Abstract
All-trans-retinoic acid (RA) treatment induces morphological remission in acute promyelocytic leukemia (APL) patients carrying the t(15;17) and expressing the PML/RARα product by inducing terminal differentiation of the leukemic clone. RA treatment induces downregulation of PML/RARα and reorganization of the PML-nuclear bodies. These events have been proposed to be essential for the induction of APL cell differentiation by RA. Here, we show that in the APL-derived NB4 cell line as well as in myeloid precursor U937 cells expressing the PML/RARα (U937/PR9) and in blasts from APL patients, the PML/RARα fusion protein is cleaved by a caspase 3–like activity induced by RA treatment. In fact, a caspase 3–like activity is detectable in PML/RARα expressing cells after RA treatment, and selective caspase inhibitor peptides are able to prevent the RA-induced degradation of the fusion protein in vivo and in vitro. Using recombinant caspases and PML/RARα deletion mutants we mapped a caspase 3 cleavage site (Asp 522) within the α-helix region of the PML component of the fusion protein. The extent of PML/RARα cleavage directly correlates with the ability of RA to restore the normal PML nuclear bodies (NBs) pattern. However, RA-induced differentiation is not prevented by the persistence of the fusion product and occurs in the absence of normally structured PML NBs. These results indicate that PML/RARα is directly involved in conferring RA sensitivity of APL cells and that the RA-induced reassembly of PML NBs is the consequence of the disappearance of PML/RARα.
THE ACUTE PROMYELOCYTIC leukemia (APL) phenotype depends on the expression of the PML/RARα fusion product, which results from the recombination between the promyelocytic leukemia (PML) gene on chromosome 15 and the retinoic acid (RA) receptor α gene (RARα) on chromosome 17 (t15;17).1,2 PML, a member of the RING finger family, is ubiquitously expressed in tissues within large multiprotein nuclear structures, termed nuclear bodies (NBs), and acts as a growth suppressor in vitro.3-6 RARα is one of the nuclear retinoid receptors that mediates RA action on myeloid differentiation.7-10 PML/RARα retains large portions of the parental proteins, including the RING, B1-B2, and coiled-coil regions of PML and the DNA and ligand binding domains of RARα.1 2
The mechanism of the PML/RARα leukemogenic activity is poorly understood. PML/RARα expression into hematopoietic precursor cell lines induces differentiation block and promotes survival.11 Both phenotypes depend on the integrity and fusion of PML and RARα sequences.12 It has been proposed that PML/RARα exerts a dominant negative action on wild-type PML and RXR, an RARα cofactor, because expression of PML/RARα provokes PML and RXR delocalization.3-5 Indeed, in APL cells and in bone marrow cells from leukemic PML/RARα transgenic mice, the PML NBs are disrupted into a microspeckled pattern.3-5,13-15 Based on these findings it has been suggested that the integrity of PML NBs is important for normal myeloid differentiation and that PML/RARα may cause leukemia by interfering with either the RAR- or PML-dependent differentiation pathways.3-5 16
APL is a unique model for differentiation therapy, as indicated by the fact that RA induces terminal differentiation of PML/RARα-expressing cells both in vivo and in vitro.1,2,16,17 Treatment with RA induces downregulation of the fusion protein, disappearance of the PML/RARα microspeckles, reorganization of PML NBs pattern, and relocalization of PML to its physiological site, therefore suggesting that the main effect of RA in APL cells is to release the dominant negative effect of PML/RARα on wild-type PML.3-5,18,19However, expression of PML/RARα into different myeloid cell lines increases RA sensitivity and alterations of PML/RARα correlates with RA resistance in APL-derived NB4 cell lines.11 20-22 These findings would indicate that the fusion protein is actively involved in conferring RA sensitivity and that the integrity of the PML NBs plays no role.
Downregulation of PML/RARα by RA occurs at the posttranslational level18 and is prevented by proteasome inhibitors.19 Recent findings show that PML is associated with ubiquitin-related proteins,23,24 and a possible role for the proteasome pathway in the RA-induced degradation of PML/RARα has been suggested.19 The proteasome is also involved in cellular pathways leading to caspase activation and apoptosis.25,26 Caspases are a family of cysteine proteases with aspartic acid substrate specificity, thought to be key effectors of cellular apoptosis in multicellular organisms.27 28
Here, we show that caspases mediate the RA-induced degradation of PML/RARα. Using different caspase inhibitor peptides, we were able to prevent RA-induced PML/RARα degradation and test directly the contribution of PML/RARα degradation and PML NBs reorganization to RA response of APL cells.
MATERIALS AND METHODS
Chemicals, antibodies, and plasmids.
All-trans-retinoic acid was obtained from Sigma (Milano, Italy). z-Al-Ala-DL-Asp-fluorometylketone (zVAD), Ac-Asp-Glu-Val-aspartic acid aldehyde (DEVD), and Ac-Tyr-Val-Ala-Asp-chloromethylketone (YVAD) were obtained from Bachem, Switzerland. RARα antibody was obtained from Dr P. Chambon (Strasbourg, France)29 and from Santa Cruz Biotechnology (Santa Cruz, CA). PG-M3 and α-PML3 are anti-PML antibodies.12 30
PML/RARα and the mutants ΔC P/R, ΔH P/R, and HA-tagged PML/RARα were previously described.11,12 The pSG5/H4-RAR mutant was constructed by polymerase chain reaction (PCR) amplification and fusion of the PML heptad region with the RARα moiety of the PML/RARα fusion protein (F. Grignani and P.G. Pelicci, manuscript in preparation). MBP-PML/RARα construct was generated by PCR/subcloning in the pMal vector (New England Biolabs, Beverly, MA) and expressed in Escherichia coli B21 cells by induction with isopropyl-1-thio-β-D-galactopyranoside (IPTG) for 1 to 3 hours at 23°C. Poly(ADP-ribose) polymerase (PARP) cDNA31 was subcloned into a pBluescript vector (Stratagene, La Jolla, CA). [35S]-PARP, -PML/RARα, and -mutant proteins were prepared by in vitro transcription-translation using the TNT T7 coupled reticulocyte lysate system (Promega, Madison, WI). [35S]-methionine was purchased from Amersham (Arlington Heights, IL).
