Control of intracellular bacterial infections requires interferon-γ (IFN-γ) both for establishing a Th1 T-cell response and for activating macrophages to kill the bacteria. Exposure of mice deficient in IFN-γ to mycobacterial infection produces an immune response characterized by a Th2 T-cell phenotype, florid bacterial growth, and death. We report here that IFN-γ–deficient mice infected with mycobacteria also undergo a dramatic remodeling of the hematopoietic system. Myeloid cell proliferation proceeds unchecked throughout the course of mycobacterial infection, resulting in a transition to extramedullary hematopoiesis. The splenic architecture of infected IFN-γ–deficient mice is completely effaced by expansion of macrophages, granulocytes, and extramedullary hematopoietic tissue. These features coincide with splenomegaly, an increase in splenic myeloid colony-forming activity, and marked granulocytosis in the peripheral blood. Systemic levels of cytokines are elevated, particularly interleukin-6 (IL-6) and granulocyte colony-stimulating factor (G-CSF). These results suggest that in addition to its central role in cellular immunity, IFN-γ may be a key cytokine in coordinate regulation of immune effector cells and myelopoiesis. This model should be valuable for deciphering the cross-talk between the immune response and hematopoiesis during bacterial infection and for improving our understanding of the mechanisms that control chronic infections.
ANALYSIS OF THE host response to mycobacterial infections has shown much about the roles of cytokines in the regulation of the aquired immune response. One of the most important cytokines involved in antimycobacterial immunity is interferon-γ (IFN-γ). Several lines of evidence demonstrate that IFN-γ has an indispensible role in antimycobacterial immunity. Mice lacking functional IFN-γ or IFN-γ receptor (IFN-γR) genes1-5 are extremely susceptible to infection with both virulent Mycobacterium tuberculosis1, 3 and avirulent M bovis BCG strain.2 Humans with null mutations in IFN-γR genes are also susceptible to mycobacterial infection.6 7
The mechanism of IFN-γ action in controlling and eliminating mycobacteria involves at least two functions; the development of a Th1 immune response and the activation of macrophages (reviewed in Cooper and Flynn8). On recognition of infected macrophages, IFN-γ production from antigen-specific CD4+ T cells is initiated to activate macrophages to kill intracellular bacteria. The mechanism of action involves the activation of downstream molecules such as the transcription factors STAT1 and IRF-1,9 which are considered essential for regulating the expression of genes whose products are required for macrophage effector functions such as inducible nitric oxide synthase (iNOS). Mice with targeted mutations in the genes encoding STAT1, IRF-1, and iNOS are susceptible to mycobacterial infection,10-13as well as other intracellular pathogens.14 15
The response of an organism to infection entails a carefully choreographed series of inflammatory events, with macrophages and neutrophils playing a critical role in the acute cellular phase followed by the development of aquired immunity specifically directed against the pathogen. The hematopoietic system must respond to infection by adjusting the production of the appropriate cell types. The roles of specific cytokines in the production of different hematopoietic cell types are relatively well understood, but less is known about the coordinate regulation of the immune response and hematopoiesis when stressed by infections. In immunodeficient mice susceptible to chronic infection, this regulation is perturbed, providing a valuable model system.
While doing experimental infections in IFN-γ–deficient mice using an avirulent M bovis strain (BCG), we observed that mice succumbed to infection as expected2 and had a total shift to a Th2 response to the bacteria. However, in contrast to wild-type animals, IFN-γ–deficient mice mounted a pathologic inflammatory response characterized by expansion of hematopoietic lineages in the spleen and bone marrow, an increase in precursor activity in these organs, and a massive granulocytosis in the spleen and blood. The results suggest that in the absence of IFN-γ and effective macrophage function, a pathologic granulocytic reponse is mounted in an attempt by the organism to combat mycobacterial infection. These data also suggest that IFN-γ is a key cytokine in regulating communication between immune effector cells and the hematopoietic system.
MATERIALS AND METHODS
Mice.
Mice heterozygous for the targeted mutation in the gene encoding IFN-γ created by Dalton et al2 were initially obtained from The Jackson Laboratories (Bar Harbor, ME). We used IFN-γ −/− mice on either the Balb/c or C57BL/6 backgrounds throughout these experiments. The pathology observed and time to death were essentially the same in either strain, however, some minor differences were observed, and these are noted in the text, tables, and figure legends where appropriate. IFN-γ −/− mice have been housed and bred under conventional conditions for over 2.5 years with no observable consequences to their health. Extensive analysis has been performed on naive IFN-γ −/− mice and relevant results are noted in the text. Most mice used in this study were obtained by intercrossing −/− or +/+ mice. In some experiments, Balb/c or C57BL/6 mice were purchased from The Jackson Laboratories and used as controls. When genotyping was necessary, Southern blots of BamHI-digested tail DNA were probed with a full-length IFN-γ cDNA.
Mycobacteria.
Infections.
Mice were infected at 8 to 12 weeks of age by either the intravenous (IV) or intraperitoneal (IP) route with comparable results. A total of seven independent experiments were performed, using four to 20 mice per group. Mice were killed at a variety of times postinfection to examine features of the pathology. For most experiments, mice were inoculated with 1 × 105 colony-forming units (CFUs) of bacteria. For time course studies, 1 × 106 CFUs bacteria were used. This increased the time to morbidity by approximately 2 weeks. Bacterial numbers injected were determined by plating serial dilutions of the bacterial suspension on MH10 plates and counting colonies 21 to 28 days later.
Histology.
Tissues (liver and spleen) were fixed in phosphate-buffered formalin and embedded. Sections were stained with hematoxylin and eosin or with the Ziehl-Neelsen stain for acid-fast bacteria and counterstained with methylene blue. Bone marrow aspirates and spleen cells were analyzed by cytospin and staining with Leukostat (Fischer Diagnostics, Pittsburgh, PA).
Blood and cytospins.
Mice were bled from the retro-orbital plexus and blood collected into heparinized tubes (Vacutainer; Becton Dickinson, Franklin Lakes, NJ). Smears were made and stained with Leukostat. White blood cell (WBC) counts were made by diluting blood 1:100 in 2% acetic acid. Numbers are expressed as WBC per microliter. Plasma was stored at −20°C until required for cytokine analysis.
