Abstract
The adhesive protein thrombospondin (TSP) potentially mediates sickle (SS) red blood cell (RBC) adhesion to the blood vessel wall, thereby contributing to vaso-occlusive crises in sickle cell disease. We previously reported that SS RBCs bind to immobilized TSP under flow conditions, whereas normal (AA) red cells do not. However, the SS RBC receptors that mediate this interaction are largely unknown. Here it is reported that integrin-associated protein (IAP), or CD47, mediates the adhesion of these cells to immobilized TSP under both flow and static conditions. A peptide derived from the C-terminal IAP binding site of TSP also supports sickle cell adhesion; adhesion to this peptide or to TSP is inhibited specifically by the anti-IAP monoclonal antibody, 1F7. Furthermore, these data suggest that IAP on SS RBCs is structurally different from that expressed on AA RBCs but that IAP expression levels do not vary between AA and SS RBCs. This structural difference may contribute to the enhanced adhesion of SS RBCs to immobilized TSP. These results identify IAP as a TSP receptor on SS RBCs and suggest that this receptor and its binding site within TSP represent potential therapeutic targets to decrease vaso-occlusion.
Introduction
Sickle cell disease (SCD) epitomizes a genetic disorder. A single DNA base mutation in the hemoglobin β chain results in a single amino acid change (glu6 → val). This mutated hemoglobin, termed hemoglobin S, or HbS, forms rigid, intracellular, insoluble polymers, causing the affected red blood cell (RBC) to assume the characteristic sickle shape presented in SCD. Patients homozygous for hemoglobin S (SS) exhibit a complex host of clinical symptoms. Manifestations of SCD include marked, chronic hemolysis and anemia, acute chest syndrome, susceptibility to infection, stroke, retinopathy, and splenic sequestration crisis.1
The characteristic manifestation of SCD, however, is the vaso-occlusive crisis. This event accounts for most of the morbidity and mortality associated with this condition and appears to result from blockage of blood flow by SS RBCs.2 Patients in vaso-occlusive crisis experience marked, localized pain arising from tissue hypoxia due to inadequate perfusion from blocked vascular beds.3 The mechanisms by which vaso-occlusive crises are initiated are largely unknown. However, data suggest that adhesion of SS RBCs plays an important role in the overall vaso-occlusive process.4
In vitro studies indicate that SS RBCs adhere to both activated endothelial cells and exposed subendothelial matrix proteins that line the blood vessel wall (reviewed in 5,6). Elevated plasma factors, such as tumor necrosis factor-α, platelet-activating factor (PAF), histamine, and IL-8, are thought to up-regulate the adhesive state of endothelial cells for SS RBCs.7 Previous work from this laboratory demonstrated that SS RBCs, but not cells from AA individuals, adhere to the plasma and matrix molecule, thrombospondin (TSP).8 Plasma TSP released from activated platelets binds to quiescent and activated endothelial cells9 and is thus thought to promote SS RBC adhesion to the endothelium in vivo.10 Levels of plasma TSP in patients with SCD are significantly elevated and can reach concentrations required to bind the SS RBCs to endothelial cells.11
Chronic endothelial cell retraction and chronic vascular injury12 in SCD potentially promote TSP expression in the subendothelial matrix and subsequent exposure to the flowing SS RBCs. In vitro evidence suggests that SS RBCs can adhere to TSP exposed in endothelial cell gaps, thus supporting a role for matrix TSP as a vascular adhesogen, potentially compounding vaso-occlusion.13 Despite the relevance of TSP as an adhesive molecule in SCD, the receptors that mediate SS RBC adhesion to this vascular protein remain unknown.
TSP is a 450-kd glycoprotein homo-trimer with several adhesive domains. Each chain contains an N-terminal domain that binds heparin sulfate proteoglycans, a type 1 repeat that binds CD36 or glycoprotein IV (GPIV), an RGD sequence that binds integrins, and a C-terminal cell-binding domain that recognizes integrin-associated protein (IAP).14-16 The cell-binding domain of TSP shares the highest degree of homology among the thrombospondins—more than any other adhesive site in the molecule17—suggesting a vital role for this region. Indeed, antibodies against the cell-binding domain of TSP block platelet aggregation,18 neutrophil oxidative burst, and the attachment of numerous cells to this adhesive substrate 18-20 through IAP.
Classically, IAP, or CD47, associates with and modulates integrin function. However, IAP shows ubiquitous tissue and hematopoietic cell distribution,21 including expression on mature erythrocytes, cells that do not express integrins.22Neither IAP expression nor a role for IAP on the SS RBC has ever been demonstrated. Based on the role of IAP as an adhesion receptor for TSP on other cells, we wanted to evaluate the adhesive potential of IAP on SS RBCs for TSP.
