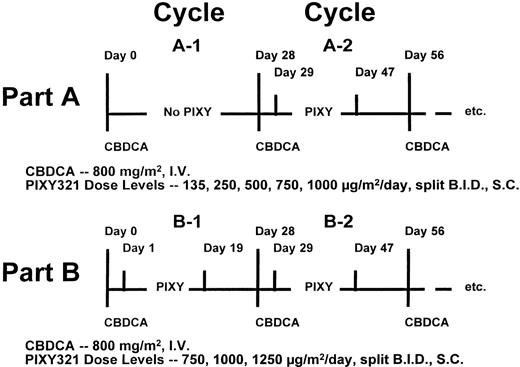
This dose-escalation study was performed to evaluate the hematologic activity, biological effects, immunogenicity, and toxicity of PIXY321 (an interleukin-3/granulocyte-macrophage colony-stimulating factor fusion protein) administered after high-dose carboplatin (CBDCA) treatment. Patients with advanced cancers received CBDCA at 800 mg/m2 intravenously on day 0 of repeated 28-day cycles. In part A of the study, patients were treated with CBDCA alone during cycle 1 and then received PIXY321 on days 1 through 18 of cycle 2 and later cycles. In part B, patients received 18 days of PIXY321 beginning on day 1 of all CBDCA cycles, including cycle 1. PIXY321 was administered subcutaneously in 2 divided doses. Total doses of 135, 250, 500, 750, and 1,000 μg/m2/d were administered to successive cohorts of 3 to 6 patients in part A. In part B, patient groups received PIXY321 doses of 750, 1,000, and 1,250 μg/m2/d. The hematologic effects of PIXY321 were assessed in the first 2 cycles of therapy. Anti-PIXY321 antibody formation was assessed by enzyme-linked immunosorbent assay (ELISA) and neutralization assay. Of the 49 patients enrolled, 31 were fully evaluable for hematologic efficacy. When comparing the first B cycle (cycle B-1; with PIXY321) with the first A cycle (cycle A-1; without PIXY321), the fusion protein had no significant effect on platelet nadirs or duration of platelets less than 20,000/μL but was able to speed the time of recovery of platelet counts to 100,000/μL (15v 20 days; P = .01). Significant improvements in neutrophil nadir and duration of ANC less than 500 were observed in cycles A-2 and B-1 (with PIXY321) as compared with cycle A-1 (without PIXY321). Initial PIXY321 prophylaxis (cycle A-2 and cycle B-1), enhanced the recovery of ANC to greater than 1,500/μL by an average of at least 8 days as compared with cycle A-1 (without PIXY321;P ≤ .004). However, positive PIXY321 hematologic effects were lost in the second course of PIXY321 among patients treated in part B. ELISA analysis showed that 92% of patients had developed neutralizing anti-PIXY321 antibodies by the completion of 2 PIXY321-containing cycles. The incidental action of PIXY321 to depress serum cholesterol levels was also abrogated during cycle B-2. We conclude that PIXY321 was active in speeding hematologic recovery but that neutralizing anti-PIXY321 antibody formation suppressed the hematologic and biochemical effects by the second cycle of PIXY321 administration. The immunogenicity of this fusion protein provides a cautionary warning that clinical development of bioengineered human molecules requires thorough testing for immune neutralization.
