Abstract
The totipotent mouse embryonic stem (ES) cell is known to differentiate into cells expressing the β-globin gene when stimulated with bone morphogenetic protein (BMP)-4. Here, we demonstrate that BMP-4 is essential for generating both erythro-myeloid colony-forming cells (CFCs) and lymphoid (B and NK) progenitor cells from ES cells and that vascular endothelial growth factor (VEGF) synergizes with BMP-4. The CD45+ myelomonocytic progenitors and Ter119+ erythroid cells began to be detected with 0.5 ng/mL BMP-4, and their levels plateaued at approximately 2 ng/mL. VEGF alone weakly elevated the CD34+ cell population though no lymphohematopoietic progenitors were induced. However, when combined with BMP-4, 2 to 20 ng/mL VEGF synergistically augmented the BMP-4-dependent generation of erythro-myeloid CFCs and lymphoid progenitors from ES cells, which were enriched in CD34+ CD31lo and CD34+CD45− cell populations, respectively, in a dose-dependent manner. Furthermore, during the 7 days of in vitro differentiation, BMP-4 was required within the first 4 days, whereas VEGF was functional after the action of BMP-4 (in the last 3 days). Thus, VEGF is a synergistic enhancer for the BMP-4-dependent differentiation processes, and it seems to be achieved by the ordered action of the 2 factors.
It is widely accepted that development of the hematopoietic system during early embryogenesis is initiated by the commitment of certain splanchnopleuric mesodermal cells (derived from the pluripotent epiblasts) into hematopoietic and endothelial cell lineages.1 Embryologic and genetic analyses inXenopus, zebrafish, and mice have led to the discovery of a number of gene products that play important roles in the embryonic generation of primitive and definitive hematopoietic cells.2,3 For some gene products, a temporal order of action has also been proposed. However, definition of the specific cellular events occurring during this process remains largely unresolved. Therefore, taking advantage of the capacity of totipotent embryonic stem (ES) cells, isolated from the inner cell mass of the mouse preimplantation embryo, to differentiate in vitro into cells of the lymphohematopoietic lineages,4-17 others and we have begun to address this problem by characterizing the intermediate cells in the differentiation pathway and evaluating extracellular factors driving this pathway.
Recent progress in understanding the differentiation pathway from ES cells to lymphohematopoietic cell lineages has been made primarily from surface marker analysis using fluorescence-activated cell sorting (FACS). ES cells express E-cadherin, a marker for the epiblast of the mouse embryo, which is quickly replaced by CD44.17-19 A fraction of differentiating ES cells also starts to express the vascular endothelial growth factor (VEGF) receptor-2 (VEGFR-2 or flk-1) protein. These cells represent the lateral mesodermal cell type, an important intermediate for later hematopoietic cell development.19 In fact, the flk-1+ cells include hematopoietic colony-forming activity18 whereas the vascular endothelial (VE)-cadherin+ flk-1+subpopulation has the potential to give rise to both endothelial and erythro-myeloid cells in vitro.19-21 These observations have been confirmed with aorta-gonad-mesonephros-derived and yolk sac-derived cells with similar cell surface characteristics.22 We have also demonstrated that the CD34+ progeny derived from ES cells, which seem to appear later than the VE-cadherin+ flk-1+cells,19,23 are enriched for lymphohematopoietic progenitor cells.17
In contrast, the question of how the roles of extracellular signaling molecules that had been defined by in vivo studies would fit into the in vitro differentiation pathway from ES cells has not been fully addressed. It has been known that BMP-2/4 is required for hematopoietic cell genesis during the early embryogenesis of Xenopus and zebrafish.24-27 Furthermore, essential roles of BMP-4 on mesoderm induction28 and the flk-1 signal transduction on primitive and definitive hematopoietic cell development have also been demonstrated in mice.29-32 Therefore, a physiologic differentiation culture for ES cells to lymphohematopoietic cell lineages should be dependent at least on BMP-4 and flk-1 ligand (including VEGF). However, none of the available culture methods has been 2-factor dependent, probably because they are supplemented with fetal calf serum (FCS) or plasma, which contains sufficient extracellular factors for the whole differentiation process to proceed. Even the stringent in vivo requirement of the flk-1 function was not reproduced in vitro with serum-containing culture methods32,33; however, positive effects of exogenously added VEGF on the in vitro hematopoietic progenitor cell development were reported.17,34 In this respect, Wiles and Johansson35 36 have already shown that in serum-free, chemically defined medium, BMP-4 is absolutely necessary for erythroid cell development from ES cells.
Here we demonstrate, with a modified serum-free culture method, that the process of lymphohematopoietic cell development from ES cells in vitro is, in fact, dependent on BMP-4 and VEGF. Under this condition, BMP-4 is essential for the generation of all types of erythro-myeloid CFCs and of B and NK lymphoid progenitors. On the other hand VEGF, which does not induce lymphohematopoietic potentials alone, shows marked enhancement of the BMP-4-dependent lymphohematopoietic cell genesis. Furthermore, this action of VEGF seems to follow that of BMP-4. Possible roles of VEGF as a synergistic cofactor for BMP-4 during early embryogenesis are discussed.
Materials and methods
Cells and reagents
The A3-1 ES cell line and OP9 stroma cell line were obtained as described before,17 and the E14 ES cell line was kindly provided by C. Saris at Amgen (Thousand Oaks, CA). Iscove's modified Dulbecco's medium, α-minimum essential medium, and phosphate-buffered saline without Mg2+ and Ca++ (PBSA) were purchased from Gibco (Gaithersburg, MD). All the tissue culture flasks and plates were from Falcon (Franklin Lakes, NJ).
Recombinant human erythropoietin (EPO), human leukemia inhibitory factor (LIF), human granulocyte colony-stimulating factor (G-CSF), human interleukin (IL)-2, mouse IL-3, human IL-6, and rat stem cell factor (SCF) were prepared at Amgen. Recombinant human BMP-4, mouse IL-7, mouse VEGF, and mouse granulocyte macrophage colony-stimulating factor (GM-CSF) were purchased from R&D Systems (Minneapolis, MN). The monoclonal antibody for mouse CD34 (clone RAM34) conjugated with fluorescein isothiocyanate (FITC) was purchased from Pharmingen (San Diego, CA). Phycoerythrin (PE)-conjugated monoclonal antibodies for mouse B220 (clone RA3-6B2), CD19 (clone 1D3), CD31 (clone MEC13.3), CD45 (clone 30F11), Sca-1 (clone E13-161.7), and Ter119 were also purchased from Pharmingen. For FACS, monoclonal antibody for mouse CD16/CD32 (clone 2.4G2) from Pharmingen was added for blocking nonspecific staining.
