To the editor:
X-linked thrombocytopenia identified by flow cytometric demonstration of defective Wiskott-Aldrich syndrome protein in lymphocytes
X-linked thrombocytopenia (XLT) is characterized by congenital thrombocytopenia with small-sized platelets and without immunodeficiency.1 XLT is an allelic variant of Wiskott Aldrich syndrome (WAS), and both entities are caused by mutations in the WAS protein (WASP) gene.2 XLT may be misdiagnosed as chronic idiopathic thrombocytopenic purpura (ITP) in which the platelets are normal-sized or enlarged. We have recently identified a 5-year-old boy with XLT who had been originally diagnosed as having chronic ITP. Deficient expression of WASP in lymphocytes from the patient was demonstrated by flow cytometric analysis using an anti-WASP monoclonal antibody (MoAb) and the diagnosis of XLT was confirmed by mutation analysis. Here we demonstrate the usefulness of flow cytometric analysis in the diagnosis of XLT.
When the patient was 1 year old, he was referred to the Toyama Red Cross Hospital for the treatment of atopic dermatitis. Thrombocytopenia (platelet count: 85 × 103/μl) was found by chance, since he had no bleeding tendency. When he was 3 years old, he developed a subcutaneous hematoma in the right inguinal region. His platelet count at that time was 52 × 103/μl and an increased level of platelet-associated IgG (99.5 ng/107platelets) was detected. He had neither neutropenia nor anemia, and his coagulation systems and immunoglobulin levels were normal. Bone marrow aspirate demonstrated increased numbers of megakaryocytes, but no abnormal cells, suggesting the diagnosis of ITP. His platelet count increased transiently following oral predonine and intravenous high-dose immunoglobulin. Because a maternal uncle (age 30 years old) had thrombocytopenic purpura since early infancy, we considered the possible diagnosis of XLT.
The demonstration of a mutation affecting the WASP gene is essential for the diagnosis of XLT.3 However, the genetic analysis is labor- and time-consuming. We have established a simple flow cytometric technique to diagnose X-linked agammaglobulinemia (XLA).4This technique has recently been adapted to analyze WASP in lymphocytes from WAS patients.5 In this report, we demonstrate the usefulness of a new anti-WASP MoAb and flow cytometry in the diagnosis of XLT. Anti-WASP MoAb 5A5 was prepared by immunizing mice with the recombinant protein encoded by the N-terminal 1.4 kilo bp obtained with the pET Trx fusion system 32 (Takara Shuzo, Kyoto, Japan). Peripheral blood mononuclear cells (PBMC) were prepared by Ficoll-Hypaque gradient centrifugation from heparinized venous blood, fixed with 4% paraformaldehyde, and permeabilized with 0.1% Triton-X in Tris-buffered saline. The cells were incubated with anti-WASP MoAb 5A5 or control IgG2a, washed twice, and incubated with FITC-conjugated goat anti-mouse IgG2a antibody (Southern Biotechnology Associates Inc, Birmingham, AL). After washing, the stained cells were analyzed with an Epics XL flow cytometer (Coulter Corporation, Miami, FL).