We report here that IAP is expressed on SS RBCs and mediates a significant proportion of SS RBC adhesion to TSP under flow and static conditions. Additionally, we provide evidence that SS RBCs adhere to the IAP binding site within the C-terminal cell-binding domain of TSP. Furthermore, we provide evidence that the structure of IAP on SS RBCs is different from the structure of IAP expressed on normal AA RBCs. This structural change results in the decreased availability of one monoclonal antibody (mAb) epitope on IAP and the potentiation of another epitope. Despite this structural change, it appears that IAP expression levels are similar or identical on SS and AA RBCs because no difference in IAP expression levels could be detected with a polyclonal antibody (pAb) or a separate mAb against this receptor. These data therefore implicate IAP on sickle cells and the cell-binding domain of TSP as mediators of SS RBC adhesion to subendothelial- and endothelial-associated TSP in vivo.
Materials and methods
Reagents
Human TSP-1 purified from platelets was obtained from Gibco BRL (Grand Island, NY), Calbiochem (La Jolla, CA), or Sigma (St Louis, MO). Platelet-purified human TSP was also kindly provided by Dean Mosher (University of Wisconsin, Madison, WI) and Jack Lawler (Brigham and Women's Hospital, Boston, MA). Antibodies against IAP, B6H12, 1F7, and 2D3 were generous gifts from Eric Brown (University of California at San Francisco). Initially, TSP peptides 4N1K (kRFYVVMWKk) and control 4NGG (kRFYGGMWKk)23 were provided by William Frazier (Washington University), as was the pAb against IAP. These peptides, as well as a scrambled 4N1K peptide termed 4N1KS (kMRVYFVWKk), were also synthesized and high-performance liquid chromatography-purified by the University of North Carolina, Chapel Hill/NIEHS Protein Chemistry Laboratory.
RBC preparation
Sickle RBCs were obtained from patients with homozygous SCD during clinic visits to the University of North Carolina Comprehensive Sickle Cell Center. All blood samples were drawn by venipuncture into 0.13 M sodium citrate and processed immediately by centrifugation at 150g for 15 minutes at ambient temperature to isolate blood cells from plasma and platelets. RBCs were then washed 3 times in CGS (1.29 mM sodium citrate, 3.33 mM glucose, 124 mM NaCl; pH, 7.2). The cells were resuspended in phosphate buffered saline and packed at 400g for 10 minutes. A 1% hematocrit was then prepared by diluting 30 μL packed RBCs per 1.5 mL perfusion media (Hanks balanced salt solution [H6136; Sigma] composed of CaCl2 · 2 H2O [0.185 g/L], MgSO4 [0.098 g/L], KCl [4 g/L], KH2PO4 [0.06 g/L], NaCl [8 g/L], Na2HPO4 [0.048 g/L], D-glucose [1.0 g/L], and phenol red · Na [0.011 g/L]) supplemented with 0.3% bovine serum albumin and 20 mM HEPES, pH, 7.4).
Flow adhesion assay and protein–peptide immobilization
The flow adhesion system used for this study was designed to mimic blood flow through postcapillary venules, as described.8 24 Purified TSP (80 μL of 18.75 μg/mL or 1.5 μg) or 4N1K, 4NGG, or 4N1KS peptide (198 nmol/well) in perfusion media was immobilized onto identical wells formed by the silicon gasket in a 35-mm polystyrene culture dish by incubating for 2 hours at 37°C. A 1% hematocrit solution (1.5 mL) was flowed over the wells at a rate of 1.0 mL/min and a constant shear stress of 1 dyne/cm2. After a wash period of approximately 4 minutes, the number of adherent cells from 4 representative areas of the well was counted from 0.25 cm2 fields and averaged. Any occasional adherent white blood cells were not included in the analysis.
SS RBC static adhesion assay
The static adhesion assay used for this study was based on an adenosine triphosphate (ATP) monitoring system, ATP-Lite (Packard Groningen, Netherlands). Microtiter plates (96-well) were coated with 1.5 μg TSP for 2 hours at 37°C and blocked for 30 minutes at 37°C with 0.3% BSA in Hanks balanced salt solution. SS RBCs (3 × 106) were added to each well and incubated for 2 hours at 37°C. Adherent cells were washed 4 times, and the remaining SS RBCs were lysed according to manufacturer's directions, transferred to Optiplate (Packard), and treated with ATP-Lite for luminescence measurement in a microtiter plate reader (TopCount; Packard).