THE MYELOTOXIC limitations on cytotoxic drug delivery have spurred considerable interest in methods for selectively ameliorating hematologic side effects. The frequency of neutropenia as an oncologic problem has been the basis for granulocyte colony-stimulating factor (G-CSF) and granulocyte-macrophage colony-stimulating factor (GM-CSF) development. However, although these agents have consistently enhanced recovery of neutrophils after intensive chemotherapy, testing in randomized clinical trials has shown that they do not beneficially alter the incidence or duration of thrombocytopenia.1,2 Among a number of molecules with the ability to enhance platelet production, the multipotential cytokine, interleukin-3 (IL-3), has shown the capacity to promote in vitro growth of megakaryocyte progenitors,3 and its clinical administration has been associated with thrombocytosis.4,5Bilineage stimulation of myelopoiesis and thrombopoiesis has been increased by concurrent or sequential use of GM-CSF and IL-3 together.6-8
Based on such considerations, investigators at Immunex Corp (Seattle, WA) constructed a fusion protein, designated PIXY321, that combines GM-CSF and IL-3 into a single molecule.9 The component cytokines are coupled via a flexible linker sequence so that the binding domains of both moieties can interact with their independent receptor binding sites.9 PIXY321 binds to cells via either its GM-CSF or IL-3 domains, has comparable or greater affinity for GM-CSF and IL-3 receptors in competitive binding studies, stimulates the proliferation of normal human megakaryocyte and myeloid progenitors, and induces bilineage platelet and neutrophil production in monkeys.9-12
We hypothesized that PIXY321 might provide a conveniently administered method of diminishing both the platelet and neutrophil toxicities associated with chemotherapy. To test this hypothesis, we conducted this dose-escalation trial of PIXY321 administered after intensive, single-agent CBDCA. The objectives of the trial were to evaluate patterns of myelosuppression and hematologic recovery associated with the combined use of CBDCA and PIXY321, examine other biological activities of PIXY321 administration, assess patients for the production of anti-PIXY321 antibodies, and determine the toxicities of the fusion protein.
MATERIALS AND METHODS
Patient eligibility and enrollment evaluation.
Patients greater than 18 years of age with metastatic solid tumors were eligible for enrollment. They were required to have a Karnofsky performance status ≥70%, relatively normal hemopoietic reserve (white blood count [WBC] ≥4,000/μL, absolute neutrophil count [ANC] ≥1,500/μL, platelet count ≥100,000/μL, hemoglobin ≥8 g/dL), estimated creatinine clearance greater than 70 mL/min, normal hepatic function, and normal serum calcium. Patients with overt solid tumor involvement of the bone marrow; previous pelvic radiotherapy or irradiation to more than 20% of bone marrow; or earlier treatment with CBDCA, nitrosoureas, or mitomycin-C were not eligible. A negative β-HCG was required before study entry in all women of childbearing potential. All patients were required to read and sign a consent form approved by the local Institutional Review Board and by the Cancer Therapy Evaluation Program (CTEP) of the National Cancer Institute.
Study drugs.
The study was sponsored by CTEP under BB-IND #4341. Glycosylated PIXY321, produced in Saccharomyces cerevisiae, was provided via CTEP by the Immunex Corp as a lyophilized powder. A lyophilized, investigational form of CBDCA (IND #19314) that is identical to commercially available CBDCA was also supplied by CTEP.
Treatment protocol.
At planned intervals of 28 days, all patients received a fixed dose of CBDCA (800 mg/m2) by 30-minute intravenous infusion. Patients enrolled to part A of the protocol received the first course of CBDCA without PIXY321 support. During second and subsequent courses of CBDCA, part A patients received CBDCA on day 0, followed by a course of PIXY321 administered subcutaneously in divided doses approximately every 12 hours beginning on day 1 and continuing for at least 18 days (Fig 1). Successive groups of 3 to 6 evaluable patients were enrolled to receive progressively higher doses of PIXY321. Once the PIXY321 dose level was assigned for a particular patient, that patient did not receive higher doses of PIXY321 in subsequent cycles. Dose levels evaluated in part A of the protocol were 135, 250, 500, 750, and 1,000 μg/m2/d.
In part B of the trial, CBDCA was administered at a dose of 800 mg/m2 by 30-minute intravenous infusion every 28 days on day 0 of each cycle. PIXY321 was initiated on day 1 and continued for at least 18 days but was administered in every cycle, including the first (Fig 1). PIXY321 doses of 750, 1,000, and 1,250 μg/m2/d were tested in part B.
