Abstract
The human immunodeficiency virus type 1 (HIV-1) long terminal repeat (LTR) introduced in association with the luciferase reporter gene into Jurkat T cells was strongly activated by a combination of human neutrophils and phorbol myristate acetate (PMA). Activation was not observed when normal neutrophils were replaced by neutrophils which lack a respiratory burst, ie, from a patient with chronic granulomatous disease (CGD), was strongly inhibited by catalase, was potentiated by vanadate, was stimulated by relatively low concentrations of azide, and was inhibited by selective inhibitors of protein kinase C (PKC). The PMA affected activation in three ways: (1) by directly activating the LTR in Jurkat LTRluc; (2) by inducing a respiratory burst in neutrophils with the formation of H2O2; and (3) by increasing the sensitivity of Jurkat LTRluc to the activating effect of H2O2. When PMA was replaced by opsonized zymosan as the neutrophil stimulus, activation of the LTR was low unless azide was added. Activation in the presence of azide was not seen when CGD neutrophils were used or when catalase was added, suggesting that azide acts by inhibiting the degradation of H2O2. These findings indicate that activation of the HIV-1 LTR in Jurkat T cells can be induced by H2O2 released by neutrophils, particularly when PKC is concomitantly activated.
PHAGOCYTES (neutrophils, eosinophils, monocytes/macrophages) respond to stimulation with a burst of oxygen consumption and much, if not all, of the extra oxygen consumed is converted initially to the superoxide anion and then to H2O2. Among the potent inducers of a respiratory burst in phagocytes is phorbol myristate acetate (PMA), which is a direct stimulus of protein kinase C (PKC), and opsonized zymosan, which acts as a phagocytic stimulus. Myeloperoxidase (MPO) (released from the cytoplasmic granules of neutrophils and monocytes) and eosinophil peroxidase (released from eosinophil granules) can react with the H2O2formed to oxidize a halide to form potent oxidants, which are toxic to ingested microorganisms and adjacent extracellular targets.
We have previously reported that neutrophils,1monocytes,2 and eosinophils,3 when appropriately stimulated, are viricidal to cell-free human immunodeficiency virus type 1 (HIV-1), and we have provided evidence for the involvement of the peroxidase-H2O2–halide antimicrobial system in this toxicity. Thus, the viricidal effect was inhibited by catalase, but not by heated catalase or superoxide dismutase (SOD) implicating H2O2 formed by the stimulus-induced respiratory burst. This conclusion was supported by the absence of a viricidal effect when neutrophils which lack a respiratory burst, ie, from patients with chronic granulomatous disease (CGD), were used, unless a source of H2O2 was added. Azide, a potent inhibitor of peroxidase, also was inhibitory, which is compatible with the involvement of the phagocyte peroxidase. This was supported by the finding that stimulated neutrophils and monocytes which lack MPO, ie, from patients with hereditary MPO deficiency, were not viricidal to HIV-1 unless MPO was added.
Biologic oxidants formed by phagocytes may also influence HIV-1 in other ways. The long terminal repeat (LTR) of HIV-1 contains promoter and enhancer sequences required for the initiation of gene transcription. H2O2 can activate the HIV-1 LTR introduced by transfection into HeLa,4Jurkat,5,6 and THP-16 cells and can increase HIV-1 replication in the chronically infected human monomyelocytic cell line U-14,6 and the chronically infected T-lymphocyte cell line Jurkat.5 This effect of H2O2may be due, at least in part, to activation of Nuclear Factor κB (NF-κB), which can recognize NF-kB binding sites in the HIV-1 LTR and thus facilitate gene transcription.5 Other mechanisms, however, cannot be excluded. The activation by H2O2 of the HIV-1 LTR in THP-1 or Jurkat cells and of viral replication in U-1 cells is greatly potentiated by vanadate.6 Vanadate reacts with H2O2 to form peroxides of vanadate with heightened biologic activity.
We report here on the activation of the HIV-1 LTR in a T-lymphocyte–derived cell line by intact neutrophils stimulated either by PMA or opsonized zymosan.
MATERIALS AND METHODS
Special reagents.
