Abstract
Plasma and platelet factor Va represent different substrates for activated protein C (APC). In this study, we have measured platelet-dependent APC resistance and the effect of aspirin and a platelet glycoprotein IIbIIIa antagonist (GR144053F) on this phenomenon. In platelet rich plasma (PRP), progressive APC resistance was observed with increasing platelet activation. APC sensitivity ratios of 1.8, 1.7, and 1.4 were observed after platelet activation with thrombin receptor activating peptide (TRAP), collagen, and A23187, respectively. Ultracentrifugation at 77,000g for 1 hour abolished APC resistance indicating that the phenotype is associated exclusively with the platelet membrane. APC resistance was not observed in the presence of phosphatidylcholine-phosphatidylserine (PCPS) vesicles or purified human plasma lipoproteins. APC resistance was observed in the presence of platelet-derived microparticles, but to a lesser degree than that in the presence of activated platelets. The platelet-dependent APC resistance phenotype was also observed when endogenous APC was generated by Protac (American Diagnostica, Inc, Greenwich, CT). In vitro inhibition of platelet activation with aspirin had no effect, but the fibrinogen receptor antagonist, GR144053F, inhibited platelet-dependent APC resistance. These results indicate that platelet activation results in an APC-resistant phenotype comparable to that observed in the plasma of patients with factor V gene mutations affecting critical APC cleavage sites. This suggests that platelet activation at the site of endothelial damage downregulates a critical natural anticoagulant mechanism. The antithrombotic effect of aspirin may be due to an indirect effect on platelet-dependent APC resistance with reduced platelet retention within a developing thrombus. The more potent antithrombotic effect of glycoprotein IIbIIIa antagonists may in addition be the result of reduced platelet factor Va expression and modulation of the platelet-dependent APC resistance phenotype.
RESISTANCE TO activated protein C (APC resistance) was described by Dahlback et al in 1993.1 The molecular defect responsible for this phenomenon is typically a mutation in the factor V gene, which results in a protein with an altered amino acid sequence at a critical APC cleavage site. In almost all cases, this is a point mutation within codon 506 (G1691A), which alters the sequence of the initial APC cleavage site in the heavy chain of factor Va (factor V Leiden, FVR506Q).2-5 However, a point mutation within codon 306 (G1091C) also causes an APC resistance phenotype. This latter mutation alters the APC cleavage site primarily responsible for loss of cofactor activity (factor V Cambridge, FVR306T).6 Resistance to APC and the FVR506Q mutation are the most common identifiable defects in patients with venous thromboembolism.7,8 In contrast, the prevalence of the FVR506Q mutation is not increased in unselected patients with myocardial infarction or thrombotic stroke.9 However, recent evidence indicates that cerebrovascular disease may be associated with APC resistance in the absence of the FVR506Q mutation.10 This pattern of APC resistance may be an acquired phenotype due to platelet activation and the presence of platelet-derived microparticles in plasma samples. In vitro studies have already shown an APC-resistant phenotype in the presence of freeze-fractured platelets11-13 and Camire et al14 have shown that platelet-derived factor Va cofactor activity is sustained on the surface of activated platelets despite the presence of APC.14
Characterization of a platelet-dependent APC resistance phenotype would define a new mechanism of platelet-dependent thrombin generation and further explain the role of platelets in arterial thrombosis. In addition, it might provide insight into the antithrombotic mechanism of established antiplatelet drugs, such as aspirin, and provide a target mechanism for new antithrombotic agents. The purpose of this current study was to quantify the effect of platelets on APC sensitivity and to determine if platelet activation causes an APC resistance phenotype comparable to that produced by mutations in the factor V gene. In addition, we aimed to determine if the platelet-dependent APC resistance phenotype could be mimicked by phospholipids, which were not of platelet origin, for example atherogenic lipoproteins, which are capable of supporting thrombin generation. Finally, we examined the differential effect of aspirin and a platelet fibrinogen receptor antagonist to determine if the antithrombotic effect of antiplatelet therapy is due to a direct effect on platelet factor V expression or an indirect effect due to reduced platelet localization within a developing clot or thrombus.