Dispersed spleen and bone marrow cells (2 × 104) were centrifuged onto slides and stained with Leukostat. Cell differentials were performed and details are recorded in the table notes and figure legends. Generally, cells from individual mice were counted (100 to 300 cells). Results are recorded and the averages ± standard devations (SD).
Cytokine levels.
Cytokine levels in the plasma were determined by enzyme-linked immunosorbent assay (ELISA) using specific reagents for interleukin-6 (IL-6), IL-3, granulocyte-macrophage colony-stimulating factor (GM-CSF), IL-12, IL-10 (Pharmingen, San Diego, CA), tumor necrosis factor-α (TNF-α) and IFN-γ (Endogen, Boston, MA). Detection limits for ELISAs were as follows: IL-3 (5 pg/mL), IL-6 (20 pg/mL), GM-CSF (100 pg/mL), IL-10 (50 pg/mL), TNF-α (100 pg/mL), IFN-γ (20 pg/mL), IL-12 (50 pg/mL). G-CSF levels were assayed using a G-CSF–responsive cell line (Ba/F3-GR) as described.18These cells are Ba/F3 cells transfected with a plasmid encoding the murine G-CSF receptor under the control of a constitutive promoter. These cells can respond to both IL-3 (Ba/F3 is an IL-3–dependent pro-B–cell line) as well as G-CSF. Each sample was analyzed for both IL-3 and G-CSF along with other cytokines. Because plasma IL-3 levels are generally low (see Fig 7), it is a reasonable assumption that G-CSF levels are being measured, with the exception of any unknown factors that could stimulate these cells. A microassay was used as described.18 Briefly, Ba/F3-GR cells were washed three times with RPMI/10% fetal bovine serum (FBS) and plated in Terasaki wells at 200 cells per well in a volume of 5 μL. Serially diluted plasma or IL-3 or G-CSF was added in a volume of 5 μL. After 36 hours, the number of live cells per well was scored visually. Results are reported as the lowest dilution factor in which there were 100 live cells per well.
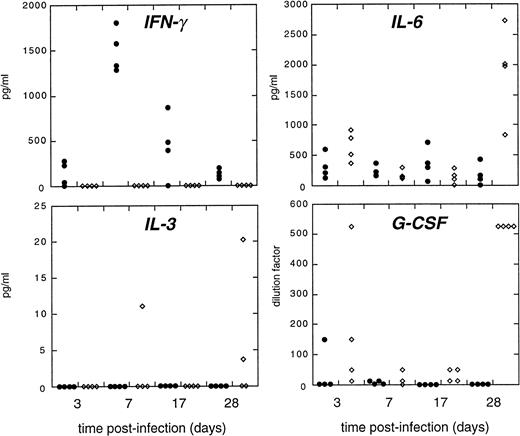
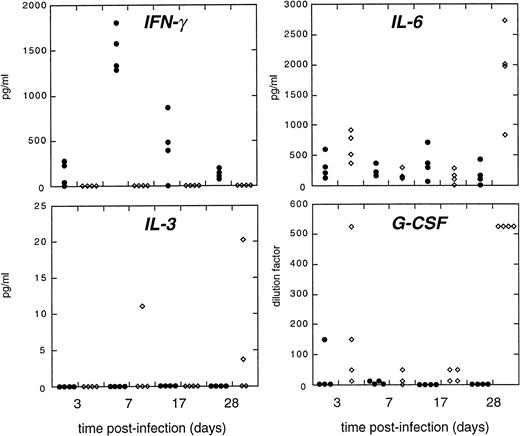
Cytokine levels in the plasma of infected mice. Cytokines were measured from plasma samples as described in Materials and Methods. Closed symbols: IFN-γ +/+ mice, open diamonds: IFN-γ −/− mice. Values are given in pg/mL except for G-CSF levels, which are given in the lowest dilution (see basis for this assay in Materials and Methods). Data representative of multipe experiments. We consistently detect IL-6, but IL-3 and GM-CSF levels are commonly at the background level of the ELISA assay.
Cytokine levels in the plasma of infected mice. Cytokines were measured from plasma samples as described in Materials and Methods. Closed symbols: IFN-γ +/+ mice, open diamonds: IFN-γ −/− mice. Values are given in pg/mL except for G-CSF levels, which are given in the lowest dilution (see basis for this assay in Materials and Methods). Data representative of multipe experiments. We consistently detect IL-6, but IL-3 and GM-CSF levels are commonly at the background level of the ELISA assay.
Antigen-specific T-cell responses.
Hematopoietic colony-forming potential.
CFUs from the bone marrow or spleen were assessed by plating cells (15,000 cells per mL) in complete methycellulose media (Stem Cell Technologies, Vancouver, Canada) containing IL-6, IL-3, erythropoietin (EPO), and stem cell factor. Colonies (greater than 30 to 50 cells) were scored 10 days after plating. Results are expressed as described in the text and figure legend to Fig 5.
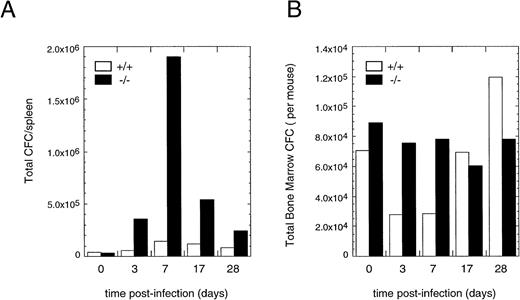
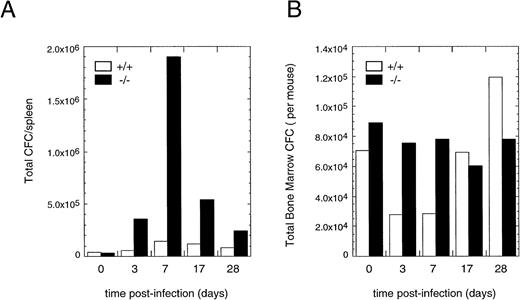
Progenitor numbers in the spleen of infected mice. (A) Spleen CFC counts were performed at different times after infection from wild-type (□) or IFN-γ −/− mice (▪). Results are reported as total CFCs per spleen. The “0” time point is from naive mice. (B) Total bone marrow CFC in wild-type (□) or IFN-γ −/− mice (▪) from the same experiment shown in (A). Results are reported as the total CFCs recovered in the leg bones of each mouse. Each time point is an average of four to six mice per group. Results were similar in three independent experiments.