PMA, sodium orthovanadate, and H2O2 (30% wt/wt) were obtained from Sigma Chemical Co (St Louis, MO). The H2O2 was assayed by its absorption at 230 nm, using an extinction coefficient of 81 mol/L−1cm−1. Human recombinant tumor necrosis factor-α (TNF-α) was generously provided by Genentech (South San Francisco, CA), and recombinant human interleukin-2 (IL-2) by Hoffman-La Roche (Nutley, NJ). Bovine liver catalase (CTS, 57,622 U/mg) was obtained from Worthington Biochem Corp (Freehold, NJ), and human erythrocyte catalase (50,000 U/mg) was obtained from Calbiochem (La Jolla, CA). The bovine liver catalase was dialyzed against water overnight and the catalase preparations were heated at 100°C for 20 minutes where indicated. Endotoxin contamination of the catalase preparations was determined using a Limulus Amebocyte Lysate kit (BioWhittaker, Inc, Walkersville, MD). Endotoxin was removed from the bovine liver catalase preparation by passage through a column containing polymyxin B immobilized on agarose (Detoxi-gel; Pierce, Rockford, IL). Superoxide dismutase (SOD, bovine erythrocytes, 5,000 U/mg) was obtained from Boehringer Mannheim Biochemicals (Indianapolis, IN). Bisindolylmaleimide 1 (BIM) and Gö 6976 were obtained from Calbiochem.
Cells.
IG5 (Jurkat LTRluc), a Jurkat T-cell–derived cell line containing a stably integrated HIV LTR-luciferase construct was obtained through the Research and Reference Reagent Program, Division of Acquired Immune Deficiency Syndrome (AIDS), National Institute of Allergy and Infectious Diseases (NIAID), National Institutes of Health (NIH) and maintained in RPMI-1640 containing 10 mmol/L Hepes buffer, 2 mmol/L L-glutamine, 50 U/mL penicillin, 50 μg/mL streptomycin sulfate, and 10% heat inactivated fetal bovine serum (RPMI-FBS) (GIBCO, Grand Island, NY). On the day of the experiment, the cells were suspended in RPMI without antibiotics or FBS (RPMI).
Neutrophils were isolated from venous blood collected from normal human volunteers and a CGD patient as previously described.7 The preparation contained greater than 97% neutrophils of which greater than 96% were viable as measured by trypan blue exclusion. The neutrophils were suspended in RPMI and used immediately.
Activation of the HIV-1 LTR.
Into 12 × 75-mm polypropylene tubes (Falcon 2063; Becton Dickinson Labware, Lincoln Park, NJ) were added 2 × 106 Jurkat LTRluc, the components indicated in the legends to the figures and table, and RPMI to a final volume of 2.0 mL. The tubes were incubated at 37°C in a CO2 incubator (5% CO2, 95% air) for 6 hours and the luciferase activity was determined using a luciferase assay kit (Promega Biotec, Madison, WI) and a Monolight 1500 luminometer (Analytical Luminescence Laboratories, San Diego, CA). Photons were counted over a 30-second period and designated as relative light units (RLU).
Chemiluminescence.
The components indicated in the legend to the figure were placed in 12 × 75 mm polypropylene tubes (Falcon 2063), which were incubated at 37°C in a CO2 incubator (5% CO2, 95% air). At intervals, chemiluminescence was measured over a 10-second period using the Monolight 1500 luminometer and the results expressed as RLU.
Statistical analysis.
The results are presented as mean ± standard error of mean (SEM) and the Mann Whitney U rank-sum test (unpaired, two-tailed) was used to analyze differences for significance unless otherwise indicated (NS, not significant P > .05).
RESULTS
Figure 1 demonstrates the activation of the HIV-1 LTR in Jurkat T cells by normal neutrophils + PMA. Neutrophils alone had no effect on the HIV-1 LTR at concentrations ranging from 3 × 104 to 107/mL. The Jurkat cell concentration was 106/mL so that the ratio of neutrophils:Jurkat cells ranged from 0.03:1 to 10:1. The LTR in Jurkat cells was activated by PMA alone (background RLU 20,218 ± 2,725; PMA 373,473 ± 65,262, n = 9, P < .001). However, when neutrophils and PMA were combined, activation of the LTR was significantly increased at a neutrophil concentration of 3 × 105/mL, reached a maximum at 106/mL (neutrophil:Jurkat ratio 1:1) and then decreased to a level significantly below that of PMA alone when the neutrophil concentration was increased to 107/mL. Activation of the LTR in the presence of PMA was significantly greater than that in the absence of PMA (P < .05) at all the neutrophil concentrations used except 107/mL. When normal neutrophils were replaced by neutrophils from a patient with CGD, the stimulatory effect in the presence of PMA was lost. The decrease in activity at high neutrophil concentration, however, was still evident.
