production by stromal cells. Supernatant from stromal cells were collected 2 days after media change and assayed by ELISA for the above cytokines. Values are the mean ± SEM of 10 experiments. (B) Induction of B-cell apoptosis by stroma CM and influence of neutralizing antibodies to cytokines. Results are expressed as percentage of apoptotic cells and represent the mean of five experiments.
(A) Cytokine production by stromal cells. Supernatant from stromal cells were collected 2 days after media change and assayed by ELISA for the above cytokines. Values are the mean ± SEM of 10 experiments. (B) Induction of B-cell apoptosis by stroma CM and influence of neutralizing antibodies to cytokines. Results are expressed as percentage of apoptotic cells and represent the mean of five experiments.
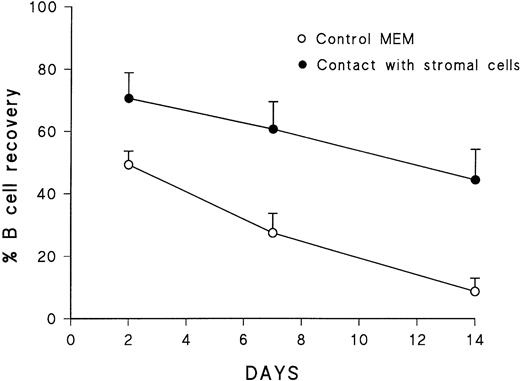
Survival of leukemic B cells on BM stromal cells.
As shown in Fig5, the culture of B cells in medium alone led to a significant decrease in cell recovery. The number of B cells recovered after 48 hours and 7 days of culture was, respectively, 49 ± 4% (mean ± SEM) and 28 ± 6% of those originally seeded. After 14 days of culture, only 9 ± 4% of B cells remained alive. However, in the contact with stromal cells, the recovery of viable cells increased significantly, with a mean cell recovery of 61± 9% and 45 ± 10%, respectively, after 7 and 14 days. In contrast, after 7 days of culture with or without stromal cells, the majority of normal B cells were dead. These results confirmed our previous observations and showed a prolonged survival of leukemic B cells seeded on stromal cells compared with that of their normal counterpart in the same culture conditions.
Percentage of leukemic B cells recovered from culture in the presence or absence of stromal cells. Values are the mean of four experiments and refer to viable B cells after various periods of culture, determined by Typan blue exclusion and compared with those originally seeded.
Percentage of leukemic B cells recovered from culture in the presence or absence of stromal cells. Values are the mean of four experiments and refer to viable B cells after various periods of culture, determined by Typan blue exclusion and compared with those originally seeded.
Viability was also assessed using flow cytometry to quantify the percentage of cells, prestained with CD19, capable of excluding propidium iodide. After 7 days of culture, in medium alone, the mean proportion of viable cells declined to 56 ± 2% (n = 3). In contrast with stromal cells, the viability of B-CLL cells was increased (88 ± 1%; data not shown).
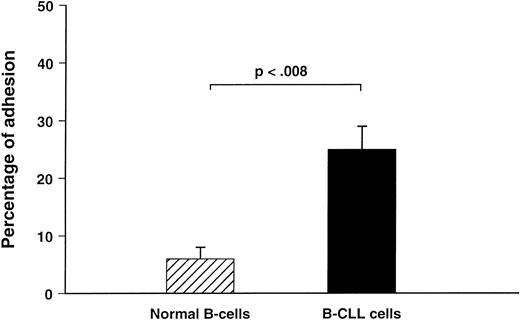
Adhesion of B cells to stromal cells.
After having observed that contact between leukemic B cells and stromal cells is essential for their protection from apoptosis, we examined the adhesion of B-CLL cells and normal B lymphocytes to stromal cells.
Figure 6 shows experiments comparing the level of adhesion of 51Cr-labeled normal (n = 5) and leukemic B cells (n = 15). After 2 hours, 25 ± 4% (range 16% to 66%) of B-CLL cells adhered to stromal cells, whereas adhesion of UCB B cells was 6 ± 2%.