Patients could continue on therapy until the occurrence of clinical or radiographic evidence of tumor progression, unacceptable toxicity, or withdrawal of patient consent. Dose reductions of CBDCA were not allowed between cycles 1 and 2 unless a patient had experienced nonhematologic CBDCA toxicity ≥CTC grade 3 or a reduction in estimated creatinine clearance to less than 60 mL/min. Subsequent therapy was delayed until the ANC was greater than 1,500/μL and platelet count increased to greater than 100,000/μL. While on protocol, patients were not eligible to receive supportive therapy with other hematologic growth factors, eg, G-CSF or GM-CSF, or nonphysiologic doses of steroids. Bacterial infection was presumed in patients who developed a fever of ≥38.5°C at a time when their ANC was less than 500/μL and appropriate antibiotic intervention was provided. Depending on availability, either 8 to 10 U of random-donor platelets or a leukopheresis pack from a single donor was administered to subjects each time that their platelet counts were less than 20,000/μL. Any patient with a hemoglobin less than 8 g/dL received at least 2 U of packed red blood cells.
Data monitoring.
Complete blood counts (CBCs) were obtained at least 3 times per week. If the platelet count decreased to less than 50,000/μL, patients were to have daily CBCs until the platelet count recovered to greater than this level without transfusion. Serum was obtained on days 1, 2, 7, 14, and 28 for evaluation of serum chemistries. Part A patients had antibody determinations obtained at baseline and at the end of cycle A-2. Among part B patients, sera were tested at the end of cycles 1 and 2. Radiographic tumor evaluations were performed after every 2 cycles.
Serum antibody studies.
Enzyme-linked immunosorbent assays (ELISAs) for anti-PIXY321, anti–IL-3, and anti–GM-CSF antibodies were performed at Immunex in duplicate. Diluted patient sera were placed in plates coated with the test cytokine. Goat antihuman IgG antibody conjugated to horseradish peroxidase was used for signal detection. Positives were scored if the sample results showed an optical density at least 4 times that of matched baseline controls obtained before any CBDCA or PIXY321 administration. Sera that were positive for PIXY321 antibodies by ELISA were tested for neutralizing antibody that prevented PIXY321-induced, IL-3–induced, or GM-CSF–induced growth of human erythroleukemia (TF-1) cells. Neutralization was considered present if the posttreatment sample produced a ≥50% reduction in tritiated thymidine incorporation as compared with that observed with the corresponding baseline serum.
Statistical considerations.
Analysis of PIXY321 efficacy as a hematorestorative agent focused on its effects on thrombocytopenia, neutropenia, and serum cholesterol during the first 2 cycles of CBDCA administration. Comparisons were made both within patients (cycle 1 v cycle 2) and between patient groups (part A v part B). The focus of this analysis was on patients who completed the first 2 courses of therapy successfully; although this practice meant a reduction in the number of patients analyzed, it was felt to be necessary to avoid bias resulting from comparisons involving patients who were healthy enough to complete 2 courses of treatment and those who were not.
Parameters of interest in assessing PIXY321 hematologic effects were the depth of the platelet and neutrophil nadirs, the duration of time that the platelet counts were less than 20,000/μL and the ANC was less than 500/μL, and the time to recovery of blood counts to values that would allow CBDCA retreatment (platelets ≥100,000/μL, ANC ≥1,500/μL). On-time retreatment with CBDCA as well as incidence of neutropenic fevers, bleeding episodes, and number of transfusions were also assessed. Changes in serum cholesterol relative to baseline were analyzed as an additional measure of PIXY321 biological effect.
Patients treated at all dose levels of PIXY321 were analyzed together to increase the power of the tests, realizing that inclusion of patients treated at lower PIXY321 dose levels might diminish the extent of any differences in hematologic recovery. Paired comparisons were made between the first and second courses of treatment in both parts A and B of the study. Differences between groups A and B were assessed with two-sample tests. Proportional differences between patient groups and cycles were evaluated with two-sided, permutation exact tests. Descriptive analyses of antibody formation were performed in all patients who received PIXY321 and for whom sufficient serum was available at any of the designated timepoints.
