Abstract
Effects of the occupation of integrin αIIbβ3 by fibrinogen on Ca++signaling in fura-2–loaded human platelets were investigated. Adding fibrinogen to washed platelet suspensions inhibited increases in cytosolic [Ca++] concentrations ([Ca++]i) evoked by adenosine diphosphate (ADP) and thrombin in a concentration-dependent manner in the presence of external Ca++ but not in the absence of external Ca++ or in the presence of the nonselective cation channel blocker SKF96365, indicating selective inhibition of Ca++entry. Fibrinogen also inhibited store-mediated Ca++ entry (SMCE) activated after Ca++ store depletion using thapsigargin. The inhibitory effect of fibrinogen was reversed if fibrinogen binding to αIIbβ3 was blocked using RDGS or abciximab and was absent in platelets from patients homozygous for Glanzmann thrombasthenia. Fibrinogen was without effect on SMCE once activated. Activation of SMCE in platelets occurs through conformational coupling between the intracellular stores and the plasma membrane and requires remodeling of the actin cytoskeleton. Fibrinogen inhibited actin polymerization evoked by ADP or thapsigargin in control cells and in cells loaded with the Ca++ chelator dimethyl BAPTA. It also inhibited the translocation of the tyrosine kinase p60src to the cytoskeleton. These results indicate that the binding of fibrinogen to integrin αIIbβ3 inhibits the activation of SMCE in platelets by a mechanism that may involve modulation of the reorganization of the actin cytoskeleton and the cytoskeletal association of p60src. This action may be important in intrinsic negative feedback to prevent the further activation of platelets subjected to low-level stimuli in vivo.
Introduction
Integrin αIIbβ3(glycoprotein IIb/IIIa) is a member of the integrin family of receptors that mediate cellular adhesion of different cell types to several ligands, such as fibrinogen, fibronectin, and von Willebrand factor.1,2 Occupancy of specific sites of the integrin αIIbβ3 by a ligand affects its structure, function, and distribution.1 In addition, during aggregation of platelets, the receptor has been reported to associate with the cytoskeleton inducing actin filament reorganization.2 It has been shown that peptides containing the Arg-Gly-Asp sequence, known as the RGD sequence, present in the A-α chains of human fibrinogen, bind to potential recognition sites on the integrin αIIbβ3 for the binding of soluble fibrinogen on activated human platelets, thus inhibiting binding of fibrinogen with the receptor.3,4Platelet agonists activate integrin αIIbβ3(inside-out signaling) to allow the binding of soluble fibrinogen followed by outside-in signals involving phosphorylation events, cytoskeletal rearrangements, and molecular translocations.5
Stimulation of human platelets with various agonists results in an elevation in the [Ca++]i that consists of 2 components; release of Ca++ from the intracellular stores and activation of Ca++ entry through plasma membrane channels.6 Store-mediated Ca++ entry (SMCE) is the main mechanism responsible for Ca++ influx in human platelets7; however, the mechanism by which the filling state of the Ca++ stores is communicated to the plasma membrane is poorly understood. Current hypotheses fall into 2 main categories: indirect coupling and direct coupling.8Recently, the direct coupling model has received support from studies indicating that the mechanism of activation of SMCE shares properties with the activation of secretion.9-11 In different cell types, including human platelets, the reorganization of the actin cytoskeleton appears to play a pivotal role in the activation of SMCE, possibly by mediating translocation of the Ca++ stores to the plasma membrane to facilitate the coupling process.9 11
It has been reported that integrin αIIbβ3might be involved in the regulation of [Ca++]i in platelets2; however, the mechanisms responsible have not been clearly addressed. It has been reported that integrin αIIbβ3 contains high-affinity Ca++-binding sites,12 and earlier studies have suggested that this integrin may act as a Ca++ channel.13 Here we have investigated the effects of occupation of integrin αIIbβ3 on agonist-induced [Ca++]i elevations. Our results indicate that integrin αIIbβ3occupation results in a reduction of SMCE by preventing agonist-induced actin polymerization and cytoskeletal association of p60srcin human platelets. Some of these data have been published in preliminary form.14
Materials and methods
Materials
Fura-2 acetoxymethyl ester (fura-2/am) was from Texas Fluorescence (Austin, TX). Apyrase (grade V), aspirin, α,β-methylene adenosine triphosphate (ATP), bovine serum albumin (BSA), adenosine diphosphate (ADP), fibrinogen, lanthanum chloride, paraformaldehyde, Nonidet P-40, fluorescein isothiocyanate–labeled phalloidin, RGDS peptide, thrombin, thapsigargin (TG), and vasopressin were from Sigma (Poole, Dorset, United Kingdom). Ionomycin, cytochalasin D (CD), PPACK dihydrochloride (D-Phe-Pro-Arg-chloromethylketone, HCl) and SKF96365 were from Calbiochem (Nottingham, United Kingdom). Jasplakinolide (JP) was from Molecular Probes (Leiden, The Netherlands). Protein A-agarose and anti-p60src monoclonal antibody GD11 were from Upstate Biotechnology (Lake Placid, NY). Antiphosphotyrosine monoclonal antibody (PY20) was from Transduction Laboratories (Lexington, KY). Horseradish peroxidase–conjugated ovine antimouse IgG antibody (NA931) was from Amersham (Buckinghamshire, United Kingdom). Reopro (abciximab) was from Lilly (Basingstoke, United Kingdom). All other reagents were of analytical grade.
Platelet preparation
Fura-2–loaded platelets were prepared as described previously.15 Briefly, blood was collected by venipuncture from healthy drug-free volunteers and mixed with one-sixth volume acid–citrate dextrose anticoagulant (85 mM sodium citrate, 78 mM citric acid, and 111 mM D-glucose). Platelet-rich plasma was then prepared by centrifugation for 5 minutes at 700g, and aspirin (100 μM) and apyrase (40 μg/mL) were added. Platelet-rich plasma was incubated at 37°C with 2 μM fura-2/am for 45 minutes. In some experiments, platelets were co-loaded with dimethyl BAPTA by adding 10 μM dimethyl BAPTA/am for the final 30 minutes of incubation. Cells were then collected by centrifugation at 350g for 20 minutes and resuspended in HEPES-buffered saline (HBS; 145 mM NaCl, 10 mM HEPES, 10 mM D-glucose, 5 mM KCl, 1 mM MgSO4, pH 7.45) supplemented with 0.1% wt/vol BSA and 40 μg/mL apyrase. Where indicated, 5 μM PPACK was added. Blood samples were also obtained from 5 adult patients homozygous for Glanzmann thrombasthenia and from age- and sex-matched healthy controls. Patients and controls did not use antiplatelet medication.
Measurement of [Ca++]i
Fluorescence was recorded from 1.5-mL aliquots of magnetically stirred washed platelet suspension (108 cells/mL) at 37°C using a Cairn Research Spectrophotometer (Cairn Research, Faversham, Kent, United Kingdom) with excitation wavelengths of 340 and 380 nm and emission at 500 nm. Changes in [Ca++]i were monitored using the fura-2 340/380 fluorescence ratio and calibrated according to the method of Grynkiewicz et al.16Measurements on platelets from patients with Glanzmann thrombocytopenia and from matched controls were performed using an SLM Aminco 8100 spectrophotometer (Aminico, Rochester, NY) as described previously.17
Determination of [Ca++]i elevation
Agonist-evoked [Ca++]i elevation was measured as the integral of the rise in [Ca++]i above basal levels for 1½ minutes after the addition of the agonist in the presence of external Ca++. Ca++ entry in TG-induced store-depleted platelets was estimated using the integral of the rise in [Ca++]i15 17 for 2½ minutes after the addition of CaCl2.