Cell culture and differentiation.
The human APL cell line NB4 was obtained from Dr M. Lanotte, INSERM, Paris, France32; the U937/PR9 and the U937/HA-PR1 are described subclones of the U937 promonocytic cell line.11,12 Leukemic cells from informed, newly diagnosed APL patients were isolated and cultured as previously described.33 Cells were maintained in RPMI 1640 medium supplemented with 10% fetal calf serum (FCS). Cell differentiation was evaluated as described.11 12
Immunofluorescence staining and immunoblot analysis.
Cells were collected, cytocentrifuged, and fixed in 100% methanol at room temperature for 5 minutes, followed by acetone for 2 minutes at −20°C. PML staining was performed with the PGM3 or with the anti-HA monoclonal antibodies as described.12 30 The immunofluorescence was detected using an Olympus BX-60 fluoromicroscope equipped with a chilled 3CCD digital color camera (C5810 Hamamatsu Photonics, Hamamatsu City, Japan).
In vitro cleavage assays.
Cells were collected by centrifugation and resuspended in 100 μL of a lysis buffer containing 50 mmol/L NaCl, 2 mmol/L MgCl2, 40 mmol/L β-glycerophosphate, 5 mmol/L EGTA, and 10 mmol/L HEPES pH 7.0. Cleavage reactions were performed in a volume of 36 μL containing 25 mmol/L HEPES, pH 7.5, 100 mmol/L NaCl, 2 mmol/L MgCl2, 5 mmol/L dithiotreitol, 0.1% Triton X, 1 mmol/L phenylmethylsulfonyl fluoride, and 2 μg/mL of each aprotinin, leupeptin, and pepstatin with 3 μL of [35S] methionine–labeled PARP and 15 μL of the cell lysates. Each reaction was incubated for 1 hour at 37°C. To map the PML/RARα caspase cleavage site, cell lysates were substituted with bacterially expressed GST or GST caspase1, or GST–caspase 3 fusion proteins.31 The reactions were fractionated on sodium dodecyl sulfate (SDS)-PAGE. The gels were fixed (acetic acid 60%, methanol 40%, and glycerol 5%), treated with the Amplify solution (Amersham), and dried. The cleavage products were visualized after an overnight exposure at −80°C or by immunoblotting as described above.
RESULTS
Inhibition of caspases prevents RA-induced PML/RARα degradation in vivo.
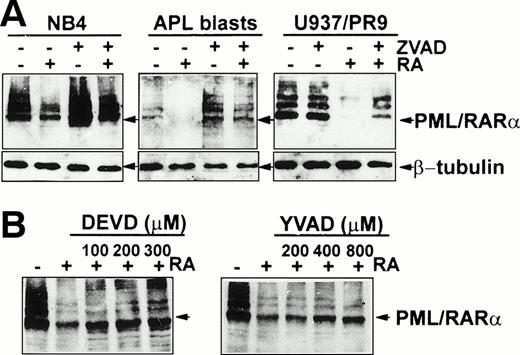
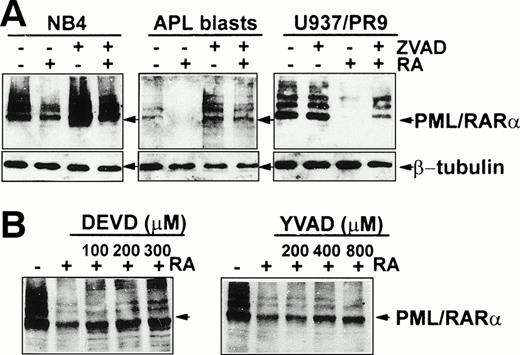
To investigate the involvement of caspases in the RA-induced degradation of PML/RARα, NB4 cells, fresh APL blasts, and the U937/PR9 cell line, a subclone of the promonocytic leukemia cell line U937 stably transfected with the PML/RARα cDNA under the control of a Zinc (Zn)-inducible promoter were treated with RA, in the presence or absence of the broad spectrum caspase inhibitor oligopeptide zVAD,34 and analyzed for PML/RARα expression by immunoblotting using the anti-RARα RPα(F) antibody.29 As shown in Fig 1A, RA-induced degradation of PML/RARα was inhibited by the addition of 100 μmol/L zVAD. Densitometric analysis of the Western blots shown in Fig 1A revealed that zVAD is able to inhibit about 40% to 50% of the RA-induced PML/RARα degradation in NB4 cells and in PML/RARα expressing U937/PR9 cells, whereas in APL blasts inhibition by zVAD is 87%. In addition, treatment of NB4 and APL blasts with zVAD in the absence of RA often resulted into increased levels of PML/RARα. This effect of zVAD was not detectable in PML/RARα expressing AML cells (U937/PR9 cells), suggesting that caspases are involved in the steady-state regulation of PML/RARα stability in APL cells.