RESULTS
Patient characteristics.
Forty-nine patients (29 men and 20 women) were enrolled in the study. The median age was 50 years (range, 24 to 71 years) and the median Karnofsky performance status was 90% (range, 70% to 100%). Thirty-four of the patients had undergone prior chemotherapy and 15 had received previous radiotherapy. The predominant tumor types were colorectal cancer (n = 15), melanoma (n = 12), renal cell (n = 7), sarcoma (n = 4), lung (n = 3), and head and neck (n = 1). One patient each with thymoma, carcinoid tumor, pheochromocytoma, and cancers of the pancreas, breast, and adrenal glands were also enrolled.
Patient evaluability.
Of the 49 patients enrolled, 6 experienced progressive cancer and 2 requested removal from study after having received CBDCA alone during cycle A-1. As a consequence, 41 patients actually received PIXY321 and were evaluable for PIXY321 toxicity (24 patients in part A and 17 patients in part B). Ten other patients were not included in the hematologic efficacy analysis. Reasons for exclusion were removal from study for progressive disease (1 patient in part A and 3 patients in part B) or excessive toxicity before completing 2 full CBDCA treatment courses (1 patient in part A and 3 patients in part B). Protocol violations were recognized in 2 part-A patients. One patient had a combination of a rapidly declining performance status and excessive prior cytotoxic therapy and the other received therapeutic G-CSF for neutropenic sepsis. Thus, 20 patients who completed the entire course of PIXY321 with full doses of CBDCA during both cycles A-1 and A-2 were fully evaluable for hematologic effects (4 patients received 135, 5 patients received 250, 3 patients received 500, 4 patients received 750, and 4 patients received 1,000 μg/m2/d of PIXY321). Eleven patients received full-dose CBDCA and a complete PIXY321 course in both cycles B-1 and B-2 (4 patients received 750, 3 patients received 1,000, and 4 patients received 1,250 μg/m2/d of PIXY321). Twenty-four patients enrolled to part A and 15 patients entered onto part B of the trial had sera available for antibody analysis.
Comparisons made both within evaluable patients (cycle 1 vcycle 2) and between evaluable patient groups (part A v part B) indicated no significant differences in mean estimated creatinine clearance (P values for all comparisons ≥.20) that might have been associated with confounding alterations in CBDCA clearance (data not shown).
Hematologic efficacy.
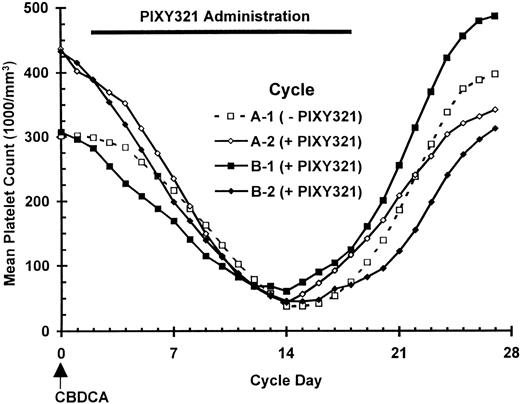
Following the expected platelet nadir after administration of CBDCA alone in cycle A-1, patients experienced a rebound thrombocytosis that left the average platelet count significantly higher (P < .001) at the start of cycle A-2 than it had been before any therapy (Fig 2). Despite this boost in platelet counts, a rapid decrease in their number during subsequent PIXY321 administration in cycle A-2 limited the ability of PIXY321 to improve the nadir or shorten the period that platelet counts were less than 20,000/μL when cycle A-2 (with PIXY321) was compared with cycle A-1 (without PIXY321; Table 1). A greater effect of PIXY321 on platelets seemed evident in the first-cycle comparison of B-1 patients (with PIXY321) to those treated in A-1 (without PIXY321); platelet counts among B-1 patients decreased more rapidly and then increased more quickly and to higher average levels than among the A-1 controls, again with no significant effect on the nadir. The use of higher PIXY321 dose levels and the lack of cumulative marrow toxicity associated with prior CBDCA use may have accounted for the more pronounced effect in cycle B-1 than in cycle A-2. Because the predominant action of PIXY321 was to shift the platelet curves to the left during cycle B-1, the time that counts were under 20,000/μL was not significantly altered. However, recovery of platelets was significantly enhanced; platelets reached 100,000/μL in 15 days with PIXY321 during cycle B-1 as opposed to a 20-day recovery time in CBDCA alone controls (P = .01).
