Abstract
Our recent studies suggest that human squamous cell carcinoma of the head and neck (SCCHN) is capable of activating an intrinsic mechanism of programmed-cell death in interacting lymphocytes in situ and in vitro. The current study used Jurkat T-cell line as a model to investigate intracellular apoptotic events in T cells interacting with SCCHN. Apoptosis induced in T lymphocytes by tumor cells was in part Fas-mediated, since it was partially, but significantly, inhibited in the presence of anti-Fas ligand Ab or in Fas-resistant Jurkat cells. The synthetic caspase inhibitors, N-benzyloxycarbonyl-Val-Ala-Asp-fluoromethyl ketone (Z-VAD-FMK) and N-benzyloxycarbonyl-Asp-glu-Val-Asp-fluoromethyl ketone (Z-DEVD-FMK), effectively blocked apoptosis of Jurkat cells co-incubated with SCCHN cell lines, suggesting the involvement of caspases in tumor-induced apoptosis of lymphocytes. Overexpression of CrmA, an inhibitor of caspase-1 and caspase-8, partially inhibited tumor-induced T-cell death. Caspase-8 and caspase-3 were identified as effector molecules in the execution of tumor-induced T-cell death, since the proform enzymes were processed into active subunits during co-incubation of T cells with tumor cells. Furthermore, co-incubation with tumor cells resulted in cleavage of poly(ADP-ribose) polymerase (PARP), a common caspase-3 substrate, and in cleavage of TcR-ζ chain, shown by us to be a T-cell specific caspase-3 substrate. Overexpression of Bcl-2 did not provide protection of T cells from SCCHN-induced DNA degradation. Instead, the Bcl-2 protein was cleaved in the target T cells during their co-incubation with tumor cells. These findings demonstrate that tumor cells can trigger in T lymphocytes caspase-dependent apoptotic cascades, which are not effectively protected by Bcl-2.
Mechanisms of tumor escape from immune destruction include evasive strategies to avoid immune recognition,1 as well as modulation and suppression of immune cell functions.2-4 A previously unknown active mechanism of tumor-induced immunosuppression has been suggested by the identification of Fas ligand (FasL) expression on tumor cells. Expression of FasL has recently been reported in solid tumors of nonhematopoietic origin, including colon,1,2 hepatocellular carcinoma,3 melanoma,4astrocytoma,5,6 lung carcinoma,7 ovarian carcinoma,8 esophageal carcinoma,9glioblastoma,10 renal cell carcinoma,11 and head and neck carcinoma.12 However, considerable heterogeneity in surface expression of FasL was detected even within a particular lineage of tumor.4,5,8,13 14 Moreover, intracellular apoptotic events, which may help identify the apoptotic pathway initiated, have not yet been elucidated in T cells interacting with solid tumors.
Fas represents one member of a family of death receptors that might be involved in death-signaling cascade induced in T cells by direct engagement of death receptors on the lymphocytes with death ligands expressed by the tumor cells. Activation-induced cell death (AICD) represents a mechanism that involves engagement of death receptors on lymphocytes by death ligands on the same lymphocyte (autocrine or suicide) or on adjacent lymphocytes (paracrine or fratricide).15,16 AICD is dependent on prior up-regulation in expression of Fas/FasL on T cells.15,17 Few reports have suggested that AICD may also be mediated by the up-regulation of the death ligand, tumor necrosis factor-related apoptosis-inducing factor (TRAIL), on activated lymphocytes.18,19 In addition to AICD, such mechanisms of inducible sensitivity to Fas-mediated killing have recently been suggested for stress-induced apoptosis in T cells treated with DNA-damaging agents, including radiation or chemotherapeutic agents.20,21 Death receptor–independent mechanisms of lymphocyte apoptosis may also be induced by inhibitory factors in the tumor microenvironment, such as TGF-β or interleukin (IL)–10,22 alterations in redox status, or changes in second messengers, such as ceramide or intracellular calcium. Since various signaling cascades might be involved in tumor-induced apoptosis of lymphocytes, it is important to identify those common intracellular events that may serve as potential targets for therapeutic intervention.
Currently, it is not precisely clear what defines the point of no return in the intracellular signaling cascade, the point at which the cell is committed to apoptotic death. Blocking of early events in tumor-induced apoptosis of lymphocytes requires the elucidation of the death pathways and effector molecules involved. Recent evidence suggests that distinct stimuli of apoptosis result in activation of specific effector molecules. Thus, different sets of caspases appear to participate in execution of apoptosis triggered by death receptors, withdrawal of growth factors, or irradiation.23-25 Consistent with this notion, various pathways of apoptosis are also differentially regulated by inhibitors of apoptosis, including Bcl-2 family members cytokine response–modifier gene A (CrmA), cellular FLICE-inhibitory protein or inhibitor of apoptosis, which target different caspases.26-28 The need to identify specific caspases that might serve as potential targets for inhibition of apoptosis is further indicated by studies performed in cells deficient in caspase-3.29 Although caspase-3 has been shown to be one of the major activated caspases present in apoptotic cells,30its requirement in apoptosis is tissue-specific and can even be stimulus-specific within the same cell type.29
The intracellular effector molecules involved in execution of tumor-induced death of lymphocytes have not yet been elucidated. This study is the first to identify caspases involved in tumor-induced death of T cells and to assess the capability of inhibitors of apoptosis to protect from tumor-induced apoptosis.
Materials and methods
Reagents
Agonistic anti-Fas antibody (Ab) (CH-11, immunoglobulin [Ig]M) was purchased from Upstate Biotechnology (Lake Placid, NY); anti–Bcl-2 monoclonal antibody (mAb) (Bcl-2 100) from Santa Cruz Biotechnology (Santa Cruz, CA); anti–caspase-3 mAb (CPP32, clone 19) from Transduction Laboratories (Lexington, KY); and anti–caspase-8 mAb (B9-2) from PharMingen (San Diego, CA). Anti–poly(adenosine diphosphate–ribose) polymerase (anti-PARP) mAb (C2.10) and fluoromethyl ketone (FMK)–conjugated inhibitors of apoptosis, including Z-VAD-FMK, Z-DEVD-FMK, and a control peptide N-benzyloxycarbonyl-Phe-Ala-fluoromethyl ketone (Z-FA-FMK), were purchased from Enzyme Systems (Livermore, CA). Anti-ζ mAb (6B10.2) was purchased from Santa Cruz Biotechnology. Apoptosis terminal deoxynucleotidyl transferase–mediated deoxyuridine triphosphate nick-end labeling (TUNEL) kits were purchased from Boehringer-Mannheim (Indianapolis, IN); DiOC6 from Molecular Probes (Eugene, OR); and the etoposide VP-16 from Sigma (St Louis, MO). Anti-α6β4 mAb (A9) was a generous gift from Dr T. E. Carey (University of Michigan Cancer Center, Ann Arbor). Goat anti-mouse Ig G (GAMIg)– conjugated magnetic beads were purchased from PerSeptive Diagnostics (Cambridge, MA).
Cell lines
The squamous cell carcinoma of the head and neck (SCCHN) cell lines PCI-13 and PCI-52 were established in our laboratory, as previously described.31 All the cell lines used, including OSC-19, SCC-68, and SCC-74, were routinely tested and confirmed to be negative for the presence of mycoplasma (Gen Probe, San Diego, CA). Fas-resistant Jurkat cells were obtained by multiple cycles of treatment with agonistic anti-Fas Ab (CH-11, 200 ng/mL), followed by selection for Fas-positive cells by fluorescence-activated cell sorter (FACS) sorting.
To generate stable cell lines expressing epitope-tagged proteins, the CMV/Neo/CrmA-KT3 or CMV/Neo/Bcl-2-KT3, expression constructs prepared as previously described,32 were introduced into Jurkat cells by electroporation (250V, 960 microfarads). As a control, the CMV/Neo vector alone was electroporated into Jurkat cells. Following electroporation, transfected cells were selected in media containing 0.5 mg/mL G418. After 2 weeks of selection, independent clones were isolated by limiting dilution. Expression of the CrmA/KT3 or Bcl-2/KT3 proteins in independent clonal cell lines was confirmed by Western blotting of whole cell lysates using anti-KT3 mAb.
Induction of apoptosis
To induce apoptosis or apoptosis-related changes in lymphocytes, SCCHN cell lines were coincubated with Fas-sensitive or Fas-resistant Jurkat cells for 16 to 24 hours at a tumor-to-lymphocyte cell ratio ranging from 20:1 to 80:1. To assess processing of intracellular proteins, including Bcl-2, caspase-3, and PARP, in the target cells, Jurkat cells were negatively selected by removal of SCCHN cells by epithelial-specific α6β4 mAb (A9) and GAMIg-conjugated magnetic beads. Cocultures of SCCHN and Jurkat cells were incubated with A9 mAb at 50 μg/107 cells/mL on ice for 1 hour. The cells were washed 3 times in cold medium and subjected to 2 cycles of incubation with and separation from GAMIg-coated magnetic beads (30:1 beads-to-cell ratio). As assessed by flow cytometry of cells stained with anti-α6β4integrin mAb, all tumor cells were removed by this procedure. Apoptotic cells triggered by agonistic anti-Fas Ab (CH-11, 200 ng/mL) or VP-16 (20 μmol/L) served as controls.