Effect of the caspase inhibitors zVAD, DEVD, and YVAD in preventing RA-induced PML/RARα degradation. (A) Cells were treated with 1 μmol/L RA for 96 hours. U937/PR9 cells were induced to express PML/RARα by treatment with 100 μmol/L Zn for 16 hours. zVAD (100 μmol/L) was added for 1 hour before RA treatment. (B) Zn-induced U937/PR9 cells were treated with the indicated concentrations of DEVD or YVAD. Immunoblot analysis was performed on total cellular proteins (50 μg) using the anti-RARα RPα(F) antibody. Immunoreactivity to β-tubulin was used for loading control.
Effect of the caspase inhibitors zVAD, DEVD, and YVAD in preventing RA-induced PML/RARα degradation. (A) Cells were treated with 1 μmol/L RA for 96 hours. U937/PR9 cells were induced to express PML/RARα by treatment with 100 μmol/L Zn for 16 hours. zVAD (100 μmol/L) was added for 1 hour before RA treatment. (B) Zn-induced U937/PR9 cells were treated with the indicated concentrations of DEVD or YVAD. Immunoblot analysis was performed on total cellular proteins (50 μg) using the anti-RARα RPα(F) antibody. Immunoreactivity to β-tubulin was used for loading control.
Caspase inhibitors containing the peptide-recognition elements of endogenous substrates may reveal the involvement of specific classes of caspases.27 28 The tetrapeptide YVAD is a potent inhibitor of the caspase 1–like subfamily and a poor inhibitor of CED-3–like caspases. Conversely, the tetrapeptide DEVD effectively inhibits caspase 3–like activities. Increasing concentrations of YVAD or DEVD were added for 1 hour, before 1 μmol/L RA treatment for 20 hours. Degradation of PML/RARα was almost completely blocked by DEVD (60% to 80%), whereas YVAD was less effective (Fig 1B). Similar results were obtained in NB4 cells (not shown). These results suggested that a caspase 3–like protease is preferentially involved in the degradation of PML/RARα by RA in vivo.
RA induces caspase 3–like activity in NB4 cells.
To evaluate whether caspase 3–like activity was induced by RA treatment, we tested NB4 cellular lysates for their capacity to induce cleavage of the nuclear enzyme poly(ADP-ribose) polymerase (PARP), an endogenous substrate for caspase 3–like proteases.28Incubation of in vitro–translated PARP with cell lysates from untreated NB4 cells resulted in a partial PARP cleavage, as shown by the appearance of the 85-kD cleavage product (Fig 2, arrow). However, PARP cleavage was greatly enhanced by lysates from RA-treated NB4 cells (Fig 2A). In both cases, this cleavage was prevented by DEVD in vitro, the inhibitor peptide mimicking the PARP cleavage site (Fig 2A). These results indicate that caspase 3–like activity is endogenously present in NB4 cells and that it is further enhanced after RA treatment.
Cleavage of in vitro–translated PARP. [35S]-PARP was incubated for 1 hour at 37°C with cell lysates from untreated or from 1μmol/L RA-treated (A) NB4 and (B) U937/PR9 cells induced (+) or not (−) by 100 μmol/L Zn to express PML/RARα. One hundred micromoles per liter DEVD was added as indicated. Arrow indicates the 85-kD PARP cleavage product.
Cleavage of in vitro–translated PARP. [35S]-PARP was incubated for 1 hour at 37°C with cell lysates from untreated or from 1μmol/L RA-treated (A) NB4 and (B) U937/PR9 cells induced (+) or not (−) by 100 μmol/L Zn to express PML/RARα. One hundred micromoles per liter DEVD was added as indicated. Arrow indicates the 85-kD PARP cleavage product.
RA-induced caspase 3–like activity requires PML/RARα expression.
We investigated the role of PML/RARα on the induction of RA-dependent PARP cleavage activity using cell lysates from the U937/PR9 clone. In these cells treatment with 100 μmol/L Zn results in the expression of the PML/RARα protein.11 Cell extracts prepared from untreated U937/PR9 cells, or from cells treated with RA or Zn, failed to cleave in vitro–translated PARP. However, PARP cleavage was induced by lysates from U937/PR9 cells treated with Zn and RA. PARP cleavage was prevented by DEVD (Fig 2B). Simultaneous treatment of parental U937 cells with Zn and RA did not induce caspase 3 activity (not shown). Therefore, PML/RARα expression is required for the induction of caspase 3–like activity that follows RA treatment.
Mapping of a major caspase 3 cleavage site within the α-helix region of PML.
We then directly tested whether PML/RARα could be cleaved by caspase 3 in vitro. Incubation of in vitro–translated or bacterially expressed (MBP-PML/RARα; see Materials and Methods) PML/RARα with recombinant GST caspase 3 for 1 hour induced the formation of ∼50 kD proteolytic fragment (Fig 3B and C). This cleavage product was specifically induced by caspase 3 because it was blocked in vitro by DEVD and was not observed using GST or GST caspase 1 (Fig 3B and C and data not shown). Anti-RARα RPα(F) antibody specifically reacted with p50 (Fig 3B), thereby suggesting that GST caspase 3 induces a p50 proteolytic fragment that contains the C-terminal F region of RARα.
(A) Schematic representation of the amino acid sequences of PML/RARα and mutants. P, proline-rich region; R, RING finger domain; B1 and B2, B-boxes; C.C., coiled-coil region; α-H, α-helix region; SP, the α-helix serine and proline-rich region; BP, PML/RARα junction. (B through F) RARα functional regions. (B) MBP-PML/RARα (MBP-P/R) or (C) in vitro–translated [35S]-PML/RARα (P/R) or (D) [35S]-▵C P/R, (E) [35S]-▵H P/R, and (F) [35S]-H4-RAR were incubated with GST or GST caspase 3 for 1 hour at 37°C. One hundred micromoles per liter DEVD was added where indicated. Samples were analyzed by discontinous 8% to 15% SDS-PAGE and visualized by autoradiography or by immunoblotting (B) using an anti-RARα antibody (Santa Cruz Biotechnology). Molecular weight markers are indicated. Arrows indicate the p50 proteolytic fragment.