SS RBC Western blot analysis and indirect immunofluorescence
SS and AA RBC membrane ghosts from 3 × 1010 cells were prepared by hypotonic lysis in 5 mM Na2HPO4 (pH, 8.0), 0.5 mM EGTA, and 2.0 mM phenylmethylsulfonyl fluoride. Washed intact membranes were then solubilized by a 20-minute incubation in 1% SDS, 1 mM EGTA, and 50 mM HEPES (pH, 7.4) at 95°C. The SDS soluble fraction essentially represented the entire membrane fraction and was loaded nonreduced onto SDS-PAGE, transferred to Immobilon-P (Millipore, Bedford, MD), and analyzed by Western blot with B6H12 mAb at 1 μg/mL, pAb against IAP, or anti-glycophorin A mAb (DAKO, Carpinteria, CA) at 1 μg/mL in Tris-buffered saline plus 0.1% Tween-20 (Sigma). Cell surface expression of IAP and saturating mAb concentrations were determined by immunostaining of washed SS RBCs with either the mAb 2D3 or the mAb 1F7 at various concentrations in perfusion media, followed by incubation with goat anti-mouse antibody conjugated to Cy3 (Jackson Immunoresearch, West Grove, PA). Stained samples were then analyzed by FACS-scan flow cytometry (Becton Dickinson, Franklin Lakes, NJ) gated to exclude any occasional white blood cells. Only RBCs of equivalent size, shape, and granularity were used in cell surface analysis of IAP expression.
Density fractionation of RBCs
For Western blotting and immunofluorescence of reticulocyte-enriched fractions of RBCs, unpacked, washed RBCs were layered over a modified arabino-galactan gradient (Larex, White Bear Lake, MN) and spun at 74 000g at 20°C for 45 minutes according to manufacturer's directions. RBCs collected from the low-density fraction of the gradient were subsequently analyzed for nuclear material content by methylene blue staining. Approximately 50% to 80% of the low-density fraction cells were identified as reticulocytes, representing an approximately 10-fold enrichment of reticulocytes in SS patients and an approximately 50-fold enrichment in AA donors.
Analysis of immobilized peptides
To determine the equivalent surface densities of the 4N1K, 4NGG, and 4N1KS peptides, varying concentrations of each peptide were adsorbed onto 96-well polystyrene culture plates for 2 hours at 37°C. Immobilized peptides were then washed in perfusion media and biotinylated at ambient temperature overnight in 10 mM EZ-Link PEO Maleimide Activated Biotin (Pierce, Rockford, IL), washed extensively in phosphate-buffered saline, and incubated for 1 hour with streptavidin–horse radish peroxidase conjugate. Peptide-bound biotin was then detected using the 3,3′, 5′5-tetramethylbenzidine liquid substrate system (Sigma) and read at 450 nm in a microplate reader (Spectra Max Plus, Molecular Devices, Sunnyvale, CA).
Results
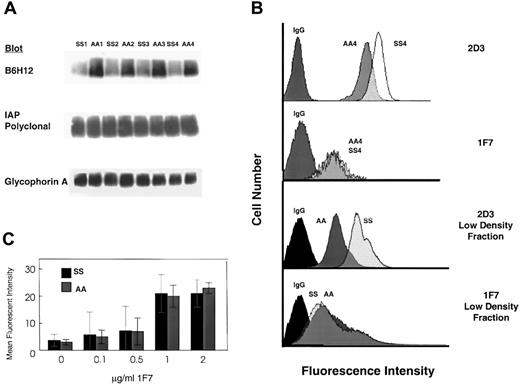
To examine IAP expression on sickle RBCs, intact RBC membranes from either SS or AA RBCs were solubilized in 1% SDS and analyzed by Western blot with B6H12, an mAb against human IAP. B6H12 readily detected a band of approximately 52 kd, consistent with the established molecular weight of IAP21 in AA RBC membranes, but reacted weakly with the same band from SS RBC membranes (Figure1A, top). The results shown are representative of 14 separate SS and AA samples each. However, a polyclonal Ab against IAP detected equivalent amounts of IAP solubilized from the same AA and SS RBC membranes (Figure 1A, middle) under identical conditions, suggesting equivalent amounts of IAP in AA and SS membrane samples. Additionally, Western blots of the same samples with an anti-glycophorin A mAb showed no significant variation in protein loading (Figure 1A, bottom). These results imply that the SDS-denatured epitope for B6H12 is compromised in SS RBCs. This epitope loss was present in every SS patient sample analyzed and strongly suggested a unique structure or conformation of IAP on SS RBCs.
SS RBCs and AA RBCs express equivalent amounts of IAP, but SS RBC IAP is structurally different from that on AA RBCs.