Activation of the HIV-1 LTR in Jurkat T cells by neutrophils and PMA. The reaction mixture contained 2 × 106 Jurkat LTRluc and, where indicated, 100 ng/mL PMA and either normal or CGD neutrophils at the concentrations indicated, in RPMI at a final volume of 2.0 mL. The effect of PMA alone is indicated by the (○) (or ▵) at zero neutrophils/mL. The results with normal neutrophils are the mean ± SEM of 4 to 11 values and the results with CGD neutrophils are the mean ± SEM of 2 to 4 values. The asterisk indicates a significant difference from PMA alone (P< .05).
Activation of the HIV-1 LTR in Jurkat T cells by neutrophils and PMA. The reaction mixture contained 2 × 106 Jurkat LTRluc and, where indicated, 100 ng/mL PMA and either normal or CGD neutrophils at the concentrations indicated, in RPMI at a final volume of 2.0 mL. The effect of PMA alone is indicated by the (○) (or ▵) at zero neutrophils/mL. The results with normal neutrophils are the mean ± SEM of 4 to 11 values and the results with CGD neutrophils are the mean ± SEM of 2 to 4 values. The asterisk indicates a significant difference from PMA alone (P< .05).
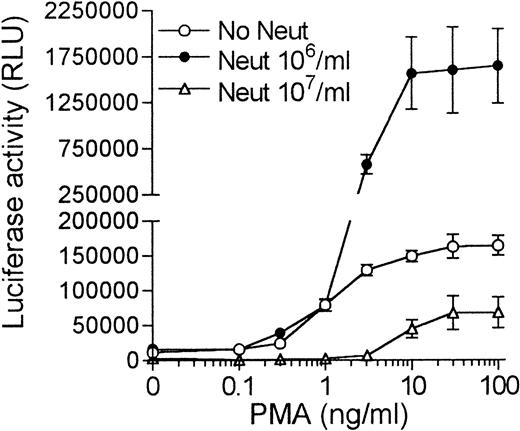
A PMA dose-response curve is shown in Fig2. A significant effect of PMA alone was observed at concentrations down to 1 ng/mL, whereas when PMA and 106 neutrophils/mL were combined, activation of the LTR was significantly greater than that produced by PMA alone at PMA concentrations down to 3 ng/mL. The decrease in activity at high neutrophil concentrations (107/mL) was observed at all of the PMA concentrations used.
PMA dose response curve. The reaction mixture contained 2 × 106 Jurkat LTRluc, either 106 or 107 neutrophils/mL and PMA at the concentrations indicated in RPMI at a final volume of 2.0 mL. The results are the mean ± SEM of four experiments. The y-axis was broken to allow for an increased scale in the lower range to illustrate the inhibitory effect of high neutrophil concentrations.
PMA dose response curve. The reaction mixture contained 2 × 106 Jurkat LTRluc, either 106 or 107 neutrophils/mL and PMA at the concentrations indicated in RPMI at a final volume of 2.0 mL. The results are the mean ± SEM of four experiments. The y-axis was broken to allow for an increased scale in the lower range to illustrate the inhibitory effect of high neutrophil concentrations.
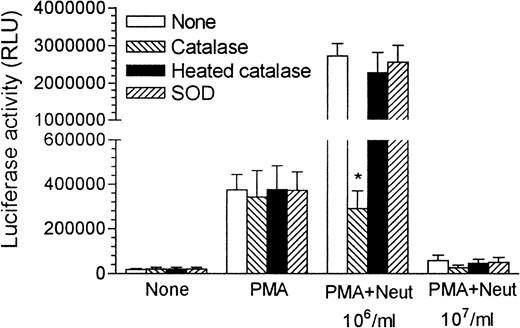
Catalase had no effect on the LTR when added alone or with either neutrophils (106 or 107/mL; data not shown) or PMA (Fig 3). However, when catalase was added to cells exposed to a combination of neutrophils (106/mL) and PMA, a significant inhibition was observed, with the activation of the LTR decreasing to the level observed with PMA alone. This inhibitory effect of catalase was lost on its heat inactivation. At the high neutrophil concentration (107/mL) where activation of the LTR by neutrophils + PMA was lower than that of PMA alone (Fig 1), the addition of catalase had no effect (Fig 3). SOD at 1 μg/mL had no effect on the activation of the LTR under any of our experimental conditions.