Apoptosis detection assays
DNA fragmentation assays included the JAM assay, in which loss of [3H]TdR-labeled DNA was measured, and the terminal deoxynucleotidyl transferase–mediated deoxyuridine-triphosphate (dUTP) nick-end labeling (TUNEL) assay, in which the presence of breaks in DNA was assessed.8 DNA labeling of Jurkat target cells for the JAM assay was performed by incubation of the cells in the presence of 5 μCi/mL [3H]TdR for 18 to 24 hours at 37°C. Tumor cells were cocultured with [3H]TdR-labeled target cells for 16 hours at 37°C at a tumor-to-lymphocyte cell ratio ranging from 20:1 to 80:1. At the end of the coincubation period, the cells were harvested (Mach IIM, TOMTEC, Walloch, Gaithersburg, MD) onto glass fiber filters. The radioactivity of unfragmented DNA retained on the glass fiber filters was measured by liquid scintillation counting. Specific DNA fragmentation was calculated according to the following formula: percentage of specific DNA fragmentation = 100 × (S-E)/S, where S = retained DNA in the absence of effector cells (spontaneous), and E = experimentally retained DNA in the presence of tumor (effector) cells.
To identify fragmented DNA in Jurkat cells, a flow cytometry–based TUNEL assay was performed (Boehringer-Mannheim).33 The cells (106/sample) were washed in phosphate-buffered saline (PBS) and fixed in 2% paraformaldehyde for 30 minutes at room temperature. After fixation, the cells were washed twice in PBS containing .01% bovine serum albumin, and resuspended in TUNEL reaction mixture containing fluorescein dUTP and terminal deoxynucleotidyl transferase (TdT). Control cells were resuspended in TUNEL reaction mixture containing fluorescein dUTP without TdT. Fluorescein labels incorporated in DNA strand breaks were detected by flow cytometry.
To identify fragmented DNA in CD3+ lymphocytes after coincubation with tumor cells, the recovered cells were first stained with either phycoerythrin (PE)–labeled anti-CD3 mAb (Becton Dickinson, Bedford, MA) or PE-labeled isotype-matched control Ab, then fixed and stained by TUNEL. Gated CD3+ cells were assessed for TUNEL staining.
Apoptosis-associated alterations in Jurkat cells were also evaluated by staining with the potential-sensitive dye DiOC6, which is incorporated into mitochondria.34 Loss in DiOC6 staining indicates disruption of the mitochondrial inner transmembrane potential associated with apoptosis.35 Cells were first stained for DiOC6 (40 nmol/L, 15 minutes at 37°C), and then without fixation, stained by PE-anti-CD3 on ice. CD3+ cells were gated to assess mitochondrial staining by DiOC6.
Intracellular caspase activity
Following apoptotic stimulation, Jurkat cells (5 × 105) were resuspended in 50 μL of 10 μmol/L PhiPhiLux-G2D2 substrate solution (OncoImmunin, College Park, MD) in RPMI-1640 supplemented with 10% FCS. After incubation for 1 hour at 37°C avoiding direct light, the sample was diluted with 0.5 mL of ice-cold flow cytometry dilution buffer (OncoImmunin). Flow cytometric analysis was performed within 60 minutes of the end of the incubation period.
Western blot analysis
Proteins were separated by sodium dodecyl sulfate–polyacrylamide gel electrophoresis using 7.5% to 12% polyacrylamide gels and transferred to polyvinylidene fluoride membranes, as previously described.36 Following probing with specific antibodies, the protein bands were detected by enhanced chemiluminescence (Pierce, Rockford, IL).
Statistics
Statistical significance of results was determined by UMann-Whitney nonparametric test. Differences between groups were considered significant at P < .05.
Results
Tumor-induced apoptosis in lymphocytes is partly Fas-mediated
To examine the ability of SCCHN cell lines to induce apoptosis in lymphocytes, tumor cells were cocultured with lymphocytes at tumor-to-lymphocyte ratios ranging from 20:1 to 80:1 and were examined by various methods detecting the presence of apoptotic T lymphocytes. A significant loss of DNA, as assessed by the JAM assay (Figure1A), as well as fragmentation of DNA, as evidenced by the TUNEL assay (Figure 1B), and altered polarization of the mitochondria, as assessed by loss in DiOC6 staining (Figure 1C), were detected in the Jurkat target cells coincubated with various SCCHN cells for 16 hours. To positively identify apoptotic T cells and exclude apoptotic tumor cells, TUNEL and DiOC6 staining were each performed in conjunction with CD3 staining. The presence of TUNEL+ or DiOC6+ cells was determined in CD3+ gated cell population (Figures 1B and 1C). Tumor-induced apoptosis of Jurkat cells was dose-dependent (not shown) and was first observed following 10 hours of coincubation, while death induced by agonistic anti-Fas Ab (CH-11, 200 ng/mL) was detected as early as 2 hours following the addition of the Ab.
Tumor-induced apoptosis of Jurkat cells as assessed by the JAM assay, flow cytometry TUNEL, and loss in DiOC6 staining of mitochondria.
(A) Apoptosis of Jurkat cells as assessed by the JAM assay. Various SCCHN cell lines were coincubated with [3H]TdR-labeled Jurkat cells at a 40:1 tumor-to-lymphocyte cell ratio for 16 hours. Treatment with agonistic anti-Fas Ab (CH-11, 200 ng/mL) served as positive control for apoptosis. Target cell death was determined by measuring fragmentation of 3H-labeled target cell DNA. The error bars represent the SEM of 8 replicates. (B) Apoptosis of Jurkat cells as assessed by flow cytometry TUNEL. Fas-sensitive or Fas-resistant Jurkat cells were treated with agonistic anti-Fas Ab (CH-11, 200 ng/mL) or coincubated with PCI-13 (tumor-to-lymphocyte cell ratio of 40:1) for 16 hours. The cells were then stained with anti–CD3-PE, fixed, and stained for DNA breaks by TUNEL. TUNEL staining was assessed by flow cytometry in CD3+-gated cells. The percentage of TUNEL positive cells is indicated at the right corners. (C) Apoptosis of Jurkat cells as assessed by loss in DiOC6 staining of mitochondria. Fas-sensitive Jurkat cells, incubated in medium alone or with PCI-13 tumor cells (tumor-to-lymphocyte cell ratio of 40:1) for 16 hours, were stained for DiOC6 (40 nmol/L, 15 minutes, 37°C) and then, without fixation, stained by PE-conjugated anti-CD3 Ab on ice. Results shown in A, B, and C were reproduced in at least 3 different experiments.
Tumor-induced apoptosis of Jurkat cells as assessed by the JAM assay, flow cytometry TUNEL, and loss in DiOC6 staining of mitochondria.
(A) Apoptosis of Jurkat cells as assessed by the JAM assay. Various SCCHN cell lines were coincubated with [3H]TdR-labeled Jurkat cells at a 40:1 tumor-to-lymphocyte cell ratio for 16 hours. Treatment with agonistic anti-Fas Ab (CH-11, 200 ng/mL) served as positive control for apoptosis. Target cell death was determined by measuring fragmentation of 3H-labeled target cell DNA. The error bars represent the SEM of 8 replicates. (B) Apoptosis of Jurkat cells as assessed by flow cytometry TUNEL. Fas-sensitive or Fas-resistant Jurkat cells were treated with agonistic anti-Fas Ab (CH-11, 200 ng/mL) or coincubated with PCI-13 (tumor-to-lymphocyte cell ratio of 40:1) for 16 hours. The cells were then stained with anti–CD3-PE, fixed, and stained for DNA breaks by TUNEL. TUNEL staining was assessed by flow cytometry in CD3+-gated cells. The percentage of TUNEL positive cells is indicated at the right corners. (C) Apoptosis of Jurkat cells as assessed by loss in DiOC6 staining of mitochondria. Fas-sensitive Jurkat cells, incubated in medium alone or with PCI-13 tumor cells (tumor-to-lymphocyte cell ratio of 40:1) for 16 hours, were stained for DiOC6 (40 nmol/L, 15 minutes, 37°C) and then, without fixation, stained by PE-conjugated anti-CD3 Ab on ice. Results shown in A, B, and C were reproduced in at least 3 different experiments.
To examine whether the Fas pathway was involved in the observed death of Jurkat cells, anti-FasL neutralizing Ab was added to the coculture of Jurkat and tumor cells (Figure 2A). In the presence of FasL blocking Ab, apoptosis of Jurkat cells induced by various SCCHN cells (results for PCI-13 cell line are presented) was partially but significantly inhibited, suggesting that Fas signaling was involved. To further investigate the involvement of the Fas pathway in SCCHN-induced apoptosis of Jurkat cells, a Fas-resistant Jurkat cell line was generated by selection of cells resistant to multiple cycles of treatment with agonistic anti-Fas Ab followed by positive selection of Fas-expressing cells using FACS cell sorting.8 When [3H]TdR-labeled Fas-resistant cells were coincubated with SCCHN cells, no DNA degradation was observed (Figure 2B).
Involvement of Fas/FasL in tumor-induced apoptosis of T cells.
(A) Inhibition of tumor-mediated apoptosis of Jurkat cells by anti-FasL Ab. [3H]TdR-labeled Jurkat cells were treated for 2 hours with anti-FasL Ab (4H9) or with a hamster IgG control at various concentrations, as indicated. Target cell death was determined at 16 hours by measuring fragmentation of 3H-labeled DNA. The error bars represent the SEM of 8 replicates. (B) Reduced sensitivity of Fas-resistant Jurkat cells to PCI-13–mediated apoptosis. Fas-resistant Jurkat cells were obtained as described in “Materials and methods.” [3H]TdR-labeled Fas-sensitive and [3H]TdR-labeled Fas-resistant Jurkat cells were coincubated with PCI-13 cells (tumor-to-Jurkat ratio, 80:1) or anti-Fas (CH-11) Ab for 16 hours, and tested for apoptosis by JAM assay.
Involvement of Fas/FasL in tumor-induced apoptosis of T cells.