(A) (top) Representative Western blots of RBC membranes (25 μg) from 4 separate SS (SS1-SS4) or AA (AA1-AA4) donors probed with B6H12 indicate that SS RBC membranes react poorly with this mAb against IAP (n = 14; 4 representative samples shown). B6H12 reacted relatively robustly with an approximately 52-kd band on prepared AA RBC membranes (n = 14; 4 representative samples shown). These results suggest that the SDS-denatured epitope for B6H12 is compromised on SS RBC IAP. Reprobing the previous blot with a pAb against IAP and quantification by densitometry detected equivalent amounts of IAP extracted from SS and AA RBC membranes (middle). This result suggests equivalent amounts of IAP in intact membranes prepared from each of the AA and SS samples. An mAb against glycophorin A also detected equivalent amounts of this cell surface receptor extracted from AA and SS RBC membranes (bottom), further reinforcing equivalent protein extraction from both sets of prepared membranes. (B) An mAb against human IAP, 2D3, bound preferentially to whole RBCs prepared from SS, relative to AA RBCs (top). AA4 and SS4 are 2 of the donors identified in panel A. Similar results were obtained from the low-density fraction of SS RBCs (third panel), as indicated by the shift to the right in fluorescence intensity of the flow cytometry histograms. Immunostaining with 1F7, however, detected similar cell surface expression of IAP on SS and AA cells in the entire RBC population (second panel) and density fractionated RBCs from SS and AA samples (bottom). Each panel also contains a histogram from a sample treated with an isotype-matched control immunoglobulin G (IgG). Each histogram depicts 50 000 events and is representative of at least 2 separate samples. (C) Indirect immunofluorescence indicates that 1F7 bound to SS and AA RBCs equivalently at saturating concentrations of the antibody, further suggesting equivalent cell surface expression of IAP on SS and AA RBCs. Results were obtained from 50 000 events from 3 separate SS and AA donors and are shown (±SD) from mean fluorescence intensity.
SS RBCs and AA RBCs express equivalent amounts of IAP, but SS RBC IAP is structurally different from that on AA RBCs.
(A) (top) Representative Western blots of RBC membranes (25 μg) from 4 separate SS (SS1-SS4) or AA (AA1-AA4) donors probed with B6H12 indicate that SS RBC membranes react poorly with this mAb against IAP (n = 14; 4 representative samples shown). B6H12 reacted relatively robustly with an approximately 52-kd band on prepared AA RBC membranes (n = 14; 4 representative samples shown). These results suggest that the SDS-denatured epitope for B6H12 is compromised on SS RBC IAP. Reprobing the previous blot with a pAb against IAP and quantification by densitometry detected equivalent amounts of IAP extracted from SS and AA RBC membranes (middle). This result suggests equivalent amounts of IAP in intact membranes prepared from each of the AA and SS samples. An mAb against glycophorin A also detected equivalent amounts of this cell surface receptor extracted from AA and SS RBC membranes (bottom), further reinforcing equivalent protein extraction from both sets of prepared membranes. (B) An mAb against human IAP, 2D3, bound preferentially to whole RBCs prepared from SS, relative to AA RBCs (top). AA4 and SS4 are 2 of the donors identified in panel A. Similar results were obtained from the low-density fraction of SS RBCs (third panel), as indicated by the shift to the right in fluorescence intensity of the flow cytometry histograms. Immunostaining with 1F7, however, detected similar cell surface expression of IAP on SS and AA cells in the entire RBC population (second panel) and density fractionated RBCs from SS and AA samples (bottom). Each panel also contains a histogram from a sample treated with an isotype-matched control immunoglobulin G (IgG). Each histogram depicts 50 000 events and is representative of at least 2 separate samples. (C) Indirect immunofluorescence indicates that 1F7 bound to SS and AA RBCs equivalently at saturating concentrations of the antibody, further suggesting equivalent cell surface expression of IAP on SS and AA RBCs. Results were obtained from 50 000 events from 3 separate SS and AA donors and are shown (±SD) from mean fluorescence intensity.
To examine cell surface expression of IAP on SS RBCs, we immunostained SS (n = 4) and AA (n = 4) RBCs with the mAbs 2D3 and 1F7 against human IAP and analyzed RBC surface antibody binding by flow cytometry. As shown in the representative histograms, saturating concentrations of the 2D3 mAb exhibited increased fluorescence intensity of SS relative to AA RBCs (Figure 1B, top), which could indicate an increased availability of this epitope on SS RBCs. However, saturating concentrations of 1F7 (1 μg/mL) bound both SS and AA RBCs in equivalent amounts relative to an isotype-matched control IgG, suggesting an equivalent availability of the 1F7 epitope on AA and SS RBCs when IAP was in a native conformation in the plasma membrane (Figure 1B, second panel). Additionally, increasing concentrations of 1F7 clearly showed that at each concentration, SS RBCs and AA RBCs bound equivalent amounts of this antibody, further supporting equivalent expression levels of IAP (Figure 1C). Taken together, these results suggest that though it is expressed in equivalent amounts on SS and AA RBCs, IAP on SS RBCs—even in its native conformation in the plasma membrane—is structurally different from IAP on AA RBCs.