Effect of catalase, heated catalase, or SOD on the activation of the LTR by neutrophils and PMA. The reaction mixture contained 2 × 106 Jurkat LTRlucand, where indicated, 100 ng/mL PMA, 106 or 107neutrophils/mL, 8.2 μg/mL catalase, 8.2 μg/mL heated catalase, or 1 μg/mL SOD in RPMI at a final volume of 2.0 mL. The results are the mean + SEM of three to six experiments, with the asterisk indicating a significant difference from the absence of catalase, heated catalase and SOD (P < .05).
Effect of catalase, heated catalase, or SOD on the activation of the LTR by neutrophils and PMA. The reaction mixture contained 2 × 106 Jurkat LTRlucand, where indicated, 100 ng/mL PMA, 106 or 107neutrophils/mL, 8.2 μg/mL catalase, 8.2 μg/mL heated catalase, or 1 μg/mL SOD in RPMI at a final volume of 2.0 mL. The results are the mean + SEM of three to six experiments, with the asterisk indicating a significant difference from the absence of catalase, heated catalase and SOD (P < .05).
The catalase used in Fig 3 was from bovine liver. It contained 58 ng endotoxin per mg protein as measured by the Limulus Amebocyte Lysate assay. Passage of the catalase preparation through a polymyxin B column resulted in the removal of greater than 99% of the endotoxin. The resultant endotoxin-poor catalase preparation inhibited the activation of the HIV-1 LTR by neutrophils + PMA to a degree comparable to that of the original catalase preparation, as did erythrocyte catalase, which contained 4.0 ng endotoxin per mg protein.
Vanadate greatly potentiates the activation of the HIV-1 LTR in Jurkat cells by H2O2.6 Under the conditions used in Fig 4, vanadate at 3 × 10−5 mol/L had no effect on the activation of the LTR by a combination of neutrophils (106/mL) and PMA. However, when the neutrophil concentration was decreased to 105/mL, activation by neutrophils + PMA was decreased and now a significant stimulation by vanadate was observed.
Effect of vanadate on the activation of the LTR by neutrophils and PMA. The reaction mixture contained 2 × 106 Jurkat LTRluc and, where indicated, 3 × 10−5 mol/L vanadate, 100 ng/mL PMA, and neutrophils at the levels indicated, in RPMI at a final volume of 2.0 mL. The results are the mean + SEM of four to five experiments, and the asterisk indicates a significant difference from the absence of vanadate (P < .05).
Effect of vanadate on the activation of the LTR by neutrophils and PMA. The reaction mixture contained 2 × 106 Jurkat LTRluc and, where indicated, 3 × 10−5 mol/L vanadate, 100 ng/mL PMA, and neutrophils at the levels indicated, in RPMI at a final volume of 2.0 mL. The results are the mean + SEM of four to five experiments, and the asterisk indicates a significant difference from the absence of vanadate (P < .05).
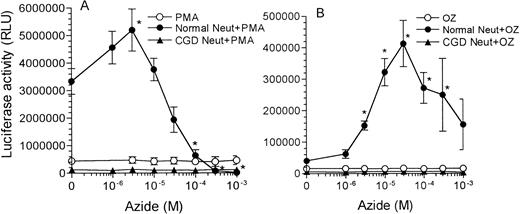
Azide is an inhibitor of hemeproteins, such as catalase and MPO, which degrade H2O2. Under the conditions used in Fig 5A,activation of the LTR by neutrophils + PMA was significantly increased by azide at 3 × 10−6 mol/L, whereas, when the azide concentration was increased to 10−4 to 10−3 mol/L, activation of the LTR was inhibited. Azide at concentrations ranging from 3 × 10−6 mol/L to 10−3mol/L had no effect on the activation of the LTR in Jurkat cells induced by PMA alone (Fig 5A). The stimulation by azide at 3 × 10−6 mol/L was not seen when normal neutrophils were replaced by CGD neutrophils.
