Abstract
We investigated whether interleukin-1β (IL-1β) is differentially expressed in plasma cells from monoclonal gammopathy of undetermined significance (MGUS) and multiple myeloma (MM) patients because IL-1β appears to play a major role in the development of lytic bone lesions, the major clinical feature distinguishing MGUS from myeloma. In situ hybridization (ISH) for IL-1β was performed using bone marrow aspirates from 51 MM, 7 smoldering MM, 21 MGUS, and 5 normal control samples. Using the ISH technique IL-1β mRNA was detectable in the plasma cells from 49 of 51 patients with active myeloma and 7 of 7 patients with smoldering myeloma. In contrast, 5 of 21 patients with MGUS and 0 of 5 normal controls had detectable IL-1β message. Bone lesions were present in 40 of the 51 MM patients analyzed, and all 40 patients had IL-1β mRNA by ISH. These results show that greater than 95% of MM patients but less than 25% of MGUS patients are positive for IL-1β production. In the future, continued follow-up of IL-1β positive and negative MGUS patients should determine whether aberrant expression of plasma cell IL-1β is predictive of those MGUS patients that will eventually progress to active myeloma.
MULTIPLE MYELOMA (MM) is a universally fatal B-cell malignancy accounting for 1% to 2% of all cancer deaths.1 MM is recognized clinically by the proliferation of malignant plasma cells in the bone marrow, the detection of a serum or urine monoclonal protein, anemia, hypercalcemia, renal insufficiency, and lytic bone lesions.2 Monoclonal gammopathy of undetermined significance (MGUS) is characterized by a monoclonal protein in the serum or urine without the other clinical features of MM. MGUS patients are asymptomatic and have stable M-protein measurements.3 MGUS is more common than myeloma occurring in 1% of the population over age 50 and 3% over age 70.4 It is of great clinical importance to distinguish patients with myeloma from individuals with MGUS because MGUS patients may be safely observed without chemotherapy.2 In long-term follow-up of 241 patients with MGUS, approximately 16% went on to develop MM.3
The molecular changes that result in the progression of MGUS to myeloma are currently unknown. However, a potential role for the acquired expression of various cytokines, oncogenes, and viruses has been implicated.5,6 Although interleukin-1β (IL-1β ) is not produced by normal plasma cells, several investigators have detected the production of IL-1β by myeloma marrow cells.7-11IL-1β is known to be a potent osteoclast activating factor and appears to play a major role in the development of lytic bone lesions,7,8,11 the major clinical feature distinguishing MGUS from myeloma.2 Torcia et al11 have shown a dose response between the level of IL-1β produced by marrow cells from patients with myeloma and osteoclast activating factor activity. IL-1β is also a potent inducer of other cytokines including IL-6, which is a major growth factor for myeloma cells.10 Based on these observations, IL-1β could be a central cytokine involved in the progression of MGUS to myeloma.
We recently showed, in a small number of patients, that IL-1β expression appears to be able to differentiate between patients with MGUS and MM using cell sorting to enrich for plasma cells followed by reverse transcriptase-polymerase chain reaction (RT-PCR).12Confirmation that the IL-1β–expressing cells were plasma cells was accomplished using an in situ hybridization (ISH) assay specific for IL-1β expression on bone marrow cells from a myeloma patient.12 Based on this earlier work, we have now investigated whether differences in IL-1β expression could be detected in monoclonal plasma cells from a large number of patients with either MGUS or myeloma using ISH. ISH has the advantage of simultaneous detection of cytokine expression and morphologic identification of the cytokine producing cell from unsorted cell populations. Our results show that IL-1β mRNA is undetectable in the plasma cells from the majority of patients with MGUS but is expressed by the plasma cells from virtually all patients with MM.
MATERIALS AND METHODS
Patients.
Bone marrow aspirates were obtained from 79 patients with plasma cell proliferative disorders consisting of 51 patients with MM, 7 patients with smoldering myeloma (SMM), 21 patients with MGUS, and 5 normal controls. Diagnoses were established using previously published criteria for MGUS, SMM, and MM.2 13 All samples used in this study were obtained from patients with informed consent according to Institutional Review Board Guidelines.
ISH for IL-1β.
ISH for IL-1β expression was performed as previously described.12 Briefly, paraformaldehyde fixed cells from Ficoll-Hypaque density gradient purified bone marrow aspirates were hybridized with a digoxigenin-11-dUTP–labeled (Boehringer Mannheim, Indianapolis, IN) antisense oligonucleotide probe specific for the human IL-1β gene. For each patient, a positive and negative control were run using commercially available fluorescein isothiocyanate (FITC)-labeled kappa and lambda probes (DAKO Corp, Carpinteria, CA). A blank slide without probe was run on each patient to control for nonspecific staining. An antiprobe antibody was added (anti-Digoxigenin-AP for the IL-1β and blanks; anti–FITC-AP for the kappa and lambda). The reactions were developed in NBT/BCIP. Hematoxylin was used as a nuclear counterstain. Slides were examined microscopically, and plasma cells were scored as positive or negative for IL-1β mRNA. Because MGUS specimens often contain a mixture of polyclonal and monoclonal plasma cells, a patient was considered to be positive for IL-1β expression by ISH if greater than or equal to 50% of the plasma cells were IL-1β positive. Each slide was scored independently by three different readers (M.Q.L., K.A.D., J.A.L.).