Progenitor numbers in the spleen of infected mice. (A) Spleen CFC counts were performed at different times after infection from wild-type (□) or IFN-γ −/− mice (▪). Results are reported as total CFCs per spleen. The “0” time point is from naive mice. (B) Total bone marrow CFC in wild-type (□) or IFN-γ −/− mice (▪) from the same experiment shown in (A). Results are reported as the total CFCs recovered in the leg bones of each mouse. Each time point is an average of four to six mice per group. Results were similar in three independent experiments.
Bacterial CFUs.
Spleen preparations from infected mice were homogenized with a hand-held blender and serially-diluted in phosphate-buffered saline (PBS)-0.05% Tween-80. Homogenates were plated onto MH10 plates and colony numbers scored 21 to 28 days later.
RESULTS
General pathological features of infected mice.
Our initial impetus to use the IFN-γ −/− mice in experimental BCG infection was to test the hypothesis that BCG strains secreting biologically active cytokines16 at the site of infection could partially rescue the pathology in the mice and delay death. We performed several experiments using BCG strains secreting biologically active IL-2, GM-CSF, or IFN-γ, but none could avert the extreme pathology in the IFN-γ −/− animals (data not shown). In the absence of effective macrophage activation in IFN-γ–deficient mice, we anticipated observing a gradual necrosis of the spleen with a concomitant expansion of bacterial numbers leading to overwhelming infection and death, as was observed in M tuberculosis infection.1,3 As expected, IFN-γ −/− mice were susceptible to BCG infection,2most mice dying by 6 to 10 weeks postinfection. However, striking pathological changes were observed in the hematopoietic system.
BCG-infected IFN-γ −/− mice rapidly developed grossly enlarged spleens (average weight ≈ 0.7 to 1.0 g compared with wild-type mice average ≈ 0.15 g) that became progressively paler in color as infection proceeded (Fig 1A). Microscopic inspection of the spleen showed an effacement of the normal tissue architecture (Fig 1, compare B with C). In contrast to wild-type animals, IFN-γ −/− mice lacked the regular follicular arrangement of the red and white pulp. The normal lymphocytic populations of the white pulp of IFN-γ −/− mice were progressively replaced with sheets of leukocytes comprised predominantly of maturing elements of the myeloid lineage, macrophages, and neutrophils (Fig 1, compare D and F with E and G and see data presented below). The splenic red pulp was extensively replaced by extramedullary hematopoietic tissue (Fig 1H). After 4 to 5 weeks postinfection, the total number of lymphocytes recoverable from the spleen dropped to ≈ 5% of the control or naive uninfected IFN-γ −/− mice (data not shown), consistent with a replacement of the normal cell populations within the spleen. The hematopoietic alterations observed in the spleen prompted further investigation of the pathology of BCG infection in IFN-γ −/− mice.
BCG infection of IFN-γ −/− causes profound changes in the spleen. (A) Spleens isolated from infected IFN-γ +/+ (top two spleens) or IFN-γ −/− (bottom two spleens) mice 5 weeks after IP administration of BCG show the change in size and color of the organs. Low power view of spleens sections from IFN-γ +/+ (B) or IFN-γ −/− (C) mice. Note that the overall structure of the red and white pulp is intact in IFN-γ +/+ mice, but the normal architecture of infected IFN-γ −/− is completely effaced (photographed using a 10X objective). Higher power views of the spleen show that the white pulp of infected IFN-γ −/− mice is extensively infiltrated by macrophages (E and G), while infected IFN-γ +/+ mice retain the normal arrangement and cellular makeup of the white pulp (D and F). Note that in (E), a small area of lymphocytes remains in the right-hand portion of the white pulp. Lymphocytes gradually disappeared from the spleen. Magnifications: (D) and (E) (20X objective); (F) and (G) (40X objective). The red pulp of infected IFN-γ −/− mice was infiltrated with extramedullary hematopoietic tissue (H). Note the presence of nucleated erythroid cells, cells of the granulocytic series, and megakaryocytes (40X objective). All sections were stained with hematoxylin and eosin (H&E).
BCG infection of IFN-γ −/− causes profound changes in the spleen. (A) Spleens isolated from infected IFN-γ +/+ (top two spleens) or IFN-γ −/− (bottom two spleens) mice 5 weeks after IP administration of BCG show the change in size and color of the organs. Low power view of spleens sections from IFN-γ +/+ (B) or IFN-γ −/− (C) mice. Note that the overall structure of the red and white pulp is intact in IFN-γ +/+ mice, but the normal architecture of infected IFN-γ −/− is completely effaced (photographed using a 10X objective). Higher power views of the spleen show that the white pulp of infected IFN-γ −/− mice is extensively infiltrated by macrophages (E and G), while infected IFN-γ +/+ mice retain the normal arrangement and cellular makeup of the white pulp (D and F). Note that in (E), a small area of lymphocytes remains in the right-hand portion of the white pulp. Lymphocytes gradually disappeared from the spleen. Magnifications: (D) and (E) (20X objective); (F) and (G) (40X objective). The red pulp of infected IFN-γ −/− mice was infiltrated with extramedullary hematopoietic tissue (H). Note the presence of nucleated erythroid cells, cells of the granulocytic series, and megakaryocytes (40X objective). All sections were stained with hematoxylin and eosin (H&E).
Granulocytosis in the blood and spleen.
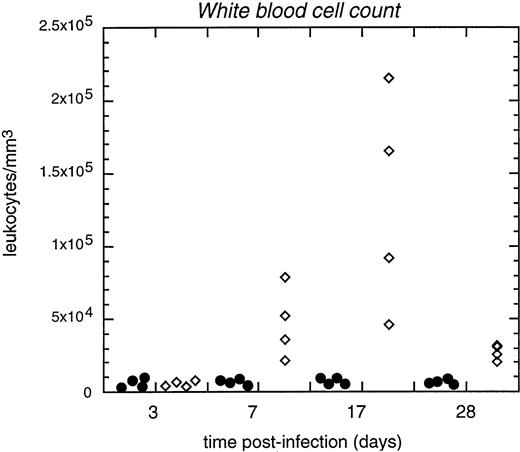
The blood of infected IFN-γ −/− mice reflected a marked leukocytosis, in extreme cases characterized by WBC counts greater than 80,000 cells/μL (Fig 2). The leukocytosis was most pronounced between days 7 and 17 postinfection (Fig 2). Microscopic examination of the blood showed that a large expansion of granulocytes and monocytes had occurred (Fig 3A). Differential WBC counts documented granulocytosis and an increase in monocytes (Table 1).