Platelet counts in patients completing 2 full cycles of CBDCA. Curves depict results from 20 part A patients and 11 part B patients.
Platelet counts in patients completing 2 full cycles of CBDCA. Curves depict results from 20 part A patients and 11 part B patients.
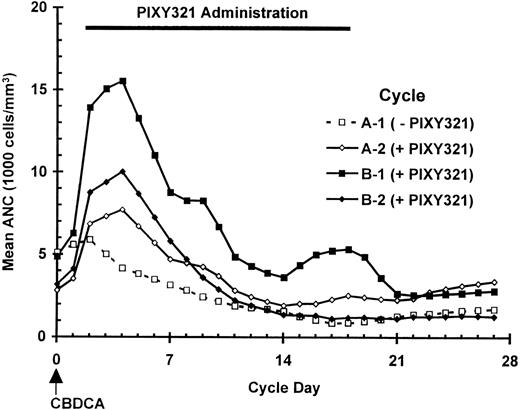
PIXY321 impact on neutrophil numbers was most conspicuous in the initial, B-1 cycle of administration, in which marked elevations in ANC were noted, peaking on day 4 (Fig 3). This initial increase was followed by a blunted nadir and more rapid neutrophil recovery. Also evident was a minor slump in average ANC after discontinuation of PIXY321 on day 18; this was most obvious among B-1 patients, but it is also apparent in those receiving PIXY321 for the first time in cycle A-2. Significant improvements in nadir neutrophil counts were noted with initial PIXY321 administration, both in cycle A-2 or B-1 (with PIXY321) as contrasted with cycle A-1 (without PIXY321; Table 2). The initial course of PIXY321 prophylaxis, whether given in cycle A-2 or cycle B-1 was also clearly able to hasten recovery of neutrophils, reducing the duration of ANC less than 500/μL by 1.6 to 2.5 days and significantly shortening the mean time required to achieve an ANC greater than 1,500/μL by at least 8 days (Table 2).
ANC in patients completing 2 full cycles of CBDCA. Curves depict results from 20 part A patients and 11 part B patients.
ANC in patients completing 2 full cycles of CBDCA. Curves depict results from 20 part A patients and 11 part B patients.
When the fusion protein was administered for 2 successive cycles, it proved unable to overcome the cumulative neutropenia associated with repeated CBDCA administration; both the depth and duration of severe neutropenia worsened in cycle B-2 as compared with cycle B-1 (Fig 3). Although a modest rise in prenadir ANC was observed, the nadir was significantly lower than seen in cycle B-1 (P = .008) and no evidence of postnadir PIXY321 effect was observed. Particularly striking was the protracted time in cycle B-2 between chemotherapy administration and recovery of ANC to at least the 1,500 cells/μL required for patients to initiate a third cycle of CBDCA. Cycle B-2 patients required a mean of 22 days to achieve this neutrophil level, a period identical to the recovery time observed in cycle A-1 patients receiving CBDCA alone (Table 2).
At least 1 platelet transfusion was administered to 65% (13/20) of control subjects in cycle A-1 and the median platelet transfusion requirement for these patients was 1 transfusion per cycle. PIXY321 was neither able to favorably decrease the proportion of patients needing platelet transfusion nor able to reduce the median number of transfusion events. No salutary effects on RBC transfusion requirements were noted. One patient had a bleeding episode associated with a peptic ulcer during cycle A-1. No bleeding occurred in cycles A-2, B-1, or B-2. Neutropenic fever occurred in fewer than 18% of patients in any cycle, and the incidence was not statistically altered by PIXY321 administration.
