Differentiation of macrophages from myeloid progenitor cells depends on a discrete balance between cell growth, survival, and differentiation signals. Interleukin-3 (IL-3) supports the growth and survival of myeloid progenitor cells through the activation of Jak2 tyrosine kinase, and macrophage differentiation has been shown to be regulated by protein kinase C (PKC). During terminal differentiation of macrophages, the cells lose their mitogenic response to IL-3 and undergo growth arrest, but the underlying signaling mechanisms have remained elusive. Here we show that in IL-3–dependent 32D myeloid progenitor cells, the differentiation-inducing PKC isoforms PKC- and PKC-δ specifically caused rapid inhibition of IL-3–induced tyrosine phosphorylation. The target for this inhibition was Jak2, and the activation of PKC by 12-O-tetradecanoyl-phorbol-13-acetate treatment also abrogated IL-3–induced tyrosine phosphorylation of Jak2 in Ba/F3 cells. The mechanism of this regulation was investigated in 32D and COS7 cells, and the inhibition of Jak2 required catalytic activity of PKC-δ and involved the phosphorylation of Jak2 on serine and threonine residues by the associated PKC-δ. Furthermore, PKC-δ inhibited the in vitro catalytic activity of Jak2, indicating that Jak2 was a direct target for PKC-δ. In 32D cells, the inhibition of Jak2 either by PKC-δ, tyrosine kinase inhibitor AG490, or IL-3 deprivation caused a similar growth arrest. Reversal of PKC-δ–mediated inhibition by the overexpression of Jak2 promoted apoptosis in differentiating 32D cells. These results demonstrate a PKC-mediated negative regulatory mechanism of cytokine signaling and Jak2, and they suggest that it serves to integrate growth-promoting and differentiation signals during macrophage differentiation.
Homeostasis during hematopoiesis requires precise coordination of cell proliferation and differentiation, and these events are critically regulated by the network of numerous hematopoietic cytokines.1 Hematopoietic cytokine receptors are structurally and functionally related, and activation of cytoplasmic Jak tyrosine kinases appears to be the triggering event in cytokine receptor intracellular signaling, leading to the activation of several signaling pathways involving signaling proteins such as Stat transcription factors, Shc, extracellular signal-regulated kinases (ERK), phosphatidylinositol 3-kinase, Akt, and phospholipase C-γ (PLC-γ).2 However, appropriate biologic responses are dependent on the tight regulation of the activation signals. Recently, cytokine receptor signaling has been found to be subject to negative regulation by several means. Jaks are down-modulated by SOCS/SSI/JAB proteins,3-5 Stats are down-modulated by association with PIAS proteins and by proteolytic degradation,6,7 and both Jaks and Stats are negatively regulated by tyrosine phosphatases.8,9 Cross-talk between different signaling pathways provides important diversity to the biologic responses of cytokines, and activation of certain cell-surface receptors10-13 and cellular signaling pathways involving protein kinase A, protein kinase C (PKC), calcium flux, and ERK kinases13-17 have also been found to inhibit cytokine receptor signaling.
Macrophages play a central role in orchestrating immune and inflammatory responses, and considerable progress has been made toward understanding the mechanisms of macrophage differentiation. Interleukin-3 (IL-3) is a growth and survival factor for immature myeloid progenitor cells that exerts its biologic activities through a heterodimeric IL-3 receptor (IL-3R) composed of α and β subunits.2 IL-3 binding to the receptor activates the IL-3Rβ–associated Jak2 tyrosine kinase, which is essential for the activation of several downstream signaling cascades regulating proliferation and survival of myeloid progenitor cells.2,18-20 Growth and differentiation of committed myeloid progenitor cells is regulated by granulocyte-macrophage colony-stimulating factor,1 but the physiologic factors that mediate terminal differentiation of macrophages are less clearly defined. However, the differentiation is known to be induced by PKC.21-23 PKC is activated by various stimuli, including receptor tyrosine kinases such as the macrophage colony-stimulating factor (M-CSF) receptor, which has been shown to induce in vitro and in vivo macrophage differentiation through the activation of PLC-γ2 and PKC.1,21,24-26 The PKC family of Ser/Thr kinases comprises at least 11 isoforms that differ in their activation mechanisms, expression patterns, and cellular functions.27 Three of the PKC isoforms, PKC-α, PKC-β, and PKC-δ, have been implicated in the induction of monocytic differentiation in cell lines or in normal progenitor cells.20-23
Induction of macrophage differentiation by the PKC-activator phorbol ester 12-O-tetradecanoyl-phorbol-13-acetate (TPA) or M-CSF results in the inhibition of IL-3–mediated proliferation.22,28,29 Subsequently, cells undergo morphologic and functional maturation, but the underlying molecular mechanisms are still largely unknown. Macrophage differentiation is associated with the modulation of several proteins that participate in the regulation of cell-cycle progression, and it involves the down-regulation of c-myc and the induction of cyclin-dependent kinase inhibitors.30,31 Interestingly, IL-3 stimulation results in the opposite regulation of these proteins, ie, the induction of c-myc and the inhibition of cyclin inhibitors.32,33 These findings prompted us to investigate whether the PKC-mediated macrophage differentiation and cell-cycle arrest involved the regulation of IL-3R signaling. As a model we used the IL-3–dependent, immature myeloid cell line 32D that is derived from normal murine bone marrow and is nontumorigenic.34 32D cells do not differentiate in response to TPA, and they express only low endogenous levels of PKC-α, PKC-δ, and PKC-η, thereby providing a useful model to study the isoform-specific functions of PKC in myeloid progenitor cells.22 Ectopic expression of PKC-α or PKC-δ, but not other PKC isoforms, renders 32D cells responsive to receptor tyrosine kinase and TPA-induced macrophage differentiation.22 35 In this report we demonstrate that the activation of PKC-α and PKC-δ caused rapid inhibition of IL-3 signaling through the abrogation of Jak2 activation and that this inhibition was accompanied by growth arrest in 32D cells.
Materials and methods
Cell culture, DNA constructs, and transfections
32Dcl3 cells expressing PKC-α, PKC-δ, and PKC-ε isoforms have been described previously.22,36 Ba/F3 cells were a kind gift from Dr M. Heim. The cDNA constructs for different PKC isoforms and HA-epitope–tagged Jak2, Stat1, and Stat5a have been described previously.22,37 38 All transfections were carried out by electroporation. For Jak2 overexpression, parental and 32D-δ cells were transfected with wild-type Jak2 in pBabe-Puro expression vector. Twenty-four hours after electroporation, 2.5 μg/mL puromycin was added to the cells, and after 2 weeks, growing cells were dilution cloned. The Jak2 expression of different clones was analyzed by Western blotting from total cell lysates.