(A) Schematic representation of the amino acid sequences of PML/RARα and mutants. P, proline-rich region; R, RING finger domain; B1 and B2, B-boxes; C.C., coiled-coil region; α-H, α-helix region; SP, the α-helix serine and proline-rich region; BP, PML/RARα junction. (B through F) RARα functional regions. (B) MBP-PML/RARα (MBP-P/R) or (C) in vitro–translated [35S]-PML/RARα (P/R) or (D) [35S]-▵C P/R, (E) [35S]-▵H P/R, and (F) [35S]-H4-RAR were incubated with GST or GST caspase 3 for 1 hour at 37°C. One hundred micromoles per liter DEVD was added where indicated. Samples were analyzed by discontinous 8% to 15% SDS-PAGE and visualized by autoradiography or by immunoblotting (B) using an anti-RARα antibody (Santa Cruz Biotechnology). Molecular weight markers are indicated. Arrows indicate the p50 proteolytic fragment.
Because in vitro–translated RARα was not cleaved by GST caspase 3 or 1 (data not shown) and the RARα component of the fusion protein is ∼46 kD, the caspase 3 cleavage site was expected to map within the C-terminal portion of the PML component of PML/RARα fusion product. To directly show it, we tested the stability of various in vitro–translated PML/RARα deletion mutants (shown in Fig 3A) in the presence of GST caspase 3. ΔC P/R is a PML/RARα deletion mutant in which the N-terminal RING and B1+ B2 regions were deleted.12 In the ΔH P/R mutant, the coiled-coil region was deleted.12 The two regions deleted in ΔC P/R and ΔH P/R are adjacent in PML. Figure 3D and E shows that p50 is released following the incubation of GST caspase 3 with in vitro–translated ΔC P/R and ΔH P/R mutants, thereby suggesting that the caspase 3 cleavage site maps downstream to PML coil-coiled region, within the α-helix region. Notably, recombinant caspase 3 was not able to cleave the H4-RAR mutant obtained by fusing the PML heptad repeats directly to the RARα portion of PML/RARα (Fig 3F). Thus, a caspase 3 cleavage site maps within the α-helix region of PML retained in both ΔC P/R and ΔH P/R mutants but not in H4-RAR. This region contains only one aspartic acid (Asp) at position 522, within a sequence (PHLD:GP) permissive to caspases cleavage. The predicted molecular weight for the 434 amino acids proteolytic product (∼49.9 kD) is consistent with the observed p50 fragment and with Asp 522 being the cleaved residue.
Inhibition of PML/RARα degradation does not prevent RA-induced myeloid differentiation.
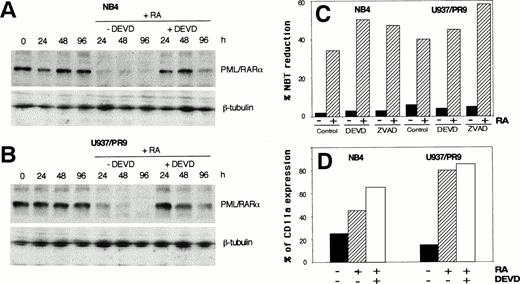
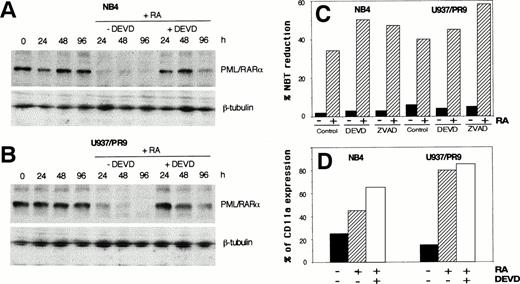
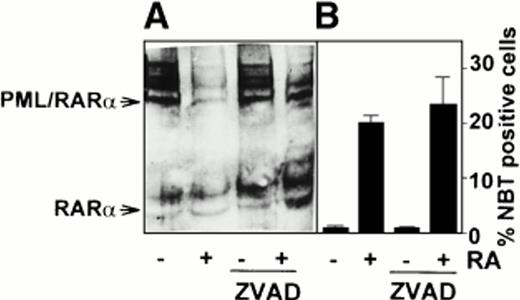
To investigate the role of PML/RARα degradation in RA-induced terminal differentiation, we took advantage of the possibility to prevent PML/RARα downregulation using caspase inhibitors. NB4 and Zn-induced U937/PR9 cells were pretreated with caspase inhibitors (DEVD or zVAD) or control medium for 1 hour before the addition of 1 μmol/L RA for 4 days. Immunoblot analysis revealed a marked effect of caspase inhibitor DEVD on the stability of PML/RARα in both NB4 (Fig 4A) and U937/PR9 (Fig 4B) cells. Treatment with RA and caspase inhibitors, either DEVD or zVAD, induced differentiation of both NB4 and Zn-induced U937/PR9 cells, as shown by the nitroblue tetrazolium (NBT) dye reduction test (Fig4C) and the quantitative fluorescence-activated cell sorter (FACS) analysis of the expression of the CD11a surface differentiation antigen (Fig 4D). In control experiments performed in the absence of RA, caspase inhibitors (DEVD or zVAD) had no effect on the differentiation properties of these cells (not shown). Comparison of differentiation in cells treated with RA or RA plus caspase inhibitors revealed a slight, but consistent, synergistic effect of caspase inhibitors (Fig 4C and D). Remarkably, similar results were obtained using leukemic blasts from peripheral blood of newly diagnosed APL patients (Fig 5).