Flow cytometry and RT-PCR for IL-1β expression.
Flow cytometry and RT-PCR were performed as previously described.12 Briefly, 25 to 30 million mononuclear cells from bone marrow aspirates were stained with a FITC-conjugated monoclonal antibody to CD45 and a phycoerythrin (PE)-conjugated antibody against CD38 (Becton Dickinson, San Jose, CA). Using a FACStar Plus flow cytometer, debris and nucleated red blood cells were excluded by gating on the larger cells as defined by intermediate-to-high forward and negative-to-intermediate orthogonal light scatter. The CD38+/CD45− region was collected and contained greater than 95% plasma cells for all patients. This was confirmed morphologically.12 Subsequently, messenger RNA was isolated from 105 to 106 unsorted (U) and sorted (S) CD38+/CD45− cells.
Oligo-dT–purified mRNA was reverse transcribed using AMV reverse transcriptase (Amersham, Arlington Heights, IL). Subsequently, 1 μL of the first-strand cDNA template reaction was added to a standard PCR mix with oligonucleotide primers specific for the full-length cDNA of IL-1β (Clontech, Palo Alto, CA). Actin-specific primers were used as a control as previously described.12Fidelity of the amplified sequences was confirmed by fragment size comparison with a known control in all experiments and Southern blotting using an Applied Biosystems (Foster City, CA) Model 394 DNA-synthesized oligonucleotide probe (5′-AGACATCACCAAGCTTTTTTGCTGTGAGTC-3′) contained within the PCR fragments in selected cases.12 14 Reactions without DNA template were run with every experiment as a negative control (data not shown).
RESULTS
Contrast in IL-1β expression between patients with MGUS and MM.
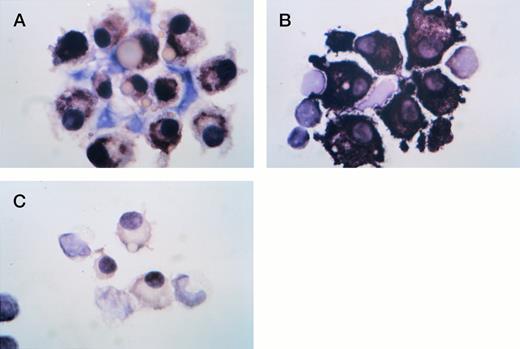
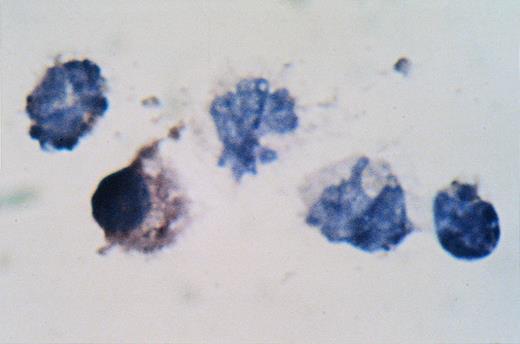
Results from several representative ISH assays are detailed in Figs 1 through3. Plasma cells from a patient with MM were positive for IL-1β and lambda expression as shown by the strong brown-black cytoplasmic staining (Fig 1A and B). The myeloma cells were negative for kappa expression (Fig 1C). All slides were counter-stained in hematoxylin. Plasma cells from a patient with MGUS were negative for lambda and IL-1β (Fig 2A and B) but positive for kappa expression (Fig 2C). In Fig 3, plasma cells from this MGUS patient were positive for IL-1β expression. The other leukocytes in the IL-1β panel are negative for IL-1β expression and serve as a useful control.
ISH for IL-1β in a patient with MM. (A) IL-1β; (B) lambda; (C) kappa. Plasma cells from a patient with MM were negative for kappa expression but positive for IL-1β and lambda expression as shown by the strong brown-black cytoplasmic staining. All slides were counter-stained in hematoxylin.
ISH for IL-1β in a patient with MM. (A) IL-1β; (B) lambda; (C) kappa. Plasma cells from a patient with MM were negative for kappa expression but positive for IL-1β and lambda expression as shown by the strong brown-black cytoplasmic staining. All slides were counter-stained in hematoxylin.