Measurement of F-actin content
The F-actin content of resting and activated platelets was determined as previously described.11 Briefly, washed platelets (2 × 108 cells/mL) were activated in HBS. Samples of platelet suspension (200 μL) were transferred to 200 μL ice-cold 3% (wt/vol) formaldehyde in phosphate-buffered saline (PBS) for 10 minutes. Fixed platelets were permeabilized by incubation for 10 minutes with 0.025% (vol/vol) Nonidet P-40 detergent dissolved in PBS. Platelets were then incubated for 30 minutes with fluorescein isothiocyanate–labeled phalloidin (1 μM) in PBS supplemented with 0.5% (wt/vol) BSA. After incubation, the platelets were collected by centrifugation in an MSE Micro-Centaur Centrifuge (MSE Scientific Instruments, Crawley, Sussex, United Kingdom) for 90 seconds at 3000g and resuspended in PBS. Staining of 2 × 107 cells/mL was measured using a Perkin-Elmer (Norwalk, CT) Fluorescence Spectrophotometer. Samples were excited at 496 nm, and emission was at 516 nm.
Analysis of cytoskeleton-associated p60src
Human platelet fractionation was carried out according to a procedure published previously.18 Briefly, activated and control platelets (2 × 109 cells/mL) were immediately lysed with an equal volume of 2 × Triton buffer (2% Triton X-100, 2 mM EGTA, 100 mM Tris-HCl, pH 7.2, 100 μg/mL leupeptin, 2 mM phenylmethylsulfonyl fluoride, 10 mM benzamidine, and 2 mM Na3VO4) at 4°C for 30 minutes. Platelet lysate was centrifuged at 16 000g for 5 minutes. The supernatant was removed, and the pellet (cytoskeleton-rich fraction) was solubilized into the original volume in Laemmli's buffer,19 boiled for 5 minutes, and subjected to Western blotting using the anti-p60src monoclonal antibody GD11.
Western blotting
Proteins were electrophoresed on 7.5% sodium dodecyl sulfate–polyacrylamide gels and electrophoretically transferred for 2 hours at 0.8 mA/cm2 in a semidry blotter (Hoefer Scientific, Newcastle, Staffordshire, United Kingdom) onto nitrocellulose membranes for subsequent probing. Blots were incubated overnight with 10% (wt/vol) BSA in Tris-buffered saline with 0.1% Tween 20 (TBST) to block residual protein-binding sites. Membranes were then incubated for 1 hour with anti-p60src monoclonal antibody (GD11) diluted 1:500 in TBST. The primary antibody was removed, and blots were washed 6 times for 5 minutes each with TBST. To detect the primary antibody, blots were incubated with horseradish peroxidase–conjugated ovine antimouse IgG antibody diluted 1:10 000 in TBST, washed 6 times in TBST, and exposed to enhanced chemiluminescence reagents for 1 minute. Blots were then exposed to preflashed photographic film. The density of bands on the film was measured using a Quantimet 500 densitometer (Leica, Milton Keynes, United Kingdom).
Statistical analysis
Values stated are mean ± SE of the number of observations (n) indicated. Analysis of statistical significance was performed using Student t test. For multiple comparison, one-way analysis of variance combined with the Dunnett test was used. P < .05 was considered statistically significant.
Results
Fibrinogen inhibits ADP-evoked Ca++ elevations
Fura-2–loaded aspirin-treated human platelets were used to assess Ca++ responses evoked by different agonists. As previously reported,20 in the presence of 1 mM external Ca++, 5 μM ADP evoked a transient increase in [Ca++]i. The addition of fibrinogen 45 seconds before stimulation with ADP decreased the [Ca++]i elevation in a concentration-dependent manner (Figure1A; n = 5). Fibrinogen significantly decreased the ADP-evoked Ca++ elevation (see “Materials and methods”) by 17% ± 6%, 41% ± 1%, and 61% ± 4% at 0.1, 0.3, and 1 mg/mL, respectively (Figure 1A;P < .05; n = 5). As shown in Figure 1B, in the presence of 1 mM external Ca++, 5 μM ADP evoked a peak [Ca++]i rise of 321 ± 22 nM (n = 7), which, in the presence of 1 mg/mL fibrinogen, was reduced to 213 ± 33 nM (P < .05; n = 7 ). When experiments were performed in the presence of 5 μM PPACK to inactivate traces of thrombin that might have been generated, the same results were obtained (data not shown). RGDS has been reported to inhibit the binding of fibrinogen with its receptor.21 Under our experimental conditions, the addition of RGDS (100 μM) did not alter the elevation in [Ca++]i evoked by ADP, thrombin, or vasopressin (data not shown). However, the addition of RGDS (100 μM) 45 seconds before fibrinogen reversed the effect of fibrinogen. In the presence of both RGDS and fibrinogen, treatment of platelets with 5 μM ADP evoked a peak [Ca++]i elevation of 285 ± 37 nM, similar to that reported under control conditions (Figure 1B;P > .05; n = 7). Similar results were obtained using abciximab (ReoPro, a chimeric antibody against αIIbβ3). Addition of abciximab (5 μM) 45 seconds before fibrinogen completely reversed its inhibitory effect (Figure 1C; n = 5).
Fibrinogen inhibits ADP-evoked elevations in [Ca++]i.
(A) Fura-2–loaded human platelets suspended in an HBS containing 1 mM Ca++ were stimulated with ADP (5 μM) in the absence (Control) or presence of various concentrations of fibrinogen (FG; 0.1-1 mg/mL). [Ca++]i was monitored as described in “Materials and methods.” (B, C) Human platelets were stimulated with ADP (5 μM) in the absence (Control) or presence of either fibrinogen alone (FG; 1 mg/mL) or fibrinogen (1 mg/mL) in combination with RGDS (100 μM) (FG + RGDS; B) or abciximab (5 μg/mL) (ReoPro; FG + Ab; C). Traces shown are representative of 5 independent experiments.
Fibrinogen inhibits ADP-evoked elevations in [Ca++]i.
(A) Fura-2–loaded human platelets suspended in an HBS containing 1 mM Ca++ were stimulated with ADP (5 μM) in the absence (Control) or presence of various concentrations of fibrinogen (FG; 0.1-1 mg/mL). [Ca++]i was monitored as described in “Materials and methods.” (B, C) Human platelets were stimulated with ADP (5 μM) in the absence (Control) or presence of either fibrinogen alone (FG; 1 mg/mL) or fibrinogen (1 mg/mL) in combination with RGDS (100 μM) (FG + RGDS; B) or abciximab (5 μg/mL) (ReoPro; FG + Ab; C). Traces shown are representative of 5 independent experiments.
Effect of fibrinogen and RGDS peptide on thrombin-evoked Ca++ elevations
Figure 2 shows that the addition of fibrinogen (1 mg/mL) 45 seconds before the agonist resulted in substantial inhibition of the elevation in [Ca++]i evoked by thrombin (0.1 U/mL) in medium containing 1 mM Ca++. The initial peak [Ca++]i elevation above basal level after treatment with agonist was decreased significantly from 351 ± 58 to 194 ± 60 nM (P < .01; n = 7). Fibrinogen significantly reduced the integral of the thrombin-evoked elevation in [Ca++]i by 44% ± 4% (P < .001). As with ADP, RGDS reversed the inhibition of the thrombin-evoked elevation in [Ca++]i by fibrinogen. In the presence of RGDS (100 μM), fibrinogen only slightly reduced the initial peak of the rise in [Ca++]i evoked by thrombin from 351 ± 58 to 272 ± 22 nM (Figure 2A; P > .05;n = 7).