Time-dependent inhibition of 1 μmol/L RA-induced PML/RARα degradation by 100 μmol/L DEVD in (A) NB4 cells and (B) Zn-induced U937/PR9 cells. Immunoblot analysis was performed on total cellular proteins using an anti-RARα antibody (Santa Cruz Biotechnology). β-tubulin antibody was used for loading control. (C and D) Effect of DEVD and zVAD on cell differentiation in cells grown in the absence (black bars) or in the presence of 1 μmol/L RA for 96 hours (diagonal bars) evaluated by NBT reduction test (C) or quantitative expression of CD11a antigen (D).
Time-dependent inhibition of 1 μmol/L RA-induced PML/RARα degradation by 100 μmol/L DEVD in (A) NB4 cells and (B) Zn-induced U937/PR9 cells. Immunoblot analysis was performed on total cellular proteins using an anti-RARα antibody (Santa Cruz Biotechnology). β-tubulin antibody was used for loading control. (C and D) Effect of DEVD and zVAD on cell differentiation in cells grown in the absence (black bars) or in the presence of 1 μmol/L RA for 96 hours (diagonal bars) evaluated by NBT reduction test (C) or quantitative expression of CD11a antigen (D).
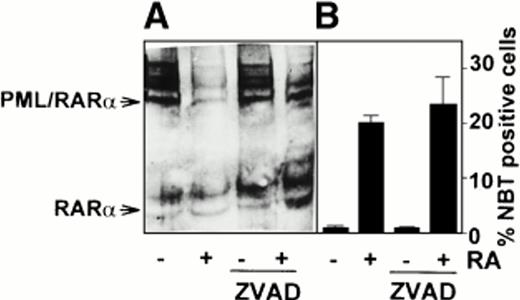
Leukemic cells isolated from a newly diagnosed APL patient were treated for 96 hours with either 1 μmol/L RA or 100 μmol/L zVAD or with the combination of both agents as indicated. (A) Immunoblot analysis performed using the anti-RARα RPα(F) antibody; (B) percentage of differentiated cells determined by NBT reduction assay.
Leukemic cells isolated from a newly diagnosed APL patient were treated for 96 hours with either 1 μmol/L RA or 100 μmol/L zVAD or with the combination of both agents as indicated. (A) Immunoblot analysis performed using the anti-RARα RPα(F) antibody; (B) percentage of differentiated cells determined by NBT reduction assay.
Inhibition of PML/RARα degradation by caspase inhibitors prevents reorganization of PML NBs.
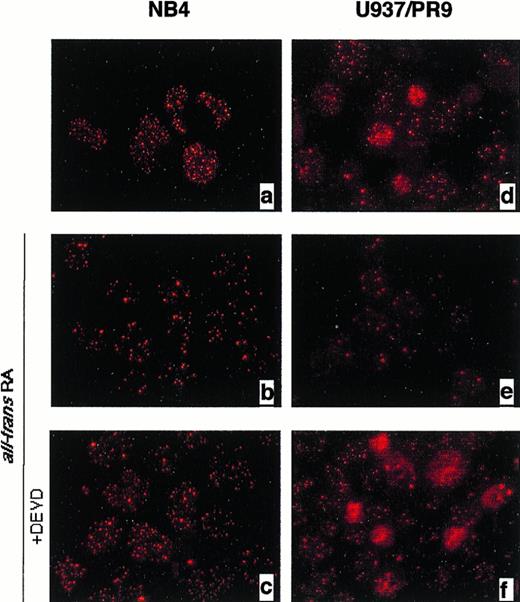
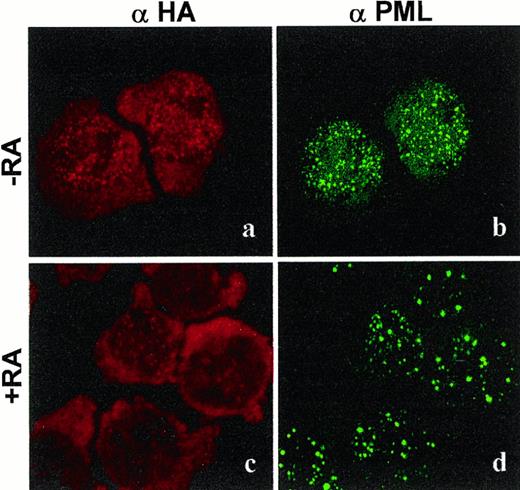
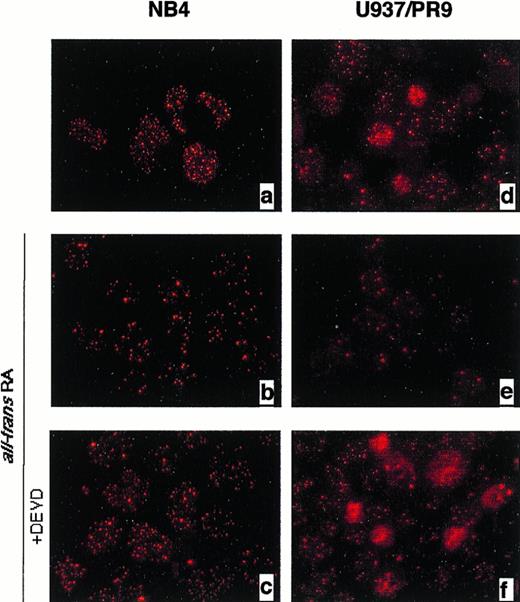
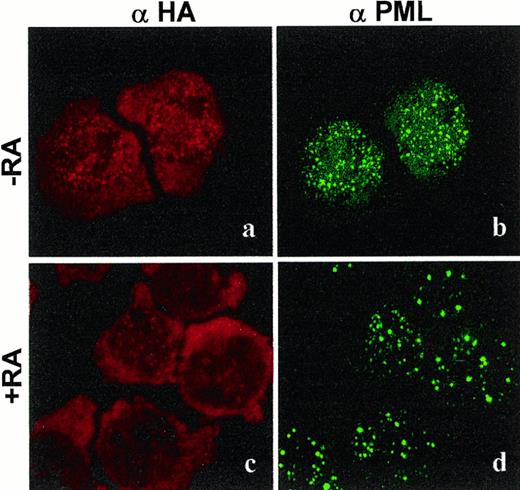
RA treatment of APL blasts induces progressive disappearance of PML/RARα microspeckles, reorganization of PML NBs, and in consequence, relocalization of PML to its physiological site. Whether these phenomena are involved in RA differentiation and the role of PML/RARα degradation is not clear. Therefore, we analyzed the effect of DEVD on the subcellular localization of PML and PML/RARα in NB4 and in U937/PR9 cells by indirect immunofluorescence using the PG-M3 anti-PML monoclonal antibody.30 NB4 and Zn-treated U937/PR9 cells showed the microspeckled pattern of PML and PML/RARα expression typical of APL cells (Fig 6a and d). RA treatment restored the speckled pattern of PML NBs in both cell lines (Fig 6b and e). However, this effect was blocked by caspase 3 inhibitor DEVD (Fig 6c and f). In fact, cells treated with both RA and DEVD revealed a microspeckled pattern of anti-PML staining (Fig 6c and f). It appears that inhibition of PML/RARα degradation