We previously demonstrated that the low-density, reticulocyte-enriched fraction of SS RBCs is the most adhesive to immobilized TSP under flow conditions.8 Therefore, we examined mAb binding and cell surface expression of IAP on this population of cells from both SS and AA donors. The difference in B6H12 reactivity on Western blots was observed in low-density, reticulocyte-enriched fractions of SS and AA RBCs (data not shown). The difference in 2D3 reactivity was observed as well; 2D3 bound preferentially to the SS reticulocyte-containing fraction compared to an equivalent population derived from AA donors (Figure 1B, third panel), further suggesting a different structure of IAP on these SS RBCs. However, by flow cytometry, both SS and AA low-density fractions bound equivalent amounts of 1F7 (Figure 1B, bottom), again suggesting equivalent cell surface expression on these immature cells. These results once more suggest that though IAP cell surface expression is equivalent among AA and SS RBCs of all ages, the structure of IAP on SS RBCs differs from that on AA RBCs.
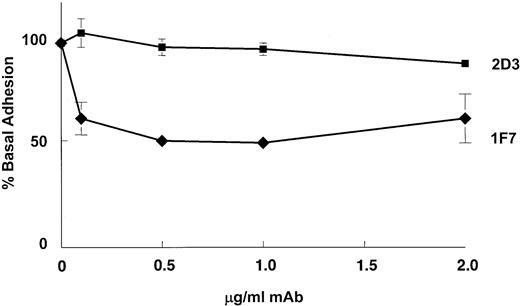
We next tested the hypothesis that IAP is an adhesion receptor on SS RBCs for immobilized TSP. Using 1F7 to selectively block any IAP–TSP interaction,22 we analyzed SS RBC adhesion to immobilized TSP under flow conditions. Pre-incubation of SS RBCs with saturating concentrations of 1F7, but not an isotype-matched control mAb (data not shown), blocked SS RBC adhesion to TSP by approximately 50% in a dose-dependent manner (Figure 2, diamonds), suggesting that IAP on SS RBCs mediates a significant amount of SS RBC adhesion to TSP under flow conditions. This result is not a general effect of an antibody binding to the surface of the RBC or even to IAP because antibodies against GPIV or glycophorin A, both of which bind SS RBCs, fail to inhibit adhesion to immobilized TSP under flow conditions.8 Additionally, 2D3, a nonfunction blocking antibody that binds to IAP,25 failed to block SS RBC adhesion to TSP at any concentration tested (Figure 2, squares), suggesting that 1F7 specifically interrupts an IAP–TSP interaction. These results suggest that IAP mediates a significant proportion of SS RBC adhesion to TSP, and implicate IAP as an adhesion receptor on SS RBCs.
IAP is an adhesion receptor on SS RBCs for immobilized TSP under flow conditions.
Pre-incubation (30 minutes) of SS RBCs with increasing concentrations of 1F7 inhibited basal adhesion of SS RBCs to immobilized TSP under flow conditions (rate, 1 mL/min; shear, 1 dyne/cm2) by approximately 50% (n = 11) (diamonds) in a dose-dependent manner. Identical incubation with the anti-IAP mAb 2D3 had no effect on adhesion (n = 3) (circles). The 100% adhesion represents an average of 212 cells/mm2 (±SD). An isotype-matched control antibody had no effect on SS RBC adhesion to TSP at any of the studied concentrations (data not shown).
IAP is an adhesion receptor on SS RBCs for immobilized TSP under flow conditions.
Pre-incubation (30 minutes) of SS RBCs with increasing concentrations of 1F7 inhibited basal adhesion of SS RBCs to immobilized TSP under flow conditions (rate, 1 mL/min; shear, 1 dyne/cm2) by approximately 50% (n = 11) (diamonds) in a dose-dependent manner. Identical incubation with the anti-IAP mAb 2D3 had no effect on adhesion (n = 3) (circles). The 100% adhesion represents an average of 212 cells/mm2 (±SD). An isotype-matched control antibody had no effect on SS RBC adhesion to TSP at any of the studied concentrations (data not shown).