Platelet recovery did not delay administration of the next cycle of CBDCA. When postponement of chemotherapy was required, failure to attain an ANC of 1,500/μL was universally responsible. PIXY321, administered for the first time in either cycle A-2 or B-1, reduced treatment delays by enhancing neutrophil recovery. This could be statistically significant; none (0/20) of the cycle A-2 patients failed to recover on time while receiving PIXY321, whereas 30% (6/20) of these same patients were unable to do so in cycle A-1 when not receiving PIXY321 (P = .03). However, the loss of neutrophil restorative activity observed with repeated administration of cytokine prophylaxis caused 55% (6/11) of the patients in cycle B-2 to be ineligible for chemotherapy on time on day 28; comparison with the 9% (1/11) occurrence of delays in cycle B-1 (P = .06) or 0% in A-2 (P = .001) indicated that this could be statistically worse.
Anti-PIXY321 antibodies.
The failure of PIXY321 to maintain its beneficial effects when administered for more than a single treatment course led us to be concerned that its activity was being suppressed immunologically. For this reason, patient sera were analyzed by ELISA for the presence of antibodies against PIXY321, IL-3, and GM-CSF. Samples that were ELISA-positive were examined for the presence of neutralizing effects on biologic function in vitro.
Greater than 80% of part B patients treated with PIXY321 were ELISA-positive for anti-PIXY321 and anti–IL-3 antibodies by the end of cycle 1 (Table 3). By the completion of cycle B-2, 93% of patients had developed anti-PIXY321 antibodies, and, in 92% of patients, this immune response proved to be neutralizing. Among patients treated in part B, 86% developed anti–IL-3 and 64% had anti–GM-CSF antibodies by the end of cycle 2, although there was a lesser likelihood that these would be neutralizing (29% and 45%, respectively). There was the general sense that cycle A-2 patients, some of whom received lower doses of PIXY321, were less likely to develop neutralizing antibody; however, a formal regression analysis failed to confirm a clear dose-response effect (data not shown). It is also hypothetically possible that cumulative immunosuppression from the chemotherapy may have blunted an antibody response in cycle A-2 patients, because they had received CBDCA twice before beginning their initial PIXY321 course.
Other laboratory endpoints.
Having observed in vitro evidence of anti-PIXY321 antibody formation and an in vivo reduction in PIXY321 effect on hematologic parameters, we sought corroborating evidence of a decrease in other biological activity. No alterations in lactate dehydrogenase, uric acid, or alkaline phosphatase were noted as have been observed with G-CSF13 or GM-CSF.14,15 However, significant decrements in serum cholesterol (Fig4) were noted, a finding consistent with known actions of GM-CSF.14 15 The declines in serum cholesterol were most pronounced when PIXY321 prophylaxis was administered for the first time; in cycle A-2 or in cycle B-1, proportional decreases on days 2, 7, and 14 were significantly more profound during PIXY321 administration than those observed with CBDCA alone on the equivalent days. However, consistent with the loss of fusion protein effect on hematologic recovery during the second cycle of administration, the PIXY321-induced depression of serum cholesterol was lost during cycle B-2 at a time when most of these patients were known to have developed in vitro neutralizing anti-PIXY321 antibodies; serum cholesterol levels were statistically comparable to those observed during the CBDCA-alone control cycle (A-1).
Proportional serum cholesterol levels. Curves depict results from 20 part A patients and 11 part B patients. Values marked by an asterisk are significantly different from (□) A-1 (-PIXY321) at those timepoints (P ≤ .05, two-sided, permutation exact tests).
Proportional serum cholesterol levels. Curves depict results from 20 part A patients and 11 part B patients. Values marked by an asterisk are significantly different from (□) A-1 (-PIXY321) at those timepoints (P ≤ .05, two-sided, permutation exact tests).
PIXY321 toxicity.