(A) Inhibition of tumor-mediated apoptosis of Jurkat cells by anti-FasL Ab. [3H]TdR-labeled Jurkat cells were treated for 2 hours with anti-FasL Ab (4H9) or with a hamster IgG control at various concentrations, as indicated. Target cell death was determined at 16 hours by measuring fragmentation of 3H-labeled DNA. The error bars represent the SEM of 8 replicates. (B) Reduced sensitivity of Fas-resistant Jurkat cells to PCI-13–mediated apoptosis. Fas-resistant Jurkat cells were obtained as described in “Materials and methods.” [3H]TdR-labeled Fas-sensitive and [3H]TdR-labeled Fas-resistant Jurkat cells were coincubated with PCI-13 cells (tumor-to-Jurkat ratio, 80:1) or anti-Fas (CH-11) Ab for 16 hours, and tested for apoptosis by JAM assay.
Activation of caspases in T lymphocytes coincubated with tumor cells
To investigate the role of caspases in tumor-induced apoptosis of T cells, Jurkat target cells were pretreated with the irreversible peptide inhibitors Z-VAD-FMK or Z-DEVD-FMK.37-39 Whereas Z-VAD-FMK is a pan-caspase inhibitor, Z-DEVD-FMK has an optimal tetrapeptide recognition motif for caspase-2, caspase-3, and caspase-7.40 In the presence of these inhibitors, tumor-induced DNA degradation (Figure 3), as well as trypan blue uptake in lymphocytes, was effectively inhibited.
Effects of peptide inhibitors of caspases on Fas- or tumor-induced DNA degradation in Jurkat cells.
[3H]TdR-labeled Jurkat cells were pretreated with Z-VAD-FMK or Z-DEVD-FMK at the indicated concentrations for 16 hours and then coincubated with tumor at a 40:1 tumor-to-lymphocyte cell ratio for an additional 16 hours. Jurkat cell apoptosis was determined by measuring the loss of 3H-labeled DNA. The error bars represent the SEM of 8 replicates. Similar results were obtained in the absence of inhibitors or in the presence of the control inhibitor Z-FA-FMK.
Effects of peptide inhibitors of caspases on Fas- or tumor-induced DNA degradation in Jurkat cells.
[3H]TdR-labeled Jurkat cells were pretreated with Z-VAD-FMK or Z-DEVD-FMK at the indicated concentrations for 16 hours and then coincubated with tumor at a 40:1 tumor-to-lymphocyte cell ratio for an additional 16 hours. Jurkat cell apoptosis was determined by measuring the loss of 3H-labeled DNA. The error bars represent the SEM of 8 replicates. Similar results were obtained in the absence of inhibitors or in the presence of the control inhibitor Z-FA-FMK.
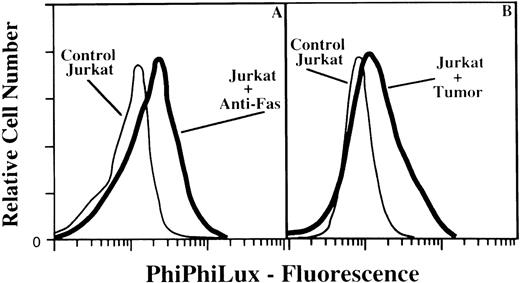
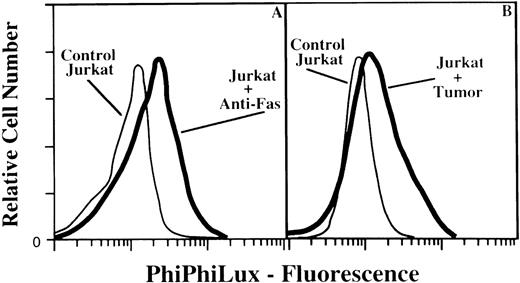
To demonstrate activation of caspases in Jurkat cells coincubated with tumor cells, the PhiPhiLux-G2D2 cell-permeable fluorescent substrate for caspases was used. This substrate emits fluorescence when it is cleaved within the sequence GDEVDGID, allowing the determination of caspase-3–like activity by flow cytometry.41 42 As shown in Figure 4, activity of caspases cleaving at DEVD sequence was detected in Jurkat cells either treated by agonistic anti-Fas Ab (38% positive cells) or cocultured with PCI-13 cells (31% positive cells).
Flow cytometric analysis of caspase activity in tumor- or Fas-stimulated T lymphocytes.
In (A) Jurkat cells were treated with anti-Fas Ab (CH-11, 200 ng/mL) for 16 hours at 37°C. In (B) Jurkat cells were cocultured on PCI-13 monolayer (tumor-to-lymphocyte cell ratio of 40:1) for 16 hours. At the end of the coincubation periods, the cells were treated with anti–CD3–fluorescein isothiocyanate followed by incubation with 10 μmol/L PhiPhiLux-G2D2 for 1 hour. CD3-positive cells were analyzed for caspase-3 cleavage activity of PhiPhiLux. Controls indicate baseline fluorescence of substrate-loaded cells in the absence of apoptotic stimulation. The percentage of positive cells for PhiPhiLux fluorescence was as follows: 5% in control; 38% in Jurkat treated with anti-Fas Ab; 31% in Jurkat coincubated with tumor cells.
Flow cytometric analysis of caspase activity in tumor- or Fas-stimulated T lymphocytes.
In (A) Jurkat cells were treated with anti-Fas Ab (CH-11, 200 ng/mL) for 16 hours at 37°C. In (B) Jurkat cells were cocultured on PCI-13 monolayer (tumor-to-lymphocyte cell ratio of 40:1) for 16 hours. At the end of the coincubation periods, the cells were treated with anti–CD3–fluorescein isothiocyanate followed by incubation with 10 μmol/L PhiPhiLux-G2D2 for 1 hour. CD3-positive cells were analyzed for caspase-3 cleavage activity of PhiPhiLux. Controls indicate baseline fluorescence of substrate-loaded cells in the absence of apoptotic stimulation. The percentage of positive cells for PhiPhiLux fluorescence was as follows: 5% in control; 38% in Jurkat treated with anti-Fas Ab; 31% in Jurkat coincubated with tumor cells.
Tumor-mediated apoptosis in T cells overexpressing cytokine response-modifier gene A
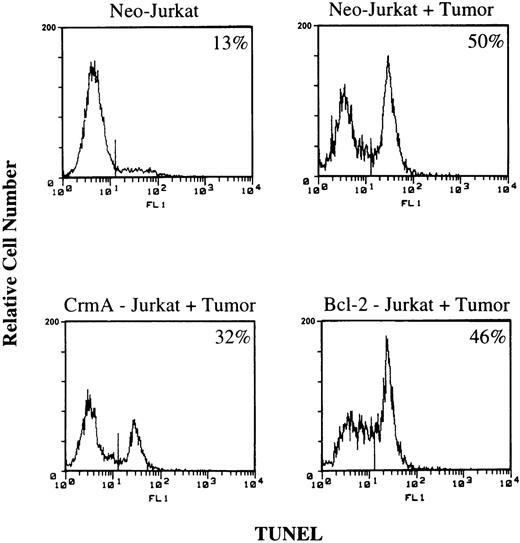
To further investigate the activation of caspases in apoptosis of lymphocytes coincubated with tumor cells, Jurkat cells overexpressing the cowpox virus–encoded serpin, CrmA, were used as target lymphocytes.32 CrmA is a potent inhibitor of caspase-1 and caspase-8, and its inhibition of caspase-3 has been shown to be indirect, resulting from inhibition of caspase-8.38 40 Overexpression of CrmA in Jurkat cells resulted in partial inhibition of apoptosis induced by either agonistic anti-Fas Ab, tumor cells, or VP-16, as assessed by the JAM assay (Figure 5). While overexpression of CrmA efficiently blocked apoptosis induced by OSC-68 cells, less protection was observed in transfected Jurkat cells cocultured with PCI-13 cells. The partial inhibition of PCI-13–induced apoptosis in Jurkat cells overexpressing CrmA was confirmed by a TUNEL assay performed in conjunction with CD3 staining (Figure6). The ability of CrmA to inhibit tumor-induced apoptosis of T cells suggests that caspase-8 is involved in this apoptotic pathway. However, the observed partial inhibition by CrmA suggests that, in addition to CrmA-sensitive caspases, CrmA-insensitive caspases were also activated in Jurkat cells following interaction with tumor cells.
Effects of CrmA overexpression on the susceptibility of Jurkat cells to tumor-mediated apoptosis.
CrmA or control Neo-Jurkat cells were labeled with [3H]TdR and coincubated with tumor cells at a tumor-to-lymphocyte cell ratio of 40:1. As controls, these cells were treated with agonistic anti-Fas Ab (CH-11, 200 ng/mL) or VP-16 (20 μmol/L). Target cell death was determined at the indicated time points by measuring loss in 3H-labeled DNA. The error bars represent the SEM of 8 replicates.
Effects of CrmA overexpression on the susceptibility of Jurkat cells to tumor-mediated apoptosis.
CrmA or control Neo-Jurkat cells were labeled with [3H]TdR and coincubated with tumor cells at a tumor-to-lymphocyte cell ratio of 40:1. As controls, these cells were treated with agonistic anti-Fas Ab (CH-11, 200 ng/mL) or VP-16 (20 μmol/L). Target cell death was determined at the indicated time points by measuring loss in 3H-labeled DNA. The error bars represent the SEM of 8 replicates.
Tumor-induced apoptosis in Jurkat cells stably transfected with CrmA, Bcl-2, or Neo vector alone.
Jurkat cells were coincubated with PCI-13 cells for 16 hours. The cells were then stained with anti–CD3-PE, fixed, and stained for DNA breaks by TUNEL. TUNEL staining was assessed by flow cytometry in CD3+-gated cells. The percentage of TUNEL-positive cells is indicated at the right corners.