Maintenance of embryonic stem cells and induction of differentiation by the embryoid body formation method
Both A3-1 and E14 ES cells were maintained and differentiated in a serum-containing medium as described before17 except that the differentiation medium contained 0.9% methylcellulose (Stem Cell Technology, Vancouver, Canada) and the dish used for the embryoid body (EB) formation was made of polymethylpentene (Nalge-Nunc, Milwaukee, WI). The serum-free differentiation was performed by replacing FCS with Knockout-SR (Gibco) from the preculture stage, and standard bacterial-grade polystyrene dishes were used for the EB formation. Knockout-SR is a bovine serum albumin (BSA) solution with lipids, vitamins, trace elements, and low concentrations of transferrin and insulin. The initial cell concentration was 500 to 700 cells/mL for the serum-containing culture and 2500 to 4500 cells/ml for the serum-free culture. The differentiation culture included 100 ng/mL SCF unless otherwise stated.
Harvesting and staining EB cells for FACS
Embryoid bodies were collected, washed twice with PBSA, and resuspended in 0.25% (wt/vol) collagenase mix in 15% FCS containing PBSA. The collagenase mix is a 1:1 mixture of Collagenase D (Boehringer Mannheim, Mannheim, Germany) and Collagenase XI (Sigma, St Louis, MO). The EBs were incubated at 37°C for 60 minutes and dissociated into a single-cell suspension by passing through a 20-gauge needle. Remaining small aggregates were removed by filtration through a 40-μm mesh (Falcon). The EB cells were spun and resuspended in 0.5% BSA (Path-O-Cyte 4; Miles, Kankakee, IL) in PBSA at 5 × 106 cells/mL. Cells were stained with 2 to 20 μg/mL antibodies. Stained samples were analyzed on a FACScan (Becton Dickinson, San Jose, CA) or were sorted for CD34, CD31, and CD45 markers using a Vantage cell sorter (Becton Dickinson).
For factor-exchange experiments, EBs were collected on day 4 and washed once with PBSA, and half of them were subjected to the same collagenase treatment for FACS analysis. The rest were replated in the serum-free methylcellulose medium in the presence of a different set of factors and were analyzed in the same way on day 7.
Colonogenic cell assay
Total EB cells obtained through the collagenase-treatment were mixed with the 1% methylcellulose (Stem Cell Technology) containing CFC medium17 and distributed onto 2 to 4 35-mm bacterial-grade dishes at 5 × 104 cells/plate. For erythroid progenitors, 100 ng/mL SCF, 10 ng/mL IL-3, and 3 U/mL EPO were added to the culture, and colony forming unit (CFU)-erythrocyte (E), burst forming unit (BFU)-E, and CFU-Emix (CFU-EM(macrophage) + CFU-n(neutrophil)E + CFU-mastE + CFU-nEM + CFU-mastEM) were counted on day 8. For myeloid colonies, 100 ng/mL SCF, 10 ng/mL IL-3, 10 ng/mL GM-CSF, 50 ng/mL G-CSF, and 25 ng/mL IL-6 were added, and CFU-M, CFU-n/mast (CFU-n + CFU-mast), and CFU-nonEmix (CFU-nM + CFU-mastM) were counted on day 9. For FACS purified EB cells, 0.5 to 1 × 104 cells were plated per 35-mm dish, cultured in the presence of 100 ng/mL SCF, 10 ng/mL IL-3, 10 ng/mL GM-CSF, 50 ng/mL G-CSF, 25 ng/mL IL-6, and 3 U/mL EPO for 9 days, and all types of colonies were counted at once.
Stroma coculture method for developing lymphokine-activated killer cells and pre-B cells from embryoid body cells
The lymphoid potential in total and in a subfraction of EBs was quantified based on the “switch” culture method described before.17 First, the OP9 stroma cell line was maintained and prepared for coculture. Then total EB cells or FACS-purified EB cells were seeded at 5 × 103 to 4 × 104 cells/well (6-well plate) on a confluent layer of OP9 and cultured in the low-serum medium17 with 100 ng/mL IL-2 and 5 ng/mL IL-7. The medium was changed one-third to one-half volume every 3 days. Generation of pre-B cells and lymphokine-activated killer (LAK) cells was quantified first by visually counting hematopoietic cell foci on day 10 or 11, which were reinspected under the microscope to further distinguish them between the dense pre-B-type foci, and hallow-containing LAK-type foci on day 14 or 15. Nonadherent cells and loosely attached cells were then mechanically harvested; this was followed by FACS phenotyping using anti-Sca-1-FITC, anti-B220-PE, and anti-CD19-PE monoclonal antibodies to confirm the generation of B220+ CD19+ pre-B cells and B220+ CD19−(Sca-1hi/lo) LAK cells as described before.17
Results
Spontaneous differentiation of embryonic stem cells to CD34−CD31− cells in the serum-free medium
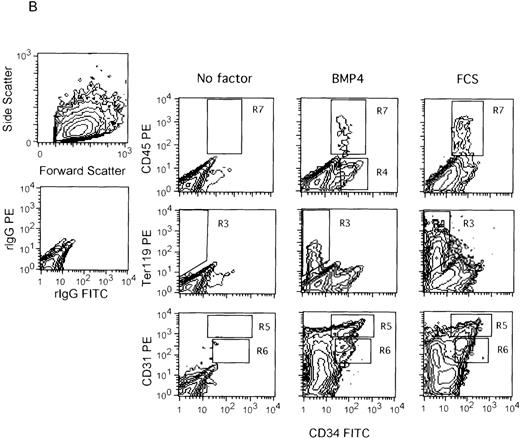
Because EB cells expressing the hematopoietic stem cell markers CD34 and ER-MP12 (CD31)37 were detected during the ES cell differentiation in the serum-containing medium,17 EBs developed in the serum-free medium were first analyzed with these markers. As shown in Figure 1A, the undifferentiated ES cells were CD34−CD31+. On induction of differentiation in the serum-free medium, virtually all became CD34− CD31−(approximately 97% and 97.6% of total A3-1 and E14 EB cells, respectively; Figure 1B). In contrast, in the presence of 15% FCS, CD34− CD31+ and CD34+CD31+ (R5 + R6 in Figure 1B) cells became readily detectable. Furthermore, 2 subpopulations within the CD34+CD31+ cell fraction, CD34+ CD31hiand CD34+ CD31lo (R5 and R6, respectively, in Figure 1B), became apparent. On the other hand, neither the erythroid-specific Ter119-expressing cells (R3 in Figure 1B) nor the leukocyte-specific CD45 expressing cells (R7 in Figure 1B) were detected in the serum-free medium, whereas both were consistently observed in the serum-containing medium. It was noted that the CD45+ cells were also CD34+.