Immunoprecipitation and Western blotting
If not otherwise stated, cells were starved for 18 hours (0.5% fetal calf serum [FCS]), pretreated with 100 ng/mL TPA or vehicle alone for 30 minutes, and stimulated with 10 ng/mL IL-3 for 15 minutes. For immunoprecipitation, cells were lysed in Triton lysis buffer (50 mmol/L Tris-HCl, pH 7.5, 10% glycerol, 150 mmol/L NaCl, 1 mmol/L EDTA, 1% Tritonx100, 50 mmol/L NaF, and 1 mmol/L Na3VO4) supplemented with protease inhibitors or in 1% NP40 lysis buffer (as Triton lysis buffer but with Nonidet P40 as detergent) for coimmunoprecipitation studies. Immunoprecipitations were carried out as previously described,37 and immunodetection was performed with the ECL system (Amersham Pharmacia Biotech, Buckinghamshire, UK). The antibodies used were anti-phosphotyrosine-antibody (clone 4G10; Upstate Biotechnology, Lake Placid, NY), polyclonal anti-Jak2 antibody18 (kind gift from Dr Ihle), polyclonal anti–PKC-δ, -α, -ε, or -ζ (Gibco BRL Life Technologies, Gaithersburg, MD), and anti–IL-3Rβ (Transduction Laboratories, Lexington, KY). Anti-influenza virus hemagglutinin (HA)-epitope antibody (clone 12CA5) was purchased from Berkeley Antibody (Richmond, CA).
Electrophoretic mobility shift assay
Cell lysates were prepared in WCE lysis buffer as previously described,37 and the lysates were analyzed using γ-32P ATP-labeled GAS oligonucleotide from the murine IRF-1 gene 5′-CTAGAGCCTGATTTCCCCGAAATGATGAG-3′. The reactions were separated in 4.5% TBE-PAGE (2.2 × TBE) followed by autoradiography.
Protein kinase assays and phospho-amino acid analysis
Jak2 substrate kinase assay was performed from immunoprecipitated proteins as described using synthetic peptide corresponding to the tyrosine phosphorylation site of Stat1 (GPKGTGYIKTELISVS).38 For PKC-δ kinase assay, the immunocomplexes were suspended in kinase reaction buffer (0.04 mg/mL phosphatidyl-L-serine, 10% glycerol, 0.1 mmol/L CaCl2, 0.02% Triton-X-100, 10 mmol/L MgCl2, 20 mmol/L HEPES, pH7.4) in the presence of γ-ATP (0.25 μCi/mL), and the reaction was allowed to proceed for 30 minutes at 30°C. The proteins were resolved in SDS-PAGE, and the gels were vacuum dried and exposed for autoradiography. Phospho-amino acid analysis was performed according to standard procedures using 2-dimensional thin-layer electrophoresis.39
Thymidine incorporation and apoptosis assays
Growing cells were washed twice and stimulated as indicated, and 18 hours later 3H-thymidine was added to the cultures for 6 hours (1 μCi/well), after which the cells were harvested. Apoptotic cells were detected by analyzing DNA fragmentation. The TUNEL assay was performed using the In Situ Cell Death Detection Kit (Boehringer Mannheim, Mannheim, Germany) according to the manufacturer's instructions. Alternatively, fragmented DNA was isolated from cells, electrophoresed in 2% agarose gels, and stained with ethidium bromide.
Results
PKC- and PKC-δ inhibit IL-3–induced tyrosine phosphorylation in 32D cells
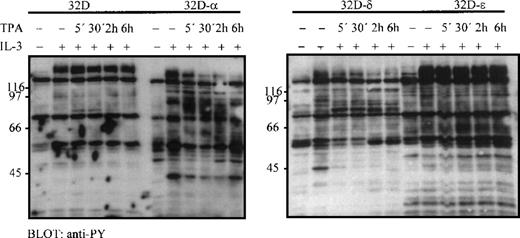
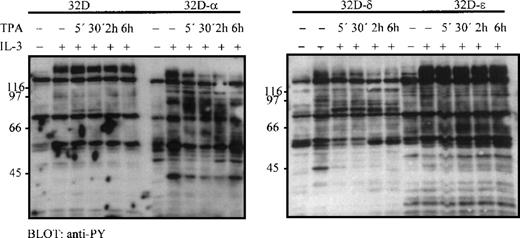
Treatment of 32D cells stably expressing PKC-α and PKC-δ (32D-α and 32D-δb, respectively) with TPA induces macrophage differentiation and cessation of cell proliferation.22 To investigate whether the differentiation-induced changes in 32D cells involved regulation of IL-3 signaling, the effect of PKC activation on cellular protein tyrosine phosphorylation was studied in 32D cell lines stably expressing different PKC isoforms.22Cells were treated with TPA for the indicated times before IL-3 stimulation. In parental (32D-wt) or in 32D-ε cells (32D cells expressing PKC-ε), TPA treatment did not affect the IL-3–induced tyrosine phosphorylation, whereas in 32D-α and 32D-δ cells, a marked inhibition in tyrosine phosphorylation was observed, particularly among the high molecular weight proteins (130-140 kd) (Figure 1). The inhibition was already evident after 5 minutes of TPA treatment and lasted for at least 6 hours. In 32D-δ cells, TPA also induced tyrosine phosphorylation of the 78-kd PKC-δ as previously reported.36
PKC- and PKC-δ inhibit IL-3–induced cellular tyrosine phosphorylation.
32D-wt, 32D-αb 32D-δ, and 32D-ε cells were starved for 18 hours (0.5% FCS), pretreated with TPA (100 ng/mL) for the indicated times, and stimulated with IL-3 (10 ng/mL) for 15 minutes. 25 μg total cellular protein was loaded on each lane, and tyrosine phosphorylation was detected by immunoblotting.
PKC- and PKC-δ inhibit IL-3–induced cellular tyrosine phosphorylation.