Tumor-induced apoptosis in Jurkat cells stably transfected with CrmA, Bcl-2, or Neo vector alone.
Jurkat cells were coincubated with PCI-13 cells for 16 hours. The cells were then stained with anti–CD3-PE, fixed, and stained for DNA breaks by TUNEL. TUNEL staining was assessed by flow cytometry in CD3+-gated cells. The percentage of TUNEL-positive cells is indicated at the right corners.
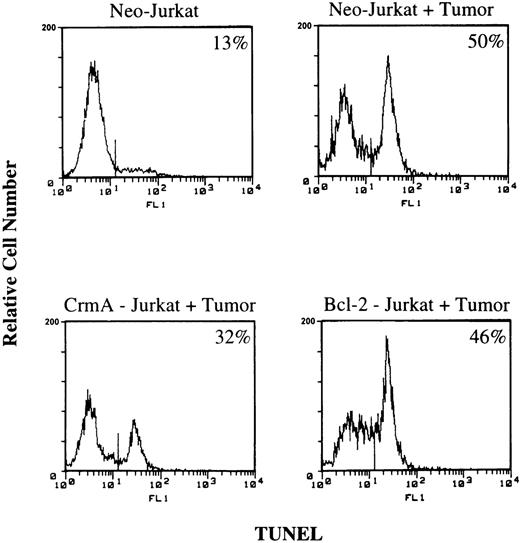
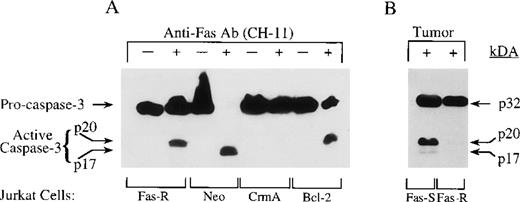
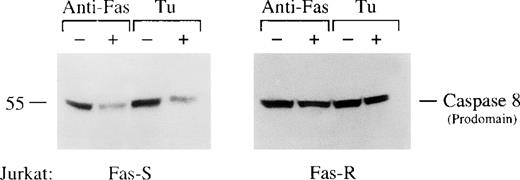
Activation of caspase-8 and caspase-3 in tumor-induced apoptosis of T cells
Caspase-8 has been recognized as the most apical caspase activated in the Fas or TRAIL pathways of cell death.43-45 As shown in Figure 7, the prodomain of caspase-8 was processed in Fas-sensitive Jurkat cells, but not in Fas-resistant Jurkat cells, that were treated with agonistic anti-Fas Ab or coincubated with tumor cells. Owing to a fast turnover, active subunits were not detected at 16 hours coincubation with tumor cells or agonistic anti-Fas Ab.
Tumor-induced activation of caspase-8.
Fas-sensitive or Fas-resistant Jurkat cells were treated with agonistic anti-Fas Ab (CH-11, 200 ng/mL) or coincubated with tumor cells for 16 hours. At the end of the incubation period, Jurkat cells were negatively selected by removal of tumor cells, lysed, and assessed by Western blotting for loss in expression of caspase-8. Equal loading was confirmed by equivalent detection of nonspecific bands on the same membrane when stripped and probed for the presence of other caspases (not shown).
Tumor-induced activation of caspase-8.
Fas-sensitive or Fas-resistant Jurkat cells were treated with agonistic anti-Fas Ab (CH-11, 200 ng/mL) or coincubated with tumor cells for 16 hours. At the end of the incubation period, Jurkat cells were negatively selected by removal of tumor cells, lysed, and assessed by Western blotting for loss in expression of caspase-8. Equal loading was confirmed by equivalent detection of nonspecific bands on the same membrane when stripped and probed for the presence of other caspases (not shown).
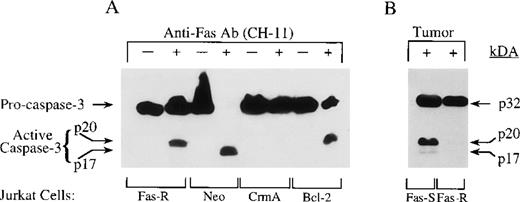
Caspase-3 has been shown to play a central executioner role in various pathways of apoptosis. Processing of pro–caspase-3 into an active enzyme results in cleavage of the pro-enzyme (p32) into p20, p17, and p10 subunit proteins37,38; p17 is generated by further cleavage of the p20 by catalytic activity, which is inhibited in the presence of DEVD-FMK.46 47 The processing of caspase-3 in Jurkat cells triggered by agonistic anti-Fas Ab or tumor cells was examined by Western blot analysis, using mAb, which detects the presence of p32, p20, and p17, but not p10. Full processing of the p32 pro-enzyme was observed in Neo-Jurkat cells treated with agonistic anti-Fas Ab (Figure 8A). The presence of CrmA inhibited the generation of active caspase-3 in response to Fas crosslinking, while only partial inhibition was observed in Fas-resistant Jurkat cells or in Jurkat cells overexpressing Bcl-2. Interestingly, p17 active caspase-3 was generated in the Neo-Jurkat cells, while only p20 was detected in either Bcl-2 or Fas-resistant Jurkat cells. Coincubation of tumor cells with Fas-sensitive Jurkat cells, but not with Fas-resistant cells, resulted in activation of caspase-3 (Figure 8B). The signal delivered by the tumor cells was less potent than that of anti-Fas agonistic Ab, since only partial processing of the p32 was observed as compared with Jurkat cells treated with anti-Fas Ab. (Similar results were obtained in untransfected or Neo-Jurkat cells.) However, both p20 and p17 were generated in response to tumor-induced apoptosis (Figure 8B).
Processing of caspase-3 in Jurkat cells treated with agonistic anti-Fas Ab or coincubated with tumor cells.
In (A) Jurkat cells, including Fas-resistant (Fas-R), Neo control, CrmA, and Bcl-2, were treated with CH-11 (200 ng/mL) for 16 hours. At the end of the incubation period, the cells were lysed and assessed by Western blotting for caspase-3 (anti-CPP32 mAb, 2.5 μg/mL). In (B) Fas-sensitive (Fas-S) and Fas-resistant Jurkat cells were coincubated with tumor cell (20:1 tumor-to-Jurkat cell ratio) for 16 hours. At the end of the coincubation period, Jurkat lymphocytes were negatively selected by removal of tumor cells, with the use of epithelial-specific anti-α6β4 mAb and magnetic beads. Negatively selected Jurkat cells were lysed and analyzed by Western blotting for processing of caspase-3.
Processing of caspase-3 in Jurkat cells treated with agonistic anti-Fas Ab or coincubated with tumor cells.
In (A) Jurkat cells, including Fas-resistant (Fas-R), Neo control, CrmA, and Bcl-2, were treated with CH-11 (200 ng/mL) for 16 hours. At the end of the incubation period, the cells were lysed and assessed by Western blotting for caspase-3 (anti-CPP32 mAb, 2.5 μg/mL). In (B) Fas-sensitive (Fas-S) and Fas-resistant Jurkat cells were coincubated with tumor cell (20:1 tumor-to-Jurkat cell ratio) for 16 hours. At the end of the coincubation period, Jurkat lymphocytes were negatively selected by removal of tumor cells, with the use of epithelial-specific anti-α6β4 mAb and magnetic beads. Negatively selected Jurkat cells were lysed and analyzed by Western blotting for processing of caspase-3.
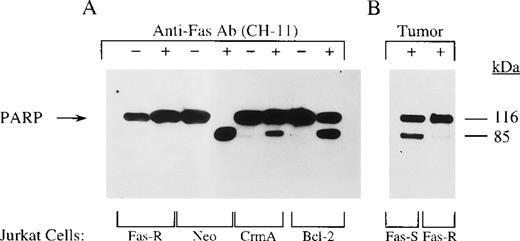
Caspase substrates in T lymphocytes coincubated with tumor cells
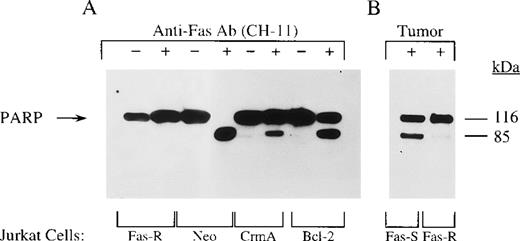
PARP is a highly conserved nuclear enzyme, which is activated following DNA damage and is implicated in DNA repair.48Proteolytic cleavage of PARP has been shown to be linked to activation of DEVD-specific caspases, including caspase-3 and caspase-7.49 PARP cleavage was observed in transfected Jurkat cells, including Neo, CrmA, and Bcl-2, following treatment with agonistic anti-Fas Ab (Figure9A). No PARP cleavage was observed in Fas-resistant Jurkat cells, and the cleavage observed in Jurkat cells overexpressing Bcl-2 or CrmA was significantly reduced as compared with Neo control cells. Since no activation of caspase-3 was observed in CrmA Jurkat cells, the PARP is probably cleaved by other activated caspases (eg, caspase-7). The absence of PARP cleavage in the Fas-resistant Jurkat cells suggests that the p20 caspase-3 detected in Figure 8A is either not active or blocked. Similar to what occurs with Fas-ligation, coincubation with tumor cells induced PARP cleavage in Fas-sensitive, but not in Fas-resistant, Jurkat cells (Figure9B). These results suggest that PARP is a common substrate cleaved in apoptotic lymphocytes induced by tumor cells or anti-Fas Ab. However, the signal delivered by the tumor appears to be less potent than that of anti-Fas Ab, as it induced only partial processing of PARP.
Cleavage of PARP in apoptotic Jurkat cells.