Expansion of blood leukocytes in infected IFN-γ −/− mice. Leukocyte counts (in cells per μL) were measured at different times after infection (abcissa). Closed symbols are IFN-γ +/+ mice, open diamonds are IFN-γ −/− mice. Results are typical of numerous experiments and are further documented in Tables 1 and 2 and Fig 4.
Expansion of blood leukocytes in infected IFN-γ −/− mice. Leukocyte counts (in cells per μL) were measured at different times after infection (abcissa). Closed symbols are IFN-γ +/+ mice, open diamonds are IFN-γ −/− mice. Results are typical of numerous experiments and are further documented in Tables 1 and 2 and Fig 4.
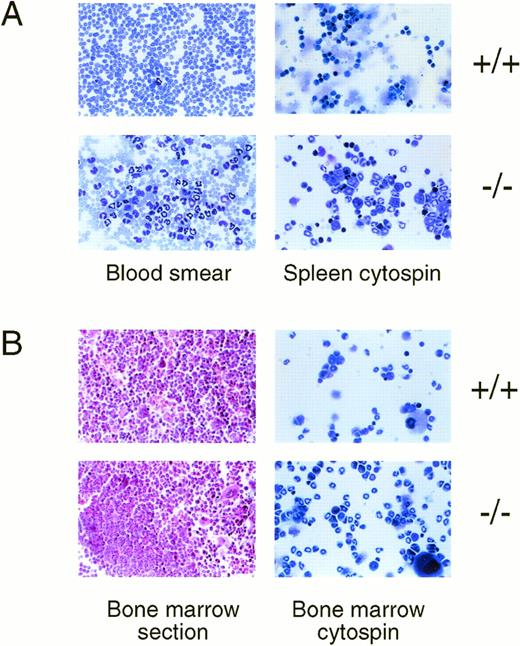
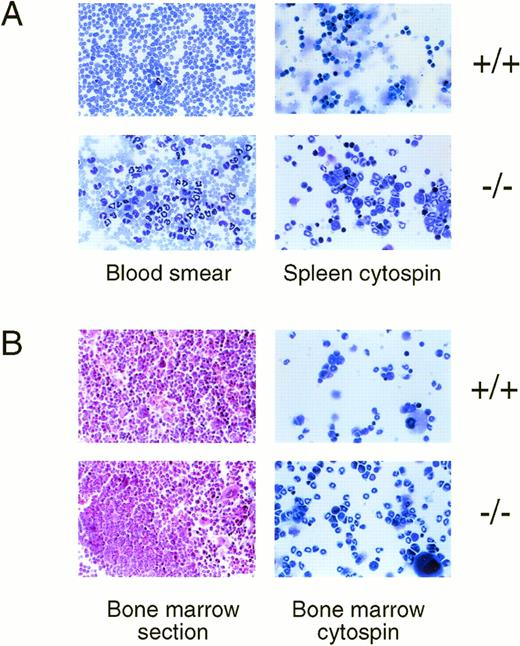
Neutrophilia in the blood, spleen, and bone marrow of infected IFN-γ −/− mice. (A) Peripheral blood (left panels) or spleen cytospins (right panels) from infected IFN-γ +/+ or IFN-γ −/− mice (indicated at right) were stained with leukostat. Note that in the peripheral blood of IFN-γ −/− mice there are large numbers of mature neutrophils as well as less mature band forms and numerous monocytes in this smear (WBC of this mouse was 1.5 × 105/mL). The spleen of IFN-γ −/− also shows cells predominantly of the granulocyte series of various stages of maturity. All figures were photographed through a 40X objective). (B) Bone marrow sections (left panels) or bone marrow cytospins (right panels) from infected IFN-γ +/+ or IFN-γ −/− mice (indicated at right) were stained with H&E (sections) or leukostat (cytospins). The bone marrow of infected IFN-γ +/+ mice displays normal cellularity and populations of the various cell types. The marrow of IFN-γ −/− mice has large foci of granulocyte development and the cell types are largely band forms. Sections were photographed with a 20X objective and cytospins with a 40X objective.
Neutrophilia in the blood, spleen, and bone marrow of infected IFN-γ −/− mice. (A) Peripheral blood (left panels) or spleen cytospins (right panels) from infected IFN-γ +/+ or IFN-γ −/− mice (indicated at right) were stained with leukostat. Note that in the peripheral blood of IFN-γ −/− mice there are large numbers of mature neutrophils as well as less mature band forms and numerous monocytes in this smear (WBC of this mouse was 1.5 × 105/mL). The spleen of IFN-γ −/− also shows cells predominantly of the granulocyte series of various stages of maturity. All figures were photographed through a 40X objective). (B) Bone marrow sections (left panels) or bone marrow cytospins (right panels) from infected IFN-γ +/+ or IFN-γ −/− mice (indicated at right) were stained with H&E (sections) or leukostat (cytospins). The bone marrow of infected IFN-γ +/+ mice displays normal cellularity and populations of the various cell types. The marrow of IFN-γ −/− mice has large foci of granulocyte development and the cell types are largely band forms. Sections were photographed with a 20X objective and cytospins with a 40X objective.