Effect of BMP-4 on the differentiating ES cells. Undifferentiated E14 ES cells (day 0) were stained with anti-CD31-PE and anti-CD34-FITC monoclonal antibodies (A). The ES cells were also induced to differentiate for 7 days in the serum-free medium with or without 2 ng/mL BMP-4 or in the serum-containing medium, and they were analyzed with anti-CD45-PE, Ter119-PE, or CD31-PE, and anti-CD34-FITC monoclonal antibodies (B). The scatter patterns as well as the isotype control staining patterns (rIgG-FITC/rIgG-PE) for the undifferentiated ES cells and EB cells are shown in the top two panels of A, and in the two panels of the left most column of B, respectively. The region R7 represents the CD45+ cell population, and R3 represents the Ter119+ cell population. R5 corresponds to CD34+ CD31hi cells, and R6 corresponds to CD34+ CD31lo cells. (A) R5: 0.16%; R6: 0.03%. (B, left to right) R7: 0.0%, 1.2%, 3.1%; R3: 0.41%, 3.2%, 14.1%; R5: 0.30%, 3.4%, 2.0%; R6: 0.37%, 2.4%, 6.5%. R4 was used as a gate for sorting CD34+ CD45− cells in Table 2.
Effect of BMP-4 on the differentiating ES cells. Undifferentiated E14 ES cells (day 0) were stained with anti-CD31-PE and anti-CD34-FITC monoclonal antibodies (A). The ES cells were also induced to differentiate for 7 days in the serum-free medium with or without 2 ng/mL BMP-4 or in the serum-containing medium, and they were analyzed with anti-CD45-PE, Ter119-PE, or CD31-PE, and anti-CD34-FITC monoclonal antibodies (B). The scatter patterns as well as the isotype control staining patterns (rIgG-FITC/rIgG-PE) for the undifferentiated ES cells and EB cells are shown in the top two panels of A, and in the two panels of the left most column of B, respectively. The region R7 represents the CD45+ cell population, and R3 represents the Ter119+ cell population. R5 corresponds to CD34+ CD31hi cells, and R6 corresponds to CD34+ CD31lo cells. (A) R5: 0.16%; R6: 0.03%. (B, left to right) R7: 0.0%, 1.2%, 3.1%; R3: 0.41%, 3.2%, 14.1%; R5: 0.30%, 3.4%, 2.0%; R6: 0.37%, 2.4%, 6.5%. R4 was used as a gate for sorting CD34+ CD45− cells in Table 2.
Generation of CD34+, Ter119+, and CD45+ progeny is dependent on BMP-4 in the serum-free medium
Next we examined the effect of BMP-4 on the CD34+ EB cell generation in our serum-free culture. As also shown in Figure 1B, when 2 ng/mL BMP-4 was added to the culture, not only CD34−CD31+ cells and CD34+ CD31+cells but also Ter119+ cells and CD45+ cells became readily detectable. Furthermore, the dose-dependency analysis showed that both CD34− CD31+ (data not shown) and CD34+ CD31+ (CD34+CD31hi+CD34+ CD31lo in Figure2) cells appeared with 0.1 to 0.15 ng/mL BMP-4, and the levels were saturated at 1.5 to 2 ng/mL. The CD34+ CD31hi and the CD34+CD31lo subpopulations also became apparent with BMP-4 (Figure 1B). Thus the overall distribution of CD34 and CD31 expression among EB cells developed in the presence of BMP-4 was essentially the same as that generated with FCS. Furthermore, both Ter119+cells and CD45+ cells began to be detected with 0.5 ng/mL BMP-4, and the numbers were maximal with 2 ng/mL (Figure 2).
Effects of BMP-4 on Ter119+ and CD45+ EB cell generation are concentration dependent. Both A3-1 and E14 ES cells were differentiated in various concentrations of BMP-4, and analyzed as in Figure 1. Generation of Ter119+ (R3), CD45+ (R7), CD34+CD31hi (R5), and CD34+ CD31lo (R6) cells were quantified as % total EB cells. Numbers derived from 2 to 5 independent experiments were averaged and plotted according to the BMP-4 concentration with the corresponding SD (vertical line). Open symbols are results from A3-1 ES cells, and closed symbols are from E14 ES cells. Squares indicate results from serum-free medium, and circles indicate results from 15% FCS-containing medium.
Effects of BMP-4 on Ter119+ and CD45+ EB cell generation are concentration dependent. Both A3-1 and E14 ES cells were differentiated in various concentrations of BMP-4, and analyzed as in Figure 1. Generation of Ter119+ (R3), CD45+ (R7), CD34+CD31hi (R5), and CD34+ CD31lo (R6) cells were quantified as % total EB cells. Numbers derived from 2 to 5 independent experiments were averaged and plotted according to the BMP-4 concentration with the corresponding SD (vertical line). Open symbols are results from A3-1 ES cells, and closed symbols are from E14 ES cells. Squares indicate results from serum-free medium, and circles indicate results from 15% FCS-containing medium.