In (A) Jurkat cells were treated with agonistic anti-Fas Ab; in (B) Jurkat cells were coincubated with tumor cells. Experimental details are similar to those described in Figure 8. C2-10 anti-PARP mAb was used for blotting (Enzyme System, 1:7500).
Cleavage of PARP in apoptotic Jurkat cells.
In (A) Jurkat cells were treated with agonistic anti-Fas Ab; in (B) Jurkat cells were coincubated with tumor cells. Experimental details are similar to those described in Figure 8. C2-10 anti-PARP mAb was used for blotting (Enzyme System, 1:7500).
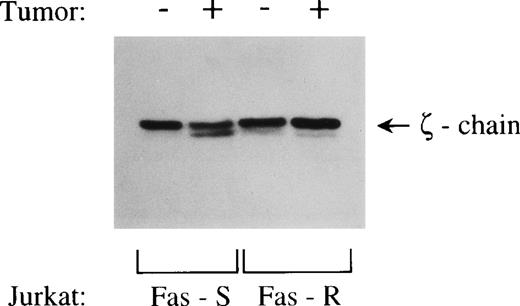
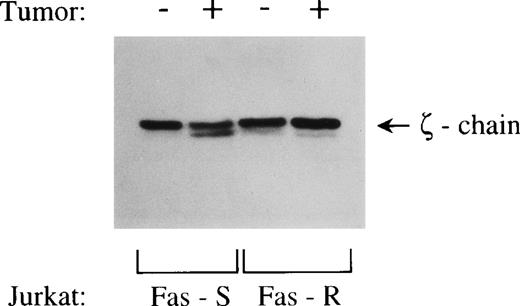
We have reported that reduced expression of TcR-ζ chain in T cells cocultured with tumor cells was related to T-cell apoptosis.8 In that study, the loss in expression of cytoplasmic TcR-ζ chain, as assessed by flow cytometry, was prevented in the presence of peptide inhibitors of caspases.8 We have also identified the TcR-ζ chain as a direct substrate for caspase-3 activity in a cell-free system, as well as in Fas-crosslinked Jurkat cells.50 To further investigate the link between caspase-mediated cleavage of ζ-chain and the tumor-induced loss of ζ-chain expression, Jurkat cells coincubated with tumor cells for 24 hours were lysed and examined by Western blotting for the presence of cleaved fragments. As shown in Figure 10, a ζ-chain fragment was detected in lysates of Fas-sensitive, but not Fas-resistant, Jurkat cells coincubated with PCI-13 cells and probed with the N-terminus–specific anti-ζ Ab. Since the C-terminal fragment of ζ-chain is being cleaved off and the epitope recognition site is presumably altered,50 a C-terminus–specific anti-ζ Ab would not detect the presence of a C-terminus deleted product. Therefore, previous studies detected only a loss in expression of full-length ζ-chain.51,52 Using N-terminus–specific anti-ζ Ab, we were able to detect tumor-induced cleavage products of ζ-chain. These results demonstrate that ζ-cleavage, shown previously to be caspase-mediated,50 is initiated by interaction with tumor cells.
Tumor-induced ζ-chain cleavage in Jurkat cells.
Fas-sensitive and Fas-resistant Jurkat cells were coincubated with tumor cells for 16 hours at a tumor-to-lymphocyte cell ratio of 20:1. Jurkat cells were then negatively selected by removal of tumor cells with the use of epithelial-specific anti-α6β4 mAb and magnetic beads. Negatively selected Jurkat cells were lysed and analyzed by Western blotting for expression of ζ-chain. N-terminus–specific anti-ζ Ab was used for probing.
Tumor-induced ζ-chain cleavage in Jurkat cells.
Fas-sensitive and Fas-resistant Jurkat cells were coincubated with tumor cells for 16 hours at a tumor-to-lymphocyte cell ratio of 20:1. Jurkat cells were then negatively selected by removal of tumor cells with the use of epithelial-specific anti-α6β4 mAb and magnetic beads. Negatively selected Jurkat cells were lysed and analyzed by Western blotting for expression of ζ-chain. N-terminus–specific anti-ζ Ab was used for probing.
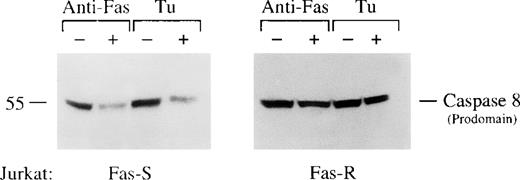
Tumor-mediated apoptosis in T cells overexpressing Bcl-2
The role of Bcl-2, an endogenous inhibitor of apoptosis, in tumor-induced apoptosis of lymphocytes was assessed in Jurkat cells stably transfected with a construct encoding epitope-tagged (KT3) Bcl-2 protein. Bcl-2 or Neo Jurkat cells were prelabeled with [3H]TdR and coincubated with agonistic anti-Fas Ab (200 ng/mL, CH-11) tumor cells (40:1 tumor-to-lymphocyte cell ratio) or VP-16 (20 μmol/L) for 8 to 24 hours. Apoptosis was assessed by loss of labeled DNA as measured by the JAM assay (Figure11). Although overexpression of Bcl-2 significantly inhibited DNA fragmentation induced in Jurkat cells by VP-16, it did not inhibit Fas-mediated DNA fragmentation induced by agonistic anti-Fas Ab or apoptosis induced by tumor cells. The failure of overexpressed Bcl-2 to protect lymphocytes from tumor-induced DNA fragmentation was also confirmed by a TUNEL assay performed in conjunction with CD3 staining (Figure 6). In these experiments, a similar proportion of apoptotic T cells was detected in Neo Jurkat (50%) and in Bcl-2 Jurkat (46%) cocultured for 16 hours with PCI-13 tumor cells. These results indicate that the intracellular pathway of death initiated in lymphocytes by interaction with tumor cells is not effectively regulated by Bcl-2.
Effects of overexpression of Bcl-2 in Jurkat cells on their susceptibility to tumor-mediated DNA degradation.
Bcl-2 or control Neo-transfected Jurkat cells were labeled with [3H]TdR and coincubated with tumor cells at a tumor-to-lymphocyte cell ratio of 40:1. As controls, these cells were treated with agonistic anti-Fas Ab (CH-11, 200 ng/mL) or VP-16 (20 μmol/L). Target cell apoptosis was determined at the indicated time points by measuring loss in 3H-labeled DNA in the JAM assay. The error bars represent the SEM of 8 replicates.
Effects of overexpression of Bcl-2 in Jurkat cells on their susceptibility to tumor-mediated DNA degradation.
Bcl-2 or control Neo-transfected Jurkat cells were labeled with [3H]TdR and coincubated with tumor cells at a tumor-to-lymphocyte cell ratio of 40:1. As controls, these cells were treated with agonistic anti-Fas Ab (CH-11, 200 ng/mL) or VP-16 (20 μmol/L). Target cell apoptosis was determined at the indicated time points by measuring loss in 3H-labeled DNA in the JAM assay. The error bars represent the SEM of 8 replicates.
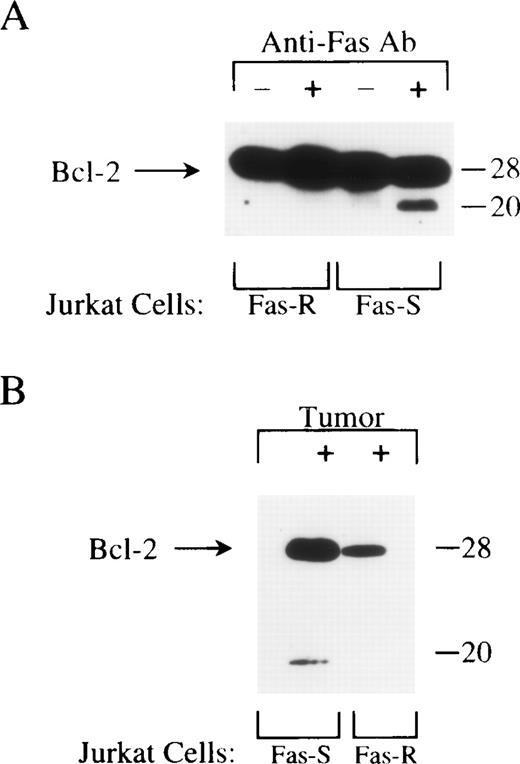
Tumor-induced cleavage of Bcl-2 in T cells
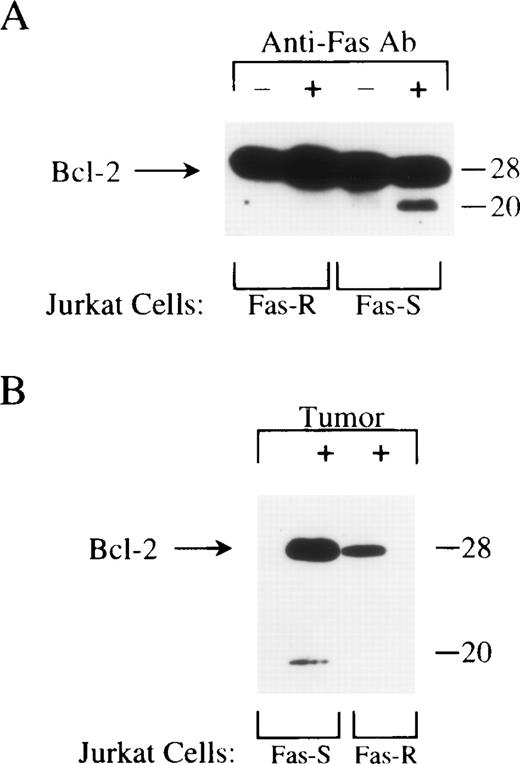
To further investigate the failure of Bcl-2 to block Fas- or tumor-mediated DNA degradation in lymphocytes, we performed Western blot analysis to assess possible changes in Bcl-2 expression following stimulation by either agonistic anti-Fas Ab or tumor cells. These studies revealed a cleaved fragment of Bcl-2 in Fas-sensitive, but not in Fas-resistant Jurkat cells triggered by anti-Fas Ab (Figure12A). Proteolytic cleavage of Bcl-2 has recently been reported in apoptosis induced by alphaviruses, Fas-ligation, or growth factors withdrawal.47 53 To test whether Bcl-2 is also cleaved by apoptosis induced in Jurkat cells by interaction with tumor cells, SCCHN PCI-13 cell line was cocultured with Fas-sensitive Jurkat or with Fas-resistant Jurkat cells at a tumor-to-lymphocyte cell ratio of 20:1 for 16 hours. At the end of the incubation period, Jurkat target cells were negatively selected by removal of tumor cells, lysed, and tested by Western blot analysis for expression of Bcl-2. Cleaved Bcl-2 was detected in Fas-sensitive Jurkat cells coincubated with tumor cells, but not in Fas-resistant Jurkat cells (Figure 12B). These results suggest that common effector molecules responsible for Bcl-2 cleavage were activated in T cells triggered by either tumor cells or anti-Fas agonistic Ab. Cleavage of Bcl-2 may, in part, explain its ineffective protection of T cells from apoptosis induced by tumor cells.