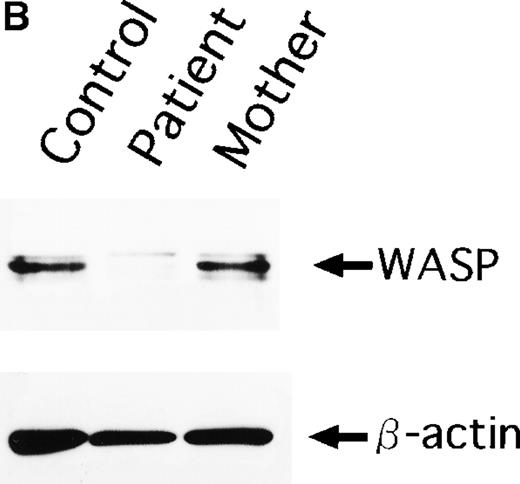
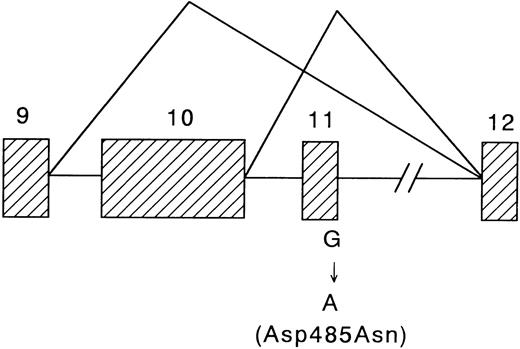
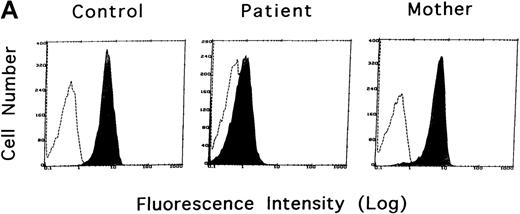
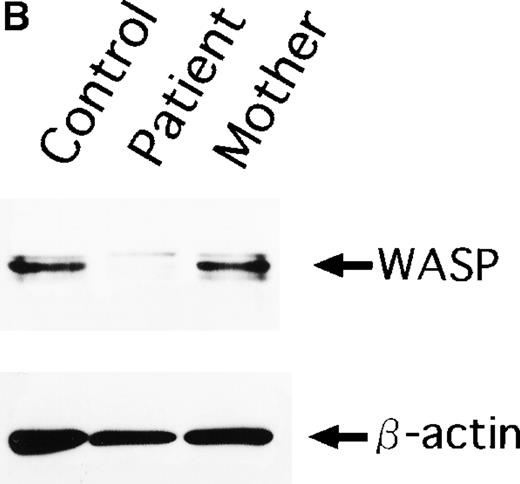
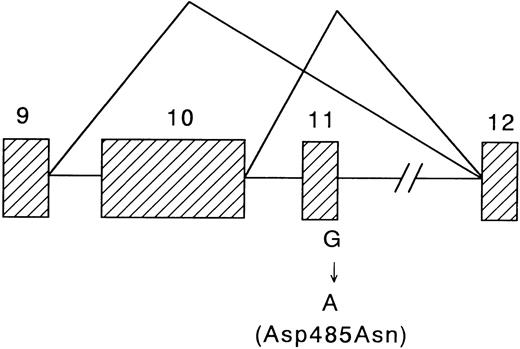
As shown in Figure 1A, deficient WASP expression in lymphocytes was demonstrable in the patient, which was in marked contrast to intense expression of WASP in lymphocytes from a healthy individual and the patient's mother. The diagnosis of XLT was confirmed by immunoblot and genetic analysis. Whole cell lysate of PBMC were subjected to immunoblot analysis using the anti-WASP MoAb 5A5. WASP protein determined as an approximately 59 kD protein was present in PBMCs from a healthy control and from the patient's mother (Figure 1B). In contrast, WASP was not detectable in the lysate of the patient's PBMC. For mutation analysis, total RNA and genomic DNA were extracted from PBMC by conventional methods, and subjected to reverse transcriptase-polymerase chain reaction (RT-PCR), as described previously.6 We found a single base substitution (G1487A) at the C-terminal end of exon 11, resulting in the skipping of exon 11 or in the skipping of both exons 10 and 11 in the major of the transcripts, and amino acid substitution (Asp485Asn) in a smaller portion of the transcript (Figure 2). His mother and sister were found to have 1 mutated and 1 normal alleles, and thus were carriers.
WASP expression in 3 subjects.
(A) Flow cytometric analysis of WASP expression in normal individual (control), XLT patient (patient), and his mother (mother). The shaded areas and the dashed line indicate the staining with anti-WASP and control antibodies, respectively. (B) A Western blot analysis of WASP protein in the lysates from the 3 subjects above. WASP and β-actin protein as internal control were determined as approximately 59 kD and 42 kD proteins, respectively.
WASP expression in 3 subjects.
(A) Flow cytometric analysis of WASP expression in normal individual (control), XLT patient (patient), and his mother (mother). The shaded areas and the dashed line indicate the staining with anti-WASP and control antibodies, respectively. (B) A Western blot analysis of WASP protein in the lysates from the 3 subjects above. WASP and β-actin protein as internal control were determined as approximately 59 kD and 42 kD proteins, respectively.
Schematic representation showing the multiple alterations in the WASP cDNA of the patient.
Exons are shown in shaded area.
Schematic representation showing the multiple alterations in the WASP cDNA of the patient.
Exons are shown in shaded area.
Flow cytometric analysis of WASP in PBMC is a simple and rapid test for the diagnosis of XLT and WAS. Although some mutations in the WASP gene may allow the expression of a normal amount of WASP in lymphocytes, the flow cytometric analysis is a useful screening test to differentiate XLT as well as WAS from chronic ITP, when the patient is male and has early childhood onset.