MATERIALS AND METHODS
Materials and Reagents
COATEST APC Resistance-C kits and chromogenic substrate (S-2366) for measurement of APC were from Chromogenix (Molndal, Sweden). Protac-C was from American Diagnostica, Inc (Greenwich, CT). The thrombin receptor activating peptide SFLLRNPNDKYEPF (TRAP), calcium ionophore A23187, collagen 885-1, and acetylsalicylic acid (aspirin), o-phenylenediamine dihydrochloride, prostaglandin E1, and Sepharose CL-6B were from Sigma Chemical Co (St Louis, MO). Thromborel R was from Behring (Marburg, Germany) and purified APC from Diagnostica Stago (Asnieres, France). Gel-chromatography columns were obtained from Pharmacia Biotech (Uppsala, Sweden). Microtiter plates were from Maxisorp (Nunc, Denmark). CD61 monoclonal antibody to platelet glycoprotein IIIa and horseradish peroxidase–conjugated rabbit anti-mouse antibodies were obtained from DAKO (Glostrup, Denmark).
Phospholipid vesicles composed of 75% (wt/wt) phosphatidylcholine and 25% (wt/wt) phosphatidylserine (PCPS) were a gift from Prof Alan Giles (Queens University, Kingston, Ontario, Canada). The fibrinogen receptor antagonist GR144053F was a gift from Glaxo Wellcome (Stevenage, UK). Heparin was purchased from CP Pharmaceuticals (Wrexham, UK) and human albumin from Bio Products Laboratory (Elstree, UK).
Preparation of Platelet-Poor Plasma (PPP), Platelet-Rich Plasma (PRP), and Platelet Microparticle-Free Plasma
Blood from healthy volunteers, without the FVR506Q mutation, was obtained by venipuncture after application of a light tourniquet and collected into 0.109 mol/L sodium citrate (9:1 vol/vol). PRP was prepared by centrifugation at 110g for 10 minutes at room temperature. Platelet counts were measured using a Coulter model STKS and platelet counts in PRP were adjusted by addition of PPP, which was obtained by centrifugation at 800g for 15 minutes. This centrifugation removes most platelets, but platelet-derived fragments and platelet microparticles (PMPs) remained in the plasma supernatant and were detectable by flow cytometric analysis with CD61 (not described) and enzyme-linked immunosorbent assay (ELISA) (see below). Ultracentrifugation at 77,000g for 1 hour at 4°C removed all detectable platelet-derived material.
Freeze-Fractured Platelets
Freeze-fractured PRP was prepared from pooled PRP after adjustment of platelet count to 400 × 109/L. The PRP was subjected to three cycles of freezing at −80°C and thawing at 37°C. The freeze-fractured platelet suspension was double diluted in platelet microparticle-free plasma, produced by ultracentrifugation at 77,000g for 1 hour, and stored at −80°C.
PCPS Vesicles
Lyophilized phosphatidylserine:phosphatidylcholine vesicles (25%:75%) were reconstituted with deionized water and resuspended in microparticle-free plasma at a stock concentration of 1.5 mmol/L. This stock concentration was double diluted in microparticle-free plasma to obtain working concentrations of vesicles (1 to 500 μmol/L).
Plasma Lipoproteins
Single classes of human plasma lipoproteins (high-density lipoprotein [HDL], very low-density lipoprotein [VLDL], low-density lipoprotein [LDL], and oxidized LDL) were prepared as previously described.15 The protein content of each lipoprotein fraction was measured by a modified Lowry method and concentration expressed as protein content.16 The ability of lipoproteins to support thrombin generation in a purified component assay was performed as previously described.15
Detection of Platelet-Derived Microparticles by ELISA
Preparation of platelet microparticles.
