Immune-mediated, acquired pure red cell aplasia (PRCA) is a rare disorder frequently associated with other autoimmune phenomena. Conventional immunosuppressive treatment is often unsatisfactory. Rituximab is a monoclonal antibody against the CD20 antigen, highly effective for in vivo B-cell depletion. An 18-month-old girl with both severe PRCA and autoimmune hemolytic anemia, refractory to immunosuppressive treatment, received 2 doses of rituximab, 375 mg/m2 per week. The drug was well tolerated. After anti-CD20 therapy, substitutive treatment with intravenous immunoglobulin was started. The treatment resulted in marked depletion of B cells; a striking rise in reticulocyte count ensued, with increasing hemoglobin levels, finally leading to transfusion independence. The child is now 5 months off-therapy, with normal hemoglobin and reticulocyte levels. This case suggests a role of anti-CD20 monoclonal antibody for treatment of patients with antibody-mediated hematologic disorders.
Introduction
Acquired pure red cell aplasia (PRCA) is rare in infancy, median age of onset being usually between 50 and 60 years.1-3 The pathogenesis of the disease is immune-mediated in most cases, soluble serum inhibitors or inhibitory T cells, able to impair in vitro growth of erythroid progenitors (burst-forming unit [BFU-E], and colony-forming unit [CFU-E]), having been demonstrated in several series of patients.1-3PRCA is frequently associated with other autoimmune phenomena, that is, production of autoantibodies directed against erythrocytes, acetylcholinesterase, smooth muscle, and so on.2 PRCA associated with autoimmune hemolytic anemia (AIHA) has been previously reported.4
Treatment of PRCA usually employs steroids and/or other immunosuppressive drugs (ie, cyclosporine-A and cyclophosphamide), or immunomodulating agents such as immunoglobulin, with response rates to these therapies ranging from 30% to 55%.2 3
Rituximab is a humanized, murine, monoclonal antibody (MoAb) directed against the CD20 antigen, expressed on pre-B lymphocytes and on mature B lymphocytes.5,6 Rituximab has been demonstrated to be highly effective for in vivo B-cell depletion, B lymphocytes becoming undetectable in peripheral blood after a single infusion, and recovering only 6-9 months after discontinuation of treatment.5,6 The antibody has been recently introduced for treatment of B-cell lymphomas.7-10
We describe the case of an 18-month-old child with immune-mediated PRCA and AIHA, refractory to first- and second-line immunosuppressive therapy, who was successfully treated with anti-CD20 MoAb.
Study design
An 18-month-old Caucasian girl was hospitalized due to recent onset of pallor and listlessness. Physical examination at admission was unremarkable, with the exception of pallor and mild jaundice; the patient did not present either spleen or liver enlargement. Full blood count at admission showed normochromic-normocytic anemia (hemoglobin = 5.6 g/dL) with reticulocytopenia (absolute reticulocyte count = 7 × 109/L) and normal white blood cell and platelet counts. Total and unconjugated bilirubin levels were increased (2.31 mg/dL and 1.77 mg/dL, respectively), and serum haptoglobin was undetectable. Tests for hereditary hemolytic anemias, as well as direct and indirect Coombs tests, were negative. Evaluation of the blood film revealed the presence of spherocytes, whereas erythrocyte fragments were not detectable. Serologic tests for parvovirus B19, human cytomegalovirus, and Epstein-Barr virus were negative. Chest x-ray was normal. A blood count performed 6 months earlier had shown normal hemoglobin (12 g/dL).
A bone marrow aspirate performed at admission demonstrated normal representation of myeloid and megakaryocyte precursors, but nearly absent erythroid precursors. In vitro cultures of patient light-density bone marrow cells, performed in triplicate as described previously,11 demonstrated that, compared with 3 healthy bone marrow donors, a significant reduction of colonies from erythroid progenitors was present, with patient and controls BFU-E and CFU-E being 20 ± 4 versus 88 ± 11 and 32 ± 3 versus 67 ± 5, respectively. By contrast, growth of the patient's granulocyte-macrophage progenitors (CFU-GM) was normal. The patient's plasma profoundly inhibited growth of BFU-E from healthy controls (93 ± 16 and 24 ± 6 without and with patient's plasma), suggesting the existence of soluble serum factors responsible for both PRCA and hemolysis.