Cleavage of Bcl-2 in Jurkat cells treated with agonistic anti-Fas Ab or coincubated with tumor cells.
In (A), Fas-sensitive and Fas-resistant Jurkat cells were treated with CH-11 (200 ng/mL) for 16 hours. At the end of the incubation period, the cells were lysed and assessed by Western blotting for Bcl-2 expression (anti–Bcl-2 mAb 100, Santa Cruz). In (B), Fas-sensitive and Fas-resistant Jurkat cells were coincubated with tumor cell (20:1 tumor-to-Jurkat cell ratio) for 16 hours. At the end of the coincubation period, Jurkat lymphocytes were negatively selected by removal of tumor cells, using epithelial-specific anti-α6β4 mAb and magnetic beads. Negatively selected Jurkat cells were lysed and analyzed by Western blotting for expression of Bcl-2. Better separation between the Bcl-2 bands was observed in B than in A, owing to longer electrophoresis.
Cleavage of Bcl-2 in Jurkat cells treated with agonistic anti-Fas Ab or coincubated with tumor cells.
In (A), Fas-sensitive and Fas-resistant Jurkat cells were treated with CH-11 (200 ng/mL) for 16 hours. At the end of the incubation period, the cells were lysed and assessed by Western blotting for Bcl-2 expression (anti–Bcl-2 mAb 100, Santa Cruz). In (B), Fas-sensitive and Fas-resistant Jurkat cells were coincubated with tumor cell (20:1 tumor-to-Jurkat cell ratio) for 16 hours. At the end of the coincubation period, Jurkat lymphocytes were negatively selected by removal of tumor cells, using epithelial-specific anti-α6β4 mAb and magnetic beads. Negatively selected Jurkat cells were lysed and analyzed by Western blotting for expression of Bcl-2. Better separation between the Bcl-2 bands was observed in B than in A, owing to longer electrophoresis.
Discussion
Our recent studies have suggested that coincubation of Jurkat T cells or peripheral T lymphocytes of cancer patients with tumor cells results in T-cell apoptosis.8,50 The biological relevance of this finding became further apparent when similar observations were made in vivo.12,54,55 An excessive death of lymphocytes at the tumor site may represent a mechanism of tumor-induced immunosuppression. Apoptosis of lymphocytes interacting with tumor cells could result from a direct engagement of death receptors expressed on lymphocytes with death ligands expressed on tumor cells. Indeed, recent studies have suggested that apoptosis-inducing proteins, such as FasL, are expressed on tumors and might be actively engaged in modulation of the immune response in situ.1,3,4,8,56However, additional mechanisms of induction of apoptosis may exist at the tumor site, including up-regulation of death receptors and/or their ligands on lymphocytes, leading to autocrine or paracrine stimulation of cell death.13 14 The present study investigated the intracellular effector molecules involved in the execution of the apoptotic cascade induced in lymphocytes by tumor cells. Characterization of the molecular mechanisms involved in T-cell death in the tumor microenvironment may have important implications for therapeutic regimens, including vaccination strategies and adoptive transfer of activated T cells into patients with cancer.
Evidence for the ability of human SCCHN cells to induce apoptosis in interacting lymphocytes was obtained by various detection methods of apoptosis, including degradation of DNA, as assessed by the JAM or TUNEL assays; appearance of changes in mitochondria permeability transition, as assessed by loss of DiOC6 staining; and enhanced activity of caspase-3–like enzymes, as assessed by cleavage of a cell-permeable fluorescent DEVD substrate. The Fas-FasL pathway appears to be involved in T-cell apoptosis induced by SCCHN cells, since it was partly inhibited by neutralizing anti-FasL Ab.
Ectopic expression of CrmA has been shown to inhibit apoptosis triggered by ligation of death receptors, but not apoptosis triggered by cytokine withdrawal or ionizing radiation.57,58 In the present study, overexpression of CrmA provided partial protection to T cells from tumor- or Fas-mediated apoptosis at an early period after stimulation of apoptosis. Since caspase-8 is a major target of CrmA inhibitory effect, the observed protection appears to be mediated by direct inhibition of caspase-8, which actively participates in execution of tumor-induced apoptosis of T cells. Overexpression of CrmA also effectively inhibited the processing of pro–caspase-3 into active subunits. Since CrmA is not an efficient inhibitor of caspase-3, the inhibition of caspase-3 processing appears to represent an indirect effect of CrmA-inhibited caspase-8.59 60 Although overexpression of CrmA effectively inhibited the activation of caspase-3, only partial inhibition of PARP cleavage was observed in CrmA cells ligated by anti-Fas Ab. Since caspase-3 appears only as an inactive proform in CrmA cells, the partial cleavage of PARP may be executed by redundant caspases with cleavage site specificity similar to that of caspase-3.
In Jurkat cells coincubated with tumor cells, activation of caspase-3 differed from that in Jurkat cells treated with anti-Fas Ab. Whereas Fas crosslinking by agonistic anti-Fas Ab resulted in processing of all the detectable pro–caspase-3 (p32) into p17, only partial processing of the pro-domain was observed in tumor-triggered T cells. Also, in contrast to the generation of p17 alone in Fas-mediated apoptosis, both p17 and p20 were detected in Jurkat cells coincubated with tumor cells. Although the presence of caspase-3 active subunit, p20, was detected in Fas-resistant Jurkat cells, its activity appears to be blocked, since viability and growth of these cells were not affected by Fas crosslinking. Furthermore, PARP or TcR-ζ chain cleaving activity was not detected in these cells.
We have recently reported that the ζ-chain is a direct substrate for caspase-3 in a cell-free system, as well as in cells triggered by anti-Fas Ab.50 However, generation of ζ-chain cleavage products in T cells interacting with tumor cells has not yet been reported. In this study, we obtained evidence demonstrating that tumor-induced activation of intracellular caspases plays a role in ζ-chain degradation. While in previous studies the use of Cterminus–specific anti-ζ Ab allowed only detection of loss in full-length ζ-chain, in the current study, the use of N-terminus–specific anti-ζ Ab revealed the presence of ζ-chain cleaved products in coculture of Jurkat and tumor cells. This is the first direct evidence that tumor-induced alteration in expression of ζ-chain is mediated by protein degradation.
Bcl-2 has been shown to be a potent inhibitor of apoptosis induced by various stimuli, including growth-factor deprivation, irradiation, and cytotoxic drugs.61 Anti-apoptotic Bcl-2 family members bind to mitochondria and inhibit cytochrome-c release.62,63Recent studies confirmed the ability of Bcl-2 to also act downstream of cytochrome-c release, binding to Apaf-1 or caspase-9.26,64-66 However, Bcl-2 does not regulate activity of caspases upstream of the mitochondria.67,68Although Bcl-2 has been reported to protect hepatocytes, P815 mastocytoma, B-cell lymphoma, and certain clones of Jurkat cells from Fas-mediated apoptosis, its ability to protect lymphocytes has been controversial.69,70 In our studies, Jurkat cells overexpressing Bcl-2 were not protected from tumor- or Fas-induced DNA degradation. The cleavage of Bcl-2 may provide an explanation for its ineffective protection. However, most of the intracellular Bcl-2 remained unprocessed, even at 24 hours after Fas crosslinking, when 90% of the cells were positive for apoptosis. Although the unprocessed Bcl-2 did not protect Jurkat cells from ultimate DNA-degradation, it was biologically active, as demonstrated by a partial processing of p32 caspase-3 or PARP in Bcl-2-Jurkat, as compared with full-processing in Neo control-Jurkat. However, this inhibitory activity of Bcl-2 was not sufficient to block the progress of the apoptotic cascade toward DNA fragmentation. Recent studies suggest that Bcl-2 can interfere with Fas-mediated apoptosis only in those cells where recruitment or activation procaspase-8 is not efficient.68 This has been suggested by a recently described mechanism of cross-talk between caspase-8 and caspase-9 via mitochondria.71-73 This cross-talk is mediated by BID, a proapoptotic member of the Bcl-2 family, which is cleaved by caspase-8, and its C-terminal fragment translocates to the mitochondria and triggers cytochrome-c release. Depletion of BID from cytosolic extracts disrupts the ability of caspase-8 to trigger cytochrome-c release in vitro.72 BID-induced cytochrome c/Apaf-1 pathway may serve to amplify the caspase-8 cascade. Thus, it appears that anti-apoptotic Bcl-2 family members can suppress Fas-induced apoptosis only in those cells where the mitochondrial amplification loop is of significance. The role of mitochondria in tumor-induced apoptosis of T lymphocytes is currently under investigation.