PRP was prepared as described above and applied to a C-series 16/40 gel-chromatography column packed with Sepharose CL-6B.17The eluting solution used for gel filtration was phosphate-buffered saline (PBS), pH 7.2. Eluted gel-filtered platelets were counted on a Coulter STKS and adjusted to 150 × 109/L in PBS. For the purpose of generating a standard curve for the microparticle ELISA, microparticle formation was induced by activating gel filtered platelets with 1.0 mmol/L A23187 and 0.5 mmol/L CaCl2(final concentrations). The suspensions were then centrifuged at 6,000g for 5 minutes to remove remnant platelets. The microparticle suspension was double diluted in PBS and 250 μL of each dilution was added to 750 μL of ultracentrifuged platelet microparticle-free plasma.
Plate preparation.
One hundred microliters of PRP and 100 μL of carbonate buffer (0.05 mol/L sodium carbonate-bicarbonate buffer, pH 9.6), were added to each well of a polystyrene microtiter plate. Plates were centrifuged at 1,000g for 12 minutes to produce a platelet monolayer coating. The supernatant was gently decanted, and 300 μL of the 1% formaldehyde and 0.01% human serum albumin fixative solution was added to each well and incubated for 1 hour. The plate was washed four times with platelet wash buffer (0.35% albumin Tyrode’s solution containing 0.5 mmol/L prostaglandin E1 and heparin 5 U/mL, pH 7.4).
Sample preparation.
Platelets were removed from plasma samples by centrifugation at 6,000g for 5 minutes. The resultant PPP (containing microparticles) was added to 1% formaldehyde and human serum albumin fixative solution at a ratio of 1:2. This fixed solution was incubated with CD61 (DAKO), final concentration 1:250, for 2 hours at room temperature, resulting in antibody-microparticle complexes and excess free antibody. A total of 100 μL of this solution was incubated in wells in the platelet-coated microtiter plates for 2 hours at room temperature to capture free CD61. After a gentle wash cycle to remove microparticle complexed CD61, 100 μL of horseradish peroxidase–conjugated rabbit anti-mouse antibody (DAKO) at a concentration of 1:500 in platelet wash buffer was added to the plate and incubated for 1.5 hours at room temperature. The plate was then developed using 100 μL of 30 mg o-phenylenediamine dihydrochloride dissolved in 10 mL of citrate phosphate buffer (0.1 mol/L, pH 6.0) that had been activated by 20 μL H2O2. The development was stopped after 5 minutes by the addition of 150 μL 1 mol/L H2SO4. Absorbance was read at a wavelength of 492 nm. The amount of free CD61 detected was inversely proportional to the number of microparticles in the plasma sample.
A standard curve was created using dilutions of ionophore-generated microparticles prepared as above. The resultant absorbance was plotted against preionophore-activation platelet count on a log-linear scale. Correlation coefficients for the standard curve were greater than 0.99. The ELISA detected increasing amounts of platelet microparticles in the spiked plasma after activation with as little as 10 nmol/L ionophore and dilutions equivalent to a preactivation platelet count of 1 × 109/L.
APC Sensitivity Ratios
Activated partial thromboplastin times (APTT) were measured with COATEST APC Resistance-C kits on a KC10 coagulometer (Amelung, Germany). A total of 100 μL of sample was incubated with 100 μL of APTT reagent (purified phospholipid with colloidal silica as contact activator) for 5 minutes at 37°C. Clot formation was initiated by the addition of 100 μL of either CaCl2(0.025 mol/L in Tris buffer containing 0.5% albumin) or CaCl2 plus APC (60 nmol/L). The APC sensitivity ratio was calculated as the APTT with APC divided by the APTT without APC. APC resistance is indicated by a ratio of less than 2.2.13
To calibrate the APC concentration in the COATEST kits, 100 μL of COATEST APC plus CaCl2 reagent was added to 100 μL of chromogenic substrate S-2366. After 4 minutes, the reaction was stopped with 100 μL of 20% acetic acid, and the absorbance recorded at a wavelength of 405 nm. Results were compared with a standard curve generated with purified APC. The concentration of APC in the COATEST kits was 60 nmol/L.