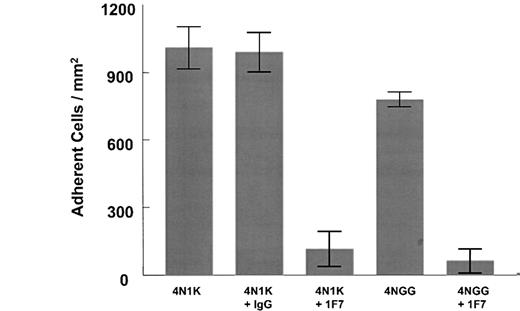
Because IAP on other cell types binds to the RFYVVMWK sequence in the cell-binding domain of TSP,23 we next asked whether this sequence in TSP also supports SS RBC adhesion. Consequently, we compared the binding of SS RBCs under flow to the immobilized 4N1K peptide containing this IAP-binding sequence, the previously characterized 4NGG control peptide containing 2 conservative mutations,23 or a scrambled 4N1K peptide termed 4N1KS (Figure 3). Although both 4N1K and 4NGG adsorbed equally to the plastic flow chamber and supported SS RBC adhesion, the native sequence appeared to be most adhesive. SS RBC adhesion to both immobilized peptides could be completely blocked by pre-incubation of the SS RBCs with 1F7 but not a control mAb, indicating an IAP-specific interaction with these peptides. In contrast, the scrambled 4N1KS peptide failed to support SS RBC adhesion, though this scrambled peptide adsorbed slightly better than the 4N1K or 4NGG peptide to the solid-phase support (data not shown). These results demonstrate a specific interaction of SS RBCs with a peptide derived from the cell-binding domain of TSP. Finally, washed RBCs from healthy controls failed to adhere to any of these peptides under flow conditions (data not shown) even though they express IAP (Figure 1). Taken together, these results indicate that a significant part of the mechanism by which sickle cells bind under basal flow conditions to immobilized TSP involves an interaction between IAP on the sickle cells and the cell-binding domain of TSP.
SS RBCs adhere to the cell-binding domain of TSP in an IAP-dependent manner.
SS RBCs were allowed to flow over immobilized 4N1K (KRFYVVMWKK) and 4NGG (KRFYGGMWKK) peptides, and adherent cells were counted. Both 4N1K and 4NGG supported adhesion under flow. Pre-incubation of the SS RBCs with 1 μg/mL 1F7 blocked adhesion to 4NGG peptide, whereas 2 μg/mL 1F7 was required to block adhesion to 4N1K. A scrambled 4N1K peptide, 4N1KS (KMRVYFVWKK), failed to support the adhesion of SS RBCs. An isotype-matched control antibody had no effect on adhesion to either peptide. Separate experiments indicated that 4N1K and 4NGG adsorbed equally, and that 4N1KS absorbed slightly more, to the plastic flow chamber, as indicated in “Materials and methods.”
SS RBCs adhere to the cell-binding domain of TSP in an IAP-dependent manner.
SS RBCs were allowed to flow over immobilized 4N1K (KRFYVVMWKK) and 4NGG (KRFYGGMWKK) peptides, and adherent cells were counted. Both 4N1K and 4NGG supported adhesion under flow. Pre-incubation of the SS RBCs with 1 μg/mL 1F7 blocked adhesion to 4NGG peptide, whereas 2 μg/mL 1F7 was required to block adhesion to 4N1K. A scrambled 4N1K peptide, 4N1KS (KMRVYFVWKK), failed to support the adhesion of SS RBCs. An isotype-matched control antibody had no effect on adhesion to either peptide. Separate experiments indicated that 4N1K and 4NGG adsorbed equally, and that 4N1KS absorbed slightly more, to the plastic flow chamber, as indicated in “Materials and methods.”
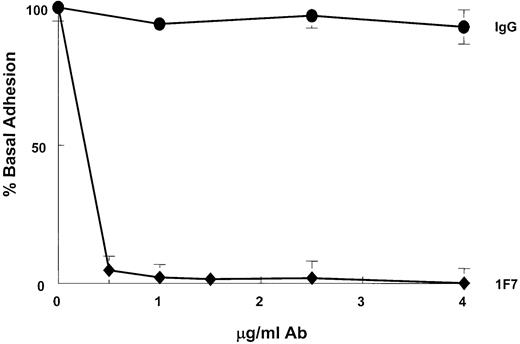
During the vaso-occlusive crisis, it is likely that blood flow and shear stress in an obstructed vessel become negligible. Therefore, we studied the contribution of IAP to SS RBC adhesion to TSP immobilized onto an identical substrate but in the absence of shear. Under static conditions, saturating concentrations of 1F7 completely inhibited SS RBC adhesion to immobilized TSP (Figure4, diamonds). This percentage inhibition was in contrast to our results under shear stress showing that 1F7 maximally inhibited adhesion by 49.5% (Figure 2, diamonds). An isotype-matched control antibody had no effect on SS RBC adhesion to TSP (Figure 4, circles). These results strongly suggest that IAP binding to the cell-binding domain in TSP may mediate SS RBC adhesion to the blood vessel wall in free-flowing vessels and under static conditions, proximal to an already formed vaso-occlusion.