Fibrinogen inhibits thrombin-evoked elevations in [Ca++]i.
(A) Fura-2–loaded human platelets were stimulated with thrombin (0.1 U/mL) in the absence (Control) or presence of either fibrinogen alone (FG; 1 mg/mL) or fibrinogen after the addition of 100 μM RGDS (FG + RGDS). Traces are representative of 7 separate experiments.
Fibrinogen inhibits thrombin-evoked elevations in [Ca++]i.
(A) Fura-2–loaded human platelets were stimulated with thrombin (0.1 U/mL) in the absence (Control) or presence of either fibrinogen alone (FG; 1 mg/mL) or fibrinogen after the addition of 100 μM RGDS (FG + RGDS). Traces are representative of 7 separate experiments.
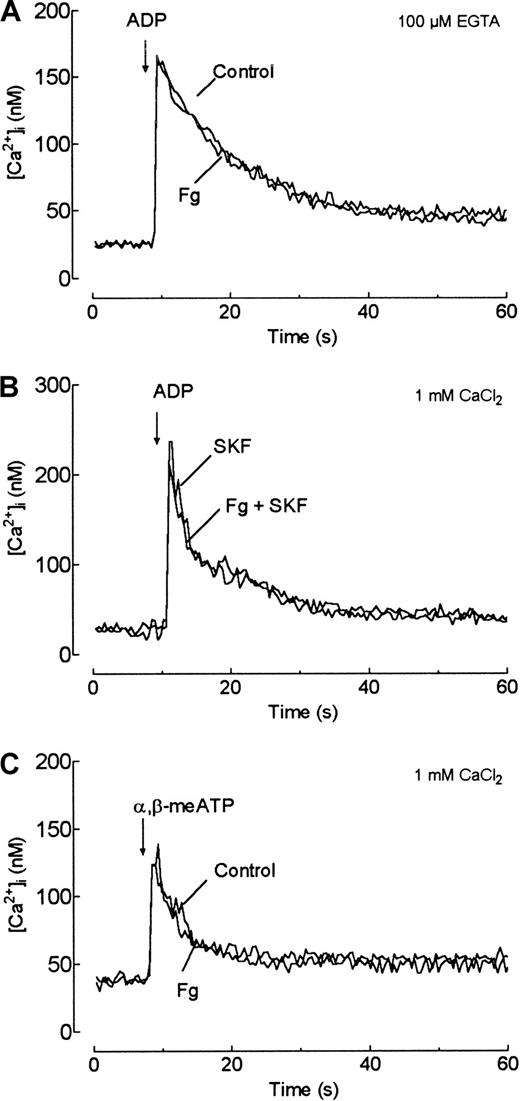
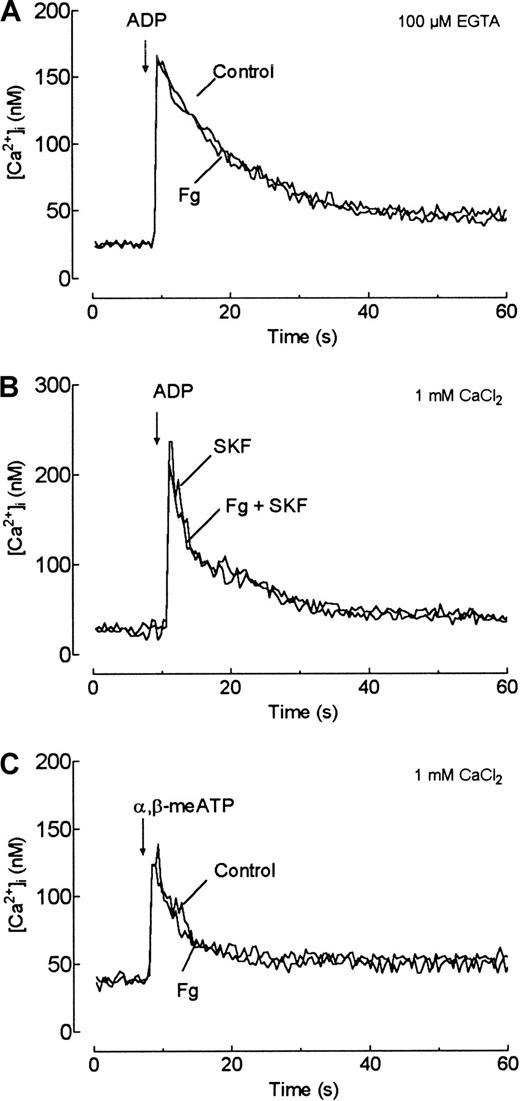
Fibrinogen inhibits receptor-operated Ca++entry
To address the role of fibrinogen in modulating Ca++signaling, we studied its effect on ADP-evoked release of Ca++ from the internal stores. Although the preincubation of platelets with high concentrations of EGTA (5 mM) induces dissociation of the αIIbβ3 complex, reducing the ability of this receptor to bind fibrinogen,22,23 more recent studies have demonstrated that incubation in the presence of lower concentrations of EGTA (500 μM) does not destroy the complex.1 Using flow cytometry, we have found that under our experimental conditions, the incubation of platelets for 30 seconds in the presence of 100 μM EGTA did not interfere with the binding of fibrinogen to the αIIbβ3 complex (data not shown). In the absence of external Ca++ (100 μM EGTA added), fibrinogen was without effect on the ADP-induced rise in [Ca++]i, suggesting no effect on the release of Ca++ from the intracellular stores (Figure3A). To further investigate this issue, we monitored ADP-evoked Ca++ release in a medium containing external Ca++ and SKF96365, a nonselective cation channel blocker.24 In a medium containing 1 mM Ca++, treatment of human platelets with ADP (5 μM) in the presence of SKF96365 (50 μM) evoked a Ca++ elevation similar to that observed in the absence of external Ca++, indicating that SKF96365 abolished Ca++ entry under our conditions (data not shown). As shown in Figure 3B, in the presence of SKF96365, the addition of fibrinogen (1 mg/mL) to the platelet suspension 45 seconds before ADP did not alter ADP-induced Ca++ mobilization (P > .05; n = 6). These findings strongly suggest that the effect of fibrinogen on Ca++ signaling is a selective inhibition of Ca++ entry over internal release.
Effects of fibrinogen on ADP-evoked release of Ca++ from internal stores and P2x1receptor-mediated Ca++ entry.
(A) Fura-2–loaded human platelets were suspended in Ca++-free medium and stimulated with ADP (5 μM) in the absence (Control) or presence of fibrinogen (FG; 1 mg/mL). (B) Human platelets were suspended in an HBS containing 1 mM Ca++ in the presence of SKF96365 (50 μM). Platelets were then stimulated with ADP (5 μM) in the absence (SKF) or presence of fibrinogen (1 mg/mL) (FG + SKF). (C) Human platelets were suspended in an HBS containing 1 mM Ca++. Platelets were then stimulated with α,β-methylene ATP (10 μM) in the absence (Control) or presence of fibrinogen (FG; 1 mg/mL). Traces shown are representative of 6 to 10 independent experiments.
Effects of fibrinogen on ADP-evoked release of Ca++ from internal stores and P2x1receptor-mediated Ca++ entry.