A modified APTT and APC sensitivity ratio was used to determine the effect of platelets and platelet activation on APC resistance. A total of 30 μL of platelet agonist was added to 90 μL of PRP (platelet count 300 × 109/L) and the mixture was stirred for 5 minutes at 37°C in a KC-10 Coagulometer. Starting concentrations of TRAP, collagen, and calcium ionophore A23187 were 600 μmol/L, 1,000 μg/mL, and 400 μmol/L, respectively. Agonists were double diluted in PBS buffer, pH 7.4, to obtain varying concentrations necessary for dose response curves. After 5 minutes 90 μL of APTT reagent was added to each cuvette and samples incubated for a further 5 minutes with stirring. Clot formation was then initiated with 90 μL of either CaCl2 or CaCl2 plus APC.
To investigate the role of PMPs in APC resistance, 30 μL of ionophore was stirred for 5 minutes at 37°C with gel filtered platelets (300 × 109/L prepared as described above). After 5 minutes, further platelet activation was halted by the addition of 10 μg/mL prostaglandin E1. Samples were centrifuged for 5 minutes at 6,000g and 30 μL of the PMP-containing supernatant was added to 90 μL of PMP-free plasma on the KC-10. A total of 90 μL of APTT reagent was then added to each cuvette for a 5-minute stirred incubation. Clot formation was then initiated by the addition of CaCl2 or CaCl2 + APC.
Aspirin (acetylsalicylic acid) and the fibrinogen receptor (glycoprotein IIbIIIa) antagonist GR144053F were incubated with PRP at 37°C for 15 minutes without stirring. Only concentrations of drug that inhibited platelet aggregation, in a light-transmission platelet aggregometer (PAP-4; Alpha, Hants, UK) after addition of collagen, were used to determine the effect of inhibition of platelet activation in the APC sensitivity assay. An aspirin concentration (final) of 40 μmol/L and a GR144053F concentration of 60 nmol/L were used for in vitro inhibition of platelet activation.
Whole-Blood Dilute Thromboplastin Assay
Nonanticoagulated venous whole blood was obtained from healthy volunteers. The initial 3 mL of blood was discarded, and the next 1 mL was used for the assay within 2 minutes of obtaining the sample. A total of 100 μL of this sample was added to 100 μL of thromboplastin diluted 1/1,000 in imidazole buffer and 100 μL of either CaCl2 or APC + CaCl2 from the COATEST kit. The mixture was stirred at 37°C in the KC10 coagulometer and clot times measured. Volunteers were then given 600 mg of aspirin orally, and a further blood sample was obtained 1.5 hours later. The whole blood dilute thromboplastin time was measured and platelet aggregation was performed to confirm that aspirin ingestion had resulted in at least a 50% reduction of collagen-induced platelet aggregation (100 μg/mL collagen final concentration).
RESULTS
Effect of Freeze-Fractured Platelets and Phospholipid Vesicles on APC Sensitivity
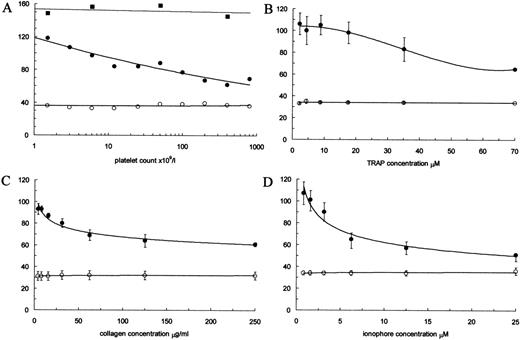
The platelet count of PRP was varied and the APTT, with and without APC, was measured before and after freeze fracturing. The APTT of fresh PRP did not vary with platelet count and was the same as that of PPP. In contrast, in the presence of freeze-fractured PRP, there was a progressive increase in APC resistance with increasing platelet count. In the absence of APC, the APTT was constant, but in the presence of APC, the APTT was progressively reduced in relation to platelet count (Fig 1A). To determine if the APC resistance was associated with the platelet membrane or was due to a soluble factor released during platelet disruption, samples of PRP were ultracentrifuged. After ultracentrifugation at 77,000g for 1 hour, the APC resistance phenotype was abolished. The APTT of the ultracentrifuged PRP (154 seconds) was longer than that of the untreated PPP (120 seconds). However, platelet microparticles were detectable in PPP samples by ELISA and not in the ultracentrifuged PRP. When PPP samples were also ultracentrifuged, microparticles were no longer detectable and the APTT was the same as that of the ultracentrifuged PRP. These results indicate that the platelet-dependent APC resistance phenotype is associated exclusively with a particulate platelet fraction rather than a soluble factor released during platelet disruption. The prolongation of the APTT after ultracentrifugation of samples indicates that normal plasma typically contains some of the platelet-derived fraction that is responsible for APC resistance.