32D-wt, 32D-αb 32D-δ, and 32D-ε cells were starved for 18 hours (0.5% FCS), pretreated with TPA (100 ng/mL) for the indicated times, and stimulated with IL-3 (10 ng/mL) for 15 minutes. 25 μg total cellular protein was loaded on each lane, and tyrosine phosphorylation was detected by immunoblotting.
Inhibition of Jak2 tyrosine phosphorylation by PKC- and PKC-δ
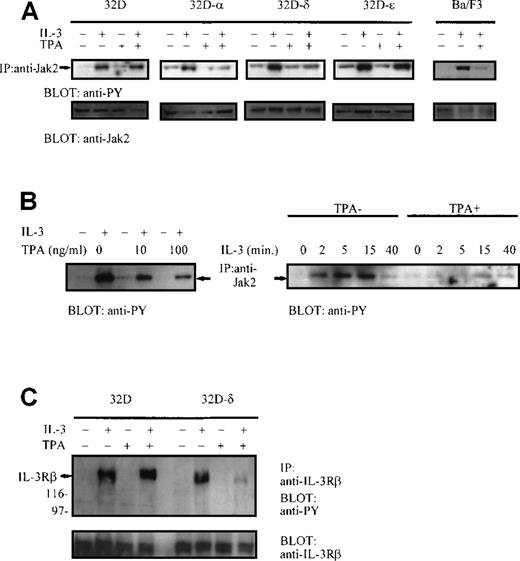
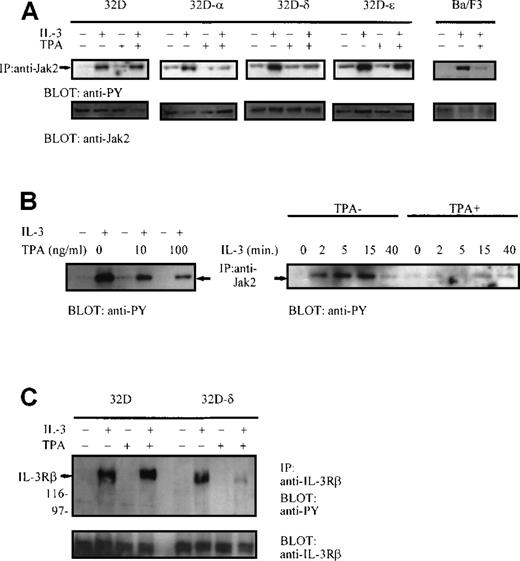
Two critical IL-3 signaling proteins, Jak2 and IL-3Rβ, are rapidly tyrosine phosphorylated on IL-3 treatment, and they migrate at approximately 130-140 kd; therefore, they were chosen as targets for further investigation. Jak2 was efficiently tyrosine phosphorylated in all 32D-derived cell lines after IL-3 stimulation, but TPA treatment inhibited tyrosine phosphorylation of Jak2 in 32D-α and in 32D-δ cells (Figure 2A). The TPA-dependent inhibition of Jak2 was analyzed in 2 independent 32D-δ clones with identical results (data not shown). In contrast, TPA stimulation had no effect on tyrosine phosphorylation of Jak2 in 32D-wt or in 32D-ε cells (Figure 2A). To verify that the observed inhibition of Jak2 was not a unique feature of 32D cells, the effect of TPA treatment on activation of Jak2 was investigated in the IL-3–dependent Ba/F3 cell line. In Ba/F3 cells, TPA-induced activation of endogenous PKC led to the abrogation of Jak2 tyrosine phosphorylation and the inhibition of IL-3–induced thymidine incorporation (Figure 2A; data not shown). The predominantly activated PKC isoform in Ba/F3 cells was PKC-α (data not shown). The PKC-mediated inhibition of Jak2 was studied in more detail in 32D-δ cells, and the inhibition was found to be TPA-concentration dependent and was not caused by the altered kinetics of Jak2 activation (Figure 2B). This differed from the previously demonstrated SHP-1 tyrosine phosphatase-mediated inhibition of Jak2, which primarily affects the kinetics of Jak2 activation.8 Taken together, these results indicate that PKC-α and PKC-δ can mediate the rapid inhibition of Jak2 in hematopoietic cells.
(A) PKC- and PKC-δ inhibit IL-3–induced tyrosine phosphorylation of Jak2.
32D-wt, 32D-α, 32D-δ, and 32D-ε cells, and Ba/F3 cells were pretreated with vehicle alone or with 100 ng/mL TPA for 30 minutes and then stimulated with IL-3 (10 ng/mL) for 15 minutes, as indicated. Jak2 was immunoprecipitated and subjected to anti-phosphotyrosine and anti-Jak2 immunoblotting. (B) The effect of TPA concentration (left panel) and kinetics (right panel) on Jak2 tyrosine phosphorylation in 32D-δ cells. 32D-δ cells were treated with vehicle alone or with TPA (30 minutes) before IL-3 stimulation, and Jak2 was immunoprecipitated and subjected to anti-phosphotyrosine immunoblotting. (C) PKC-δ inhibits IL-3–induced tyrosine phosphorylation of IL-3Rβ. 32D-wt and 32D-δ cells were treated with TPA (30 minutes) and IL-3 (15 minutes), as indicated. IL-3Rβ was immunoprecipitated and immunoblotted with anti-phosphotyrosine antibody and reprobed with anti–IL-3Rβ antibody.
(A) PKC- and PKC-δ inhibit IL-3–induced tyrosine phosphorylation of Jak2.
32D-wt, 32D-α, 32D-δ, and 32D-ε cells, and Ba/F3 cells were pretreated with vehicle alone or with 100 ng/mL TPA for 30 minutes and then stimulated with IL-3 (10 ng/mL) for 15 minutes, as indicated. Jak2 was immunoprecipitated and subjected to anti-phosphotyrosine and anti-Jak2 immunoblotting. (B) The effect of TPA concentration (left panel) and kinetics (right panel) on Jak2 tyrosine phosphorylation in 32D-δ cells. 32D-δ cells were treated with vehicle alone or with TPA (30 minutes) before IL-3 stimulation, and Jak2 was immunoprecipitated and subjected to anti-phosphotyrosine immunoblotting. (C) PKC-δ inhibits IL-3–induced tyrosine phosphorylation of IL-3Rβ. 32D-wt and 32D-δ cells were treated with TPA (30 minutes) and IL-3 (15 minutes), as indicated. IL-3Rβ was immunoprecipitated and immunoblotted with anti-phosphotyrosine antibody and reprobed with anti–IL-3Rβ antibody.