(A) Fura-2–loaded human platelets were suspended in Ca++-free medium and stimulated with ADP (5 μM) in the absence (Control) or presence of fibrinogen (FG; 1 mg/mL). (B) Human platelets were suspended in an HBS containing 1 mM Ca++ in the presence of SKF96365 (50 μM). Platelets were then stimulated with ADP (5 μM) in the absence (SKF) or presence of fibrinogen (1 mg/mL) (FG + SKF). (C) Human platelets were suspended in an HBS containing 1 mM Ca++. Platelets were then stimulated with α,β-methylene ATP (10 μM) in the absence (Control) or presence of fibrinogen (FG; 1 mg/mL). Traces shown are representative of 6 to 10 independent experiments.
To assess whether fibrinogen might mediate these effects by Ca++ channel blockage, we investigated the effect of fibrinogen on Ca++ entry mediated by activation of P2x1 receptors, which act as cation channels.25 As shown in Figure 3C, the addition of fibrinogen 45 seconds before the P2x1-selective agonist, α,β-methylene ATP, did not modify the entry of Ca++ by P2x1 receptors (P > .05; n = 10), suggesting that the inhibitory effect of fibrinogen on agonist-evoked Ca++ entry is not caused by the blockage of this Ca++ channel.
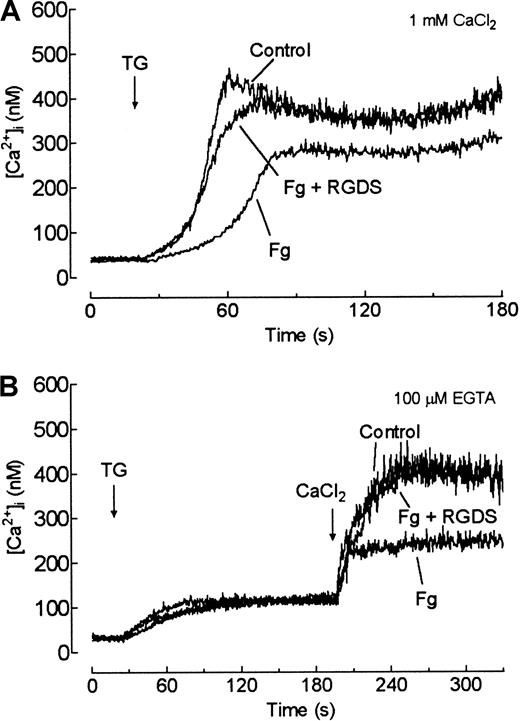
Fibrinogen reduces store-mediated Ca++ entry
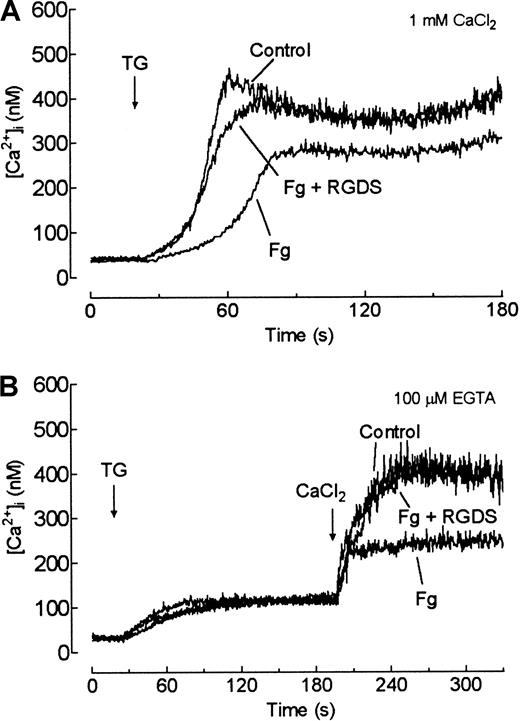
To directly address the specific inhibitory role of fibrinogen on Ca++ entry, we investigated its effect on SMCE. In a medium containing 1 mM Ca++, TG, a specific inhibitor of the Ca++-ATPase of the internal stores (the sarcoplasmic/endoplasmic–reticulum Ca++-ATPase, or SERCA),26 27 evoked a transient increase in [Ca++]i in platelets mediated by the release of Ca++ from the internal stores and Ca++ entry (Figure 4A). The addition of fibrinogen (1 mg/mL) 45 seconds before TG (200 nM) significantly decreased the elevation in [Ca++]i by 25% ± 5% (Figure4A; P < .01; n = 5). As shown in Figure 4A, the addition of RGDS (100 μM) before fibrinogen reversed the fibrinogen-induced inhibition of TG-evoked Ca++entry.
Fibrinogen inhibits store-mediated Ca++entry.
(A) Fura-2–loaded human platelets suspended in HBS containing 1 mM Ca++ were stimulated with TG (1 μM) in the absence (Control) or presence of either fibrinogen (1 mg/mL) (FG) or fibrinogen after the addition of 100 μM RGDS (FG + RGDS). (B) Human platelets were stimulated in a Ca++-free medium (100 μM EGTA) with ΤG (200 nM) in the absence (Control) or presence of fibrinogen 1 mg/mL (FG) or fibrinogen after the addition of (100 μM) RGDS (FG + RGDS). Three minutes later, CaCl2 (final concentration, 300 μM) was added to the medium to initiate Ca++ entry. Traces shown are representative of 5 to 6 independent experiments.
Fibrinogen inhibits store-mediated Ca++entry.
(A) Fura-2–loaded human platelets suspended in HBS containing 1 mM Ca++ were stimulated with TG (1 μM) in the absence (Control) or presence of either fibrinogen (1 mg/mL) (FG) or fibrinogen after the addition of 100 μM RGDS (FG + RGDS). (B) Human platelets were stimulated in a Ca++-free medium (100 μM EGTA) with ΤG (200 nM) in the absence (Control) or presence of fibrinogen 1 mg/mL (FG) or fibrinogen after the addition of (100 μM) RGDS (FG + RGDS). Three minutes later, CaCl2 (final concentration, 300 μM) was added to the medium to initiate Ca++ entry. Traces shown are representative of 5 to 6 independent experiments.
Another index for SMCE is the rapid elevation in [Ca++]i after the addition of CaCl2 to suspensions of store-depleted platelets. Cells were treated with TG (200 nM) in a Ca++-free medium, and, 3 minutes later, CaCl2 (300 μM) was added to initiate Ca++ entry. Consistent with the results obtained in the presence of 1 mM Ca++, the addition of fibrinogen (1 mg/mL) before TG significantly reduced the Ca++ entry by 61% ± 6% (Figure 4B; P < .01; n = 6). As shown in Figure 4B, this effect of fibrinogen was completely blocked by RGDS.