Effect of azide on the activation of the LTR by neutrophils and either PMA or opsonized zymosan. The reaction mixture contained 2 × 106 Jurkat LTRluc, either 100 ng/mL PMA (A) or 1 mg/mL opsonized zymosan (OZ) (B), azide at the concentrations indicated and, where indicated, 106 normal or CGD neutrophils/mL in RPMI at a final volume of 2.0 mL. The results are the mean ± SEM of three to six experiments, with the asterisk indicating a significant difference from the absence of azide (P < .05).
Effect of azide on the activation of the LTR by neutrophils and either PMA or opsonized zymosan. The reaction mixture contained 2 × 106 Jurkat LTRluc, either 100 ng/mL PMA (A) or 1 mg/mL opsonized zymosan (OZ) (B), azide at the concentrations indicated and, where indicated, 106 normal or CGD neutrophils/mL in RPMI at a final volume of 2.0 mL. The results are the mean ± SEM of three to six experiments, with the asterisk indicating a significant difference from the absence of azide (P < .05).
These findings suggested that the H2O2 formed by the respiratory burst of PMA-stimulated neutrophils can activate the HIV-1 LTR in Jurkat T cells. It was, therefore, surprising that another potent stimulus of the respiratory burst of neutrophils, opsonized zymosan, when combined with neutrophils, had only a small effect on the LTR (Table 1). The combination of neutrophils and opsonized zymosan was significantly different from background by paired (P < .01), but not by unpaired, analysis. Azide at concentrations ranging from 3 × 10−6 to 3 × 10−4 mol/L significantly increased the activation of the LTR by normal neutrophils + opsonized zymosan, with an optimum effect observed at 3 × 10−5 mol/L azide (Fig 5B). Azide had no effect on the activation of the LTR either alone (data not shown), with normal neutrophils alone (data not shown), with opsonized zymosan alone (Fig5B), or with CGD neutrophils + opsonized zymosan (Fig 5B). The activation of the LTR by opsonized zymosan-stimulated normal neutrophils in the presence of azide was strongly inhibited (P< .001), but not abolished (P < .001) by catalase, whereas heated catalase was without effect (Table 1), implicating H2O2.
The considerably greater responsiveness of the LTR to neutrophils stimulated by PMA as compared with neutrophils stimulated by opsonized zymosan, despite both acting as strong stimuli of the neutrophil respiratory burst appears to be due, at least in part, to a synergism between H2O2 and PMA in the activation of the LTR. Under the conditions used in Fig 6, H2O2 alone at the optimum concentration of 10−4 mol/L increased luciferase activity from a background of 23,379 RLU to 110,956 RLU and PMA alone at 100 ng/mL increased luciferase activity to 403,823 RLU. When H2O2 and PMA were combined, luciferase activity was 3,096,165 RLU, which was significantly greater than the effect of H2O2 (P < .005) or PMA (P < .005) alone or than the additive effect of H2O2and PMA (P < .005). Thus, under these conditions, H2O2 and PMA act together to produce an effect, which is considerably greater than the sum of the effects of each alone. Synergism with H2O2 was not observed when PMA was replaced by TNF-α or IL-2 at 100 U/mL (Fig 6). IL-2 alone had no effect on the LTR in Jurkat cells under our experimental conditions.
Synergistic effect of H2O2 and PMA on activation of the LTR. The reaction mixture contained 2 × 106 Jurkat LTRluc and, where indicated, 100 ng/mL PMA, 100 U/mL TNF-, 100 U/mL IL-2, and H2O2 at the concentrations indicated in RPMI at a final volume of 2.0 mL. The effect of PMA, TNF-, or IL-2 alone is indicated by the (○) at zero H2O2concentration. The results are the mean ± SEM of four to six experiments. The asterisk indicates a significantly greater effect of a combination of PMA (or TNF- or IL-2) and H2O2 than the additive effect of each alone (P < .05).