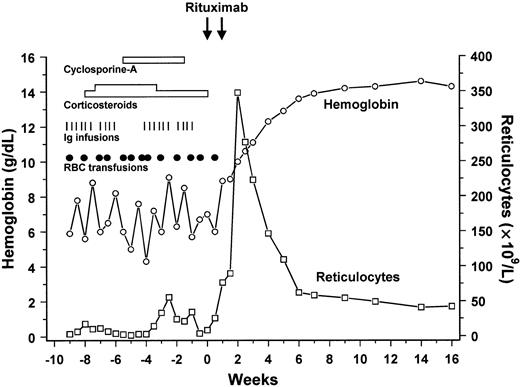
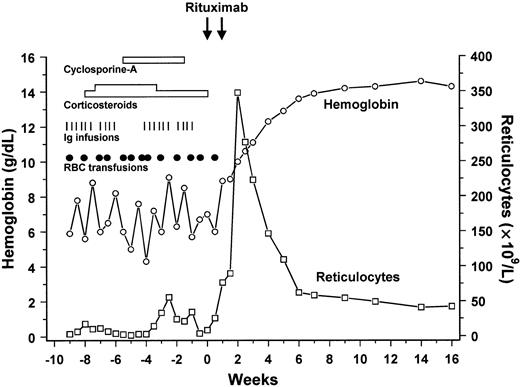
Due to a steadily decreasing hemoglobin level, the child was transfused. Repeated administration of red blood cell concentrates was required in order to maintain hemoglobin above 6 g/dL (Figure1). In the following weeks, she remained transfusion-dependent, with erythrocyte consumption much higher than that compatible with hyporegenerative anemia (transfusion of 15-20 mL/kg of packed red blood cells every 5-7 days was necessary). In detail, during a period of 10 weeks, 13 erythrocyte transfusions were administered. Serum bilirubin levels remained above normal levels, whereas serum haptoglobin was constantly undetectable. Despite clinical and biochemical signs of continuing hemolysis, the direct antiglobulin test (DAGT), repeatedly performed during this time, remained negative. In AIHA the DAGT is positive, but patients with AIHA and PRCA in whom the DAGT has been persistently negative have been occasionally reported.4 Because other causes of persistent hemolysis could reasonably be excluded, a diagnosis of AIHA with PRCA was made in our patient and immunosuppressive treatment was started.
Clinical course of the patient and response to treatment.
Reticulocyte count and hemoglobin levels are reported in the graph. Black circles represent red blood cell transfusion, tick marks represent immunoglobulin infusions, and rectangles treatment with corticosteroids and cyclosporine-A. Arrows show the 2 infusions of anti-CD20 monoclonal antibody.
Clinical course of the patient and response to treatment.
Reticulocyte count and hemoglobin levels are reported in the graph. Black circles represent red blood cell transfusion, tick marks represent immunoglobulin infusions, and rectangles treatment with corticosteroids and cyclosporine-A. Arrows show the 2 infusions of anti-CD20 monoclonal antibody.
Methylprednisolone, first at conventional doses (2 mg/kg per day), then at high doses (5 mg/kg per day), together with intravenous immunoglobulin infusions, were administered, both proving ineffective in increasing reticulocyte count and in reducing erythrocyte consumption. Concomitant treatment with cyclosporine-A during 6 weeks was equally ineffective (Figure 1). Because a case of immune-mediated thrombocytopenia successfully treated with anti-CD20 monoclonal antibody (rituximab) had been published,12 we reasoned that selective destruction of B cells producing antibodies responsible for both PRCA and hemolysis might be effective. Rituximab was administered intravenously at the dose of 375 mg/m2 as a 4-hour infusion, once weekly for a total of 2 doses. Before each infusion, the child received pre-medication with methylprednisolone and diphenhydramine. The drug was well tolerated and the child did not present any adverse reaction or side effects. Substitutive treatment with intravenous immunoglobulin (400 mg/kg every 3 weeks) was given, in order to prevent treatment-induced hypogammaglobulinemia.