Cytosolic Ca++ concentration is a result of the balance between the mechanisms involved in Ca++ intake and removal from the cytosol. Ca++ release from the intracellular stores and Ca++ entry are responsible for rises in [Ca++]i, whereas the sequestration of Ca++ in the internal stores—and mainly the plasma membrane Ca++ ATPase—remove Ca++ from the cytosol in human platelets.28 Sequential activation of these systems results in changes in [Ca++]i. To investigate whether the effect of fibrinogen on [Ca++]icould be mediated by enhancing the activity of plasma membrane Ca++ ATPase and the subsequent removal of Ca++from the cell, we studied this process in platelets in the absence and presence of fibrinogen, following a recently described procedure.28 The treatment of human platelets in a Ca++-free medium with TG (1 μM) plus a low concentration of ionomycin (50 nM, required for extensive depletion of the internal Ca++ stores in platelets) resulted in a transient increase in [Ca++]i mediated by the leakage of Ca++ from the internal stores minus Ca++extrusion. The rate of decay of [Ca++]i to basal levels can be used as an index to estimate Ca++extrusion.28 Under these conditions, in both the absence and the presence of fibrinogen (1 mg/mL), treatment of platelets with TG plus ionomycin induced a similar elevation in [Ca++]I, and the rates of decay of [Ca++]i to basal levels were also similar under both conditions (data not shown). These findings suggested that the smaller Ca++ elevation observed after the stimulation of platelets in the presence of fibrinogen were not mediated by acceleration of the rate of Ca++ extrusion in human platelets. Therefore, because we demonstrated that fibrinogen did not modify Ca++ release from the internal stores, these results provide further evidence to suggest that fibrinogen interferes with Ca++ entry.
Effect of fibrinogen on Ca++ elevations in preactivated platelets
To further investigate the role of fibrinogen in Ca++entry, we examined the effect of the addition of fibrinogen after platelet activation. As shown in Figure5A, the addition of fibrinogen (FG; 1 mg/mL) 45 seconds before ADP (5 μM) clearly reduced the ADP-induced Ca++ elevation (FG ± control). Addition of fibrinogen 10 seconds after platelet activation had no effect on the ADP-induced response. The lack of effect of fibrinogen after platelet activation was confirmed using TG to activate the platelets. In both a Ca++-free medium and the presence of 1 mM external Ca++, the addition of fibrinogen (1 mg/mL) to TG-pretreated platelets did not alter store depletion-induced Ca++ entry (Figure 5B-C). In contrast, the addition of 100 μM lanthanum, a nonspecific cation channel blocker, caused a rapid decrease in [Ca++]i over the same time course (Figure5C), indicating that Ca++ entry had been inhibited. Together, these results indicate that fibrinogen is able to inhibit agonist-evoked and store-regulated Ca++ entry, an effect that can be reversed by the RGDS peptide. The lack of effect of fibrinogen on previously activated platelets indicates that it affects the activation but not the maintenance of SMCE.
Effect of fibrinogen on the maintenance of Ca++ entry.
(A) Fura-2–loaded human platelets suspended in HBS containing 1 mM Ca++ were stimulated with ADP (5 μM) (Control). Fibrinogen (1 mg/mL) was added 10 seconds later (FG), as shown by the arrow, or 45 seconds before the addition of ADP (FG [control]). (B) Human platelets suspended in HBS containing 1 mM Ca++ were stimulated with TG (200 nM) (Control). The addition of fibrinogen (FG; 1 mg/mL) was made 1½ minutes after the addition of TG, as shown by the arrow. (C) Human platelets were stimulated in a Ca++-free medium (100 μM EGTA) with ΤG (200 nM). Three minutes later, CaCl2 (final concentration, 300 μM) was added to the medium to initiate Ca++ entry (Control). The addition of fibrinogen (FG; 1 mg/mL) or lanthanum chloride (LaCl3; 100 μg/mL) was made 2 minutes after the addition of Ca++, as shown by the arrow. Traces shown are representative of 6 independent experiments.
Effect of fibrinogen on the maintenance of Ca++ entry.
(A) Fura-2–loaded human platelets suspended in HBS containing 1 mM Ca++ were stimulated with ADP (5 μM) (Control). Fibrinogen (1 mg/mL) was added 10 seconds later (FG), as shown by the arrow, or 45 seconds before the addition of ADP (FG [control]). (B) Human platelets suspended in HBS containing 1 mM Ca++ were stimulated with TG (200 nM) (Control). The addition of fibrinogen (FG; 1 mg/mL) was made 1½ minutes after the addition of TG, as shown by the arrow. (C) Human platelets were stimulated in a Ca++-free medium (100 μM EGTA) with ΤG (200 nM). Three minutes later, CaCl2 (final concentration, 300 μM) was added to the medium to initiate Ca++ entry (Control). The addition of fibrinogen (FG; 1 mg/mL) or lanthanum chloride (LaCl3; 100 μg/mL) was made 2 minutes after the addition of Ca++, as shown by the arrow. Traces shown are representative of 6 independent experiments.
Fibrinogen does not modify platelet Ca++ signaling in platelets from patients with Glanzmann thrombasthenia