Synergistic effect of H2O2 and PMA on activation of the LTR. The reaction mixture contained 2 × 106 Jurkat LTRluc and, where indicated, 100 ng/mL PMA, 100 U/mL TNF-, 100 U/mL IL-2, and H2O2 at the concentrations indicated in RPMI at a final volume of 2.0 mL. The effect of PMA, TNF-, or IL-2 alone is indicated by the (○) at zero H2O2concentration. The results are the mean ± SEM of four to six experiments. The asterisk indicates a significantly greater effect of a combination of PMA (or TNF- or IL-2) and H2O2 than the additive effect of each alone (P < .05).
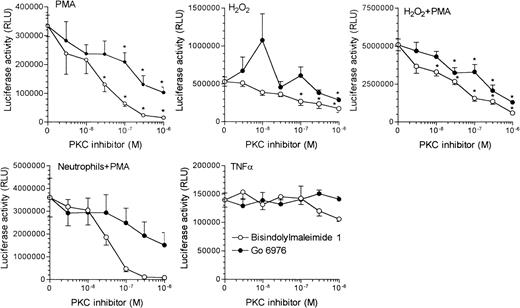
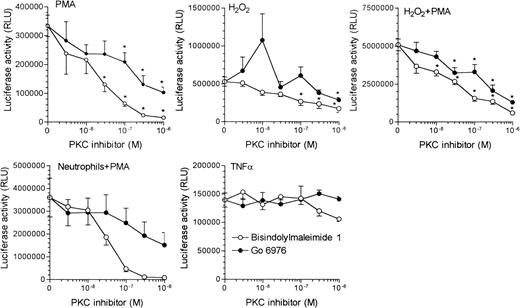
Because PMA activates PKC, the synergism between PMA and H2O2 may reflect a priming effect of PKC activation on the activation of the LTR by H2O2. This prompted a study of the effect of the PKC selective inhibitors BIM and Gö 6976 on the activation of the HIV-1 LTR in Jurkat T cells. BIM strongly inhibited the activation of the LTR by PMA, H2O2, H2O2 + PMA, and neutrophils + PMA, with an inhibitory effect observed at a concentration of 10−7mol/L, and in some instances, lower (Fig7). Gö 6976 was less effective with an inhibition observed at 10−6 mol/L in all instances. BIM and Gö 6976 at concentrations ranging from 3 × 10−9 to 10−6 mol/L were without effect on the activation of the LTR by TNF-α.
Effect of the PKC inhibitors BIM and Gö 6976 on activation of the LTR. The reaction mixture contained 2 × 106 Jurkat LTRluc and where indicated 100 ng/mL PMA, 10−4 mol/L H2O2, 106 neutrophils/mL, 100 U of TNF-/mL, and BIM and Gö 6976 at the concentrations indicated in RPMI at a final volume of 2.0 mL. The results are the mean + (Gö 6976) or − (BIM) SEM of four experiments with the asterisk indicating a significant difference from the absence of the PKC inhibitors (P < .05).
Effect of the PKC inhibitors BIM and Gö 6976 on activation of the LTR. The reaction mixture contained 2 × 106 Jurkat LTRluc and where indicated 100 ng/mL PMA, 10−4 mol/L H2O2, 106 neutrophils/mL, 100 U of TNF-/mL, and BIM and Gö 6976 at the concentrations indicated in RPMI at a final volume of 2.0 mL. The results are the mean + (Gö 6976) or − (BIM) SEM of four experiments with the asterisk indicating a significant difference from the absence of the PKC inhibitors (P < .05).
The effect of BIM on the respiratory burst of neutrophils stimulated with either PMA or opsonized zymosan as measured by either luminol or lucigenin-enhanced chemiluminescence is shown in Fig 8. Luminol-enhanced chemiluminescence by neutrophils is predominantly dependent on peroxidase-catalyzed reactions, whereas lucigenin-enhanced chemiluminescence is largely peroxidase-independent and related to superoxide anion release.8 Opsonized zymosan was more effective than PMA as a stimulus of luminol-enhanced chemiluminescence by neutrophils, whereas, when lucigenin-enhanced chemiluminescence was measured, PMA was more effective than opsonized zymosan as the stimulus. This may reflect a greater MPO release by the phagocytic stimulus opsonized zymosan. With both luminol and lucigenin, BIM almost completely inhibited PMA-induced chemiluminescence, whereas opsonized zymosan-induced chemiluminescence was decreased approximately 50%.