prevents the reorganization of PML NBs. These results imply that PML/RARα localization is not sensitive to RA and that restructuring of the PML NBs induced by RA might be the consequence of the degradation of PML/RARα within the microspeckles, rather than its relocalization to PML NBs. To directly test this hypothesis, we analyzed the effects of RA treatment independently on the localization of PML and PML/RARα using an U937 clone expressing the HA-tagged PML/RARα protein (clone HA-PR1), where PML/RARα and the endogenous PML stainings can be recognized by double immunostaining using α-HA and α-PML3 antibodies, respectively. The anti-PML3 polyclonal antibody recognizes a carboxyterminal, isoform-specific PML3 epitope not retained within PML/RARα.12 Immunofluorescence analysis performed in untreated U937-HA-PR1 cells showed that both PML and PML/RARα are expressed into a microspeckled pattern (Fig7a and b). After RA treatment, the immunofluorescence analysis of HA-PML/RARα–expressing cells using the α-HA antibody revealed a progressive disappearance of the labeling (Fig 7c). Immunostaining of the same cells with the α-PML3 antibody demonstrated the simultaneous reformation of the PML NBs pattern (compare the microspeckled pattern of staining in control cells with the speckled pattern in RA-treated cells, Fig 7b and d, respectively). These data confirm that PML/RARα expression is downregulated by RA and indicate that RA-induced PML/RARα degradation takes place into the microspeckles and that there is minimal, if any, RA-induced PML/RARα relocalization to the PML NBs.
Immunofluorescence analysis in NB4 (a through c) and Zn-induced U937/PR9 cells (e through g) using the PG-M3 anti-PML monoclonal antibody. Control cells (a and d) and cells treated for 96 hours with 1 μmol/L RA (b and e) or 1 μmol/L RA + 100 μmol/L DEVD (c and f).
Immunofluorescence analysis in NB4 (a through c) and Zn-induced U937/PR9 cells (e through g) using the PG-M3 anti-PML monoclonal antibody. Control cells (a and d) and cells treated for 96 hours with 1 μmol/L RA (b and e) or 1 μmol/L RA + 100 μmol/L DEVD (c and f).
Immunofluorescence analysis in Zn-induced U937/HA-PR1 cells analyzed after 24 hours in the absence (a and b) or in the presence (c and d) of 1 μmol/L RA using the monoclonal anti-HA (a and c) or the polyclonal anti-PML3 antibodies (b and d).
Immunofluorescence analysis in Zn-induced U937/HA-PR1 cells analyzed after 24 hours in the absence (a and b) or in the presence (c and d) of 1 μmol/L RA using the monoclonal anti-HA (a and c) or the polyclonal anti-PML3 antibodies (b and d).
DISCUSSION
It has been recently proposed that the PML/RARα fusion protein is degraded through the proteasome during RA treatment of APL cells and that this event is required for the differentiative activity of RA.16,18,19 Recent studies show that a proteasomal pathway can be upstream to caspase activation in thymocytes and neurons induced by different stimuli,25 26 suggesting a possible linkage between these two pathways.