IAP is a major adhesion receptor for immobilized TSP on SS RBCs under static conditions.
The 1F7 mAb blocked SS RBC adhesion to immobilized TSP in a dose-dependent manner under static conditions (diamonds), whereas an isotype-matched control IgG (circles) had no effect. Nearly maximal inhibition occurred at approximately 1 μg/mL 1F7 (94.5%; n = 3), and complete inhibition occurred at 4 μg/mL. The 100% adhesion represents an average of 9.6 × 105 total adherent cells/well (±SD). Neither 1F7 nor the isotype-matched control antibody had any effect on the sparse adhesion of AA RBCs to immobilized TSP observed under static conditions (data not shown).
IAP is a major adhesion receptor for immobilized TSP on SS RBCs under static conditions.
The 1F7 mAb blocked SS RBC adhesion to immobilized TSP in a dose-dependent manner under static conditions (diamonds), whereas an isotype-matched control IgG (circles) had no effect. Nearly maximal inhibition occurred at approximately 1 μg/mL 1F7 (94.5%; n = 3), and complete inhibition occurred at 4 μg/mL. The 100% adhesion represents an average of 9.6 × 105 total adherent cells/well (±SD). Neither 1F7 nor the isotype-matched control antibody had any effect on the sparse adhesion of AA RBCs to immobilized TSP observed under static conditions (data not shown).
Discussion
In this work, we provide evidence that IAP serves as an adhesion receptor on SS RBCs for immobilized TSP, a conformation of TSP thought to mimic matrix TSP or TSP adherent to the endothelium. We demonstrate that IAP is expressed on SS RBCs in amounts similar to those on AA RBCs but that the structure–conformation of IAP on SS RBCs is altered from that expressed on normal AA RBCs. We also show that the selective blockade of this receptor blocks SS RBC adhesion to immobilized TSP under flow conditions by approximately 50%, whereas the disruption of IAP function under static conditions results in a virtual ablation of SS RBC adhesion to immobilized TSP. Additionally, the IAP binding site within the C-terminal cell-binding domain of TSP supports SS RBC adhesion under flow conditions, implicating this adhesive sequence as a sickle cell binding site within TSP and supporting an adhesive role for IAP on SS RBCs.
Our data also suggest that IAP on the SS RBCs is structurally different than that expressed on AA RBCs, based on the relative loss of the denatured B6H12 epitope and the potentiation of 2D3 binding to the surface of SS RBCs compared to AA RBCs (Figure 1). Although it is intriguing to speculate that this change in antibody binding and the inferred structural difference in IAP on SS RBCs is solely responsible for a gain of IAP function on the SS RBCs, we are considering this possibility along with several other models. In the first model, we propose that expression of IAP is necessary, but not sufficient, to confer maximal SS RBC adhesion to TSP under flow conditions. We speculate that IAP-mediated adhesion under flow is also dependent on other TSP receptors expressed on SS RBCs, thus providing one explanation of the incomplete inhibition of adhesion by 1F7 under flow, even at saturating concentrations of this antibody. These other as yet unidentified, but necessary, receptors may serve to bind TSP, provide multiple adhesive contacts, and synergize with IAP to firmly anchor the SS RBC to TSP under shear stress. Studies of density-separated subpopulations of SS RBCs show that adhesion to TSP under flow is enhanced in the immature SS reticulocyte-enriched fraction of SS RBCs.8 Analysis of the same fraction of SS RBCs using flow cytometry also demonstrates that these “younger” cells express the TSP receptor CD36 or GPIV, as well as integrin α4β1.26,27 Despite the fact that CD36 alone does not mediate SS RBC adhesion to TSP under flow,26 either it or other poorly characterized TSP receptors in SS RBC adhesion may serve as co-receptors with IAP for TSP. In this regard, CD36 has been implicated in SS RBC binding to endothelial cells under static conditions.10 In contrast, normal RBCs that express IAP, but not the other adhesive receptors, remain nonadherent under flow.