Effect of the PKC inhibitor BIM on the respiratory burst of neutrophils induced by PMA and opsonized zymosan. The reaction mixture contained 106 neutrophils/mL and where indicated 10−5 mol/L luminol, 10−4 mol/L lucigenin, 100 ng/mL PMA, 1 mg/mL opsonized zymosan, and 10−6 mol/L BIM in a standard salt solution (4 × 10−3 mol/L sodium phosphate buffer pH 7.4, 0.128 mol/L NaCl, 1.2 × 10−2mol/L KCl, 10−3 mol/L CaCl2, 2 × 10−3 mol/L MgCl2, 2 × 10−3mol/L glucose) at a final volume of 0.5 mL. The results are the mean + SEM of four experiments.
Effect of the PKC inhibitor BIM on the respiratory burst of neutrophils induced by PMA and opsonized zymosan. The reaction mixture contained 106 neutrophils/mL and where indicated 10−5 mol/L luminol, 10−4 mol/L lucigenin, 100 ng/mL PMA, 1 mg/mL opsonized zymosan, and 10−6 mol/L BIM in a standard salt solution (4 × 10−3 mol/L sodium phosphate buffer pH 7.4, 0.128 mol/L NaCl, 1.2 × 10−2mol/L KCl, 10−3 mol/L CaCl2, 2 × 10−3 mol/L MgCl2, 2 × 10−3mol/L glucose) at a final volume of 0.5 mL. The results are the mean + SEM of four experiments.
DISCUSSION
Activation of the HIV-1 LTR occurs by a variety of mechanisms, of which reaction of the product of the TAT gene with the TAR sequence in the LTR appears to be the most important. Activation of the LTR by H2O2 is an additional mechanism, raising the possibility that biologic sources of H2O2 such as stimulated phagocytes, may influence the replication of HIV-1. We report here that neutrophils, when combined with the stimulus PMA, strongly activate the HIV-1 LTR introduced by transfection into the Jurkat T-lymphocyte cell line. This activation by neutrophils and PMA is due to, at least, three processes: (1) the direct activation of Jurkat LTRluc by PMA; (2) the activation of the LTR by H2O2 formed by the PMA-induced respiratory burst of neutrophils; and (3) synergism between H2O2 and PMA in the activation of the LTR.
The direct activation of the LTR in Jurkat cells by PMA could account for only 12% to 13% of the total luciferase synthesis induced by neutrophils (106/mL) + PMA. Activation by PMA alone was unaffected by catalase or by vanadate (see also Kazazi et al6), which would argue against the involvement of H2O2, at least H2O2accessible to these agents. PMA is a potent activator of PKC. The involvement of PKC in the activation of the LTR by PMA is suggested by the inhibitory effect of the selective PKC inhibitors BIM and Gö6976. BIM had an IC50 for PMA-induced LTR activation of 0.02 μmol/L and Gö 6976 was approximately 10-fold less effective.
That H2O2 formed by the PMA-induced respiratory burst of neutrophils is also responsible, in part, for the activation of the LTR is supported by the inhibitory effect of catalase, the stimulatory effect of vanadate at suboptimal neutrophil concentrations and the loss of activity when normal neutrophils were replaced by neutrophils from a CGD patient. The effect of catalase is lost on its heat-inactivation and is unrelated to endotoxin contamination. Catalase reduces the activation of the LTR by neutrophils + PMA to the level observed with PMA alone, as did the substitution of CGD for normal neutrophils, suggesting that the total additional effect on the addition of neutrophils to PMA is due to the H2O2 formed.
Although both PMA and H2O2 can individually activate the HIV-1 LTR in Jurkat cells,6 the effect of their combination is considerably greater than the sum of each alone. The combination of PMA and reagent H2O2increases the activation of the LTR to the level observed with neutrophils + PMA. This suggests that PMA acts not only directly and by inducing H2O2 formation by the neutrophils, but also by increasing the sensitivity of the LTR in Jurkat cells to activation by H2O2. Some selectivity for PMA was observed, as H2O2 did not synergize with either TNF-α or IL-2 in the activation of the LTR. A synergism between PMA and H2O2 in the activation of NF-κB has been reported,9 and this may form the basis for the synergistic activation of the LTR by these agents. Activation of the LTR by PMA in the presence of neutrophils or H2O2 is inhibited by BIM and Gö 6976 suggesting the involvement of PKC in the synergism. PKC consists of a number of isoforms, which have in common catalysis of the phosphorylation of protein serine/threonine residues. PKC has been implicated in the replication of HIV-1 at a number of sites including the activation of the HIV-1 LTR10,11 where PKC may act in part through its activation of NF-κB.12-14 Activation of the LTR by H2O2 alone also is inhibited by the PKC inhibitors raising the possibility of an autostimulatory mechanism by which activation of PKC by H2O2 amplifies the subsequent response to H2O2. The PKC inhibitors at concentrations up to 10−6 mol/L did not inhibit the activation of the LTR by TNF-α, indicating some selectivity for PMA- and/or H2O2-induced activation.