The most definite adverse PIXY321 event was low-grade skin irritation at injection sites. Occasional patients also noted minor bruising at injection sites during periods of thrombocytopenia. Generalized rashes were not observed. The other common toxicities associated with PIXY321 administration were minor constitutional complaints of fever, chills, myalgias, arthralgias, and headache that predominated in the first several days of PIXY321 administration, primarily in the initial course of treatment. Six serious adverse events were observed in patients enrolled to the trial. Events felt not to be PIXY321-related included an exacerbation of gout, acute renal failure, deep vein thrombosis, and a fatal ischemic cerebral vascular accident. One patient had a subendocardial infarction and another developed atrial fibrillation; PIXY321 was listed as having a possible contributing role in these conditions. Thirteen patients received chemotherapy beyond cycle 2 of the protocol. None of these patients experienced any late or cumulative PIXY321 toxicity; in particular, no allergic reactions or prolonged neutropenia or thrombocytopenia occurred.
DISCUSSION
In this phase I trial of PIXY321, we attempted to characterize several biological activities of PIXY321 over a range of doses that would likely have positive hematologic activity and tolerable side effects based on past experience with glycosylated forms of IL-34,5,7 and GM-CSF.16-18
We found that, during the initial cycle of CBDCA, PIXY321 prophylaxis was able to induce a more rapid recovery of platelet counts. However, the depth of the nadir was less clearly affected by the cytokine, and the time that platelet counts were less than 20,000/μL was not altered because platelet counts decreased more quickly when the fusion protein was administered. These relatively modest effects of PIXY321 on platelet counts may have been presaged by the marginal evidence for benefit that emerged from clinical trials using recombinant IL-3 prophylaxis after chemotherapy.19-21 Because it acts so early in hematopoiesis and can stimulate such a broad variety of cell lineages, the thrombocytosis induced by IL-3 occurs relatively late5,22,23 and may be dampened by the counterregulatory effects of other cell types and cytokines present in the hematopoietic cascade. Evidence from canine studies indicates that GM-CSF stimulates Kupffer-cell–mediated platelet destruction within the liver, shortening platelet half-life24; such an effect may explain the relatively rapid decrease in platelet counts that has been a feature of PIXY321 prophylaxis25 and has also been seen with administration of GM-CSF16,26 or IL-3.27 28
Favorable actions on neutrophil numbers were much more evident with PIXY321; significant improvements in both the depth and duration of neutropenia were observed during the first course of fusion protein administration, and these benefits enhanced the prospect that subsequent chemotherapy could be administered on time. Unfortunately, it became apparent during the B portion of the study, when patients received PIXY321 prophylaxis after both first and second cycles of CBDCA, that these advantages were not sustained. Neutrophil recovery after the nadir was clearly worse late in cycle B-2 than during the B-1 cycle. Of particular note, the postnadir neutrophil recovery in cycle B-2 was also less rapid than that observed in A-2 patients who received PIXY321 for the first time in the second cycle. It appeared that the second-cycle advantages of PIXY321 use were being abrogated only if the fusion protein had been previously administered.
This loss of activity was most readily explained by immunologic neutralization in patients who received 2 courses of the cytokine. The timing of the loss of hematologic effects late in cycle B-2 was consistent with in vivo induction of a primary immune response in cycle B-1 that was boosted by later injection of antigen in the B-2 cycle. In vitro, 53% of the patients had developed neutralizing antibodies by the end of the B-1 cycle, and 92% of the participants had become neutralizing-antibody positive at the completion of cycle B-2. The correlation between the presence of in vitro neutralizing antibody and loss of biological activity was strengthened by the finding that the incidental actions of PIXY321 to lower serum cholesterol levels during the first course of fusion-protein prophylaxis (cycles A-2 or B-1) were also negated during cycle B-2. In vitro neutralization in PIXY321 assays appeared greater than in IL-3 and GM-CSF assays, suggesting that the foreign linker portion of the molecule might have been involved in inducing the immunogenic effect. However, specific studies to determine the location of the immunogenic epitopes on the PIXY321 protein were not performed, and it is not possible to exclude other reasons (eg, a greater number of epitopes on the larger PIXY321 molecule) for the findings.