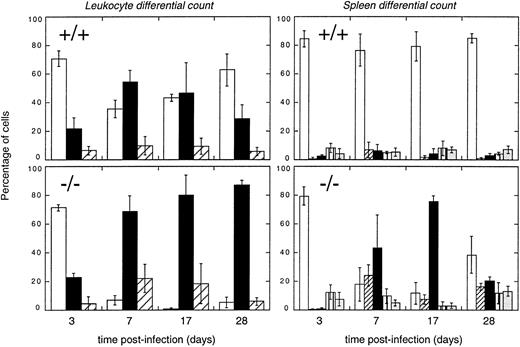
Examination of the cell types within the spleen (Fig 3B) confirmed that replacement of the normal lymphoid population with extramedullary hematopoietic elements had occurred. Enumeration of the cells types recovered showed a relative expansion of progenitor and maturing elements of the granulocytic and monocyte-macrophage lineages (Table 2). Kinetically, granulocyte numbers increased 7 days postinfection and remained high in the blood until morbidity (Fig 4, left panels). In the spleen, mature and immature granulocyte numbers also increased early in infection (Fig 4, right panels) and declined as morbidity was established.
Differential leukocyte analysis of blood and spleen populations measured over time in infected animals. Cell counts were made on blood (left-hand panels) or spleen (right-hand panels) leukocytes from the time course experiment (see Fig 3). Cells from +/+ mice are shown in the top panels, while −/− cells are in the bottom panels. Time after infection is shown in the abscissa. Blood differential counts: open bars, lymphocytes; closed bars, neutrophils and band forms (note that few band forms were observed in +/+ mice while the number was high in −/− mice); striped bars, monocytes. Spleen differential counts: open bars, lymphocytes; diagonally striped bars, blast forms; closed bars, band forms; vertically striped bars, mature (fully segmented nucleus) neutrophils; grey bars, monocytes and macrophages. Eosinophils, which comprised only a minor fraction of cells in the spleen, and erythroid series cells, which were detected in comparable numbers, are not depicted.
Differential leukocyte analysis of blood and spleen populations measured over time in infected animals. Cell counts were made on blood (left-hand panels) or spleen (right-hand panels) leukocytes from the time course experiment (see Fig 3). Cells from +/+ mice are shown in the top panels, while −/− cells are in the bottom panels. Time after infection is shown in the abscissa. Blood differential counts: open bars, lymphocytes; closed bars, neutrophils and band forms (note that few band forms were observed in +/+ mice while the number was high in −/− mice); striped bars, monocytes. Spleen differential counts: open bars, lymphocytes; diagonally striped bars, blast forms; closed bars, band forms; vertically striped bars, mature (fully segmented nucleus) neutrophils; grey bars, monocytes and macrophages. Eosinophils, which comprised only a minor fraction of cells in the spleen, and erythroid series cells, which were detected in comparable numbers, are not depicted.
Granulocytosis in the bone marrow.
The bone marrow of infected IFN-γ −/− mice developed a spectacular expansion of granulocytic precursors (mainly band forms, Fig 3B, “−/− bone marrow cytospin”), but the total nucleated cell numbers recovered from the bone marrow at various times after infection remained similar. The increased myeloid to erythroid ratio was confirmed by differential counting (Table 3). Interestingly, there was no apparent anemia in the infected animals, suggesting that the increased erythropoiesis in the spleen had effectively compensated for any reduction in bone marrow production. Although spleen erythroid numbers did not increase in proportion, there was an absolute 10-fold to 15-fold increase in erythroid precursor mass due to splenomegaly (data not shown).
Expansion of precursor cells on the spleen and bone marrow.
The shift towards myelopoiesis observed in the bone marrow and spleen of infected IFN-γ −/− mice suggested that there would be an increase in progenitor frequency in both of these organs. To address this, total myeloid colony forming activity was measured. Relative to wild-type infected animals, spleen CFCs increased significantly in IFN-γ −/− mice, verifying the large expansion of hematopoietic progenitors in the spleen following BCG infection (Fig 5A). The increase, as great as two orders of magnitude, was detectable 3 days after infection and remained high until morbidity. Analysis of the bone marrow showed that wild-type animals mounted a distinct hematopoietic response to infection. Wild-type mice manifested an initial decrease in myeloid progenitor frequency, perhaps reflecting a mobilization of inflammatory cells, but subsequently augmented bone marrow cellularity and myeloid progenitor numbers during the course of infection. In contrast, total nucleated cells remained relatively constant, as did CFC activity in the bone marrow of IFN-γ −/− mice (Fig 5B). Thus, the cellular response in the spleen and bone marrow differed dramatically between wild-type and IFN-γ −/− animals, with IFN-γ −/− mice mobilizing a pathologic extramedullary myeloid response. At baseline in uninfected animals, spleen and marrow CFC numbers were comparable in wild-type or IFN-γ −/− mice, demonstrating that the dramatic hematopoietic remodeling occurred in response to mycobacterial infection.
Bacterial numbers.