Results and discussion
Treatment with rituximab resulted in marked depletion of B cells in peripheral blood, as demonstrated by the percentage of CD19+ and CD20+ cells dropping from the pretreatment values of 12% and 11%, respectively, to values less than 0.5% for both antigens 2 days after the first infusion.
Shortly after the first anti-CD20 MoAb infusion, the patient showed a striking rise in reticulocyte count, with a maximum value of 347 × 109/L achieved 2 weeks after starting the treatment. Progressive increase of hemoglobin level and achievement of transfusion independence (Figure 1) followed the rise in reticulocytes. Bilirubin and haptoglobin levels normalized, as well. The course of the response was as expected and gave further support to a diagnosis of AIHA with concomitant antibody-mediated PRCA.
The child, 5 months after MoAb therapy, is transfusion-independent, with normal hemoglobin and reticulocyte levels. She is no longer receiving immunosuppressive treatment. The percentage of the patient's B lymphocytes is still below 1%. During the observation period, the child did not develop any significant infectious complication.
As mentioned, so far only one case of immune-mediated thrombocytopenia, successfully treated with anti-CD20 MoAb, has been extensively reported in the literature.12 In that patient, the administration of 4 doses of rituximab induced complete and long-lasting normalization of platelet count. Treatment of patients with AIHA using rituximab has been preliminarily reported with variable response.13-15
In our experience, response to anti-CD20 infusion occurred 4 days after the first administration, and it was sustained, allowing discontinuation of all other immunosuppressive therapies. The rapid response and disappearance of B cells from peripheral blood suggested that 2 doses of monoclonal antibody might be sufficient, thus saving costs.
Recovery of B lymphocytes after treatment with rituximab has been described to start from 6 to 9 months after the last administration; a normal B-lymphocyte number is usually achieved only 12 months after treatment discontinuation.5 As a consequence, a significant reduction in immunoglobulin M (IgM) and IgG serum levels is to be expected,16 with a possible risk of infectious complications, as recently reported.17 18 For this reason, we gave replacement therapy with intravenous immunoglobulins.
The outcome of childhood severe, immune-mediated, hematologic cytopenia with conventional immunosuppressive approaches is sometimes unsatisfactory.1-3 For this reason, the recent introduction of new immunomodulating agents, such as MoAbs approved for in vivo use, represents an appealing and promising treatment modality for patients with the most severe and/or refractory forms of disease. In refractory or chronic disease, use of rituximab is attractive also because it could reduce or avoid some side effects of prolonged therapy with steroids (eg, fluid retention, severe catabolic damage, hyperglicemia, avascular necrosis of bone, growth impairment) and/or other aspecific immunosuppressive drugs.
In conclusion, even though a longer follow-up is required to assess the long-term efficacy of this treatment, this case provides a basis for future prospective trials aimed at defining the role of anti-CD20 MoAb for antibody-mediated hematologic disorders.
We would like to thank Rita Maccario for the immune-phenotype study of peripheral blood lymphocytes and Patrizia Comoli for help in revising the manuscript.
Supported in part by grants to F.L. from AIRC (Associazione Italiana per la Ricerca sul Cancro), CNR (Consiglio Nazionale delle Ricerche), and IRCCS (Istituto di Ricovero e Cura a carattere Scientifico) Policlinico San Matteo, Pavia.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Franco Locatelli, Oncoematologia Pediatrica, IRCCS Policlinico San Matteo, P.le Golgi 2, I-27100 Pavia, Italy; e-mail:f.locatelli@smatteo.pv.it.