Another potential target for the PKC-mediated inhibitory effect was IL-3Rβ. Tyrosine phosphorylation of IL-3Rβ was investigated from immunoprecipitated proteins in 32D-wt and in 32D-δ cells. IL-3 stimulation resulted in rapid phosphorylation of IL-3Rβ, which was strongly inhibited on TPA treatment in 32D-δ cells but not in parental cells (Figure 2C). IL-3Rβ expression levels remained unchanged, and the mobility of the IL-3Rβ in SDS-PAGE was unaffected by TPA treatment, thus suggesting that the reduction in tyrosine phosphorylation resulted from the inhibition of Jak2 and not from the shedding or degradation of the receptor.
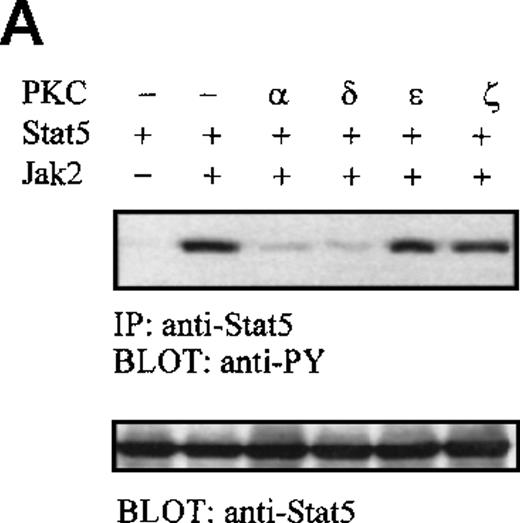
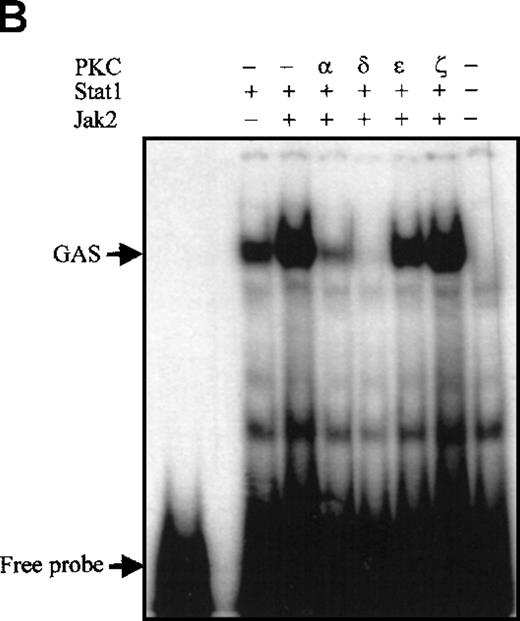
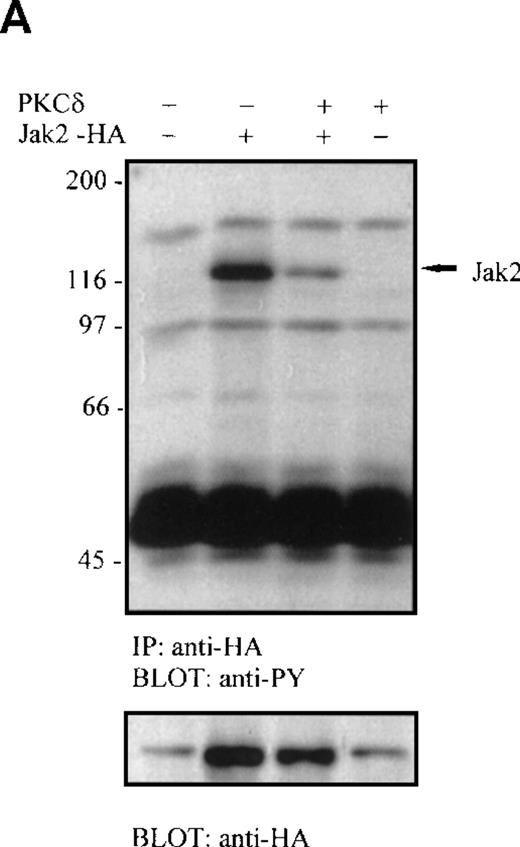
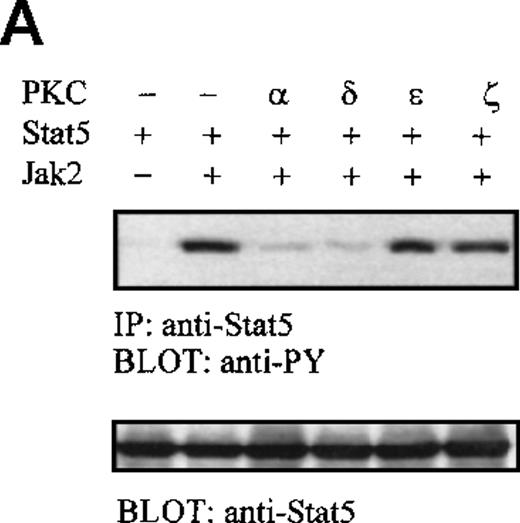
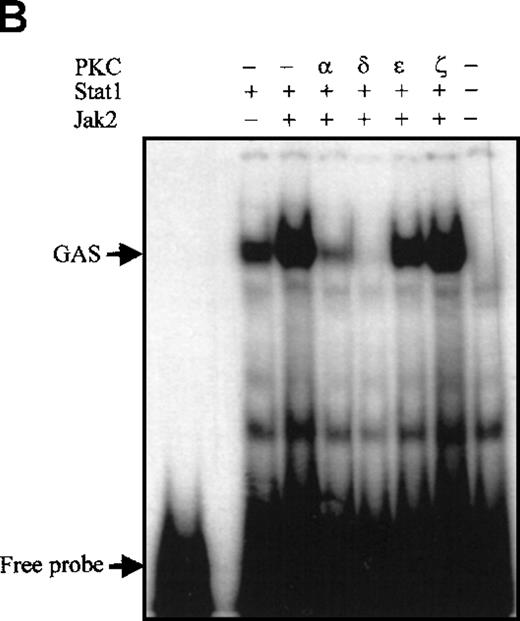
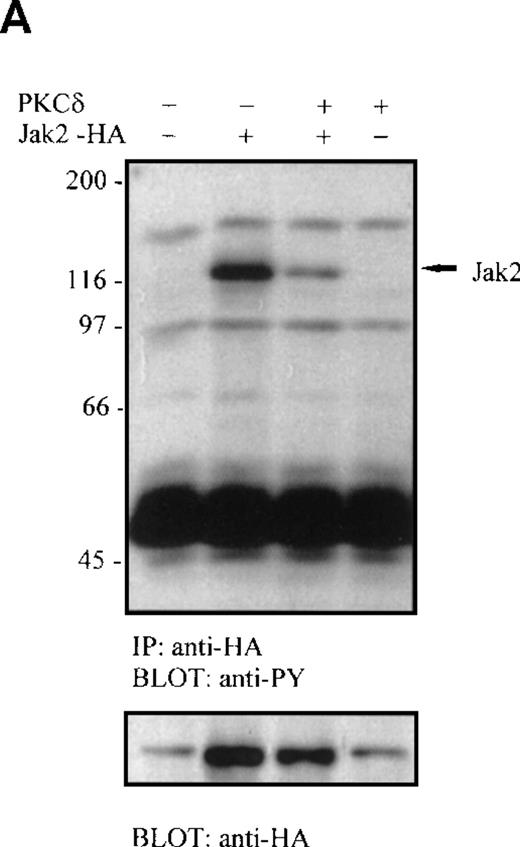
PKC-δ inhibits the catalytic activity of Jak2
Protein kinase C is known to regulate several cellular signaling pathways, and at least 2 possible mechanisms for PKC-mediated inhibition of Jak2 can be envisaged: PKC could activate tyrosine phophatase(s)8,16 or it could induce Ser/Thr phosphorylation of Jak2, either directly or through the activation of other kinase(s), such as the MEK-ERK pathway. Pretreatment of 32D-δ cells with either tyrosine phosphatase inhibitor Na3VO4 (1 mmol/L, 30 minutes) or with the MEK inhibitor PD09805950 (μmol/L, 30 minutes) did not reverse the TPA-dependent inhibition of Jak2 activation in response to IL-3 (data not shown). To investigate whether Jak2 is the primary target for PKC-mediated inhibition of IL-3 signaling, Jak2 was activated independently of the receptor by overexpression in COS7 cells. Coexpression of either PKC-α, -δ, -ε, or -ζ with Jak2 and Stat5 revealed striking specificity of PKC isoforms in the inhibition of Jak2. In accordance with the results obtained in 32D cells, only PKC-α and PKC-δ could inhibit the in vivo catalytic activity of Jak2 as measured by Jak2-induced tyrosine phosphorylation of Stat5 (Figure 3A). A similar degree of overexpression of the PKC isoforms was verified by immunoblotting from cell lysates (data not shown). PKC-α and PKC-δ also inhibited the Jak2-induced functional activation of Stat1 in electrophoretic mobility shift assay (Figure 3B). Coexpression of Jak2 with PKC-δ in COS7 cells resulted in the inhibition of Jak2 tyrosine phosphorylation (Figure 4A). Further proof for a direct PKC-mediated inhibition of Jak2 was obtained from in vitro kinase reactions. COS7 cells were transfected with either Jak2 alone or together with PKC-δ or PKC-ζ, and Jak2 was immunoprecipitated and subjected to in vitro substrate kinase reaction. Coexpression of PKC-δ resulted in the inhibition of the catalytic activity of Jak2, whereas PKC-ζ did not reduce Jak2 activity (Figure 4B). Collectively, these results indicated that Jak2 is the target for the PKC-δ–mediated inhibition of cytokine signaling.