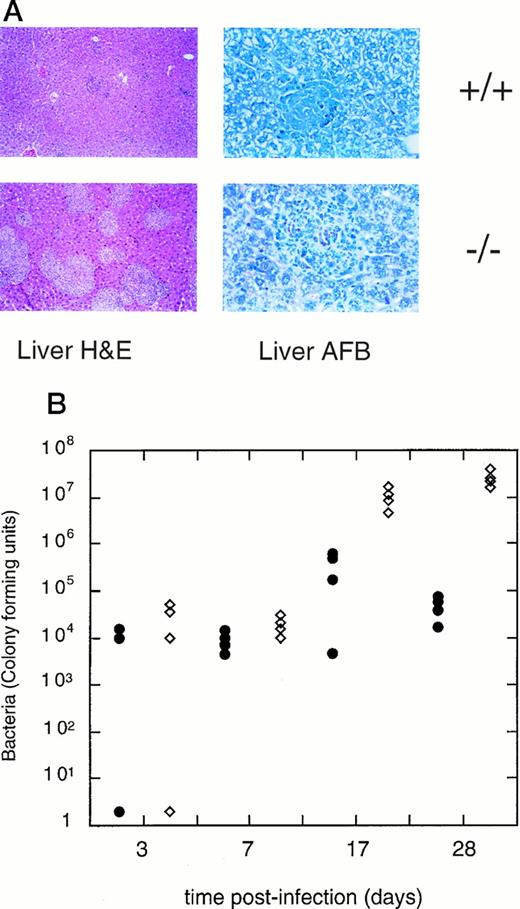
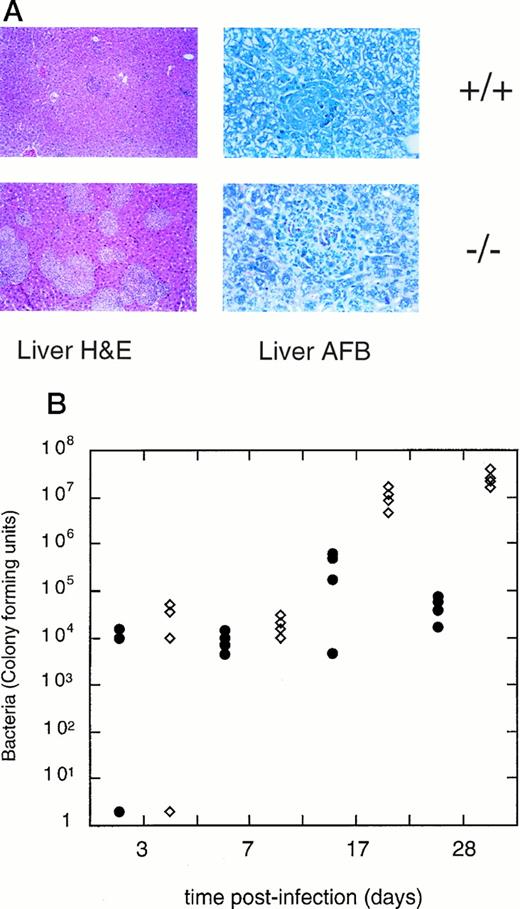
The organs that carry the greatest burden of mycobacteria following IP injection, the liver and spleen,1,2,16 19 were analyzed for bacterial numbers by plating tissue homogenates onto agar selective for mycobacteria, as well as examing acid-fast-stained organ sections. As shown in one example (Fig 6), bacterial numbers in the spleen (after an IP injection of 1 × 106 CFUs BCG) increased in both +/+ and −/− mice and were comparable at early time points (days 3 and 7; Fig 6B). In wild-type animals, bacterial numbers peaked at 17 days and declined thereafter, but in IFN-γ −/− mice, the bacterial load increased throughout the course of infection. Microscopic examination of Ziehl-Neelson-stained sections of the spleen and liver showed comparable numbers of acid-fast bacteria in wild-type and IFN-γ–deficient mice at early time points. Later in infection, numerous granulomatous lesions were observed in the livers of infected IFN-γ −/− mice and were associated with florid bacterial growth and necrosis in both liver and spleen (Fig 6). The expansion of splenic myeloid progenitors and blood neutrophils in IFN-γ −/− mice is observed as early as day 7 postinjection, before expansion of bacterial numbers in the spleen and liver, and occurs when mycobacterial numbers are comparable in IFN-γ −/− and wild-type animals, suggesting that the pathologic myeloid response in IFN-γ −/− animals is a consequence of IFN-γ deficiency rather than elevated mycobacterial burden.
Bacterial loads in infected mice. (A) Histopathology in the liver. Low power (20X objective) views of the liver of infected IFN-γ +/+ (top) or IFN-γ −/− (bottom) mice show that numerous granulomatous lesions form in the liver of IFN-γ −/− mice, while IFN-γ +/+ mice have few granulomas. Granulomas in IFN-γ +/+ mice contained no acid-fast bacteria (right-hand panel) at the time assayed (5 weeks postinfection), while IFN-γ −/− mice contained numerous bacteria (red rods within the granuloma structure). At the stage shown, 100% of granulomas contained acid-fast bacteria (data not shown) (B) Quantitation of bacterial numbers in the spleen. Closed symbols: IFN-γ +/+ mice, open diamonds: IFN-γ −/− mice. Time after infection is shown in the abscissa. Dilutions of spleen homogenates were plated onto MH9 media and bacterial colonies measured 21 to 28 days later.
Bacterial loads in infected mice. (A) Histopathology in the liver. Low power (20X objective) views of the liver of infected IFN-γ +/+ (top) or IFN-γ −/− (bottom) mice show that numerous granulomatous lesions form in the liver of IFN-γ −/− mice, while IFN-γ +/+ mice have few granulomas. Granulomas in IFN-γ +/+ mice contained no acid-fast bacteria (right-hand panel) at the time assayed (5 weeks postinfection), while IFN-γ −/− mice contained numerous bacteria (red rods within the granuloma structure). At the stage shown, 100% of granulomas contained acid-fast bacteria (data not shown) (B) Quantitation of bacterial numbers in the spleen. Closed symbols: IFN-γ +/+ mice, open diamonds: IFN-γ −/− mice. Time after infection is shown in the abscissa. Dilutions of spleen homogenates were plated onto MH9 media and bacterial colonies measured 21 to 28 days later.
Levels of cytokines in the peripheral blood.
To investigate the possible mechanisms of the pathologic changes in the BCG-infected IFN-γ −/− mice, we analyzed plasma levels of a series of cytokines. Levels of IL-6 were increased in infected −/− mice compared with wild-type mice, while other cytokines that may be relevant for hematopoietic expansion (such as IL-3 and GM-CSF) remained low. An example of such an analysis is depicted in Fig 7. Plasma from individual mice was examined at four time points after infection, and cytokine levels were analyzed by ELISA or bioassay. Results are shown for IFN-γ, IL-6, IL-3, and G-CSF. We did not detect GM-CSF, TNF-α, or IL-12 in the plasma, and levels of IL-10 were very low. The results show that in wild-type animals, IFN-γ levels increase, then fall systemically as the infection is controlled. In mice lacking IFN-γ, however, levels of IL-6 and G-CSF were generally higher at all time points examined, but increased dramatically when most mice were moribund (Fig 7). The systemic increase in IL-6 and G-CSF may contribute to the observed granulocytosis, but the greatest increase in these factors occurs well after the peak of myeloid activity detected in the blood and spleen.
Antigen-specific T-cell responses.
Because IFN-γ is essential for the development of a Th1 response to mycobacteria, we also tested if the expected shift to a Th2 phenotype had occurred in the infected IFN-γ −/− mice. When splenocytes were stimulated with PPD, readily detectable levels of Th2-associated cytokines such as IL-3, IL-4, and IL-5 were produced (Fig 8). These results confirm the findings of others using IFN-γ −/− mice and show that IFN-γ is essential for the development of a Th1 response to BCG. In the absence of IFN-γ, T-cell activity is shifted to a Th2 phenotype.