ISH for IL-1β in a patient with MGUS. (A) IL-1β; (B) lambda; (C) kappa. Plasma cells from this MGUS patient were positive for kappa expression and negative for lambda and IL-1β.
ISH for IL-1β in a patient with MGUS. (A) IL-1β; (B) lambda; (C) kappa. Plasma cells from this MGUS patient were positive for kappa expression and negative for lambda and IL-1β.
ISH for IL-1β in a patient with MGUS. Plasma cells from this MGUS patient were positive for IL-1β.
ISH for IL-1β in a patient with MGUS. Plasma cells from this MGUS patient were positive for IL-1β.
Using the ISH technique IL-1β mRNA was detectable in the plasma cells from 49 of 51 patients with active myeloma (Table 1). In contrast, only 5 of 21 patients with MGUS showed detectable IL-1β expression by ISH (P < .0001). None of the plasma cells from the 5 normal controls had detectable IL-1β mRNA. Interestingly, 7 of 7 patients with SMM had detectable IL-1β message (Table 1).
Bone lesions were present in 40 of the 51 MM patients analyzed, and all 40 patients with bone lesions had IL-1β mRNA detected in the monoclonal plasma cells by ISH (Table2). In addition, 9 of the 11 patients in whom bone lesions were undetectable on a metastatic bone survey were IL-1β positive. No patient with detectable bone lesions was found to be IL-1β negative.
Correlation of ISH and RT-PCR for IL-1β expression.
Fourteen of the patients had concurrent marrow aspirates sorted by flow cytometry using anti-CD38 and anti-CD45 antibodies. Messenger RNA was isolated from 105 to 106 unsorted (U) and sorted CD38+/CD45− (S) cells. Subsequently, RT-PCR with specific cytokine primers was performed to detect the presence of message for IL-1β and actin. In Fig 4, IL-1β mRNA was detectable in sorted CD38+/CD45− cells from a myeloma patient but not from a MGUS patient. Nine patients had detectable IL-1β mRNA in the plasma cells by both techniques including one patient with MGUS and eight with MM (Table3). Five patients had no detectable IL-1β mRNA in the plasma cells by either technique (Table 3). This group included four patients with MGUS and one patient with MM. All patients that were positive by ISH were also found to be positive by RT-PCR. Of note, all unsorted bone marrow populations contained IL-1β expressing cells by RT-PCR. Therefore, it is important to use a technique that allows for significant purification of the cells of interest (ie, flow cytometric sorting) or one that allows for visual identification of the IL-1β expressing cells (ie, ISH).
Cytokine detection by flow cytometry/RT-PCR. Marrow aspirates were sorted by flow cytometry using anti-CD38 and anti-CD45 antibodies. Messenger RNA was isolated from 105 to 106 unsorted (U) and sorted CD38+/CD45− (S) cells. Subsequently, RT-PCR with specific cytokine primers was performed to detect the presence of message for IL-1β and actin. IL-1β mRNA was detectable in sorted CD38+/CD45−cells from the myeloma patient but not from the MGUS patient.
Cytokine detection by flow cytometry/RT-PCR. Marrow aspirates were sorted by flow cytometry using anti-CD38 and anti-CD45 antibodies. Messenger RNA was isolated from 105 to 106 unsorted (U) and sorted CD38+/CD45− (S) cells. Subsequently, RT-PCR with specific cytokine primers was performed to detect the presence of message for IL-1β and actin. IL-1β mRNA was detectable in sorted CD38+/CD45−cells from the myeloma patient but not from the MGUS patient.
DISCUSSION
In a follow-up of 241 patients with MGUS, Kyle has shown that 16% of patients went on to develop multiple myeloma.3 Closer examination of those individuals who developed myeloma revealed that the majority of patients remained stable for an extended period of time and then subsequently progressed to overt myeloma over a relatively short period.3 Based on these clinical observations, it is likely that genetic differences exist between MGUS and myeloma in which subsequent mutations arise in the monoclonal plasma cells leading to active myeloma. These mutations could induce aberrant expression of cytokines that may play a role in the transition from MGUS to myeloma.5
In this regard, although the IL-1β gene is not expressed in normal plasma cells, we have shown that IL-1β mRNA is expressed by myeloma cells obtained from greater than 95% of MM patients. In contrast, plasma cell IL-1β mRNA expression was observed in less than 25% of MGUS patients. These results in myeloma patients are supported by several previous studies that have detected IL-1β at both the mRNA and protein levels.7-12 However, our studies on plasma cells from normal individuals and MGUS patients using ISH and flow cytometric sorting/RT-PCR are unique. Sixteen of 21 patients with MGUS failed to express detectable IL-1β message suggesting that plasma cell IL-1β expression may be useful to distinguish MGUS from MM. Furthermore, if the remaining five MGUS patients that were IL-1β positive develop myeloma in the future, then upregulation of plasma cell IL-1β production may be predictive of those MGUS patients that will eventually progress to active myeloma.