Effect of freeze-fractured platelets and platelet activation on the APTT. In each panel, the vertical axis is the APTT in seconds in the presence of APC (•) and in the absence of APC (○). Error bars indicate standard error of the mean. In (A), the effect of freeze-fracturing is shown. In the absence of APC, the APTT was constant, but in the presence of APC, the APTT was reduced even at a platelet count of 2 × 109/L. In the example shown, the APC sensitivity ratio of PPP and fresh PRP was 3.2. This was reduced in freeze-fractured PRP to a ratio of 1.7 at a platelet count of 400 × 109/L. After ultracentrifugation at 77,000g for 1 hour, the APC resistance phenotype was abolished (▪). In (B, C, and D), the effect of platelet activation with different agonists is shown: (B) TRAP (n = 3); (C) collagen (n = 7); and (D) A23187 (n = 3).
Effect of freeze-fractured platelets and platelet activation on the APTT. In each panel, the vertical axis is the APTT in seconds in the presence of APC (•) and in the absence of APC (○). Error bars indicate standard error of the mean. In (A), the effect of freeze-fracturing is shown. In the absence of APC, the APTT was constant, but in the presence of APC, the APTT was reduced even at a platelet count of 2 × 109/L. In the example shown, the APC sensitivity ratio of PPP and fresh PRP was 3.2. This was reduced in freeze-fractured PRP to a ratio of 1.7 at a platelet count of 400 × 109/L. After ultracentrifugation at 77,000g for 1 hour, the APC resistance phenotype was abolished (▪). In (B, C, and D), the effect of platelet activation with different agonists is shown: (B) TRAP (n = 3); (C) collagen (n = 7); and (D) A23187 (n = 3).
To determine if APC resistance was simply phospholipid-dependent, the experiment was repeated with synthetic phospholipid vesicles. With the PCPS vesicle concentration varied between 0.5 μmol/L and 500 μmol/L there was no effect on the APTT with or without APC, ie, PCPS vesicles did not cause APC resistance.
Effect of Atherogenic Lipoproteins on APC Resistance
Purified lipoproteins (HDL, VLDL, LDL, and oxidized LDL) were added to microparticle free plasma and APC sensitivity ratios were determined. Maximum final concentrations in the APC resistance assay were 3,700 μg/mL for HDL, 2,400 μg/mL for VLDL, 1,000 μg/mL for LDL, and 620 μg/mL for oxidized LDL. These concentrations of VLDL and oxidized LDL were shown to support thrombin generation in the purified component thrombin generation assay, but did not affect APC sensitivity in the standard APC resistance assay. The result was therefore similar to that with PCPS vesicles.
Quantification of APC Resistance Due to Platelet Activation
The effect of platelet activation on APC sensitivity was determined after activation of platelets with TRAP, collagen, and the calcium ionophore A23187 (Fig 1B through D). Progressive APC resistance was observed at a TRAP concentration of 35 μmol/L and above, at a collagen concentration of 32 μg/mL and above, and an ionophore concentration of 6.25 μmol/L and above. The experiments were repeated using Protac to generate endogenous protein C activation within the plasma sample. The results were the same as that observed with addition of APC, with an identical pattern and degree of APC resistance with increasing platelet activation.