Adhesion of normal (n = 5) and leukemic (n = 15) B cells to stromal cells. Percentage of adhesion was calculated as described in Materials and Methods.
Adhesion of normal (n = 5) and leukemic (n = 15) B cells to stromal cells. Percentage of adhesion was calculated as described in Materials and Methods.
The differences in behavior observed between normal and leukemic B cells plated on stromal cells could be related to the level of cell adhesion.
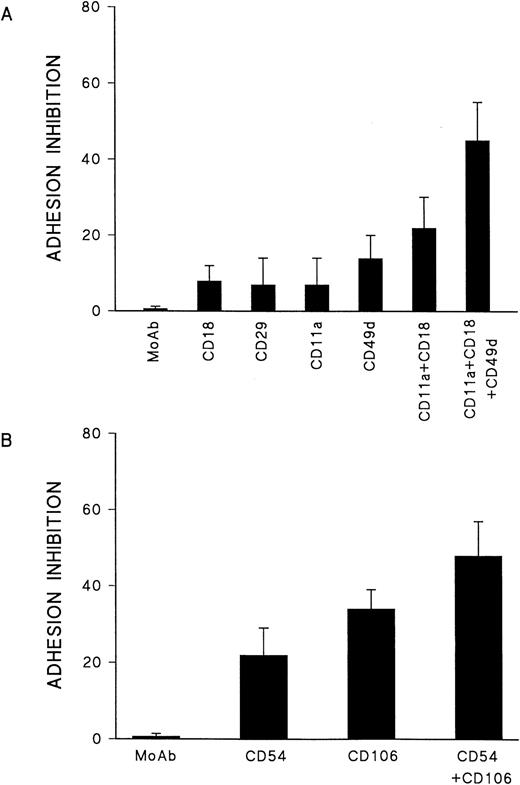
To investigate the mechanism of adhesion, the binding of leukemic B-lymphocytes to stromal cells was evaluated in the presence of several blocking antibodies to antagonize β1- and β2-integrin–dependent pathways. As shown in Fig 7A, blocking of CD18- or CD29-dependant adhesion mechanisms did not reduce the binding of B-CLL cells to stromal cells (<10% inhibition). There was also no inhibition of B-CLL binding after treatment with anti-CD11a. In six out of eight cases examined, anti-CD49d induced moderate inhibition of B-CLL adhesion (14 ± 6%). However, when anti-CD11a was associated to anti-CD18, more than 20% inhibition was observed (P < .04). Addition of anti-CD49d to the combination of anti-CD18/anti-CD11a increased significantly the inhibition of binding in all cases tested (45 ± 10%, P < .04). Adhesion of B-CLL cells to stromal cells is thus partly mediated by β1- and β2-integrins acting simultaneously.
(A) Blocking of adhesion of B-CLL cells to stromal cells. Leukemic cells were preincubated for 1 hour with blocking antibodies before plating on stromal cells. Each bar represents the mean of adhesion inhibition of eight experiments. (B) Blocking of B-CLL cell adhesion to stromal cells untreated or treated with anti-CD54 and/or anti-CD106. B-CLL cells were simultaneously preincubated with antibodies to CD11a/CD18 or CD49d.
(A) Blocking of adhesion of B-CLL cells to stromal cells. Leukemic cells were preincubated for 1 hour with blocking antibodies before plating on stromal cells. Each bar represents the mean of adhesion inhibition of eight experiments. (B) Blocking of B-CLL cell adhesion to stromal cells untreated or treated with anti-CD54 and/or anti-CD106. B-CLL cells were simultaneously preincubated with antibodies to CD11a/CD18 or CD49d.