It is interesting that SS RBC adhesion to TSP appears to be more sensitive to 1F7 inhibition under static conditions. In fact, saturating concentrations of 1F7 ablate SS RBC adhesion to TSP in the absence of shear (Figure 4, diamonds). This result may indicate that fewer adhesive contacts are required to sustain adhesion under static conditions and that the IAP–TSP interaction is sufficient in number and avidity to sustain stable adhesion to TSP in the absence of shear. Under flow conditions, however, 1F7 may be less efficient in disrupting the IAP–TSP interaction or may fail to bind all IAP sites. As a result, only a partial inhibition of SS RBC adhesion is observed under flow.
The loss of the denatured B6H12 epitope and the potentiation of 2D3 binding exclusively on SS RBCs clearly suggest a consistent difference between the structure of IAP on these cells versus AA RBCs. Therefore, another model of IAP's role on SS RBCs is that this structural change confers a gain of IAP function, namely enhanced RBC avidity for immobilized TSP. In support of this model, only SS RBCs, but not AA RBCs, adhere in an IAP-dependent manner to the immobilized IAP ligands (the 4N1K peptide derived from the cell-binding domain of TSP or TSP itself), even though both sets of RBCs express equivalent amounts of IAP. Therefore, an inference can be made that the structure or conformation of IAP on SS RBCs relative to AA RBCs more readily supports RBC adhesion under flow and static conditions.
Based on the structural gain of function model, it is tempting to speculate about the nature of the change between IAP on SS RBCs versus AA RBCs. The consistent difference in the structure of IAP between SS RBCs and AA RBCs could represent a linked polymorphism between the gene for IAP and expression of HbS. However, we hypothesize that any changes in IAP most likely result from differences in enzymatic and/or nonenzymatic, post-translational modification of IAP in SS patients. IAP has an immunoglobulin variable-like amino-terminal extracellular domain, followed by a predicted 5-membrane spanning region and a short cytoplasmic, carboxy-terminal region.21 IAP contains 6 N-linked glycosylation sites, 5 of which are in the immunoglobulin variable region—the region in which B6H12 binds.22 28Therefore, one structural change in IAP that could result in a change in B6H12 binding to denatured protein is a change in glycosylation of the protein. Alternatively, this change could be caused by post-translational modification of specific amino acids, such as the conversion of glutamic acid to glutamine, or glycation of ε-amino groups, which is known to occur in some proteins. Because of low oxygen tension, repeated ischemia–reperfusion injury, and hosts of other chronic vascular injuries and anemia in SS patients, it is likely that essential enzymes linked to protein processing have altered activity in SCD, potentially resulting in the expression of altered cellular proteins. The amino acid sequence of IAP, or other integral membrane proteins, has never been examined in SCD. Therefore, studies are under way to determine the exact nature of the change in IAP in this disease, and these studies may lead to the identification of several other abnormal modifier proteins in SCD.
Our data also identify the cell-binding domain of TSP as an adhesive sequence to which SS RBCs can bind under flow conditions. This result is consistent with that of Hillery et al,29 who demonstrated that the C-terminal domain of TSP is required for SS RBC adhesion, and it suggests that the identification of this sequence can be therapeutically exploited in SCD as an inhibitor of SS RBC adhesion to components in the vascular wall. Additionally, this adhesive sequence is present in the matrix molecule laminin,19,20,23 a molecule to which SS RBCs adhere under flow conditions,24 and it is elevated in the plasma of SCD patients.30 Thus, our results suggest that the TSP sequence indicated by the 4N1K peptide could represent a major adhesive and regulatory sequence for SS RBC adhesion in vivo.
In summary, our results suggest that IAP may be a major adhesion receptor on SS RBCs for the vascular protein TSP under flow and static conditions. We have further identified the site in TSP to which IAP binds as the cell-binding domain of this adhesive protein. Significantly, we have demonstrated that IAP on SS RBCs is structurally different from that expressed on AA RBCs. We speculate that this structural change may contribute directly to SS RBC adhesion in SCD and may, therefore, contribute to vaso-occlusion in this chronic illness. Although our studies thus far have identified IAP and the cell-binding domain of TSP as novel therapeutic targets in SCD, future studies promise to fully elucidate mechanisms of SS RBC adhesion, protein expression, and vaso-occlusion in SCD.
We thank Patrick Hines, Tina Leisner, E. M. Pickens, and David Shock for their assistance, support, and technical expertise in the preparation of this manuscript. In addition, we thank Jim Thompson, Dell Strayhorn, Susan Jones, and Jamie Hodges at the University of North Carolina Comprehensive Sickle Cell Center for their help in patient recruitment.
Supported by HL58939 (L.V.P.) and RR00046 (E.P.O.) from the National Institutes of Health.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Leslie V. Parise, Dept of Pharmacology, The University of North Carolina at Chapel Hill, CB#7365, Chapel Hill, NC 27599; e-mail: parise@med.unc.edu.