The strong activation of the LTR by neutrophils + PMA reached a maximum at 106 neutrophils/mL and then decreased to levels below that of PMA alone when the neutrophil concentration was increased to 107/mL. The mechanism of this decrease in activity at high neutrophil concentration is unclear. The generation of reactive oxygen species as measured by chemiluminescence was increased at high neutrophil concentration raising the possibility of a toxic effect of products of the respiratory burst on the Jurkat LTRluccells; however, the decrease in LTR activation was not prevented by catalase suggesting that H2O2 was not a toxic species under these conditions. Neutrophils heated at 65°C for 15 minutes lose their ability to respond to PMA with a respiratory burst, but remain inhibitory of the LTR at high concentration (0.9 × 107 heated neutrophils + 106 normal neutrophils/mL) (data not shown). It is possible that a product of neutrophils unrelated to the respiratory burst is toxic to Jurkat cells at high neutrophil concentrations.
When opsonized zymosan was used instead of PMA as the stimulus of the neutrophil respiratory burst, activation of the LTR was considerably decreased. A small, but significant, activation was observed, which was less than 1% of that observed with neutrophils + PMA. Unlike PMA, opsonized zymosan did not have a direct effect on the Jurkat LTRluc nor did opsonized zymosan act synergistically with H2O2 to activate the LTR (data not shown). Azide is a potent inhibitor of the heme enzymes catalase and myeloperoxidase, which degrade H2O2 and, thus, the amount of H2O2 detected in the extracellular fluid on stimulation of neutrophils by PMA or opsonized zymosan is greatly increased by azide.15 The addition of azide thus would be expected to increase the availability of H2O2 for LTR activation. When Jurkat LTRluc were exposed to neutrophils + opsonized zymosan in the presence of azide, increased activation of the LTR was observed, which was strongly inhibited by catalase, but not by heated catalase, and was not seen when normal neutrophils were replaced by CGD neutrophils. In contrast, addition of azide to neutrophils stimulated by PMA had only a small stimulatory effect at low (3 × 10−6 mol/L) azide concentration, possibly due to the strong activation in the absence of azide.
Our findings suggest that H2O2 generated by the respiratory burst of neutrophils may influence the survival and replication of HIV-1 in two opposing ways: (1) by reaction with peroxidase and a halide to produce a viricidal effect1; and (2) by activation of the HIV-1 LTR with consequent stimulation of gene transcription and viral replication. The latter effect is favored by the addition of azide (which promotes the accumulation of H2O2 and its release into the extracellular fluid) or vanadate (which forms a bioactive complex with H2O2). Further, activation by H2O2 is amplified by procedures, such as the addition of PMA, which activates PKC. Activation of PKC occurs when receptor-mediated hydrolysis of inositol phospholipids induced by a variety of stimuli, including mitogens, growth factors, and cytokines results in the release of diacylglycerol.16H2O2, as well as other forms of oxidant stress, can also activate PKC.17-21 Activation of PKC by these and other mechanisms would be expected to increase the sensitivity of the HIV-1 LTR to further activation by H2O2generated by adjacent phagocytes, certain microorganisms such as vaginal lactobacilli, as well as from other sources.
ACKNOWLEDGMENT
We thank Peggy Sue O’Brien for the preparation of the manuscript.
Supported in part by Grant No. AI07763 from the National Institutes of Health, Bethesda, MD.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Seymour J. Klebanoff, MD, PhD, Department of Medicine, Box 357185, University of Washington, Seattle, WA 98195-7185; e-mail: seym@u.washington.edu.