To evaluate the potential role of ICAM-1 (CD54) and VCAM-1 (CD106) in the adhesion of B-CLL cells, BM stromal cells were incubated with antibodies directed to these two ligands. B-CLL cells were simultaneously preincubated with antibodies to β1- and β2-integrins (VLA-4/VCAM-1 and LFA-1/CD54). Blocking antibodies against ICAM-1 and VCAM-1 inhibited adhesion by 22 ± 7% and 34 ± 5% (Fig 7B). However, the combination of these two antibodies impaired significantly B-CLL cell adhesion to stromal cells (inhibition of 48 ± 9, P < .04) compared with cells treated with anti-CD54 or anti-CD106 alone. These results show that both β1- and β2-integrins VLA-4 and LFA-1 and their ligands VCAM-1 and ICAM-1 are involved in the adhesion of B-CLL cells to stromal cells. However, the fact that the combination of β1- and β2- integrins, associated with their ligands CD106 and CD54, was unable to block completely adhesion process suggests that other mechanisms are involved in the adhesion of B-CLL cells to stroma.
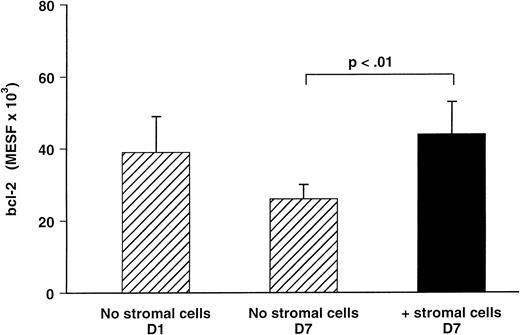
Bcl-2 analysis by flow-cytometry.
Bcl-2 was studied at the protein level by flow-cytometry on permeabilized cells in eight cases of B-CLL (Fig 8). Before culture, more than 90% of cells from all cases tested constitutively expressed bcl-2 at a high level (39 ± 10 × 103 MESF). After 7 days of culture in medium alone, the level of bcl-2 expression was downregulated (26 ± 4 × 103 MESF), although the percentage of bcl-2 positive cells remained constant.
Bcl-2 expression of B-CLL cells cultured in the presence or absence of stromal cells. The results are expressed as the mean ± SEM of eight experiments and represent the level of bcl-2 expressed as MESF.
Bcl-2 expression of B-CLL cells cultured in the presence or absence of stromal cells. The results are expressed as the mean ± SEM of eight experiments and represent the level of bcl-2 expressed as MESF.
However, after 7 days of culture in the presence of stromal cells, the expression of bcl-2 in B cells was 44 ± 9 × 103MESF and comparable with the level of bcl-2 seen at day 0. The loss of bcl-2 protein was thus inhibited in the presence of stromal cells.
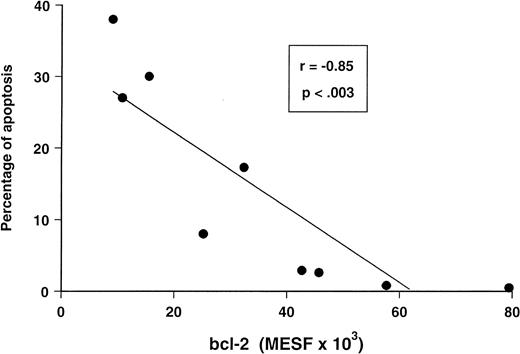
For nine B-CLL cases tested, the reduction in bcl-2 expression was found to correlate with the rate of B-CLL apoptosis (Fig 9).
Relationship between the level of bcl-2 protein in B-CLL cells and their degree of apoptosis during in vitro culture. These two parameters were determined in nine cases.
Relationship between the level of bcl-2 protein in B-CLL cells and their degree of apoptosis during in vitro culture. These two parameters were determined in nine cases.
DISCUSSION
B-CLL cells in vivo display enhanced survival, and their level of apoptosis remains low compared with that of normal B lymphocytes. In contrast, B-CLL cells in vitro die spontaneously and are difficult to keep alive. We have shown in the present study that leukemic B cells become able to survive in vitro when BM stromal cells are added in vitro, as they do in vivo and as long as a cell contact is maintained between these two cell types.