In infected IFN-γ −/− mice, the T-cell response to BCG is profoundly shifted to the Th2 phenotype. Splenocytes from infected IFN-γ +/+ mice (left side of each panel) or IFN-γ −/− mice (right side of each panel) were stimulated in vitro with media alone (open bars) or PPD (filled bars). Cytokine levels were measured by ELISA after 72 hours stimulation and expressed in pg/mL. In the experiment shown, mice on the C57BL/6 background were used. Similar results were obtained using IFN-γ −/− on the Balb/c background.
In infected IFN-γ −/− mice, the T-cell response to BCG is profoundly shifted to the Th2 phenotype. Splenocytes from infected IFN-γ +/+ mice (left side of each panel) or IFN-γ −/− mice (right side of each panel) were stimulated in vitro with media alone (open bars) or PPD (filled bars). Cytokine levels were measured by ELISA after 72 hours stimulation and expressed in pg/mL. In the experiment shown, mice on the C57BL/6 background were used. Similar results were obtained using IFN-γ −/− on the Balb/c background.
DISCUSSION
Models systems where the normal regulation of cytokine levels is disrupted are valuable tools to understand hematopoiesis, and in particular, to probe the mechanisms of leukocyte differentiation and production. Bacterial, protozoan, and viral infection in these models can provide additional information about how the immune system component of hematopoiesis responds to invading microorganisms. In the absence of IFN-γ, BCG-infected mice profoundly remodeled their hematopoietic system to favor increased granulocyte production in the marrow and spleen. The model described here yielded unexpected results that further defines the critical role of IFN-γ in regulating both macrophage function and the adaptive response to infection.
Pathological consequences of BCG infection in IFN-γ–deficient mice.
We anticipated that experimental infection of IFN-γ −/− mice with BCG would expose the strain's faulty immunity. As expected, the mice became visibly moribund about 4 to 5 weeks after a standard IP administration of BCG and died several weeks later. However, in our attempts to purify splenic T cells to analyze the Th2 response, we were intrigued by the pathologic changes observed. Despite gross splenomegaly, T cells were virtually absent from the spleen 4 weeks after infection of IFN-γ −/− mice, and histologic examination showed effacement of normal red and white pulp. The red pulp contained numerous hematopoietic elements and superficially resembled bone marrow. The white pulp was tightly packed with macrophage-like cells and granulocytes, giving the spleen the pathologic appearance of a myeloproliferative disorder. Quantitation of the cell types in the spleen showed a diminution in the percentage and absolute numbers of lymphocytes and an expansion of granulocytic elements. The expansion of granulocyte numbers in the spleen was also reflected in an increased blood leukocyte count, comprised almost exclusively of neutrophils and band forms. The bone marrow also showed a large increase in the percentage of cells in the granulocytic series. The pathologic changes resembled a severe leukemoid reaction or a myeloproliferative disorder. This was in marked contrast to what was observed in infected wild-type animals; the leukocyte count remained steady at all times after infection, although the percentage of neutrophils increased during the transient phase of active infection (see Fig 4). On successful resolution of infection, the relative percentage of neutrophils in the blood returned to normal. Cell populations in the spleen and marrow of wild-type mice remained steady in all experiments.
Examination of cytokine levels in the plasma showed that in infected wild-type mice, IFN-γ levels were easily detectable early in the infection (see for example Fig 7), presumably as a consequence of increased T-cell and macrophage activity. Increased IL-6 levels were recorded in most mice, but particularly late in IFN-γ −/− mice, suggesting that IL-6 may have played a role in driving the pathologic granulocytosis in IFN-γ −/− mice. In addition, G-CSF levels were greatly elevated in IFN-γ −/− mice, particularly towards death. Because G-CSF is essential for regulating neutrophil production18 (and see below), any increase in levels of this cytokine may be a significant factor in expansion of granulocytes in infected mice.
Our attempts to reverse the extreme phenotypes observed in IFN-γ–deficient mice by administration of a BCG strain secreting active IFN-γ failed, despite data that adequate levels of IFN-γ were produced by the mycobacteria to activate macrophages and induce IRF-1 and iNOS expression in vitro16 (and data not shown). Attempts by Flynn et al3 to reconstitute M. tuberculosis-infected IFN-γ–deficient mice with exogenous IFN-γ similarly failed to rescue lethality caused by infection. The context in which IFN-γ is used by the immune system appears essential in controlling mycobacterial infection.
Comparison to other models of disregulated hematopoiesis.
Some previously described murine models of perturbed hematopoiesis have exhibited hematopoietic parameters similar to those described here; namely increased spleen EMH, increased granulocyte production, and decreased cellularity in the bone marrow. Continuous administration of the IL-4–like Th2 cytokine IL-13 induces extra-medullary hematopoiesis (EMH) and splenomegaly with markedly elevated numbers of hematopoietic CFUs, a pathology mimicked by infection with Nippostrongylus brasiliensis, which induces a strong Th2 response.20 Mice lacking the IL-8 receptor show a deficiency in neutrophil migration and recruitment to sites of infection and consequently develop a compensatory neutrophilia and excessive EMH.21 Overexpression of cytokines including IL-6,22 G-CSF,23 and IL-524 has been shown to induce grossly elevated levels of neutrophils or eosinophils. Enhanced granulopoiesis due to genetic changes that increase the pool of progenitors has been documented in the max41 transgenic mouse25 and following retroviral transduction of the bcr-abl oncogene.26 The model described by Johnson et al27 in which bone marrow cells transduced with a GM-CSF–expressing retrovirus are allowed to repopulate a lethally-irradiated recipient has similar features to BCG-infected IFN-γ −/− mice. These mice develop a lethal myeloproliferative syndrome with progressive loss of cells in the bone marrow, enhanced neutrophil and monocyte/macrophage production, spleen hypercelluarity, and a possible decrease in lymphocyte numbers.