The absolute percentage of some of the cell populations analyzed (eg, CD34+ CD31hi) varied significantly among experiments, resulting in the large standard deviation (SD) values. However, the dose-dependent response to BMP-4 in each experimental set was essentially the same as shown, and it reproduced with both A3-1 and E14 ES cell lines. We therefore concluded that in serum-free ES cell differentiation, BMP-4 was a strong inducer of progeny expressing various hematopoietic markers, and all the BMP-4 effects tested were maximal at 1.5 to 2 ng/mL.
VEGF alone weakly up-regulates the generation of CD34+ CD31+ progeny but does not induce Ter119+ and CD45+ EB cells
We demonstrated previously that VEGF up-regulates the CD34+ cell population in EBs, where lymphohematopoietic progenitors were highly enriched, in the serum-containing medium.17 Therefore, we determined whether this would also be the case in the serum-free medium. Addition of 0.2 to 20 ng/mL VEGF alone weakly elevated the CD34+ CD31+ EB cell population (R5 and R6 in Figure 3; CD34+ CD31hi + CD34+CD31lo in Figure 4) in the serum-free medium. However, contrary to the BMP-4 effect, the VEGF effect was so weak that no clear CD34+ CD31hiand CD34+ CD31lo subpopulations were observed, and no concomitant increase in the CD34−CD31+ cell population was detected (Figure 3). Furthermore, neither the Ter119+ nor the CD45+cells were generated (Figures 3 and 4). Thus, although VEGF was an up-regulator for the CD34+ CD31+ cells, it seemed to achieve this through a pathway different from BMP-4.
Synergistic effect of VEGF on the BMP-dependent generation of CD34+ CD31+, Ter119+, and CD45+ EB cell population. E14 ES cells were induced to differentiate for 7 days in the serum-free medium without additional growth factor, with 20 ng/mL VEGF, with low concentration of BMP-4 (0.15 ng/mL), and with 0.15 ng/mL BMP-4 + 20 ng/mL VEGF. EB cells were harvested and stained with anti-CD45-PE, Ter119-PE or CD31-PE, and anti-CD34-FITC antibodies. Scatter patterns and isotype control staining patterns for EB cells are essentially the same as shown in Figure 1B. The designation of the regions is the same as in Figure 1. (left to right) R7: 0.0%, 0.05%, 0.22%, 3.5%; R3: 0.09%, 0.43%, 0.44%, 4.9%; R5: 0.25%, 0.71%, 1.0%, 3.5%; R6: 0.24%, 0.70%, 0.71%, 5.7%.
Synergistic effect of VEGF on the BMP-dependent generation of CD34+ CD31+, Ter119+, and CD45+ EB cell population. E14 ES cells were induced to differentiate for 7 days in the serum-free medium without additional growth factor, with 20 ng/mL VEGF, with low concentration of BMP-4 (0.15 ng/mL), and with 0.15 ng/mL BMP-4 + 20 ng/mL VEGF. EB cells were harvested and stained with anti-CD45-PE, Ter119-PE or CD31-PE, and anti-CD34-FITC antibodies. Scatter patterns and isotype control staining patterns for EB cells are essentially the same as shown in Figure 1B. The designation of the regions is the same as in Figure 1. (left to right) R7: 0.0%, 0.05%, 0.22%, 3.5%; R3: 0.09%, 0.43%, 0.44%, 4.9%; R5: 0.25%, 0.71%, 1.0%, 3.5%; R6: 0.24%, 0.70%, 0.71%, 5.7%.
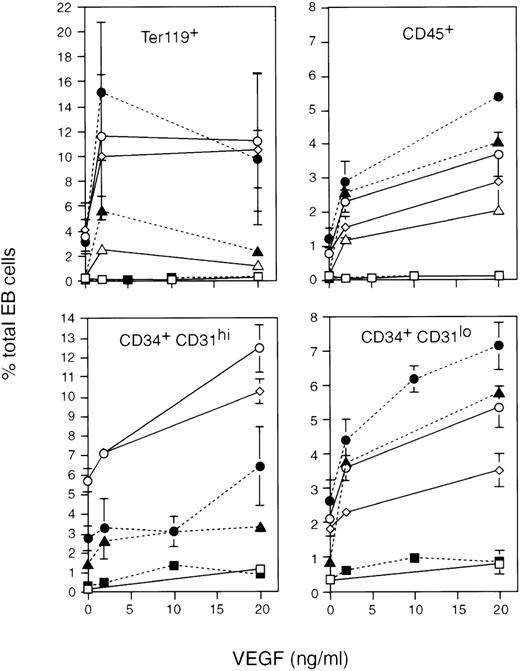
Effects of VEGF on Ter119+ and CD45+ EB cell generation are concentration dependent. Both A3-1 and E14 ES cells were differentiated in various concentrations of BMP-4 and VEGF analyzed as in Figures 1 and 3. Generation of Ter119+ (R3), CD45+ (R7), CD34+ CD31hi (R5), and CD34+CD31lo (R6) cells were quantified as % total EB cells. Except for the results with 0.15 ng/mL BMP4, which were obtained once with each ES cell line, numbers were derived from an average of 2 to 5 independent experiments and were plotted according to the VEGF concentration with the corresponding SD (vertical line). Open symbols are results from A3-1 ES cells, and closed symbols are from E14 ES cells. Squares indicate results from 0 ng/mL BMP-4, triangles indicate results of 0.15 ng/mL BMP-4, circles indicate results from 1.5 ng/mL BMP-4, and the diamond indicates results of 15 ng/mL BMP-4.
Effects of VEGF on Ter119+ and CD45+ EB cell generation are concentration dependent. Both A3-1 and E14 ES cells were differentiated in various concentrations of BMP-4 and VEGF analyzed as in Figures 1 and 3. Generation of Ter119+ (R3), CD45+ (R7), CD34+ CD31hi (R5), and CD34+CD31lo (R6) cells were quantified as % total EB cells. Except for the results with 0.15 ng/mL BMP4, which were obtained once with each ES cell line, numbers were derived from an average of 2 to 5 independent experiments and were plotted according to the VEGF concentration with the corresponding SD (vertical line). Open symbols are results from A3-1 ES cells, and closed symbols are from E14 ES cells. Squares indicate results from 0 ng/mL BMP-4, triangles indicate results of 0.15 ng/mL BMP-4, circles indicate results from 1.5 ng/mL BMP-4, and the diamond indicates results of 15 ng/mL BMP-4.