In this study, we have elucidated the molecular mechanism and the biological significance of PML/RARα degradation by RA. We first show that a member of the caspase 3 family is responsible for PML/RARα proteolysis during RA treatment of APL cells. In fact, RA-induced degradation of PML/RARα can be prevented in vivo with the broad spectrum caspase inhibitor zVAD and the caspase 3 selective inhibitor tetrapeptide DEVD. Degradation of the fusion protein can be reconstituted in a cell-free system by using in vitro–translated PML/RARα and recombinant caspases. One major caspase cleavage site maps within the PML component of the fusion protein (α-helix; Asp 522), and the proteolytic event leaves the RARα component intact and potentially able to mediate RA-dependent transcriptional events. Notably, Asp 522 is not retained in a shorter variant of PML/RARα (bcr3-PML/RARα isoform)1,2 found in approximately 35% of patients.35,36 This short PML/RARα isoform is indeed resistant to RA-induced degradation.37
The mechanisms involved in the triggering of caspase-mediated degradation of PML/RARα by RA treatment remain unclear. A caspase 3–like activity responsible for the proteolysis of PARP was detectable after treatment with RA in NB4 cells as well as in U937/PR9 cells induced to express PML/RARα. However, caspase activation also depends on PML/RARα expression, as shown by the finding that RA induces caspase activation in U937 cells only when the fusion protein is expressed. These findings are in agreement with recent data that shows that PARP polypeptide and its enzymatic activity decline dramatically during RA-induced differentiation in NB4 cells but not in HL-60 cells, a myeloblastic cell line that does not express PML/RARα.38 It appears, therefore, that the PML/RARα target protein is also required for RA-induced caspase activation in APL cells.
Caspase activation is a complex and still obscure process that is triggered by apoptotic signals.28,39 Bcl2 family members control the mitochondrial APAFs and the activation of caspase 3.28,39-41 Downregulation of Bcl2 by RA has been reported for some myeloid cells,42-44 and it is a constant and more pronounced phenomenon in PML/RARα-expressing cells.37,42,45 Therefore, Bcl2 might be a direct molecular target of PML/RARα, and its RA-induced downregulation might contribute to caspase activation and consequent PML/RARα degradation. Notably, RA-induced downregulation of Bcl2 and caspase activation is not followed by apoptotic cell death in APL cells,33 45-47thereby suggesting that additional molecular events are required to complete the apoptotic program.
Finally, these results show that APL cell differentiation might occur despite the persistence of PML/RARα expression. Oligopeptides that are selective caspase inhibitors could effectively prevent RA-induced PML/RARα degradation without impairing RA-induced differentiation in NB4 cells, in U937/PR9 cells, and in cells derived from APL patients, as evaluated by morphology, NBT reduction, and quantitative FACS analysis of the CD11a surface antigen expression. Indeed, in the presence of caspase inhibitors, we observed increased expression of the fusion protein and a parallel increased differentiative effect of RA, thereby suggesting an active contribution of PML/RARα to RA-induced differentiation. This is supported by the fact that RA induces cell differentiation and clinical remission also in APL patients expressing the short isoform of PML/RARα (bcr3),35,36 which appears to be resistant to RA-induced degradation.37
Inhibition of PML/RARα degradation largely maintained the microspeckled localization of the fusion protein preventing the reorganization of the PML NBs. Thus, in APL cells, RA-induced reassembly of NBs seems to be the consequence of the disappearance of PML/RARα within microspeckles and may not be required for myeloid differentiation. Taken together these data suggest that RA might convert PML/RARα to an active inducer of myeloid differentiation, possibly by triggering its trascriptional activator function on specific RA-target genes.
It has been recently shown that unligated nuclear receptors, including RARs, are associated with coregulatory proteins such as N-CoR and SMRT that can act as transcriptional corepressors. SMRT and N-CoR associate with the corepressor Sin3 and the histone deacetylase protein to form a transcriptional repressor complex.48,49 RA binding releases this complex and recruits the multisubunit activation complex, which possesses histone acetyltransferase activity.48 PML/RARα has been found to be associated with transcriptional corepressors that can dissociate from the fusion products at much higher RA concentrations than from wild-type RARα.50-54 In agreement with these findings, we propose that in APL cells, RA binding to PML/RARα induces allosteric changes of the fusion protein that release the corepressors and recruit the activator complex resulting in histone acetylation, modification of gene expression, and cell differentiation. The same allosteric changes in PML/RARα conformation might also allow specific PML/RARα amino acid sequences to be cleaved by caspases.
ACKNOWLEDGMENT
We gratefully acknowledge Wilson Miller, Giulio Cossu, and Angelika Rosenauer for helpful suggestions and discussions. We also thank P. Chambon, M. Lanotte, K. Schulze-Osthoff, R. Beyaert, and Sara Droetto for providing reagents.
Supported by grants from the Associazione Italiana per la Ricerca sul Cancro (AIRC), Ministero Università e Ricerca Scientifica e Tecnologica (MURST), CNR Biotechnology and European Community (Biomed).
Address reprint requests to Clara Nervi, MD, PhD, Dipartimento di Istologia ed Embriologia Medica, University of Rome “La Sapienza,” Via A. Scarpa 14, 00161 Rome, Italy; e-mail:nervi@axrma.uniroma1.it.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" is accordance with 18 U.S.C. section 1734 solely to indicate this fact.