Quantification of APC Resistance Due to Platelet-Derived Microparticles
To determine if platelet-dependent APC resistance was associated with platelet-derived microparticles, as well as activated platelets, ultracentrifuged plasma was spiked with microparticles generated from gel-filtered platelets. The APTT of ultracentrifuged microparticle free plasma in the presence of APC was 165 seconds with an APC sensitivity ratio of 3.7. After addition of microparticles (produced from 300 × 109/L gel-filtered platelets with 1 μmol/L ionophore), this fell to 114 seconds with a ratio of 2.5. The plasma was then ultracentrifuged again at 77,000g for 1 hour. This removed all detectable microparticles and the APC resistance phenotype was abolished with the APTT returning to 165 seconds.
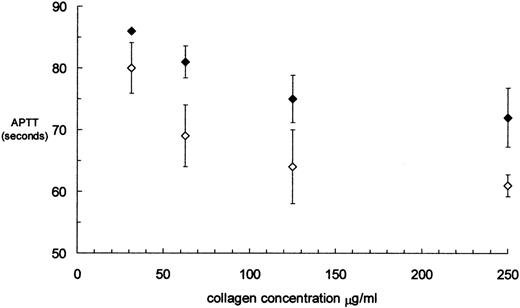
Effect of In Vitro Inhibition of Platelet Activation
Collagen-induced platelet activation was performed before and after incubation of PRP (platelet count 300 × 109/L) with aspirin and the platelet glycoprotein IIbIIIa antagonist GR144053F. Aspirin at a concentration of 40 μmol/L abolished collagen-induced platelet aggregation, but had no effect on the APTT in the presence of APC (F = 1.155, P = .288, analysis of variance [ANOVA] pairwise comparison Bonferroni test). GR144053F at a concentration of 65 nmol/L abolished collagen-induced platelet aggregation and prolonged the APTT in the presence of APC (F = 25.743,P < .001, ANOVA pairwise comparison Bonferroni test) (Fig 2).
Effect of GR144053F at a concentration of 65 nmol/L on the APTT in the presence of APC. There was a significant difference between APTTs with (⧫) and without (◊) GR144053F (F = 25.743;P < .001; ANOVA pairwise comparison).
Effect of GR144053F at a concentration of 65 nmol/L on the APTT in the presence of APC. There was a significant difference between APTTs with (⧫) and without (◊) GR144053F (F = 25.743;P < .001; ANOVA pairwise comparison).
Effect of In Vivo Inhibition of Platelet Activation With Aspirin
To determine if aspirin influenced the effect of APC on thrombin generation in vivo, a dilute thromboplastin time was measured on nonanticoagulated fresh whole blood taken from healthy volunteers before and 90 minutes after ingestion of 600 mg of aspirin. In nonanticoagulated blood, there is a slow intrinsic activation of coagulation resulting in clot formation at variable times between 15 and 20 minutes. To minimize this activation, the blood sample was taken without a tourniquet and the first 3 mL of blood was discarded. When thromboplastin at a final dilution of 1 in 1,000 was added to whole blood, the variance of the clot time was eliminated and coagulation occurred within 6 minutes with synchronization between experiments, although clot times varied with different dilutions of thromboplastin. The same clot times were observed in plasma samples when the dilute thromboplastin was added at any time up to 5 minutes after collection of the blood sample.
Ten healthy volunteers on no medication participated in the study (mean age, 36 years; range, 23 to 50, seven men). The mean clot times without APC, before and after aspirin, were 240 seconds (standard deviation [SD], 70) and 230 seconds (SD, 45), respectively. The mean clot times with APC, before and after aspirin, were 372 seconds (SD, 106) and 422 seconds (SD, 119). The difference in clot times with APC, before and after aspirin, was not significant (pairedt-test 1.437, P = .185). The mean ratio of the dilute thromboplastin time with and without APC was 1.61 (SD, 0.14) before aspirin and 1.83 (SD, 0.10) after aspirin (paired t-test 1.313,P = .222).