In summary, tumor-induced apoptosis of lymphocytes may combine the engagement of various apoptotic stimuli and pathways. Therefore, it is important to identify those intracellular apoptotic events that might be potential targets for therapeutic intervention in the future. The current study is the first to identify intracellular components involved in execution or inhibition of apoptotic cascades induced in lymphocytes interacting with SCCHN cells.
Supported by grants from The Pittsburgh Foundation (H.R.); The Wendy Will Case Cancer Fund, Inc (H.R.); American Cancer Association, Grant RPG-98-288-01-CIM (H.R.); and The National Cancer Institute, Grant PO1DE 12321-01 (T.L.W., H.R.).
Reprints:Hannah Rabinowich, University of Pittsburgh Cancer Institute, W952 Biomedical Science Tower, 200 Lothrop Street, Pittsburgh, PA 15213; e-mail: rabinow+@pitt.edu.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.

![Fig. 1. Tumor-induced apoptosis of Jurkat cells as assessed by the JAM assay, flow cytometry TUNEL, and loss in DiOC6 staining of mitochondria. / (A) Apoptosis of Jurkat cells as assessed by the JAM assay. Various SCCHN cell lines were coincubated with [3H]TdR-labeled Jurkat cells at a 40:1 tumor-to-lymphocyte cell ratio for 16 hours. Treatment with agonistic anti-Fas Ab (CH-11, 200 ng/mL) served as positive control for apoptosis. Target cell death was determined by measuring fragmentation of 3H-labeled target cell DNA. The error bars represent the SEM of 8 replicates. (B) Apoptosis of Jurkat cells as assessed by flow cytometry TUNEL. Fas-sensitive or Fas-resistant Jurkat cells were treated with agonistic anti-Fas Ab (CH-11, 200 ng/mL) or coincubated with PCI-13 (tumor-to-lymphocyte cell ratio of 40:1) for 16 hours. The cells were then stained with anti–CD3-PE, fixed, and stained for DNA breaks by TUNEL. TUNEL staining was assessed by flow cytometry in CD3+-gated cells. The percentage of TUNEL positive cells is indicated at the right corners. (C) Apoptosis of Jurkat cells as assessed by loss in DiOC6 staining of mitochondria. Fas-sensitive Jurkat cells, incubated in medium alone or with PCI-13 tumor cells (tumor-to-lymphocyte cell ratio of 40:1) for 16 hours, were stained for DiOC6 (40 nmol/L, 15 minutes, 37°C) and then, without fixation, stained by PE-conjugated anti-CD3 Ab on ice. Results shown in A, B, and C were reproduced in at least 3 different experiments.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/95/6/10.1182_blood.v95.6.2015/6/m_bloo00630001x.jpeg?Expires=1766198548&Signature=raYvLp~H1Uj7VJatuGdgkn1TgMX1UT9U6hV7kFgOpeLBWEJHBwZLmNLj5DDRL5l6Rrc16e~C5CBkvGQv0T1V7hIQjgl95oUbKFqp~kJwICvzdRu-S10eYggyZV0sUIsXMwB8VKQE7N8LkQUFMBSwzdP7OmiiPU9qlubPMsvCN2j54BePWTml85Ysc9hw2aN-RB3tmTYTRh3XzG9yZ5mIFYoQusPvq~U9iP~i-1wyLPerkEhJBWqEYUKfby3aeHilpA449GjMXL~2aFyi3sxnrTwEI~RmUSaTe82o1kGP9GYxcw-I88905fgLN7~hnsG07nBGsmAHf-kSJK2oQqdT4Q__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 2. Involvement of Fas/FasL in tumor-induced apoptosis of T cells. / (A) Inhibition of tumor-mediated apoptosis of Jurkat cells by anti-FasL Ab. [3H]TdR-labeled Jurkat cells were treated for 2 hours with anti-FasL Ab (4H9) or with a hamster IgG control at various concentrations, as indicated. Target cell death was determined at 16 hours by measuring fragmentation of 3H-labeled DNA. The error bars represent the SEM of 8 replicates. (B) Reduced sensitivity of Fas-resistant Jurkat cells to PCI-13–mediated apoptosis. Fas-resistant Jurkat cells were obtained as described in “Materials and methods.” [3H]TdR-labeled Fas-sensitive and [3H]TdR-labeled Fas-resistant Jurkat cells were coincubated with PCI-13 cells (tumor-to-Jurkat ratio, 80:1) or anti-Fas (CH-11) Ab for 16 hours, and tested for apoptosis by JAM assay.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/95/6/10.1182_blood.v95.6.2015/6/m_bloo00630002x.jpeg?Expires=1766198548&Signature=z9LGUWzAUAFN5YVMhALdYE2J5wSCPTFAi9cMYWYLTBdMb~cd7~9LAkvjT2KeK7JJWParZt39IiZ9-wGcnw0LpaC~fYagonDWQayFV9UYM0I9ZXpqIrtzWDNhY7gmurpKWk58Dxu8pd36rhWSuVuHSrHM2JNHtist3FWLNNp6I3UhCCCouAgcVkuuCmv5ljWtwiGNZfjd1~FxeOHtAWOvgLEdHLs8nEGg0h8tP-RrjIQOnHnNauKVtyjQ16kajLW3EvErfoxqjayGOaZJt5xvbBXsEcaXXHMCPtKPTkQR4OevOrEtfhSZySxjIKRVGX9TifnU0i67JGFba~oZNctptw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 3. Effects of peptide inhibitors of caspases on Fas- or tumor-induced DNA degradation in Jurkat cells. / [3H]TdR-labeled Jurkat cells were pretreated with Z-VAD-FMK or Z-DEVD-FMK at the indicated concentrations for 16 hours and then coincubated with tumor at a 40:1 tumor-to-lymphocyte cell ratio for an additional 16 hours. Jurkat cell apoptosis was determined by measuring the loss of 3H-labeled DNA. The error bars represent the SEM of 8 replicates. Similar results were obtained in the absence of inhibitors or in the presence of the control inhibitor Z-FA-FMK.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/95/6/10.1182_blood.v95.6.2015/6/m_bloo00630003x.jpeg?Expires=1766198548&Signature=xewUOJEe2r~StliZgMosjuldu2xOUNwYlL5Y06xGnpXlrKsC5x1QqBUQDwSVx~9hYcXgDN-eUMOPi9wypbrYtAOvzhSMfZ9g-BglIvnTXCqRUQ6CUSWnHJm~EAsxHFIg4nYCRCR4soeePYioq8a3U5Cw95iPNlP3BtA93U7VJaaYYltwYmnipPUVDrvVdt7nfgqJ7LJYdVL1Um53sOXKapJ1oeDYUvhXz~0SldnaI9416cUdyD8PQHaW4IyiijFeiuP1WrPyS11eMFHWN6-ciGntoLWInf9Wd6gzl2D0qHKHtSY4PEjswHyyHfj2Ncik72t4~bKEn6n7LbKZUGRpiA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 5. Effects of CrmA overexpression on the susceptibility of Jurkat cells to tumor-mediated apoptosis. / CrmA or control Neo-Jurkat cells were labeled with [3H]TdR and coincubated with tumor cells at a tumor-to-lymphocyte cell ratio of 40:1. As controls, these cells were treated with agonistic anti-Fas Ab (CH-11, 200 ng/mL) or VP-16 (20 μmol/L). Target cell death was determined at the indicated time points by measuring loss in 3H-labeled DNA. The error bars represent the SEM of 8 replicates.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/95/6/10.1182_blood.v95.6.2015/6/m_bloo00630005x.jpeg?Expires=1766198548&Signature=F2KMrenttnKI7VGSkZUPNqsSFIpQd8GF48WwX4BPNstA7YYTcDFB97XcQ33dpRsvZ8pkJVevx90ClZeam3Tv1E0Z5NQ2ICSzw4fhg2FtdDpZCibyxRGZGc32ZgwNcv5lxSgWj6H-wkfvlhvUpPlRTHnQk9FeSWNx9F-e~e2ca7igpKiNTAJNrq-o4ZlRE~TFvC1CkFiJO7e111BUb9CHPMDh0cgWZZ6raCdjN7JWY0XgIyjdnsdmHbQhkzKf8JgyOE8dWATxqkmxQ9zRBNXzt17NrFLx5QsasczVXS-oCMJBZhPwEoLPBN6VcoGP9gk~0SNai56vphoOKFAF4MyYiA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 11. Effects of overexpression of Bcl-2 in Jurkat cells on their susceptibility to tumor-mediated DNA degradation. / Bcl-2 or control Neo-transfected Jurkat cells were labeled with [3H]TdR and coincubated with tumor cells at a tumor-to-lymphocyte cell ratio of 40:1. As controls, these cells were treated with agonistic anti-Fas Ab (CH-11, 200 ng/mL) or VP-16 (20 μmol/L). Target cell apoptosis was determined at the indicated time points by measuring loss in 3H-labeled DNA in the JAM assay. The error bars represent the SEM of 8 replicates.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/95/6/10.1182_blood.v95.6.2015/6/m_bloo00630011x.jpeg?Expires=1766198548&Signature=lewwQKRhm7aT~NglQupcxwhljdGBkFVSWkrs6271JBwxFruuCan4PfFaT-3~olBFb8Bw9o30rjgJFn6qQtb~ZQvyG41diIGH7rPdfhX1QQVqiK2fv9y28BVvg-4J98NR1oICTyif5UUpqX8sB3~vh2dy2QWWh5Jjv10XRHZS-r8vCapzd90fxMlDak4dvamZhtYqe-pqkgDQg8n7q7c1Y1PHkFH1DT7~XkPSB6KxcFX5DHl89xJtqTet0-kiCPTLYTOTyI5mI2XUWiat2U2cgaSOeTlBUAgHUJc9KeJJqPNvFgO5GDY4-6c4JLFBSLHLtiMNzSXKZ4OFKfvyPjLn-g__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)