Specificity of PKC isoforms on inhibition of Jak2.
(A) Jak2-induced tyrosine phosphorylation of Stat5 is specifically inhibited by PKC-α and PKC-δ. COS7 cells were transfected with Stat5a, Jak2, and equal amounts of different PKC isoform expression plasmids, as indicated. Forty-eight hours after transfection, the cells were lysed and Stat5a was immunoprecipitated and subjected to anti-phosphotyrosine and anti-Stat5a immunoblotting. (B) COS7 cells were transfected with Stat1, Jak2, and equal amounts of different PKC isoform expression plasmids, as indicated. After 48 hours the cells were lysed for electrophoretic mobility shift assay. 8 μg protein from each lysate was incubated with 32P-labeled GAS oligonucleotide and separated on 4.5% TBE-PAGE, followed by autoradiography.
Specificity of PKC isoforms on inhibition of Jak2.
(A) Jak2-induced tyrosine phosphorylation of Stat5 is specifically inhibited by PKC-α and PKC-δ. COS7 cells were transfected with Stat5a, Jak2, and equal amounts of different PKC isoform expression plasmids, as indicated. Forty-eight hours after transfection, the cells were lysed and Stat5a was immunoprecipitated and subjected to anti-phosphotyrosine and anti-Stat5a immunoblotting. (B) COS7 cells were transfected with Stat1, Jak2, and equal amounts of different PKC isoform expression plasmids, as indicated. After 48 hours the cells were lysed for electrophoretic mobility shift assay. 8 μg protein from each lysate was incubated with 32P-labeled GAS oligonucleotide and separated on 4.5% TBE-PAGE, followed by autoradiography.
Tyrosine phosphorylation and kinase activity of Jak2 are inhibited by PKC-δ.
(A) COS7 cells were transfected with HA-tagged Jak2 and PKC-δ expression plasmids, as indicated. Jak2 was immunoprecipitated with anti-HA antibody and subjected to anti-phosphotyrosine and subsequently anti-HA immunoblotting. (B) COS7 cells were transfected with Jak2, PKC-δ, and PKC-ζ expression plasmids, as indicated. Jak2 was immunoprecipitated and subjected to in vitro kinase assay using Stat1 tyrosine phosphorylation-site peptide as substrate. The reactions were separated on 20% SDS-PAGE, followed by autoradiography.
Tyrosine phosphorylation and kinase activity of Jak2 are inhibited by PKC-δ.
(A) COS7 cells were transfected with HA-tagged Jak2 and PKC-δ expression plasmids, as indicated. Jak2 was immunoprecipitated with anti-HA antibody and subjected to anti-phosphotyrosine and subsequently anti-HA immunoblotting. (B) COS7 cells were transfected with Jak2, PKC-δ, and PKC-ζ expression plasmids, as indicated. Jak2 was immunoprecipitated and subjected to in vitro kinase assay using Stat1 tyrosine phosphorylation-site peptide as substrate. The reactions were separated on 20% SDS-PAGE, followed by autoradiography.