DISCUSSION
This study has produced several new observations. First, platelet-dependent APC resistance results from activation of platelets with a variety of platelet agonists. The responses to TRAP and collagen suggest that platelet activation in vivo is likely to produce APC resistance. Second, the degree of APC resistance resulting from platelet activation is comparable to that observed in the plasma of patients with factor V gene mutations affecting critical APC cleavage sites. This indicates that platelet-dependent thrombin generation is not susceptible to regulation by the protein C system in the same way that thrombin generation is regulated in a platelet poor environment. Third, the ultracentrifugation studies indicate that platelet-dependent APC resistance is associated exclusively with the platelet membrane. Fourth, the phenomenon is not simply due to exposure of anionic phospholipid, as APC resistance was not induced by the addition of PCPS vesicles. Fifth, while atherogenic lipoproteins supported assembly of the prothrombinase complex, they did not confer APC resistance in the APC sensitivity assay. Therefore, lipoprotein-supported thrombin generation appears to be susceptible to regulation by the protein C system. Sixth, platelet-derived microparticles confer APC resistance, although to a lesser degree than that observed on the surface of activated platelets. Seventh, inhibition of platelet activation with a fibrinogen receptor antagonist attenuated APC resistance associated with platelet activation. This indicates a direct effect of this inhibitor on platelet-dependent APC resistance. In contrast, aspirin had no effect, suggesting that any modification of platelet-dependent APC resistance by aspirin is an indirect effect due to reduced platelet localization within a developing clot or thrombus.
Previous studies performed by ourselves13 and others11,12,18 have shown that the addition of platelets into an APC-resistance assay results in a decrease in the APC sensitivity ratio. However, the effect of platelet activation with a variety of platelet agonists had not previously been examined. Camire et al14,19 recently showed that plasma and platelet factor Va represent different substrates for APC, suggesting that platelets sustain thrombin generation by releasing a factor Va molecule with an APC-resistant phenotype and possibly by providing a membrane surface that delays cofactor inactivation. In our experiments, the degree of APC resistance in the presence of TRAP or collagen was comparable to that found in the plasma of many patients who are heterozygous, and some patients who are homozygous, for the FVR506Q mutation.6,7 This suggests that platelet activation at the site of endothelial damage downregulates a critical natural anticoagulant mechanism. This effect would promote thrombin generation. In addition, fibrinolysis would be inhibited due to increased thrombin activatable fibrinolysis inhibitor (TAFI) activity.20 The combined effect would be an amplification of the hemostatic response to injury.
Delivery of platelets to an area of damaged artery is rapid with platelets aggregating over an area of damaged arteriole at a rate of 10,000 per second despite high blood flow.21 As a result, the concentration of platelet-derived factor V within a platelet-rich thrombus is increased at least 100-fold.22 In PRP plasma, the ratio of platelet-derived factor V to plasma factor V is only 1:4.23 In contrast, the ratio in a developing thrombus will be 25:1 when there is a 100-fold relative increase in platelet concentration. Therefore, the predominant source of factor Va in a developing clot or thrombus is the platelet pool of factor V. In this situation, thrombin generation is dependent on a factor Va protein with an APC-resistant phenotype. If the accumulation of activated platelets within a developing clot or thrombus is retarded, then the amount of platelet-derived factor Va will diminish and the platelet:plasma factor V ratio will be reduced. Using anticoagulated blood and flow conditions similar to those in arteries, Weiss et al24 have shown that aspirin does not reduce adhesion of platelets to denuded artery, but it reduces the percentage of adherent platelets that have platelet thrombi superimposed on them. They used blood, taken from healthy volunteers before and after ingestion of 900 mg of aspirin, in a denuded rabbit aorta model. The percentage of superimposed platelet thrombi was reduced from 20.3% to 0.1%, and the number of thrombi that reached a height of 5 μm was reduced from 16.5% to 0.1%. This observation is supported by morphologic examination of