The formation of neutralizing antibodies clearly has precedent based on past experience with other recombinant cytokines, eg, interferon-α29 and IL-2.30,31 Ecogramostim GM-CSF had also provoked antibody formation, both to itself and to therapeutic monoclonal antibodies.32,33 Breaking of tolerance to endogenous cytokines has been observed with G-CSF in an experimental dog model34 and with pegylated recombinant megakaryocyte growth and development factor (MGDF) in human trials,35 resulting in neutropenia and thrombocytopenia, respectively.
Although we noted no overt clinical evidence that administration of PIXY321 induced patients to break tolerance to endogenous GM-CSF or IL-3, PIXY321 did appear to be potently immunogenic in this study. A number of reasons may exist to explain this finding beyond the artificial nature of PIXY321 and the fact that we very systematically looked for antibody induction. It has become evident that GM-CSF has a critical role in the proliferation, maturation, trafficking, and function of antigen-presenting dendritic cells.36,37 It is interesting to speculate that the GM-CSF moiety in PIXY321 might assist dendritic cells in finding and processing the IL-3 or linker portions of the fusion protein for presentation to lymphocytes. Such a strategy has already been exploited preclinically to enhance the immunogenicity of a tumor vaccine.38 Because relatively high concentration of dendritic cells is found in the skin, the subcutaneous administration of the drug twice per day in this trial may have enhanced the likelihood of PIXY321 antigenic processing. It is also possible that a high incidence of antibody induction was observed because we treated patients with solid tumors who were better capable of mounting an immune response; by contrast, individuals with lymphoid malignancies might have relatively low rates of antibody induction to recombinant cytokines.32
In other experience with PIXY321, patients received the cytokine after very immunosuppressive treatment with high-dose alkylating agents, steroids, or whole body irradiation,25,39-48 modalities that may be more immunosuppressive than CBDCA.49 The contention that we did not induce substantial immune dysfunction with administration of single-agent CBDCA may be supported by an Immunex review of antibody formation in patients receiving PIXY321 in these other studies; only 25% (76/302) developed anti-PIXY321 antibodies and in only 4.3% (13/302) was in vitro neutralization demonstrated (L. Garrison, personal communication, May 1996).
In conclusion, we have found that, although PIXY321 proved quite tolerable over a wide range of doses when administered subcutaneously after high-dose CBDCA, it had only modest platelet restorative activity. In addition, the striking improvements in neutrophil accounts observed with use of the PIXY321 were rapidly abrogated by the near universal induction of neutralizing anti-PIXY321 antibodies. Ultimately, this experience with PIXY321 may represent an important warning that we must carefully assess the immunogenicity of new recombinant human hematopoietins and other proteins as they enter clinical trials. This may prove particularly important when the new agent is a substantially modified version of a native molecule, immune compromise is not likely to be present, the subcutaneous route is used, and/or immune stimulatory molecules such as GM-CSF are administered concurrently.
ACKNOWLEDGMENT
The authors recognize the enormous contributions made to the completion of this study by the nursing, laboratory, and administrative staffs of the Biological Response Modifiers Program and the Clinical Services Program of SAIC Frederick. The expert bibliographic assistance of Carolyn Nagler is gratefully acknowledged. Our appreciation is also extended to Nilsen L. Miller for diligence in collating study data.
Preliminary results presented at the 12th (1993) and 15th (1996) Annual Meetings of the American Society of Clinical Oncology, Orlando and the 8th Annual (1994) NCI-EORTC Symposium on New Drugs in Cancer Therapy, Amsterdam, The Netherlands.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Langdon L. Miller, MD, Pharmacia & Upjohn, Inc, Mail Code 7216-298-163, 7000 Portage Rd, Kalamazoo, MI 49001-0199; e-mail: langdon.l.miller@am.pnu.com.