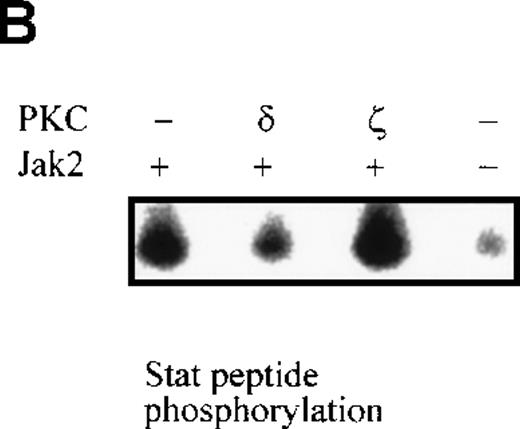
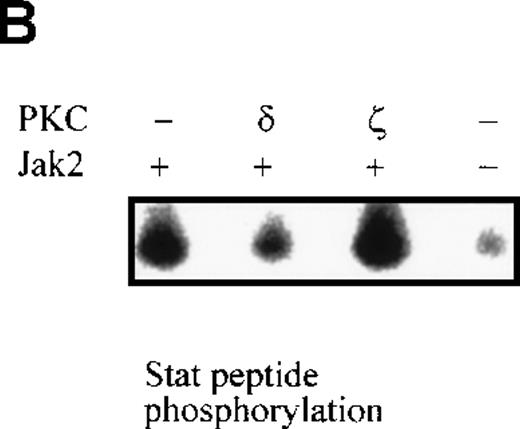
Jak2 is phosphorylated by PKC-δ on serine/threonine residues
The role of the catalytic activity of PKC in inhibition of Jak2 was studied in 32D cells constitutively expressing a kinase-inactive mutant of PKC-δ.36 In these cells, TPA treatment did not inhibit IL-3–induced tyrosine phosphorylation of Jak2, suggesting that the inhibition of Jak2 required PKC-δ–mediated phosphorylation (Figure5A). Identical results were obtained with 2 independent 32D clones expressing kinase-inactive PKC-δ (data not shown). To investigate whether Jak2 was a substrate for PKC, COS7 cells were transfected with HA-tagged Jak2 either alone or together with PKC-δ or PKC-ε, and the immunoprecipitated Jak2 was subjected to in vitro kinase assay under conditions that support the catalytic activity of PKC but not Jak2. In this assay, only Jak2, which was purified from PKC-δ–expressing cells but not from PKC-ε cells, became phosphorylated (Figure 5B). Phosphorylation of Jak2 by PKC-δ indicated a direct interaction between the proteins, and, in support of this notion, PKC-δ was found to coimmunoprecipitate with the HA-tagged Jak2 (Figure 5C). The band corresponding to the phosphorylated Jak2 was excised from the gel, and phospho-amino acid analysis demonstrated that Jak2 was phosphorylated by PKC-δ on both serine and threonine residues but not on tyrosine residues (Figure 5C).
Phosphorylation of Jak2 by PKC-δ.
(A) IL-3–induced tyrosine phosphorylation of Jak2 in 32D-wt (left), 32D-δ (middle), and 32D cells expressing kinase-negative (KN) PKC-δ (right). Cells were treated with TPA and IL-3, as indicated. Jak2 was immunoprecipitated and subjected to anti-phosphotyrosine blotting. (B) Phosphorylation of Jak2 by PKC-δ. COS7 cells were transfected with HA-tagged Jak2 and PKC-δ and PKC-ε expression constructs as indicated, and Jak2 was immunoprecipitated with anti-HA antibody. The immunocomplexes were subjected to PKC kinase assay and resolved by SDS-PAGE before autoradiography. Expression of Jak2 was analyzed by anti-HA immunoblotting. (C) Cellular complex formation between PKC-δ and Jak2. HA-tagged Jak2 and PKC-δ were transfected to COS7 cells, as indicated. Cells were lysed in 1% NP40 lysis buffer. Jak2 was immunoprecipitated with anti-HA antibody, subjected to PKC kinase assay, and resolved by SDS-PAGE. Jak2, PKC-δ, and immunoglobulin-heavy chain are indicated by arrows. The band corresponding to PKC-δ–phosphorylated Jak2 protein was extracted from gel and subjected to phospho-amino acid analysis using 2-dimensional thin-layer electrophoresis.
Phosphorylation of Jak2 by PKC-δ.
(A) IL-3–induced tyrosine phosphorylation of Jak2 in 32D-wt (left), 32D-δ (middle), and 32D cells expressing kinase-negative (KN) PKC-δ (right). Cells were treated with TPA and IL-3, as indicated. Jak2 was immunoprecipitated and subjected to anti-phosphotyrosine blotting. (B) Phosphorylation of Jak2 by PKC-δ. COS7 cells were transfected with HA-tagged Jak2 and PKC-δ and PKC-ε expression constructs as indicated, and Jak2 was immunoprecipitated with anti-HA antibody. The immunocomplexes were subjected to PKC kinase assay and resolved by SDS-PAGE before autoradiography. Expression of Jak2 was analyzed by anti-HA immunoblotting. (C) Cellular complex formation between PKC-δ and Jak2. HA-tagged Jak2 and PKC-δ were transfected to COS7 cells, as indicated. Cells were lysed in 1% NP40 lysis buffer. Jak2 was immunoprecipitated with anti-HA antibody, subjected to PKC kinase assay, and resolved by SDS-PAGE. Jak2, PKC-δ, and immunoglobulin-heavy chain are indicated by arrows. The band corresponding to PKC-δ–phosphorylated Jak2 protein was extracted from gel and subjected to phospho-amino acid analysis using 2-dimensional thin-layer electrophoresis.