Synergistic enhancement of BMP-4-dependent generation of CD34+ CD31lo, Ter119+, and CD45+ cells by VEGF
However, when 10 ng/mL VEGF was added with BMP-4 at 0.15 ng/mL, the concentration insufficient for inducing Ter119+ or CD45+ cells by itself, both cell populations became readily detectable (induced by 10- to 19-fold and 11- to 24-fold, respectively; Figure 3). The CD34+ CD31+ cell population (R5 + R6, Figure 3) was also elevated 3- to 5-fold. Furthermore, dose-dependency analyses revealed that these VEGF-dependent enhancements were functions of both VEGF and BMP-4 concentrations (Figure 4). At a given BMP-4 concentration, CD34+CD31+ and CD45+ EB cell generation was dependent on the VEGF concentration from 2 to 20 ng/mL. The Ter119+ EB cell formation was also VEGF concentration dependent and was maximal at 2 ng/mL. However, these VEGF effects became less pronounced when the BMP-4 concentration was increased. In fact, compared with the results using 0.15 ng/mL BMP-4, the enhancement was reduced to 3- to 4-fold for Ter119+ cells and CD45+ cells and to 2- to 3-fold for CD34+CD31+ cells (CD34+ CD31hi + CD34+ CD31lo, Figure 4) when using 1.5 ng/mL BMP-4, even though the VEGF concentration was brought up to 20 ng/mL.
It was noted that the VEGF effects on the CD34+CD31hi and CD34+ CD31losubpopulations were not necessarily equal. Especially in the case of E14 ES cells, the CD34+ CD31lo EB cells were more sensitive to VEGF than the CD34+ CD31hi EB cells. The former were elevated 2- to 3-fold even at 2 ng/mL, whereas the latter were not significantly up-regulated until 10 ng/mL VEGF (Figure 4). However, when the VEGF concentration was brought to 20 ng/mL or higher, both subpopulations were significantly enhanced.
Although the absolute percentage of some of the cell populations analyzed (eg, Ter119+) varied significantly, the dose-dependent responses to VEGF shown in Figure 4 were representatives of the individual results obtained and essentially were reproduced with 2 ES cell lines. Therefore, in conclusion, VEGF served as a synergistic stimulator for BMP-4 to develop progeny expressing hematopoietic markers from ES cells, and it seemed to be especially effective when the BMP-4 concentration was low (0.1-0.15 ng/mL).
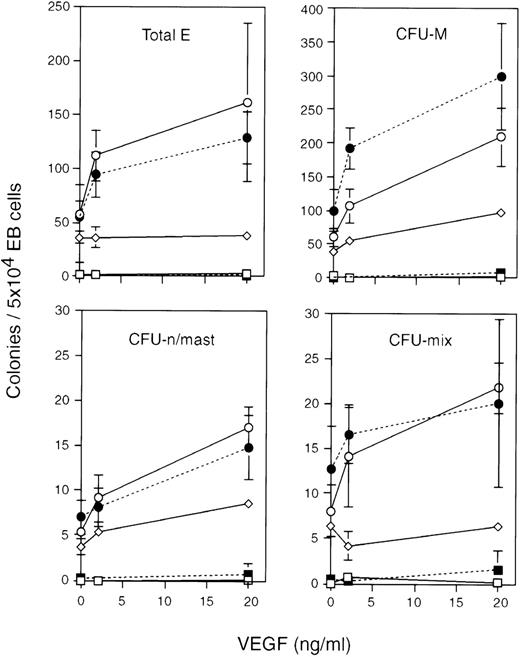
Generation of erythro-myeloid CFCs from embryonic stem cells in the serum-free medium requires BMP-4, and VEGF is a synergistic stimulator
Next we addressed whether the synergistic increase in the number of erythro-myeloid progenitor cells would be observed with BMP-4 and VEGF. Therefore, BMP-4 at 1.5 ng/mL or 15 ng/mL with or without 2 ng/mL or 20 ng/mL VEGF was added to the serum-free differentiation medium, and the occurrence of CFC produced was compared. As shown in Figure5, BMP-4 was absolutely necessary for any CFC types to be generated in EBs, and the addition of VEGF synergistically elevated the numbers of all type of CFCs in a dose-dependent manner (2- to 4-fold with 20 ng/mL). In the presence of 1.5 ng/mL BMP-4, VEGF induced a synergistic enhancement of the CFC numbers from 2 ng/mL. Increasing the VEGF concentration to 20 ng/mL preferentially elevated the numbers of myeloid CFCs (CFU-n/mast and CFU-M), whereas erythroid CFCs (total E: CFU-E + BFU-E) did not respond as clearly. These observations correlated well with the previous FACS phenotyping results for CD45+ and CD34+ CD31lo cell populations and for the Ter119+ cell population, respectively (Figure 4). The number of multipotential progenitor cells (CFU-mix) varied significantly among experiments. However, in every experiment, 2 to 20 ng/mL VEGF did show enhancement in the presence of 1.5 ng/mL BMP-4 (data not shown). In addition, consistent with the FACS phenotyping results, the response to VEGF was significantly weaker at a high concentration of BMP-4 (15 ng/mL) than at the lower concentration (1.5 ng/mL). Erythroid CFCs and CFU-mix in particular appeared to become insensitive to VEGF at 15 ng/mL BMP-4 (Figure 5).
Effects of BMP-4 and VEGF on the development of erythro-myeloid CFCs in EBs. A3-1 and E14 ES cell lines were differentiated for 7 days in the serum-free medium in the presence of 1.5 ng/mL BMP-4 or 15 ng/mL BMP-4 with or without 2 ng/mL VEGF or 20 ng/mL VEGF. EB cells were collected and subjected to erythro-myeloid CFC assays. Total-E (CFUE + BFU-E), CFU-M, CFU-n/mast, and CFU-mix were counted separately, and individual colony numbers were averaged over 3 to 4 independent experiments. The colony numbers are plotted/5 × 104 total EB cells according to the VEGF concentration with the corresponding SD (vertical line). Open symbols are results from A3-1 ES cells, and closed symbols are from E14 ES cells. Squares indicate results obtained with 0 ng/mL BMP-4, circles indicate results obtained with 1.5 ng/mL BMP-4, and the diamond indicates results obtained with 15 ng/mL BMP-4.