![Fig. 2. Cleavage of in vitro–translated PARP. [35S]-PARP was incubated for 1 hour at 37°C with cell lysates from untreated or from 1μmol/L RA-treated (A) NB4 and (B) U937/PR9 cells induced (+) or not (−) by 100 μmol/L Zn to express PML/RARα. One hundred micromoles per liter DEVD was added as indicated. Arrow indicates the 85-kD PARP cleavage product.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/92/7/10.1182_blood.v92.7.2244/3/m_blod41942002w.jpeg?Expires=1766112505&Signature=HnGGfeKI~eS0mhLLJTG04gNAM~yq6yPGXGebF5kUfpSjsjLAZJjwyXGYZvjt8uUbWBN7ANHwsiCRTJDU0Yvi2oVZAGNrW20ouGjSL7uWYnbQKUyJpjuU-U45qgEPSYLK9QcD~9AokqiWFcssVIaEGKTDDsl85y~6nDdCHjPNObPyh9E-atdXCHZkuuVYwkaqJg273QccXVRSvPqY70smEbnvLW1-yhWLb0ZACSp4FbB6R~ogFk3Obe-SUDJN7EEpg-28jF9xdNyeCXdLCFQasZhGabecEGxopZy2093kTFRlGekupuCb2tUc5A3G9aMHJHxSHuUmRMoYcRHKCh-w9g__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 3. (A) Schematic representation of the amino acid sequences of PML/RARα and mutants. P, proline-rich region; R, RING finger domain; B1 and B2, B-boxes; C.C., coiled-coil region; α-H, α-helix region; SP, the α-helix serine and proline-rich region; BP, PML/RARα junction. (B through F) RARα functional regions. (B) MBP-PML/RARα (MBP-P/R) or (C) in vitro–translated [35S]-PML/RARα (P/R) or (D) [35S]-▵C P/R, (E) [35S]-▵H P/R, and (F) [35S]-H4-RAR were incubated with GST or GST caspase 3 for 1 hour at 37°C. One hundred micromoles per liter DEVD was added where indicated. Samples were analyzed by discontinous 8% to 15% SDS-PAGE and visualized by autoradiography or by immunoblotting (B) using an anti-RARα antibody (Santa Cruz Biotechnology). Molecular weight markers are indicated. Arrows indicate the p50 proteolytic fragment.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/92/7/10.1182_blood.v92.7.2244/3/m_blod41942003w.jpeg?Expires=1766112505&Signature=QEZ0X-r~nvbgUg2iMLC54WULzaIQb0aAg1An7JD2NUHarzO9O3BgHxyI46ISY-idcTeb6ZqZuDQ06LiLmy5QEIHhjD-8wp3cwI8EMK8ElM8ME-s6S0nqoSSEaBdj3qNv5CRj0G8Vk2BCQAjUkjVOSkVr6DLEu3DMOp0qEQjr77n5LEW~W5NXT14LpsQURWYJGZ2HySImaBQwHoRb2hrTfMH4ObqHaiD7eAy~Zz3Z7hNj9tVVwvuBSZzoALmTZTdIevCSNR~FTIJSZHRuu3wQR1pj7Cahaslxbacjfqm~4MMbMYZfb08xB-tcz9ZsfrcEn2Fes5zT3iaG9Tq84ZKJwA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)

![Fig. 2. Cleavage of in vitro–translated PARP. [35S]-PARP was incubated for 1 hour at 37°C with cell lysates from untreated or from 1μmol/L RA-treated (A) NB4 and (B) U937/PR9 cells induced (+) or not (−) by 100 μmol/L Zn to express PML/RARα. One hundred micromoles per liter DEVD was added as indicated. Arrow indicates the 85-kD PARP cleavage product.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/92/7/10.1182_blood.v92.7.2244/3/m_blod41942002w.jpeg?Expires=1766375127&Signature=suwKq2lhNSHe-sjaJSLZSRMeI4KwNdfgCS0Bxu6bGFHQy1Z3ciJ6dPROuDXX-rZdgI1QrGxp8KlaULkorE8plPq5Top1jEZLIx3euogf8Zc59ZHzhb4aAcYUHEWbzghf5Ba7JprBmL4iUtMloJVU2dlxKhqRann~65MVTIh7pkYMrqEiCsLWqm6Kr4iFoL6jvno5HVbfYqfd2L~r7495DRVDwOBXHFvyrAY9SSa1ukTYBjwhQg6o6oxDfAu8alye-ypFR9d5Gs0s9yedEbwvp8moAplUJAQGOFrssGS5DL3eaWbO~6hNSZg3RdWhJG5Sg4tUhyYm0BSX1xAlccrcSA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 3. (A) Schematic representation of the amino acid sequences of PML/RARα and mutants. P, proline-rich region; R, RING finger domain; B1 and B2, B-boxes; C.C., coiled-coil region; α-H, α-helix region; SP, the α-helix serine and proline-rich region; BP, PML/RARα junction. (B through F) RARα functional regions. (B) MBP-PML/RARα (MBP-P/R) or (C) in vitro–translated [35S]-PML/RARα (P/R) or (D) [35S]-▵C P/R, (E) [35S]-▵H P/R, and (F) [35S]-H4-RAR were incubated with GST or GST caspase 3 for 1 hour at 37°C. One hundred micromoles per liter DEVD was added where indicated. Samples were analyzed by discontinous 8% to 15% SDS-PAGE and visualized by autoradiography or by immunoblotting (B) using an anti-RARα antibody (Santa Cruz Biotechnology). Molecular weight markers are indicated. Arrows indicate the p50 proteolytic fragment.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/92/7/10.1182_blood.v92.7.2244/3/m_blod41942003w.jpeg?Expires=1766375127&Signature=xEYh4qqNDw8VKD2AXL811crBOFlrZM95Pkv8sjWOW5ZbyPen4qMRGFy3Nh6KbPd1U1se0I9-nHEqSooHk~6e3jQEa9lWx5HBfJBL~mXdb7jQdCUktOFBtx7iuIz2vWILyc4Ok3JEQKmzNudIJiEjGI0XYD5Nf8NtKVuA9G4mywyVfC7HIVCvqRnSewgEm~ps~skAavmVesX9vIJruvWZKo8g6Uf0Ql5GTWUTsE-ecZRLAQ5RQ0qGaVVbMtK-XEa1foJFi4i2asaQsgT3JUqnhGfZiyolQhQxnG~Une6d4KbSvN773H3dU-B~YKO4GCBNGmjo6EEdg~uVEby0D-Ri8g__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)