BM stromal cells synthesize several cytokines, including CSFs, IL-6, IL-7, IL-10, TGF-β, and SCF, and exert a complex regulatory function mediated by these soluble growth factors and extracellular matrix proteins.20 Self-renewal and differentiation of B-cell precursors depend on interactions with BM stromal cells and extracellular matrix.21 B-lymphocyte production is also regulated by cytokines produced in the microenvironment.22A number of previous studies have shown that contact with BM stroma induces proliferation and survival of acute lymphoblastic leukemia (ALL) cells in cultures.23 24 The adhesion of B-CLL cells to stromal cells is crucial for their survival because these cells die when separated from the stromal cells by a microporous membrane. Moreover, the protective effect from apoptosis, mediated by contact, cannot be substituted by addition of stroma CM.
Our results obtained with stroma CM indicate that soluble factors or cytokines produced by stromal cells are unable to protect B-CLL cells from apoptosis but on the contrary significantly increase their apoptosis. Indeed, it has been described that B-CLL cell apoptosis can be influenced by various cytokines such as IL-4, IFN-α, IFN-γ, and IL-10.8-11 Soluble factors produced constitutively by stromal cells are responsible for the induction of apoptosis in B-CLL cells. So far, only two cytokines, IL-5 and IL-10, have been described as inducers of apoptosis in CLL.11, 25However, IL-5 is not produced by stromal cells, and our results obtained with neutralizing antibodies to IL-6, IL-10, and TGF-β show that these cytokines are not involved in the increase of apoptosis by stroma CM. It seems thus interesting to isolate factor(s) inducing apoptosis by methods such as gel filtration and reverse-phase chromatography.
Signals other than soluble factors present in conditioned medium are clearly required for the survival of these B-CLL cells, such as matrix- or membrane-bound cytokines and/or messages transduced to the nucleus by way of other cell surface receptors.
The survival of B-CLL cells in coculture with stroma has been reported recently. Panayiotidis and coworkers26 described the survival of leukemic B cells up to 6 weeks in an in vitro BM environment. Other in vitro studies revealed that stromal cell cultures supplemented with conditioned media from the human bladder carcinoma line 5637 were able to support the growth of B-CLL cells for up to 9 to 13 weeks.27
In our study, CD5+ B cells, which have been reported to be abundant in UCB and have been suggested to represent a normal counterpart of B-CLL cells, were also examined.28 In contrast to B-CLL cells, normal CD5+ B cells were unable to survive in coculture with stromal cells. The difference in behavior observed between normal and leukemic B cells plated on stromal cells can be explained by our observation that only a few UCB B cells adhered to stromal cells in comparison with B-CLL cells. It has been suggested that specific binding to marrow fibroblasts is part of the differentiation program of B-lineage precursors and that this binding activity decreases during B-lineage differentiation.29 This could therefore explain a different adhesion between normal and leukemic CD5+ B lymphocytes. However, another hypothesis could be that normal B cells are insensitive to the “survival signal” mediated by contact between B cells and stromal cells.
Indeed, two cytokines so far, IL-5 and IL-13, can induce the apoptosis in B-CLL but not in normal peripheral B cells.25 30However, although the intimate mechanism of stroma-mediated cell survival remains unknown, our data at least show that the survival of leukemic cells depends on direct cell-cell contact but not on soluble cytokines produced constitutively by stromal cells.
Survival signals may be provided by interactions between adhesion proteins expressed on B-CLL cells and their ligands in the microenvironment. Such adhesion interactions have been shown to modulate apoptosis in others systems.31 Long et al13 have shown that, in B-CLL, apoptosis and IL-7 gene expression can be mediated by cell-cell contact with endothelial cells. It has been described that B-CLL cells express integrins, such as VLA-4, and various adhesion molecules, such as LFA-1 and ICAM-1, at a variable level.32 33 The fact that VLA-4 and its ligand VCAM-1 are obligatory proteins in the adhesion of B precursors to stromal cells led us to evaluate the role of β1- and β2-integrins in the adhesion of B-CLL cells to stromal cells.