Effects of BMP-4 and VEGF on the development of erythro-myeloid CFCs in EBs. A3-1 and E14 ES cell lines were differentiated for 7 days in the serum-free medium in the presence of 1.5 ng/mL BMP-4 or 15 ng/mL BMP-4 with or without 2 ng/mL VEGF or 20 ng/mL VEGF. EB cells were collected and subjected to erythro-myeloid CFC assays. Total-E (CFUE + BFU-E), CFU-M, CFU-n/mast, and CFU-mix were counted separately, and individual colony numbers were averaged over 3 to 4 independent experiments. The colony numbers are plotted/5 × 104 total EB cells according to the VEGF concentration with the corresponding SD (vertical line). Open symbols are results from A3-1 ES cells, and closed symbols are from E14 ES cells. Squares indicate results obtained with 0 ng/mL BMP-4, circles indicate results obtained with 1.5 ng/mL BMP-4, and the diamond indicates results obtained with 15 ng/mL BMP-4.
These results indicated that BMP and VEGF synergistically induced the development of all types of erythro-myeloid CFCs during the differentiation of ES cells in the serum-free medium and that a high concentration of BMP-4 (15 ng/mL) may be detrimental for CFCs to respond to VEGF.
Generation of lymphoid progenitor cells from embryonic stem cells in the serum-free medium also requires BMP-4 and is enhanced by VEGF
Embryoid bodies were formed under the same conditions, and total EB cells were cocultured with OP9 stroma cells for 10 to 14 days in the presence of IL-7 and IL-2 as described.17 As summarized in Table 1, regardless of the presence of VEGF, cells derived from EBs formed in the absence of BMP-4 generated neither pre-B nor LAK cells. Conversely, the addition of 1.5 ng/mL BMP-4 during EB formation reproducibly induced 1 to 2 foci of pre-B cells, LAK cells, or both. The addition of VEGF at 2 or 20 ng/mL with 1.5 ng/mL BMP-4 resulted in a significant increase in the pre-B/LAK focus numbers (4 to 9 foci). Furthermore, at the end of the OP9 coculture, the yield of nonadherent cells and the fraction of cells expressing the lymphocyte markers, such as Sca-1, B220, and CD19, were found to be highest when EBs were formed with VEGF + 1.5 ng/mL BMP-4 (data not shown).
Consistent with results from the FACS phenotyping and CFC analyses, the lower concentration (1.5 ng/mL) of BMP-4 gave reproducibly higher numbers of lymphoid foci (4 to 9 foci) than the high concentration (1 to 2 foci at 15 ng/mL) in response to VEGF. This synergistic effect of VEGF was already evident at 2 ng/mL, and no additional enhancement was observed at 20 ng/mL. Thus the development of lymphoid progenitors from ES cells in vitro was also dependent on BMP-4 and enhanced by VEGF.
VEGF may also enhance the BMP-4-dependent generation of nonhematopoietic CD34+ cells in the serum-free medium
We also addressed whether the synergistic enhancement of BMP-4-dependent CD34+ EB cell generation by VEGF was achieved specifically through the increase in the CD34+lymphohematopoietic progenitor cell numbers. Therefore, CD45+ and CD34+ CD45− or CD34+ CD31lo and CD34+CD31hi fractions were isolated from EBs treated with BMP-4 with or without VEGF, and the frequencies of CFCs and B/NK progenitor numbers were compared.
No significant increases in the concentration of erythro-myeloid CFCs were observed in all the CD34+ EB cell subsets (1.2-fold on average; Table 2). However, the calculated frequency of the CD34+ CFCs per 106 total EB cells increased by 3.9-fold, consistent with the results using the whole EB cells (Figure 5). Similar results were obtained with the B/NK potentials: a 0.8-fold increase in the subfractions of CD34+ cells and a 3-fold increase in the total EB cell population (Table 2). Thus no indication of preferential increase of lymphohematopoietic progenitor cells by VEGF was detected within the CD34+ cell fraction. This supports the idea that VEGF may enhance the generation not only of the lymphohematopoietic CD34+ cells but also of the other types of CD34+ cells by BMP-4.
It is worth noting that marked differences in the distribution of the lymphohematopoietic cell potentials within the CD34+ cell fraction were observed (Table 2). The CD34+CD31lo fraction was enriched for BFU-E, CFU-M, CFU-n/mast, and CFU-mix, and it represented 70% to 94% of the total CD34+ CFCs, whereas the CD45+ fraction was enriched for CFU-M and represented only 37% to 40% of the total CD34+ CFCs. In fact, the CD45+ EB cells were CD34+ CD31lo, and CD34+CD45− cells were primarily CD34+CD31hi (data not shown). On the other hand, the B/NK progenitors were highly enriched in the CD34+CD45− fraction, which is consistent with the in vivo observation reported previously,22 and the CD34+ CD31hi fraction showed more B/NK potentials than the CD34+ CD31lo fraction. Therefore, CD34+ erythro-myeloid CFCs were primarily CD34+ CD31lo cells, and the CD34+lymphoid progenitors were likely to be in the CD34+CD31hi CD45− fraction.
Ordered function of BMP-4 and VEGF
It has been expected from genetic analyses in zebrafish and mice that the mesoderm-inducing function of BMP-4 should be followed by flk-1 for successful hematopoietic cell development.25,28,30 38 This ordered function of BMP-4 and the VEGF receptor can explain the synergy between BMP-4 and VEGF for the in vitro production of lymphohematopoietic progenitor cells. Therefore, we addressed this question by changing factors on day 4. Whether with VEGF (Figures 6e, 6g) or without VEGF (Figures 6c, 6d) for the last 3 days, continuous exposure to BMP-4 for longer than 4 days (Figures 6d, 6g) did not show any effects on the levels of Ter119+ and CD45+ cell types in the day 7 EBs compared with those treated only for the first 4 days (Figures 6c, 6e). On the contrary, 3-day treatment of BMP-4 after ES cells had been differentiated for 4 days in the absence of BMP-4 with VEGF (Figure 6f) or without VEGF (Figure 6b) induced neither Ter119+ nor CD45+ cell formation. Therefore, BMP-4 was necessary and sufficient to work during the initial 4 days of differentiation regardless of VEGF.