The addition of 1 mM fibrinogen 45 seconds before stimulation with 5 mM ADP had little effect on the elevation in [Ca++]i in platelets from patients homozygous for Glanzmann thrombasthenia, reducing this to 94.3% ± 5.7% of control (P > .1; n = 8). In platelets from healthy controls prepared in parallel, fibrinogen reduced the ADP-evoked rise in [Ca++]i to 72.9% ± 4.7% of control (P < .001; n = 7). The integral of the ADP-evoked rise in [Ca++]i was reduced to 71.5% ± 2.0% of control (P < .001; n = 7) in platelets from healthy controls compared with 93.5% ± 8.5% of control (P > .2; n = 8) in platelets from patients with Glanzmann thrombasthenia.
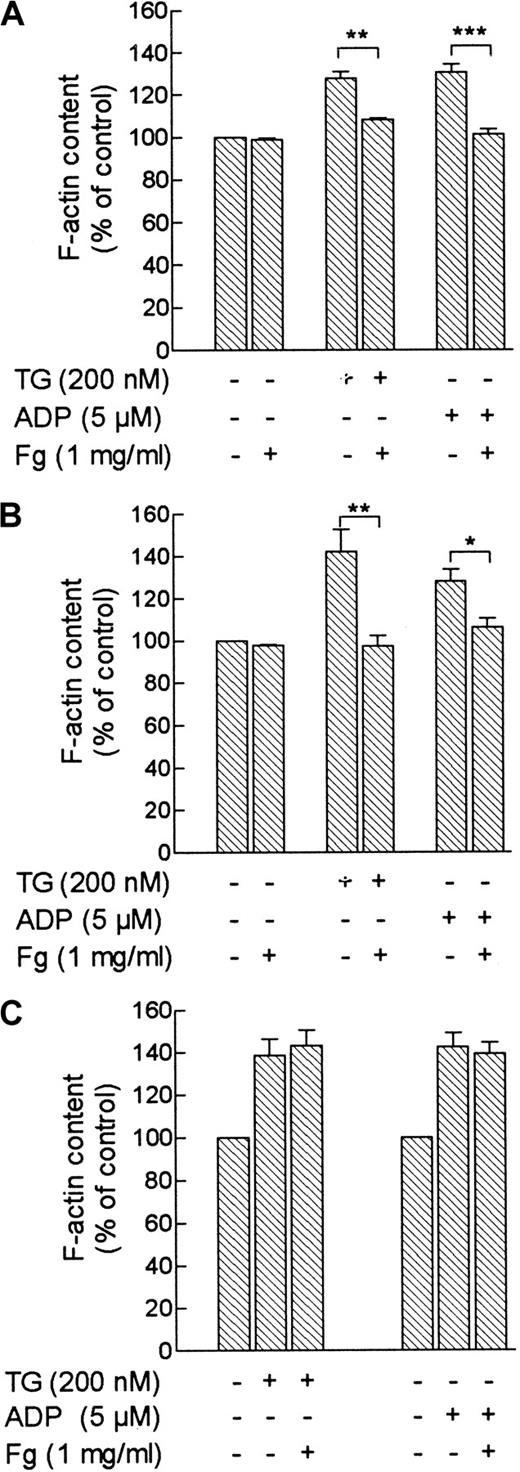
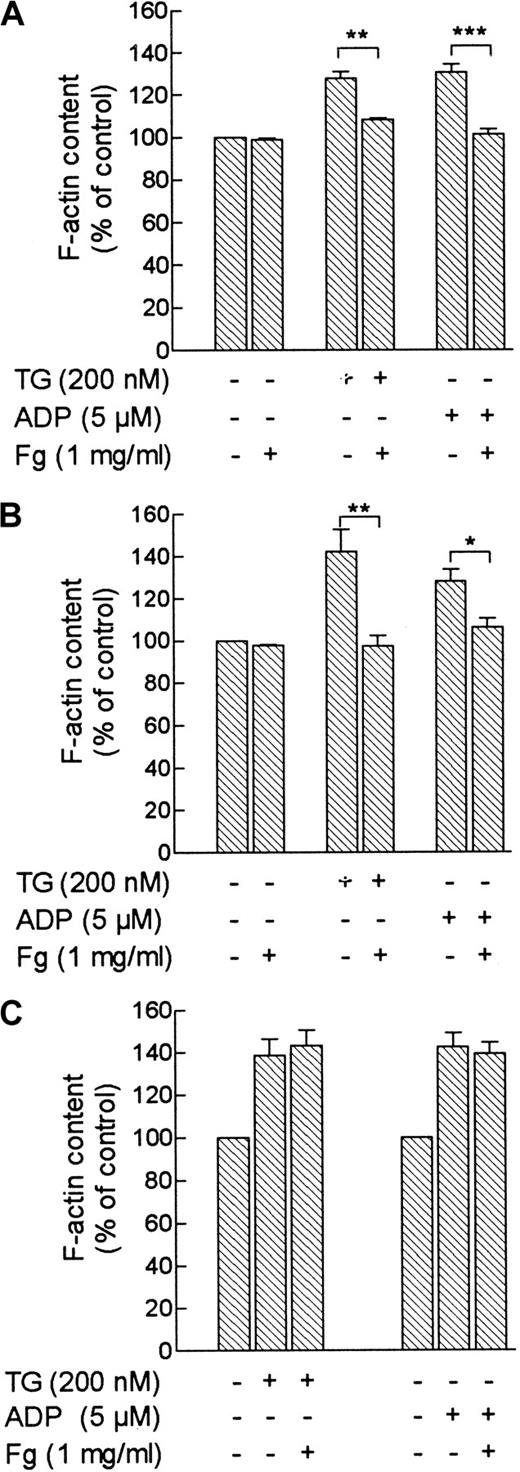
Role of fibrinogen in reorganization of the actin cytoskeleton in human platelets
It has previously been shown that the treatment of human platelets with ADP or TG induces actin polymerization.15,29 Because reorganization of the actin cytoskeleton has been reported to play a key role in the activation and maintenance of SMCE in different cell types, including platelets,9-11 we tested whether the actin cytoskeleton was involved in the inhibitory effect of fibrinogen on Ca++ entry in platelets. Treatment of platelets with TG (1 μM) or ADP (5 μM) in the presence of 1 mM external Ca++ enhanced F-actin content by 30% ± 3% and 34% ± 4%, respectively. In the presence of fibrinogen (1 mg/mL), TG- and ADP-induced actin polymerization was significantly inhibited by 66% ± 1% and 88% ± 2%, respectively (Figure6A; P < .01; n = 6). As shown in Figure 6A, fibrinogen was without significant effect on the actin filament content of unstimulated platelets. To investigate whether the effect of fibrinogen is mediated by a reduction in [Ca++]i elevation, we loaded platelets with the Ca++ chelator dimethyl BAPTA to prevent [Ca++]i rises.30 In dimethyl BAPTA-loaded human platelets, we found similar results. Treatment of platelets with 1 μM TG or 5 μM ADP enhanced actin filament content by 51% ± 10% and 32% ± 6%, respectively. The responses observed after platelet stimulation with TG or ADP were significantly reduced in the presence of fibrinogen (1 mg/mL) by 88% ± 5% and 72% ± 5%, respectively (Figure 6B; P < .05; n = 6).
Effect of fibrinogen on TG- or ADP-evoked actin polymerization in platelets.
Control human platelets (A) or dimethyl BAPTA-loaded platelets (B) were treated with TG (200 nM), ADP (5 μM), or the vehicle (HBS) in the absence or presence of 1 mg/mL fibrinogen. Samples were removed 5 seconds before and 3 minutes after the addition of the stimuli, and actin filament content was determined as described in “Materials and methods.” Values given are actin filament content as percentages of basal (HBS-treated platelets) and are expressed as mean ± SE from 6 independent determinations. *P < .05; **P < .01; ***P < .001. (C) Human platelets were stimulated with TG (200 nM) or ADP (5 μM), and 10 seconds later fibrinogen (1 mg/mL) or the vehicle (HBS) was added. Samples were removed 5 seconds before and 3 minutes after the addition of the stimuli, and actin filament content was determined as described in “Materials and methods.” Values given are actin filament contents as percentages of basal (nontreated platelets) and are expressed as mean ± SE from 6 independent determinations.
Effect of fibrinogen on TG- or ADP-evoked actin polymerization in platelets.
Control human platelets (A) or dimethyl BAPTA-loaded platelets (B) were treated with TG (200 nM), ADP (5 μM), or the vehicle (HBS) in the absence or presence of 1 mg/mL fibrinogen. Samples were removed 5 seconds before and 3 minutes after the addition of the stimuli, and actin filament content was determined as described in “Materials and methods.” Values given are actin filament content as percentages of basal (HBS-treated platelets) and are expressed as mean ± SE from 6 independent determinations. *P < .05; **P < .01; ***P < .001. (C) Human platelets were stimulated with TG (200 nM) or ADP (5 μM), and 10 seconds later fibrinogen (1 mg/mL) or the vehicle (HBS) was added. Samples were removed 5 seconds before and 3 minutes after the addition of the stimuli, and actin filament content was determined as described in “Materials and methods.” Values given are actin filament contents as percentages of basal (nontreated platelets) and are expressed as mean ± SE from 6 independent determinations.
Because fibrinogen did not alter [Ca++]ielevation stimulated by TG or ADP when added after the activation of platelets, we investigated the effect of fibrinogen on the actin filament content of preactivated platelets. A series of experiments was carried out under conditions identical to those used for [Ca++]i measurements. Treatment of human platelets with TG (1 μM) or ADP (5 μM) enhanced F-actin content by 38% ± 7% and 42% ± 6%, respectively. When fibrinogen (1 mg/mL) was added to activated platelets, no significant changes were detected in TG- or ADP-evoked actin polymerization, which remained enhanced over basal levels by 43% ± 7% and 39% ± 2%, respectively (Figure 6C; P > .05; n = 6). These results suggest that actin polymerization is independent of [Ca++]i elevation and might be the target for fibrinogen-mediated modulation of Ca++ signaling.