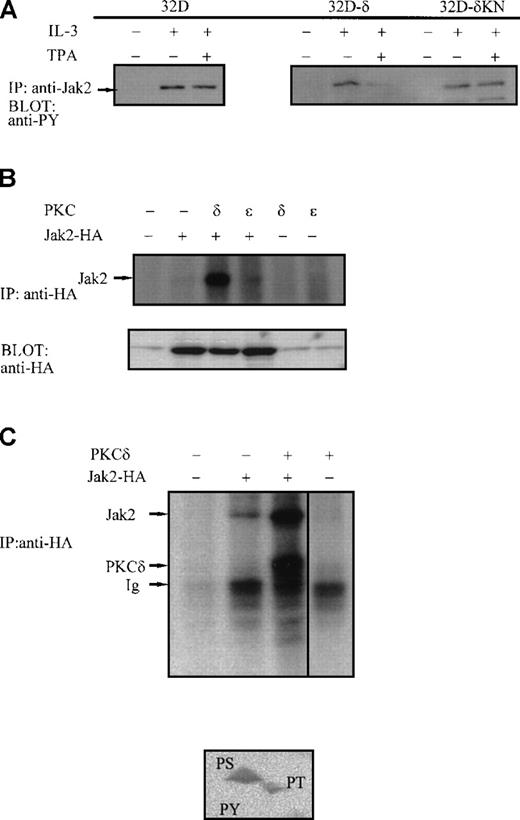
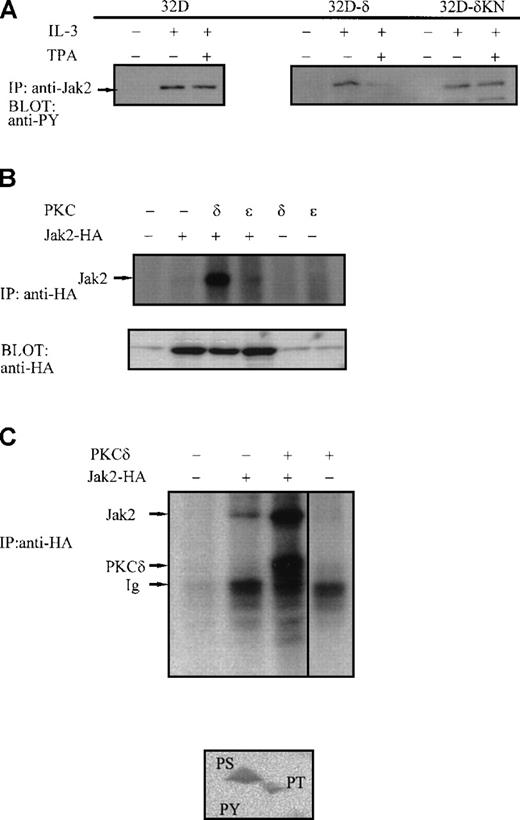
Inhibition of Jak2 is associated with growth arrest in differentiating 32D cells
To investigate the in vivo significance of Jak2 inhibition during macrophage differentiation, we wanted to revert the inhibitory effect of PKC by stably overexpressing Jak2 in 32D-δ cells (32D-δ–Jak2). In those cells, overexpression of Jak2 resulted in increased IL-3–dependent tyrosine phosphorylation of Jak2 and subsequently diminished PKC-δ–mediated inhibition compared with 32D-δ cells (Figure 6A). In thymidine incorporation assay, overexpression of Jak2 doubled the IL-3–induced increase in DNA synthesis (Figure 6B). As predicted, TPA treatment inhibited DNA synthesis only in PKC-δ–expressing cells but not in parental 32D cells. By contrast, the tyrosine kinase inhibitor AG490, which has been shown to inhibit various Jak kinases, inhibited cell proliferation both in parental and in 32D-δ cells. Furthermore, TPA-treated 32D-δ cells, like the IL-3 starved or the AG490-treated cells, similarly arrested in the G1 phase of the cell cycle, thus supporting the notion that Jak2-induced cell-cycle progression signal were abrogated by PKC-δ (data not shown). TPA induced early morphologic differentiation in 32D-δ and 32D-δ–Jak2 cells, but the sustained activation of Jak2 in differentiating 32D-δ–Jak2 cells promoted apoptotic cell death, as shown by the TUNEL analysis (Figure 6C). The overexpression of either Jak2 or PKC-δ did not cause apoptosis because the apoptotic DNA ladder was observed only in TPA-treated 32D-δ–Jak2 cells but not in similarly treated parental 32D cells overexpressing Jak2 at a comparable level or in 32D-δ cells (data not shown). This result was confirmed using several independent cell clones. Together these results suggested that the inhibition of Jak2 activity serves as an important mechanism for cell-cycle arrest during macrophage differentiation of IL-3–dependent 32D progenitor cells.
Inhibition of Jak2 is associated with growth arrest during differentiation of 32D-δ cells.
(A) Tyrosine phosphorylation of Jak2 in 32D-δ and 32D-δ–Jak2 cells. Cells were treated with TPA and IL-3, as indicated, and Jak2 was immunoprecipitated and subjected to anti-phosphotyrosine immunoblotting. Upper panel shows Jak2 protein levels. (B) Effect of Jak2 overexpression on IL-3 induced proliferation of 32D cells. Growing cells were washed twice and treated as indicated (AG490, 100 μmol/L, TPA 100 ng/mL). After 18 hours 3H-thymidine was added to the cultures for 6 hours, after which the cells were harvested. (C) TPA-induced differentiation and apoptosis in different derivatives of 32D cells. The microphotographs were taken from cells cultured for 24 hours in 2% FCS + IL-3 in the absence (left) or presence (right) of TPA (100 ng/mL). Insets show TUNEL staining of cells grown under identical conditions on coverslips.
Inhibition of Jak2 is associated with growth arrest during differentiation of 32D-δ cells.
(A) Tyrosine phosphorylation of Jak2 in 32D-δ and 32D-δ–Jak2 cells. Cells were treated with TPA and IL-3, as indicated, and Jak2 was immunoprecipitated and subjected to anti-phosphotyrosine immunoblotting. Upper panel shows Jak2 protein levels. (B) Effect of Jak2 overexpression on IL-3 induced proliferation of 32D cells. Growing cells were washed twice and treated as indicated (AG490, 100 μmol/L, TPA 100 ng/mL). After 18 hours 3H-thymidine was added to the cultures for 6 hours, after which the cells were harvested. (C) TPA-induced differentiation and apoptosis in different derivatives of 32D cells. The microphotographs were taken from cells cultured for 24 hours in 2% FCS + IL-3 in the absence (left) or presence (right) of TPA (100 ng/mL). Insets show TUNEL staining of cells grown under identical conditions on coverslips.