![Fig. 1. Tumor-induced apoptosis of Jurkat cells as assessed by the JAM assay, flow cytometry TUNEL, and loss in DiOC6 staining of mitochondria. / (A) Apoptosis of Jurkat cells as assessed by the JAM assay. Various SCCHN cell lines were coincubated with [3H]TdR-labeled Jurkat cells at a 40:1 tumor-to-lymphocyte cell ratio for 16 hours. Treatment with agonistic anti-Fas Ab (CH-11, 200 ng/mL) served as positive control for apoptosis. Target cell death was determined by measuring fragmentation of 3H-labeled target cell DNA. The error bars represent the SEM of 8 replicates. (B) Apoptosis of Jurkat cells as assessed by flow cytometry TUNEL. Fas-sensitive or Fas-resistant Jurkat cells were treated with agonistic anti-Fas Ab (CH-11, 200 ng/mL) or coincubated with PCI-13 (tumor-to-lymphocyte cell ratio of 40:1) for 16 hours. The cells were then stained with anti–CD3-PE, fixed, and stained for DNA breaks by TUNEL. TUNEL staining was assessed by flow cytometry in CD3+-gated cells. The percentage of TUNEL positive cells is indicated at the right corners. (C) Apoptosis of Jurkat cells as assessed by loss in DiOC6 staining of mitochondria. Fas-sensitive Jurkat cells, incubated in medium alone or with PCI-13 tumor cells (tumor-to-lymphocyte cell ratio of 40:1) for 16 hours, were stained for DiOC6 (40 nmol/L, 15 minutes, 37°C) and then, without fixation, stained by PE-conjugated anti-CD3 Ab on ice. Results shown in A, B, and C were reproduced in at least 3 different experiments.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/95/6/10.1182_blood.v95.6.2015/6/m_bloo00630001x.jpeg?Expires=1767480553&Signature=xjW9n4g96OUg7ipfepDMzr87fYhEvXnY0acF21QXkk5Y4yLhrZ7d1j~3J6TYH2hOp9RPeBBArJlfiup4T0P2mkE8qtNFc7Vvs8UcYwfBTDIfwsIon~cNuVDs4NH3EU5hkkLXZYgzPd3bsEcY4rHXW6P4LjTsIvwd4RhpPdqrHN~5dtfJclllyf7tQwxN9XVwgbU8qRs26VwG2djm6CBI2GH00-5HCuCtrmv9KWK0jHYuVhW3r6PTTRCYBr-hM8tw8nEk7gmOz8MgZxf43vI2M7NlEdQHT5YTXAFQYTpZVMlJvHwmn2QnUbuLaVtHSJrbBnYkXMi~wxyeqLtW4dl9Xw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 2. Involvement of Fas/FasL in tumor-induced apoptosis of T cells. / (A) Inhibition of tumor-mediated apoptosis of Jurkat cells by anti-FasL Ab. [3H]TdR-labeled Jurkat cells were treated for 2 hours with anti-FasL Ab (4H9) or with a hamster IgG control at various concentrations, as indicated. Target cell death was determined at 16 hours by measuring fragmentation of 3H-labeled DNA. The error bars represent the SEM of 8 replicates. (B) Reduced sensitivity of Fas-resistant Jurkat cells to PCI-13–mediated apoptosis. Fas-resistant Jurkat cells were obtained as described in “Materials and methods.” [3H]TdR-labeled Fas-sensitive and [3H]TdR-labeled Fas-resistant Jurkat cells were coincubated with PCI-13 cells (tumor-to-Jurkat ratio, 80:1) or anti-Fas (CH-11) Ab for 16 hours, and tested for apoptosis by JAM assay.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/95/6/10.1182_blood.v95.6.2015/6/m_bloo00630002x.jpeg?Expires=1767480553&Signature=SLjgoQwFMNQi~KWRCOcnaCfsRRwtopdvVi80KFnptactmEfU4~SQnmTZL9h0jfPxGKK5DXsv3Ns7KHhx~8Q4GsXft7aGwh5WKgDhb1uzATqRPKtwjZLEaONKClq4g6p56cByom6URzlgQhuTl4tKYUg~fUEJScaDJBiTdEQzCbiIakedwrl4e3WJNZRtbxOmxhf7tmWAUxmEfHVFOjA3w2aw9FWuEdKCA41eZegb04F5nO4RxV6TQrWMv52eE~C7-xLmAcHUArkhxpvhjVGaAK5we643e6SyE~n-LSDRXk~9LN-eu~C8YCTd~KWfgrmsgqT50m09iYiyOgNBkn3FfA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 3. Effects of peptide inhibitors of caspases on Fas- or tumor-induced DNA degradation in Jurkat cells. / [3H]TdR-labeled Jurkat cells were pretreated with Z-VAD-FMK or Z-DEVD-FMK at the indicated concentrations for 16 hours and then coincubated with tumor at a 40:1 tumor-to-lymphocyte cell ratio for an additional 16 hours. Jurkat cell apoptosis was determined by measuring the loss of 3H-labeled DNA. The error bars represent the SEM of 8 replicates. Similar results were obtained in the absence of inhibitors or in the presence of the control inhibitor Z-FA-FMK.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/95/6/10.1182_blood.v95.6.2015/6/m_bloo00630003x.jpeg?Expires=1767480553&Signature=io4GTdCC8e0OungHKvrLjjjGqUO9HvhIEnSocQW7UMHeQGjMj~SR5B5d-eZNc0EhMMT0xb8If4tagexBkTOz5DmhWbaqmNz0kcKIQDmGJrOlNpAsW9UtEPzbWr9pZg4mUu9H3uIsw3fyhNgKSl8QaVvCXMnDsX3~QDfQ9rBnFXfvAXUoR2dgoGxfweXNZGzNIMLA-Ma63hb7s3BhlkU73HBnbqXKZhNPPv7tzIYbJnEntyA-7lPMWwRQcZugk9qyyy-o7Cr~68ZCEuuOzOXskBkXWYssZQO-nWFeIQZoRgkHKdOWwwAyPKc0RNICyVZvR0QaZKFlREcHefmkGx2Uxg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 5. Effects of CrmA overexpression on the susceptibility of Jurkat cells to tumor-mediated apoptosis. / CrmA or control Neo-Jurkat cells were labeled with [3H]TdR and coincubated with tumor cells at a tumor-to-lymphocyte cell ratio of 40:1. As controls, these cells were treated with agonistic anti-Fas Ab (CH-11, 200 ng/mL) or VP-16 (20 μmol/L). Target cell death was determined at the indicated time points by measuring loss in 3H-labeled DNA. The error bars represent the SEM of 8 replicates.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/95/6/10.1182_blood.v95.6.2015/6/m_bloo00630005x.jpeg?Expires=1767480553&Signature=tNaOPs95EvC-ljlnvy3q-FSoyGTP~vAi77-Q7zQxbbA6taY9x~at2n7B6ba0moynTV3aFO8YJzK87XRaeaiQ6eUS3hYV-KNm71WlFpPtXajCKNZUMGjXyGkK5mMDUitm3my8kLs-I35KTj76P9-di9qI9Mh~tMJDz-rg27MruFhOBeIQjcAWD~h7jDLyJqSEqREszZsjJsVe0Dp8KHQA25EQMi7op9ol1L0Bm2m~UojYAz0NyNHFN0X6LB~gAcsI5P3Xa-FOEOUgXQctuMVkg1xWK12qtDogUGgLNshRTrmzKzrBnLe0pp71tu4ekP~9z9OTHx7QdZClKuEz1Gq1Bg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 11. Effects of overexpression of Bcl-2 in Jurkat cells on their susceptibility to tumor-mediated DNA degradation. / Bcl-2 or control Neo-transfected Jurkat cells were labeled with [3H]TdR and coincubated with tumor cells at a tumor-to-lymphocyte cell ratio of 40:1. As controls, these cells were treated with agonistic anti-Fas Ab (CH-11, 200 ng/mL) or VP-16 (20 μmol/L). Target cell apoptosis was determined at the indicated time points by measuring loss in 3H-labeled DNA in the JAM assay. The error bars represent the SEM of 8 replicates.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/95/6/10.1182_blood.v95.6.2015/6/m_bloo00630011x.jpeg?Expires=1767480553&Signature=N-Bo-VuIzcGDqEWSLpUhH2TY6PANuD5~geja2Qbo86jRQGmECHuSObMeExAObfXtkdRWY2rwJ5hsLR3nb18UP~PGjb6hFy2niOWH8ifF9nNTMwKRBTycr0hVSuzDKfEWqOS-Hy7HT8JHpD3aYXRLrSCOagJ5fGgIQACVd5EXLJMP2kc9jG0Rr~UflIWFk7OlYTJsmf6LK-l1dobxKPz2Wm-drKSJ~Um1HGBsFXhrgNHANuJF9zK7z0Cl40zTNAGXD9sPjOWWqnPj7lAnFZ8~aZ8ypC2lI7JtdHmGDcRLzXgZJEY-g8VrK78rRTLVuJD~w04-3NftIrDJcn6roHc3sw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)