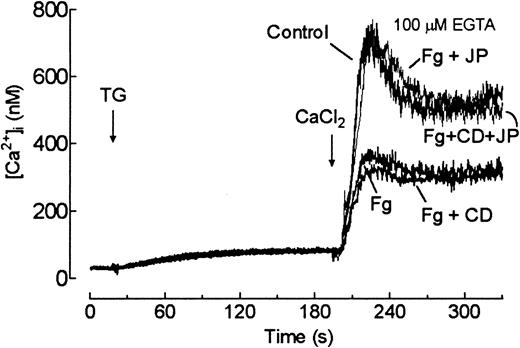
To further investigate the possibility that fibrinogen modulates Ca++ entry by interfering with actin polymerization, we examined the effect of CD and JP on fibrinogen-induced inhibition of SMCE. CD is a widely used inhibitor of actin polymerization,31 whereas JP induces stabilization of the actin filaments.32 We have previously reported that treatment with 10 μM CD for 40 minutes abolishes TG-induced actin polymerization without having any effect on the actin filament content in resting cells.15 Treatment of human platelets with 10 μM JP for 60 seconds had no effect either on the actin filament content of resting platelets or on TG-induced actin polymerization (data not shown). As reported above, the addition of fibrinogen 45 seconds before TG reduced SMCE by 60%. A similar effect was observed when cells were treated with a combination of CD and fibrinogen (58% ± 7%, Figure 7, n = 4). In contrast, the preincubation of human platelets for 60 seconds with 10 μM JP impaired the effect of fibrinogen and, on the basis that the binding affinity of JP for F-actin (Kd = 15 nM)32 is greater than that of CD (Kd = 50 nM),33 also impaired the combined effect of fibrinogen and CD (Figure 7, n = 4). Treatment of platelets for 60 seconds with JP (10 μM) did not alter SMCE (data not shown). These results clearly suggest that fibrinogen modulates SMCE in platelets by a mechanism involving the inhibition of actin polymerization.
Effect of cytoskeletal modifiers on fibrinogen-induced inhibition of store-mediated Ca++ entry.
Fura-2–loaded human platelets were preincubated in the presence of 10 μM CD for 40 minutes, 10 μM JP for 60 seconds, both agents, or the vehicles. Cells were then stimulated in a Ca++-free medium (100 μM EGTA) with ΤG (200 nM) in the absence (Control) or presence of 1 mg/mL fibrinogen (FG, FG + CD, FG + JP, and FG + CD + JP). Three minutes later, CaCl2 (final concentration, 300 μM) was added to the medium to initiate Ca++ entry. Traces shown are representative of 4 independent experiments.
Effect of cytoskeletal modifiers on fibrinogen-induced inhibition of store-mediated Ca++ entry.
Fura-2–loaded human platelets were preincubated in the presence of 10 μM CD for 40 minutes, 10 μM JP for 60 seconds, both agents, or the vehicles. Cells were then stimulated in a Ca++-free medium (100 μM EGTA) with ΤG (200 nM) in the absence (Control) or presence of 1 mg/mL fibrinogen (FG, FG + CD, FG + JP, and FG + CD + JP). Three minutes later, CaCl2 (final concentration, 300 μM) was added to the medium to initiate Ca++ entry. Traces shown are representative of 4 independent experiments.
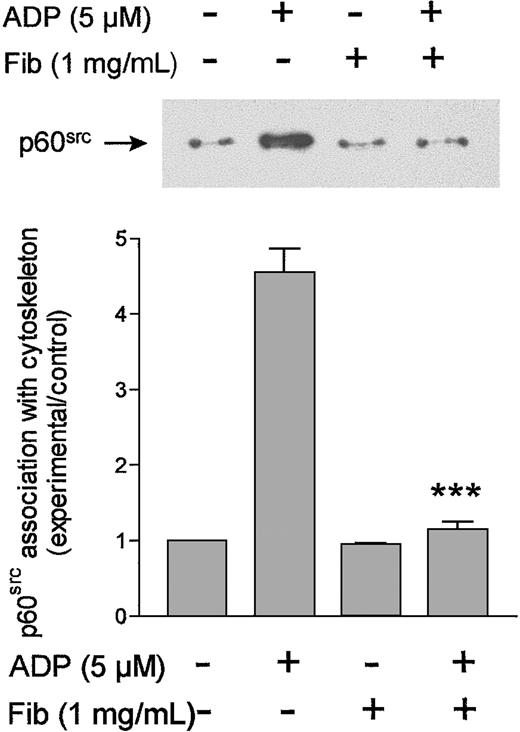
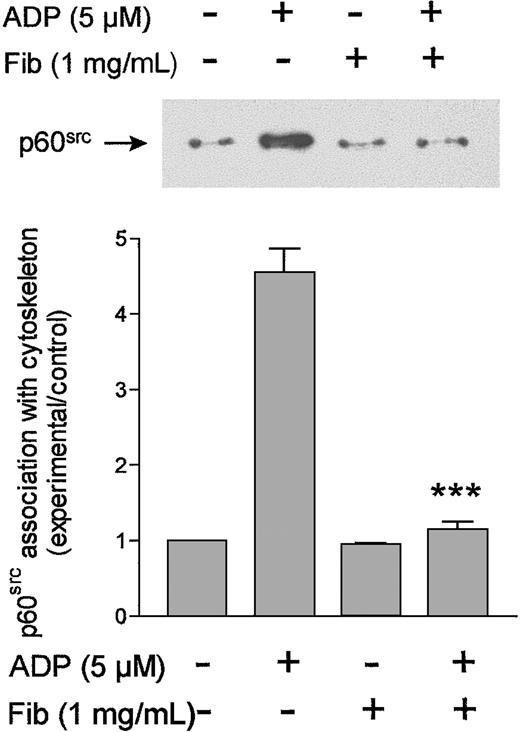
Translocation of p60src to the cytoskeletal fraction in store-depleted platelets
Tyrosine kinases have been shown to be involved in the activation of SMCE in several cell types, including human platelets.34-36 Previous studies have shown that ADP induces association of the tyrosine kinase p60src to the actin cytoskeleton in human platelets,37 an important process for phosphorylation of its substrates during platelet activation.18 To investigate the effect of fibrinogen in the cytoskeletal association of p60src induced by ADP, Western immunoblot analysis was performed on the cytoskeletal fraction of resting and ADP-activated platelets. Platelets heavily loaded with dimethyl BAPTA were used for this study to eliminate the Ca++-dependent association of p60src with the cytoskeleton. When the cytoskeletal fraction was probed for the presence of the protein tyrosine kinase p60src, a small amount of this protein was detected and was associated with the cytoskeleton of resting platelets (Figure8). Treatment of platelets with ADP (5 μM) for 3 minutes enhanced the amount of p60srcassociated with the cytoskeleton by 4.5 ± 0.3-fold (Figure 8). As shown in Figure 8, in the presence of fibrinogen (1 mg/mL), no change was detected in the association of p60src with the cytoskeleton in resting platelets; however, the ADP-evoked response was almost completely abolished (there was only a 1.1 ± 0.1-fold increase over basal levels; P < .001;n = 4).
Fibrinogen inhibits ADP-evoked cytoskeletal association of p60src.
Dimethyl BAPTA-loaded human platelets were stimulated for 3 minutes with no addition or with ADP (5 μg/mL) in the absence or presence of fibrinogen (1 mg/mL) and then lysed with a Triton X-100 buffer and centrifuged to separate the detergent-insoluble fraction. These samples were subjected to SDS–PAGE and analyzed by Western blotting with the specific anti-p60src antibody GD11, as described in “Materials and methods.” Bands were revealed using chemiluminescence and were quantified by scanning densitometry. (Top) Results from a representative experiment. (arrow) Position of p60src. (Bottom) Data are means ± SE of 4 independent experiments and are expressed as -fold increases over the resting levels (experimental/control).
Fibrinogen inhibits ADP-evoked cytoskeletal association of p60src.