Does unregulated cytokine production play a role in the hematopoietic abnormalities observed in BCG-infected IFN-γ −/− mice? Our results show that IL-6 and G-CSF levels are indeed elevated in infected IFN-γ −/− mice. Interestingly, the highest levels were observed late in infection and did not correlate with the expansion of spleen progenitor numbers or blood leukocytes. Because our assays determine plasma cytokine levels and not local production in the marrow or spleen, our analysis of the role of cytokines is limited. Current studies are aimed at addressing the exact roles of these factors through a genetic approach by intercrossing mutant strains of mice to generate animals lacking both IFN-γ and IL-6 or IFN-γ and G-CSF. We will also need to determine if ectopic production of other cytokines such as GM-CSF or IL-3 play a role in the pathology. Because IFN-γ −/− mice have a strong Th2 response, T-cell production of IL-3 and GM-CSF is elevated (Fig 8 and P.J.M., unpublished observations). It would also be informative to test BCG infection in mice which lack IFN-γ and T cells by intercrossing IFN-γ −/− with RAG2 −/− or nu/numice. A similar strategy was used by Sharara et al28 to show that T cells drive EMH in mice laking the common γ chain of the receptors for IL-2, IL-4, IL-7, IL-9, and IL-15.
Comparison to other infection models of IFN-γ–deficient mice.
Pathogenesis in IFN-γ–deficient mice has been studied in several other well characterized models. M tuberculosis-infected IFN-γ −/− mice die rapidly with unchecked bacterial growth and caseous necrosis in the liver and other organs.1-3 These investigators described some granulocytic infiltration in the lungs, but other hematopoietic parameters were not noted. Toxoplasma gondii infection of IFN-γ −/− mice was particularly revealing.29 These mice fail to control the infection, but develop a robust IL-12 response. Significantly, the mice had granulomatous infiltration of the peritoneum (the site of innoculation) characterized by excess neutrophils and eosinophils. Examination of other hematopoietic parameters in T gondii-infected IFN-γ −/− mice may show similarities with the model described here. Finally,Leishmania infection of IFN-γ −/− mice has been described by several groups. L major is lethal to these mice, which develop a prominent Th2 response.30 In contrast,L donovani infection provided a contrary example of a parasite whose growth was initially unchecked, but surprisingly began to resolve 3 months after infection.31 Taylor and Murray31speculate that, in the absence of IFN-γ, IL-12 drives an anti-Leishmanial pathway that depends on TNF-α to activate macrophage effector function. Thus IFN-γ −/− mice have been useful in defining absolute requirements for IFN-γ action (eg, in all mycobacterial infection) as well as IFN-γ–independent effector functions. It will be interesting to determine if hematopoietic remodeling occurs in these other models.
Possible mechanisms of hematopoietic expansion in infected IFN-γ −/− mice.
A fascinating pathologic process is initiated in BCG-infected IFN-γ −/− mice that leads to a profound dysregulation of normal hematopoiesis. The lessons learned from this system help demonstrate the role of IFN-γ in normal immunity and expose compensatory mechanisms that arise under conditions of immune deficiency. There are several mechanisms that might account for the pathologic changes we observed in the IFN-γ–deficient mice. The most provocative hypothesis to arise from our observations is that IFN-γ normally plays a critical role in downregulation of the acute inflammatory response and modulation of the humoral (neutrophilic) and cellular (macrophage) arms of the immune response; loss of the negative regulatory function of IFN-γ itself predisposes to pathologic neutrophilia. This hypothesis is supported by observations on the activity of IFN-γ on hematopoietic colony assays in vitro and various clinical observations.
IFN-γ is a key activator of macrophage function, but it is also a potent suppressor of hematopoiesis. IFN-γ has been shown to have potent inhibitory effects on a diversity of myeloid and lymphoid progenitors and long-term culture initiating cells (LTC-IC) when expressed in stromal cells in long-term bone marrow cultures32 or in transgenic mice.33 IFN-γ binds directly to receptors on erythroid precursors and suppresses erythroid colony formation in vitro.34 IFN-γ appears to be a central effector of aplastic anemia,35 the anemia of chronic disease,36 and acquired immunodeficiency syndrome (AIDS)-related cytopenias.37,38 IFN-γ inhibits the neutrophil-stimulating activity of IL-8 and ENA-7839; the absence of IFN-γ function may thus lead to unopposed neutrophil activation. The precise role of IFN-γ in hematopoietic regulation is complex, as some in vitro data argue that IFN-γ may promote modest expansion of the earliest CD34+ hematopoietic precursors40,41and may stimulate platelet production by effects on megakaryocytes.42 Other work on the direct effects of IFN-γ on single cell colony assays of CD34+bone marrow progenitors show that IFN-γ stimulates monocytic colonies and inhibits granulocytic colonies, effects that are antagonized by the Th2 cytokine IL-4.43
Genetically deficient strains of mice provide insights that complement the in vitro data on the role of interferons in hematopoiesis. Mice deficient in the type I interferon receptor and the interferon response genes IRF-2 and ICSBP manifest hematopoietic abnormalities and immunodeficiency.44-46 Indeed, a myeloproliferative disorder that resembles human chronic myeloid leukemia arises in ICSBP-deficient mice.45 In the IFN-γ −/− mice subjected to mycobacterial challenge as described in this report, the loss of the negative regulatory role of IFN-γ leads to pathologic neutrophilia. Because the mice succumb to mycobacterial infection, we are unable to determine whether a prolonged period of dysregulated myeloid hyperplasia predisposes to acute leukemia, as occurs in the ICSBP−/− strain. Naive IFN-γ −/− mice have normal blood leukocyte counts and normal bone marrow and spleen progenitor numbers. Thus, it appears that IFN-γ plays a role in regulation of hematopoiesis only under conditions of stress. When hematopoiesis is challenged by infection, the absence of IFN-γ tilts the inflammatory response towards neutrophilic predominance.
ACKNOWLEDGMENT
We thank Chuck Dangler and Abul Abbas for advice and interest in the pathology of the IFN-γ–deficient mice, Doug Hilton for the gift of reagents to assay G-CSF levels, Vic Myer for help with photography of organs, and Heidi LeBlanc and Brenda Schulman for critical appraisal of the manuscript.
G.Q.D. is the recipient of a Career Award from the Burroughs-Wellcome Fund.
Address reprint requests to George Q. Daley, MD, PhD, Whitehead Institute for Biomedical Research, 9 Cambridge Center, Cambridge MA 02142.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.