the hemostatic plug in human skin wounds after aspirin ingestion.25 This 100-fold to 200-fold decrease in platelet retention would restore the platelet:plasma factor V ratio to that found in plasma and potentially abolish the platelet-dependent APC resistance phenotype. Aspirin would therefore exert an “anticoagulant effect.” This would explain the reduction of fibrinopeptide A formation reported in a skin injury model after ingestion of aspirin.26 While an effect on platelet flip-flop would be expected to reduce thrombin generation, by limiting provision of the anionic phospholipid surface required for prothrombinase assembly, previous studies suggested that platelet flip-flop is not affected by aspirin.27-29 Our latest results suggest that the platelet-dependent APC resistance phenotype is probably influenced by aspirin through an indirect effect, with a reduction of platelet localization within a developing clot or thrombus. In contrast, the fibrinogen receptor blocker, GR144053F, reduced platelet-dependent APC resistance through a direct effect. Fibrinogen receptor blockade has previously been shown to reduce platelet-dependent thrombin generation,29 but an effect on APC resistance has not previously been shown. Our results suggest that the high potency of this type of platelet inhibitor30 is, in part, due to a direct effect on platelets with a reduction of platelet-dependent APC resistance. This suggests that “outside-in” signalling, resulting from fibrinogen receptor-ligand binding, may be required for maximum platelet membrane factor V expression, as it is for maximum platelet aggregation.31 This differential effect of antiplatelet agents requires clarification, as it may provide further insight on the mechanism of platelet activation and the effects of different antiplatelet drugs.
In this study, we have also shown that platelet-derived microparticles are responsible for APC sensitivity ratios of less than 3.0 in normal plasma samples. In the absence of microparticles, sensitivity ratios above 3.0 are observed. From analysis of factor V proteolytic cleavage patterns, Camire et al14 concluded that APC resistance was not associated with platelet-derived microparticles. Our data indicate that APC resistance is associated with microparticles, but the degree is comparatively less than that associated with activated platelets. This may reflect a difference in the amount of platelet-derived factor Va that is associated with microparticles compared with activated platelets. In the Rotterdam Study, the odds ratio for cerebrovascular disease increased with decreasing response to APC.10 This relationship between plasma APC response and cerebrovascular disease might be explained by in vivo platelet activation and the formation of microparticles, which are not removed during the preparation of plasma samples.
We have previously shown that atherogenic lipoproteins support assembly of the prothrombinase complex leading to thrombin generation.15 In this latest study, we have shown that plasma-derived lipoproteins do not confer APC resistance in the standard APC sensitivity assay. This suggests that thrombin generation on the surface of noncellular lipoproteins is susceptible to regulation by the protein C system.
In conclusion, we have shown that the platelet-dependent APC resistance phenotype is of the same degree as that observed in the plasma of patients with factor V gene mutations affecting critical APC cleavage sites. The control of thrombin generation by platelets within a developing clot or thrombus may be subject to pathologic alteration and is a target for the development of novel antithrombotic therapy. The standard APC sensitivity assay is well-characterized in patients with venous thromboembolism, and it is a simple technique that is available in most coagulation laboratories. It is now necessary to determine if quantification of the platelet-dependent APC resistance phenotype in clinical samples has predictive value for arterial thrombotic events and if and how the phenomenon is altered in vivo by antithrombotic therapy.
ACKNOWLEDGMENT
We are grateful to Alan Giles, Mike Nesheim, and John Samis of Queens University, Kingston, Ontario, for much helpful discussion and the kind gift of PCPS vesicles.
Supported in part by grants from the Addenbrooke’s Trust Endowment, the MRC, Anglia and Oxford Health Authority, and the Royal Society. C.D.B. is an MRC Clinician Scientist Fellow.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Trevor Baglin, FRCP, Department of Haematology, Box 234, Addenbrooke’s NHS Trust, Cambridge CB2 2QQ, UK; e-mail: tpb20@cus.cam.ac.uk.