Discussion
Development and maintenance of hematopoietic cells require coordinated regulation of cytokine signaling. Terminal differentiation of macrophages is accompanied by the cessation of cytokine-dependent cell growth, which is likely to be important for the successful accomplishment of the differentiation program.40 In cytokine-dependent progenitor cells, growth arrest could potentially involve the inhibition of cytokine receptor mitogenic signaling. The current study was aimed at characterizing the IL-3R signaling events during terminal differentiation of macrophages induced by PKC activation. Biologic responses to PKC activation are regulated by the differential expression of various PKC isoforms and by their functional specificities.27 In support of this notion we found that 2 PKC isoforms, PKC-α and PKC-δ, specifically inhibited the activation of Jak2. The PKC-α and PKC-δ isoforms mediate macrophage differentiation and growth inhibition of myeloid progenitor cells,21,22 and in 32D cells the differentiation-inducing PKC isoforms caused a rapid inhibition of IL-3R–induced activation of Jak2 that was closely correlated with growth arrest. The inhibition was not cell-type dependent, and the activation of endogenous PKC in Ba/F3 cells inhibited IL-3–stimulated activation of Jak2. During macrophage differentiation, the M-CSF receptor has been shown to inhibit IL-3 growth signal through a PLC-γ2–dependent mechanism.26,28 29 In light of our current results, the PKC-mediated inhibition of Jak2 could serve as a molecular mechanism for this response.
Our results indicated that PKC-α and PKC-δ isoforms displayed significant specificity for the inhibition of Jak2, and the inhibition involved direct PKC-δ–mediated phosphorylation of Jak2 on serine and threonine residues. Inhibition of Jak2 was not caused by the down-regulation of IL-3R, and the PKC-α and PKC-δ isoforms also specifically inhibited Jak2 in ligand-independent overexpression models. The possibility that the PKC-induced inhibition of Jak2 would be mediated indirectly either by tyrosine phosphatases8,16or by MEK-ERK kinases was argued against by experiments with tyrosine phosphatase and MEK kinase inhibitors, which did not affect the inhibition. Furthermore, MEK1 is activated similarly by all PKC isotypes, which makes it a less likely mediator of the PKC isoform-specific inhibition of Jak2 in these cells.41 On the other hand, the rapid kinetics of the inhibition does not support involvement in this response for the transcriptionally regulated Jak inhibitors SOCS/SSI/JAB.3-5 Recently, ERK2 kinase was shown to associate with and to inhibit Stat3.13,14 Interestingly, the effect of ERK2 was receptor specific because the inhibition was observed in IL-6 but not in interferon-α–induced activation of Stat3.13 Thus, it appears that PKC, or certain isoforms of PKC, can regulate cytokine signaling by 2 distinct mechanisms, directly through interaction with Jak2 and indirectly through activation of ERK2 in a receptor-specific manner.
Jak2 plays an indispensable role in IL-3R mitogenic signaling.18-20 PKC-mediated inhibition of Jak2 was closely correlated with the abrogation of cell growth in differentiating 32D cells. The inhibition of Jak2 either by PKC-δ, tyrosine kinase inhibitor AG490, or IL-3 deprivation all resulted in similar G1 arrest of the cell cycle. However, the differentiated phenotype was observed in only TPA-treated cells (data not shown). These results are in agreement that Jak2 activation is critical for cell-cycle progression and induction of short-term proliferation,20,42 and they suggest that in growth factor–dependent myeloid cells, the inhibition of Jak2 functions as a mechanism to control cell proliferation during differentiation. However, cell-cycle progression can be negatively regulated by other mechanisms. In growth factor–independent myeloid cell lines, differentiation-inducing agents have been shown to stimulate cyclin-dependent kinase inhibitor gene expression.43,44 The existence of parallel mechanisms for controlling cell proliferation emphasizes the importance of this regulation for successful execution of cellular differentiation. In support of this notion, the reversal of Jak2 inhibition by ectopic expression of Jak2 resulted in increased apoptosis among the differentiating cells. The molecular mechanism for the observed apoptosis in 32D-δ–Jak2 is unknown. However, c-myc has been shown to be directly regulated by Jak2,42 and constitutive c-myc expression has been shown to promote apoptosis under restrictive growth conditions.45,46 In our experiments, apoptosis was more pronounced in reduced serum concentrations, though it was observed also in optimal growth conditions. On the other hand, PKC-δ has been associated with the induction of apoptosis.47 Prolonged (24-hour) TPA treatment used in our differentiation experiments resulted in the down-regulation of PKC; thus, the observed apoptosis could have been caused by either PKC-δ–mediated signaling or the absence of PKC-δ. Proteolytic cleavage and activation of PKC-δ have been directly implicated in the onset of apoptosis in various cell types,47-49 possibly because of the PKC-δ–mediated inhibition of DNA-dependent protein kinase-mediated phosphorylation of p53.50 However, in 32D-δ cells, macrophage differentiation did not result in marked apoptosis. Therefore, it is likely that the activation of PKC-δ, rather than its down-regulation, with the simultaneous activation of Jak2 in 32D-δ–Jak2 cells, results in a proapoptotic effect that overrides the Bcl-2– and Bcl-xL–mediated anti-apoptotic pathway from IL-3R and Jak2.20
Inhibition of Jak2 by specific PKC isoforms represents a previously uncharacterized mechanism of negative regulation of cytokine signaling that appears to integrate different signaling pathways during hematopoietic cell differentiation. However, IL-3 deprivation or AG490 treatment does not lead to macrophage phenotype. Thus, Jak2 inhibition alone is not sufficient to cause terminal differentiation of 32D cells. This suggests that PKC mediates at least 2 distinct signals, both of which are required for proper execution of the differentiation process: one signal for the direct phosphorylation and inhibition of Jak2 associated with growth arrest, and another signal for the induction of differentiation.
Acknowledgments
We thank Paula Kosonen for technical assistance, Drs O. Jaakkola, H. Kankaanranta, and A. Lagerstedt for help with apoptosis assays and photography, Dr K. Saksela for discussions, and Drs K. Alitalo, L. Andersson, M. Hurme, and H. Jacobs for reading the manuscript.
Supported by the Academy of Finland, Sigrid Juselius Foundation, the Medical Research Fund of Tampere University Hospital, and the Emil Aaltonen Foundation.
Reprints:Olli Silvennoinen, Laboratory of Molecular Immunology, Institute of Medical Technology, University of Tampere, Lenkkeilijankatu 6, FIN-33101 Tampere, Finland; e-mail:olli.silvennoinen@uta.fi.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.