4-day treatment with BMP-4 followed by 3-day treatment with VEGF induced Ter119+ and CD45+ EB cells. E14 ES cells were induced to differentiate for 4 days with or without 1.5 ng/mL BMP-4, 10 ng/mL VEGF, or both in the serum-free medium followed by another 3 days in the presence or absence of these factors. Generations of Ter119+ erythroid cell and CD45+ macrophage progenitors were analyzed by FACScan on day 7. Scatter pattern, gate setting, and staining pattern of the isotype controls were as shown in Figure 1. Note that this series of experiments was performed without SCF. (a) Without factor for 7 days. (b) Without factor for 4 days followed by BMP-4 for 3 days. (c) With BMP-4 for 4 days, then without factor for 3 days. (d) With BMP-4 for 7 days. (e) With BMP-4 for 4 days followed by VEGF for 3 days. (f) With VEGF for 4 days followed by BMP-4 for 3 days. (g) With BMP-4 for 4 days followed by BMP-4 + VEGF for 3 days. (h) With BMP-4 + VEGF for 7 days. Data are displayed as averaged percentage total EB cell population obtained from 4 (for CD45) to 5 (for Ter119) independent experiments with the corresponding SD. Exception: (c) experiments were performed 3 times each.
4-day treatment with BMP-4 followed by 3-day treatment with VEGF induced Ter119+ and CD45+ EB cells. E14 ES cells were induced to differentiate for 4 days with or without 1.5 ng/mL BMP-4, 10 ng/mL VEGF, or both in the serum-free medium followed by another 3 days in the presence or absence of these factors. Generations of Ter119+ erythroid cell and CD45+ macrophage progenitors were analyzed by FACScan on day 7. Scatter pattern, gate setting, and staining pattern of the isotype controls were as shown in Figure 1. Note that this series of experiments was performed without SCF. (a) Without factor for 7 days. (b) Without factor for 4 days followed by BMP-4 for 3 days. (c) With BMP-4 for 4 days, then without factor for 3 days. (d) With BMP-4 for 7 days. (e) With BMP-4 for 4 days followed by VEGF for 3 days. (f) With VEGF for 4 days followed by BMP-4 for 3 days. (g) With BMP-4 for 4 days followed by BMP-4 + VEGF for 3 days. (h) With BMP-4 + VEGF for 7 days. Data are displayed as averaged percentage total EB cell population obtained from 4 (for CD45) to 5 (for Ter119) independent experiments with the corresponding SD. Exception: (c) experiments were performed 3 times each.
When VEGF was added to (Figure 6g) or in place of (Figure 6e) BMP-4 on day 4, significant enhancement of Ter119+ and CD45+ cell generation was observed on day 7 (2.9% to 3.3% for Ter119+; 1.1% to 1.2% for CD45+) compared with the levels achieved without VEGF (1.1% to 1.2% for Ter119+; 0.5% to 0.8% for CD45+) (Figures 6c,6d). This indicated that VEGF could still be effective after the BMP-4 treatment, supporting the idea of the ordered function of the 2 factors: BMP-4 followed by VEGF. However, when VEGF was added from the beginning with BMP-4 (Figure 6h), it gave higher levels of Ter119+ cells and CD45+ cells (5.0% and 1.3%, respectively). Therefore, it is still possible that VEGF functions at the same time with BMP-4 to produce the synergistic increase in progenitor cell number.
Discussion
We have demonstrated that VEGF synergistically enhanced the effect of BMP-4 on the in vitro development of lymphohematopoietic cells from ES cells and that the synergy was likely to be achieved by the ordered action of the 2 factors during the differentiation process. We have also provided evidence that BMP-4 was the essential factor not only for developing erythroid cells, as reported,35 36 but also for generating myeloid-CFCs and lymphoid cell potentials from ES cells.
Differences between the serum-containing culture and the serum-free culture in the ability to support the differentiation of ES cells into a variety of progeny-cell types were striking. Without FCS, ES cells were differentiated, but apparently only into CD34−CD31− cell types (Figure 1). No sign of lymphohematopoietic cell development was detected (Figure 5; Table 1). One interpretation for these observations is that ES cells may be differentiated through a default pathway without FCS, which does not lead to hematopoietic cell development. The fact that ES cells are spontaneously differentiated into cell populations expressing pax-6, a neuroectoderm marker, in a chemically defined medium suggests that the presumptive default pathway may lead to neuroectoderm cell formation.36 On the other hand, when BMP-4 was added, it appeared to convert the serum-free culture to a serum-containing-like culture; the distribution of CD34- and CD31-expressing cells became similar, Ter119+ cells and CD45+ cells were detected (Figures 1, 3), and all types of CFCs and B/NK lymphoid progenitors were generated (Figure 5; Table 1). Therefore, as demonstrated for the erythroid cell development from ES cells,35 36 BMP-4 seemed to induce all the necessary signals for ES cells to differentiate into lymphohematopoietic cell lineages. However, there were some differences between the effects of BMP-4 and FCS. The maximal levels of the erythro-myeloid CFC-containing cell fractions—such as Ter119+ cells, CD45+cells, and CD34+ CD31lo cells—were lower with BMP-4 than with 15% FCS, whereas those of CD34+CD31hi cells were higher with BMP-4 than with 15% FCS (Figure 2). Thus FCS contained activity that seemed to preferentially support the generation of erythro-myeloid progenitor cells from ES cells.