As reported by other groups, we were unable to inhibit significantly B-CLL adhesion using individual blocking antibodies directed to CD11a, CD18, CD29 or CD49d. Approximately 30% to 50% inhibition of B-CLL adhesion could be obtained with the combination of anti-CD11a/CD18/CD29/CD49d suggesting that binding of leukemic cells to stromal cells requires the simultaneous action of β1- and β2-integrins. CD54 and CD106 represent the ligands on stromal cells for B-CLL cell binding and interact with CD11a/CD18 and CD49d expressed by leukemic cells. However, concomitant blockade of β1- and β2-integrins was essential to obtain significant inhibition of B-CLL adhesion. This simultaneous intervention of β1- and β2-integrins has been previously reported by other groups evaluating the adhesion of acute myeloid leukemia (AML) cells or normal hematopoietic progenitors to stromal cells.34,35 It has been recently shown that binding through both the CD11a/CD18-CD54 and CD49d–VCAM-1 pathways can prevent apoptosis of germinal center B cells and may thus contribute to the process of B-cell selection.36
Presently, we can only speculate on the nature of signals involved in the survival of B-CLL cells observed in this study; further studies are required to answer this question. For instance, the contact between B cells and stromal cells could induce the release of specific factors able to protect B cells from apoptosis. The factors crucial for the survival of B-CLL cells could be either membrane-bound or concentrated in the extracellular matrix. In this context, Verfaillie et al37 have suggested that, although not necessary for proliferation, the close association of progenitor cells with the stroma may be crucial for the regulation and ordered progression of normal hematopoiesis. This effect may be mediated by high levels of cytokines concentrated by glycoaminoglycans in the stromal extracellular matrix.37
Because apoptosis seems to be controlled, at least in part, by the proto-oncogene bcl-2, we investigated the possibility that stromal cells maintain CLL B-cell viability by regulating bcl-2 expression. Using flow cytometry, we observed a reduction in bcl-2 expression in B-CLL cells during in vitro culture, and this reduction was found to correlate with the level of apoptosis as reported recently.38 39
Contact between B cells and stromal cells could trigger delivered “signals” that prevent the loss of bcl-2 and consequently inhibit cell death. In a recent study, BM stromal cells have also been shown to regulate not only bcl-2 but also bax expression in pro–B cells, confirming the importance of stromal cell function in the maintenance of cell viability of B-lineage cells.40 Bcl-2 is only one factor among several genes regulating apoptosis. Indeed, several groups have reported the existence of bcl-2–related genes that produce a range of heterodimers that function as dominant regulators of apoptosis.41 Bcl-2, bax, bcl-xL, and bcl-xS have an interrelated role in the control of apoptosis, and their expression in CLL is skewed toward prevention of apoptosis .42 43Additional experiments will address the influence of stromal cells in the regulation of bcl-2 gene family.
In summary, we have shown that contact with BM stromal cells protects leukemic B cells from spontaneous apoptosis and apoptosis induced by soluble factors produced constitutively by stromal cells. However, further investigations will be necessary to identify other molecules involved in the interaction between stromal cells and leukemic cells and the signals able to rescue leukemic cells from apoptosis.
Understanding of the role of adhesion proteins in B-CLL cell adhesion to stromal cells and the mechanisms responsible for the prolonged survival of B-CLL cells in vivo could lead to the elucidation of the pathogenesis of B-CLL and to the development of new therapeutic strategies.
Supported by Télévie-FNRS Grant No. 7.4506.94 and by a grant from the Bekales Foundation.
Address reprint requests to L. Lagneaux, Institut J. Bordet, Laboratoire d'hématologie, 1 Rue Héger-Bordet, 1000 Brussels, Belgium.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" is accordance with 18 U.S.C. section 1734 solely to indicate this fact.