The development of osteolytic lesions is an important clinical finding that clearly distinguishes MGUS from myeloma,2 and IL-1β has potent osteoclast activating factor (OAF) activity.7,8 11 Forty of the 51 myeloma patients analyzed had osteolytic disease on a metastatic bone survey and were IL-1β positive. Nine of the remaining 11 myeloma patients and 7 of 7 smoldering myeloma patients with a negative bone survey were positive for IL-1β expression as well. These patients may exhibit osteolytic disease in the future. A subgroup of patients present with active myeloma in which bone lesions are absent at diagnosis but subsequently develop over time. For example, one of the SMM patients studied was found to be positive for IL-1β expression 2 years before bone lesions were detectable on his bone survey. A potential explanation may be that plasma cells from MM patients without bone lesions at diagnosis produce quantitatively less IL-1β when compared to myeloma patients with bone lesions at diagnosis. Alternatively, it may take several years between the time patients develop IL-1β producing monoclonal plasma cells and bone lesions that can be detected on a standard metastatic bone survey.
Torcia et al11 have shown a critical role for IL-1β in the pathogenesis of bone disease in myeloma by showing that the OAF activity of myeloma cells from patients is almost completely related to IL-1β. Using the fetal rat long-bone tissue culture assay, they showed that the OAF activity of culture supernatants from unfractionated bone marrow cells from myeloma patients correlated with the IL-1β content (r = .949). Furthermore, the OAF activity could be completely abolished by IL-1 receptor antagonist, soluble IL-1 receptor type I or II, or neutralizing anti–IL-1β antibodies but not anti–IL-6 antibodies.11 In a mouse model, Hawley and colleagues introduced an IL-1 cDNA into an IL-6–dependent murine B-cell line by retroviral-mediated gene transfer.15 After injection of these IL-1–producing B-cells into syngeneic mice, these cells were shown to “home” to the bone marrow and produce metastatic bone lesions. By comparison, intravenous injection of autonomously growing B-cell lines generated in vitro by retroviral insertion of an IL-6 cDNA rarely resulted in bone marrow or bone metastases.15 Subsequent work has shown that aberrant expression of IL-1 can alter adhesion molecules such as ICAM and CD44 on the surface of mouse plasmacytoma cells.16 A similar mechanism may occur in human myeloma in which aberrant expression of IL-1β induces increased expression of adhesion molecules such as VLA-4, CD44, CD54, CD56, and other surface molecules.17-21In addition, the localization of myeloma cells in the bone marrow is also dependent on their requirement for other cytokines such as IL-6 that are produced in the bone marrow microenvironment.
In summary, IL-1β has potent osteoclast activating factor activity, can increase the expression of adhesion molecules, and can induce paracrine IL-6 production (Fig 5). The increased production of adhesion molecules could explain why myeloma cells are found predominantly in the bone marrow. Subsequently, these “fixed” monoclonal plasma cells could now stimulate osteoclasts through the production of IL-1β and paracrine generation of IL-6 resulting in osteolytic disease (Fig 5).
The cause of acquired IL-1β expression in myeloma is unknown. However, the IL-1β gene is highly inducible and its expression can be affected by many microbial and cellular products.22Recently, a role for Kaposi’s sarcoma–associated herpesvirus (KSHV) in the pathogenesis of myeloma has been reported.6 Although it has not been shown for KSHV, Epstein-Barr virus (EBV), human immunodeficiency virus-1 (HIV-1), and respiratory syncytial virus (RSV) have been shown to upregulate IL-1 expression either by directly interacting with genomic sequences or indirectly by altering levels of transcription factors involved in IL-1β expression.23-25Of note, subsequent reports by other investigators have failed to confirm the presence of KSHV in myeloma specimens.26 If KSHV is involved in the pathogenesis of myeloma, it would not be unlikely that it could play a role either directly or indirectly in the aberrant expression of the IL-1β gene.
Our data show that the majority of patients with MGUS are negative for IL-1β expression but virtually all myeloma patients are positive for IL-1β production. In the future, continued follow-up of IL-1β positive and negative MGUS patients should determine whether aberrant expression of IL-1β by monoclonal plasma cells is a critical event in the transition of MGUS to myeloma. Because MGUS is relatively common in the general population and myeloma is incurable in virtually all cases, identification of those MGUS patients likely to progress to active myeloma will be important in the development of new therapeutic strategies. For example, prevention or delay of the transition from MGUS to myeloma with an effective chemopreventive agent27may have a major impact on the treatment of patients with monoclonal gammopathies.
Supported by Grant No. CA62242 from the National Institutes of Health and the Eastern Cooperative Oncology Group (ECOG).
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to John A. Lust, MD, PhD, Division of Hematology, Mayo Clinic, Rochester, MN 55905.