VEGF clearly induced the number of Ter119+ erythroid cells and CD45+ and CD34+ CD31loerythro-myeloid progenitors when added with BMP-4 (Figures 3, 4). In fact, EBs produced by BMP-4 and VEGF were red, whereas those developed only with BMP-4 were white (data not shown). Especially when the concentration of BMP-4 was insufficient for inducing these cells by itself (0.1-0.15 ng/mL), the culture seemed to become totally dependent on BMP-4 and VEGF (Figures 3 and 4; the results shown in Figure 6provide more definitive evidence because SCF was omitted). However, even at the optimal concentration of BMP-4 (1.5-2 ng/mL), VEGF still increased the frequency of erythro-myeloid CFCs and lymphoid potentials (Figure 5; Table 1). As far as we know, this is the first demonstration that the in vitro differentiation of ES cells toward lymphohematopoietic cell lineages is dependent on a flk-1 ligand. Given that the flk-1 signaling is essential for the hematopoietic cell development in vivo,30 the in vivo concentration of BMP-4 might be in the range of 0.1 to 0.15 ng/mL. Interestingly, at a higher concentration of BMP-4 (15 ng/mL), the VEGF effect was less pronounced (Figures 4, 5), and many cells (mainly macrophage-like cells) formed either no colonies or microcolonies during the CFC analysis (data not shown). Therefore, a high concentration of BMP-4 might also stimulate differentiation of hematopoietic progenitor cells or, alternatively, desensitize their ability to respond to various growth factor/cytokine signals.
VEGF as a synergistic enhancer of BMP-4-dependent lymphohematopoietic cell generation from ES cells appears to contradict the finding by Hidaka et al33 in that VEGF is inhibitory for generating CFCs in 6- to 12-day-old EBs. However, because their EB culture method includes hematopoietic cytokines and FCS and because the VEGF effect on the CFC generation is stimulating (ie, positive) in day 4 EBs, it is likely that the inhibitory effect of VEGF is on the long-term growth/maturation of CFCs during EB culture. All our results were derived from day 7 EBs. Therefore, day 7 EB in the serum-free culture might correspond to day 4 EB in the serum-containing culture. In this regard, it is worth mentioning that during the 14-day culture of various subsets of CD34+ cells on OP9 cells, VEGF was inhibitory for pre-B/LAK cell formation (data not shown).
The synergistic effect of VEGF on the BMP-4-dependent differentiation processes does not seem to be restricted to the hematopoietic cell lineages because the CD34+ cell subpopulations, all of which were elevated with VEGF, contained concentrations of CFCs and lymphoid progenitors virtually identical to those obtained without VEGF (Table 2). However, this result also implies that there may be no preferential enhancement of nonhematopoietic CD34+ cell types (presumably including endothelial cells). This observation seems to contradict the finding with chicken embryonic flk-1+cells in that VEGF preferentially shifts their differentiation toward the endothelial cell lineage, thereby inhibiting their differentiation into hematopoietic progenitor cells.39 However, the difference may account for the intrinsic differences in the characteristics of chicken cells and mouse cells.
Although the ES cell differentiation into lymphohematopoietic progenitor cells was dependent on VEGF in the serum-free medium, VEGF was dispensable when BMP-4 was supplied at the optimal concentration (Figures 1, 2, 5; Table 1). However, with flk-1−/−mutant ES cells, it has been shown that an active role of the VEGF receptor, flk-1, is necessary for the in vitro generation of β-globin-expressing erythroid cells in the presence of BMP-4 alone.32 The former suggests that the VEGF receptor signaling is not required, and the latter indicates that it is required. One possible explanation for the apparent differences is that, at the optimal concentration, BMP-4 may induce the expression of VEGF or other VEGF family members, which helps the in vitro lymphohematopoietic cell generation through flk-1, presumably at low levels, so that further activation of flk-1 by exogenous VEGF is still able to show the synergistic effect. Nevertheless, this notion is an interesting parallel with the in vivo observations that VEGF is not so strictly required as flk-1 for the primitive erythroid cell development.29-31 40
How, then, is the synergistic effect achieved? Genetic analyses in zebrafish and mice suggest a model that implicates BMP-4 as an earlier-acting factor that is followed by the stimulation of flk-1 action for successful hematopoietic cell development.25,28,30 38 Based on this model, BMP-4 may effectively induce the differentiation of ES cells into uncommitted mesodermal precursors but only poorly support the further differentiation of such cells into lymphohematopoietic progenitor cells. In contrast, VEGF may be a later-acting factor that facilitates the latter stage of development. Alternatively, the synergy may result from the presence of a critical mesoderm intermediate whose proliferation/differentiation is dependent on both factors. In search of the critical timing required for each factor to work during the 7 days of in vitro differentiation, the BMP action was found to be required within the first 4 days, whereas VEGF was able to exert the synergistic effect after the BMP-4 treatment (Figure 6). Thus although the latter possibility has not been entirely ruled out, this result would support the former model that fits with the in vivo observations.
The idea of VEGF as the “second-stage factor” is supported by the recent report that flk-1−/− ES cells are able to generate levels of blast-CFCs in vitro similar to those for wild-type ES cells.32 The blast-CFC represents a VEGF-dependent common progenitor cell for primitive and definitive erythropoiesis34 and has endothelial potential21 that leads to the hypothesis that VEGF may be a growth/differentiation factor for the hypothetical hemangioblast.41 Therefore, although the experiments were performed in serum-containing media, the results suggest that the flk-1-dependent signal may not be required for the generation of the “hemangioblast.” Furthermore, flk-1 does not seem to be necessary for generating the erythro-myeloid CFC activity in early mouse embryos (E7.5), whereas it is required for maintaining the activity through the later stages of embryogenesis (E8.5).30 32 Thus it is tempting to speculate that VEGF-sensitive cells, which are induced by BMP-4 from ES cells during the first 4 days of in vitro differentiation, might be the hemangioblast. This is a question currently being addressed.
Acknowledgments
We thank L. Souza for G-CSF, T. Boone for IL-3 and IL-6, K. Langley for SCF, W. Kenney for IL-2, and B. Samal for LIF. We also thank C. Saris for providing E14 cells and E. Medlock, C. Saris, and I. Ponting for sharing information and interesting discussions and particularly for critically reading this manuscript. We give warm thanks to W. Boyle for support and encouragement.
Reprints:Naoki Nakayama, Department of Cell Biology, Amgen Inc, MS14-1-D, One Amgen Center Drive, Thousand Oaks, CA 91320; e-mail: naoki.nakayama@amgen.com.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.