Dimethyl BAPTA-loaded human platelets were stimulated for 3 minutes with no addition or with ADP (5 μg/mL) in the absence or presence of fibrinogen (1 mg/mL) and then lysed with a Triton X-100 buffer and centrifuged to separate the detergent-insoluble fraction. These samples were subjected to SDS–PAGE and analyzed by Western blotting with the specific anti-p60src antibody GD11, as described in “Materials and methods.” Bands were revealed using chemiluminescence and were quantified by scanning densitometry. (Top) Results from a representative experiment. (arrow) Position of p60src. (Bottom) Data are means ± SE of 4 independent experiments and are expressed as -fold increases over the resting levels (experimental/control).
Discussion
Integrin αIIbβ3 is a platelet surface receptor for ligands such as fibrinogen, fibronectin, or von Willebrand factor.1,2 Aggregation of circulating platelets requires activation by agonists, converting the integrin αIIbβ3 receptor from a resting to an active conformation, a process termed inside-out signaling, and it depends on fibrinogen binding to the integrin αIIbβ3complex, serving as a link with surrounding platelets.1,5The aggregation mechanism is then amplified and becomes irreversible with the secretion of the platelet intragranular substances. This process has its own mechanisms of control that regulate or modulate platelet activation as the balance between tyrosine kinase and phosphatase activity or through Ca++metabolism.38 When fibrinogen binds to integrin αIIbβ3 on platelets, outside-in signals are raised involving protein phosphorylation, cytoskeletal rearrangement, and molecular translocation events.5 Previous studies have reported the ability of fibrinogen to inhibit several intracellular mechanisms induced by low-intensity stimuli, such as ATP secretion or [Ca++]i elevation.1,2 These earlier reports1 2 are inconsistent about whether occupation of the integrin influences Ca++ store depletion or Ca++ influx. Our findings confirm the inhibitory role of fibrinogen on ADP- or thrombin-induced elevations in [Ca++]i.
In the present study, we demonstrate that the effect of fibrinogen is selectively mediated by the inhibition of Ca++ entry rather than Ca++ release from the intracellular stores. Our studies performed in the absence of external Ca++, in which EGTA (100 μM) was added at the time of experiment to avoid uncoupling of the integrin αIIbβ3, clearly demonstrate that fibrinogen does not modify either the accumulation of Ca++ in the internal pools or the ability of ADP or the SERCA blocker TG to release Ca++ from the internal stores. We confirmed this hypothesis by performing a series of studies with the specific cation channel blocker, SKF96365.24
We found that the effect of fibrinogen was specifically mediated by binding to its receptor, integrin αIIbβ3, because the inhibitory effect was reversed by the previous addition of either RGDS, a peptide containing the carboxy-terminal region of the A-α chain (Arg-Gly-Asp) of the fibrinogen molecule,39 or of abciximab (ReoPro), the Fab fragment of the monoclonal antibody 7E3.40 Further evidence that fibrinogen acts through the integrin αIIbβ3 comes from the finding that fibrinogen was without significant effect on Ca++ responses in platelets from patients homozygous for Glanzmann thrombasthenia, who are deficient in αIIbβ3. It has been observed that RGD peptides and abciximab inhibit the binding of adhesive proteins, such as fibrinogen, to activated platelets with a subsequent inhibition of platelet aggregation.22,39,40 It has been reported that the exposure of platelets to high concentrations of RGD peptides interferes with several cellular processes, such as secretion or [Ca++]ielevations.1,2 Under our conditions we used an optimal concentration of RGDS (100 μM) that reversed the effect of fibrinogen without interfering with intracellular calcium signaling on its own. Because RDGS has been reported to activate integrin αIIbβ3 in platelets,41 our results indicate that the inhibitory effect of fibrinogen is not dependent on affinity modulation of the integrin but on clustering (avidity modulation) of the integrin, with modulation of SMCE occurring through early outside-in signaling events.42 In addition, we have observed that the ability of fibrinogen to inhibit Ca++ entry is not caused by Ca++ channel blockage because it does not alter the entry of Ca++mediated by α,β-methylene ATP, an agonist of the P2x1purinoreceptor that is directly coupled to a nonselective cation channel.25
In human platelets, a major mechanism for Ca++ influx is SMCE, where depletion of the intracellular stores induces Ca++ entry across the plasma membrane. Our results demonstrate for the first time that the occupation of integrin αIIbβ3 by fibrinogen modulates SMCE in platelets. The inhibitory effect of fibrinogen on SMCE was directly examined using TG to deplete the intracellular Ca++ stores in the presence or absence of external Ca++. Store depletion-induced Ca++ entry was reduced in the presence of fibrinogen. Consistent with the results presented above, the effect of fibrinogen was reversed by RGDS, suggesting that the inhibitory effect of fibrinogen is entirely mediated by binding to the integrin αIIbβ3. Interestingly, when fibrinogen was added to preactivated platelets, no changes in [Ca++]i elevations were observed, indicating that fibrinogen inhibits the activation but not the maintenance of SMCE. In addition, these findings strongly support the idea that the effect of fibrinogen is not mediated by Ca++ channel blockage or Ca++ chelation.
Recently, it has been reported that the actin cytoskeleton might play a key role in the activation of SMCE in platelets and other cells.9-11 In human platelets, actin polymerization is also important for the maintenance of SMCE, an observation supporting the conformational coupling model.11 We further investigated the role of the integrin αIIbβ3 in SMCE by testing the effect of fibrinogen on actin polymerization in platelets. In agreement with previous studies,11,15,29 we found that the treatment of platelets with ADP or TG induced actin polymerization, a process not dependent on intracellular Ca++ mobilization as demonstrated by using the intracellular Ca++ chelator dimethyl BAPTA. Our results indicate that in the presence of fibrinogen, ADP- or TG-induced actin polymerization was clearly inhibited, whereas no change was detected when fibrinogen was added to preactivated platelets. In contrast, fibrinogen did not modify the actin filament content of unstimulated platelets, in agreement with previous studies showing that the activation of platelets is a prerequisite to enable integrin αIIbβ3 to bind soluble ligands.5 To further investigate the involvement of the actin cytoskeleton in fibrinogen-induced inhibition of Ca++ entry, we examined the effect of 2 cytoskeletal modifiers (which have opposite effects) on fibrinogen-induced reduction of SMCE. We found that combined treatment with fibrinogen and CD inhibited SMCE to the same extent as fibrinogen alone. In addition, we observed that stabilization of the actin filaments by JP impaired the effect of fibrinogen alone or fibrinogen in combination with CD. These results indicate that fibrinogen specifically exerts its effect by inhibiting actin polymerization. It has recently been reported that the cytoskeleton plays a role in the regulation of the affinity of integrin αIIbβ3 for fibrinogen.43 Thus, the actin cytoskeleton seems to play a pivotal role in the initial stages of platelet activation.
Recent studies have shown that tyrosine kinases of the Src family associate with the platelet cytoskeleton on stimulation with different agonists, a process that has been shown to be independent of platelet aggregation44 and that is important for phosphorylation of their substrates.18 In addition, we have recently found that Ca++ store depletion stimulates translocation of the tyrosine kinase p60src to the actin cytoskeleton,45 a process that might be essential for SMCE activation.46 In the present study, we show that ADP-evoked translocation of p60src is independent of [Ca++]i mobilization, as demonstrated using cells loaded with dimethyl BAPTA, a Ca++ chelator. In addition, we have found that the effect of ADP on p60srctranslocation is blocked in the presence of fibrinogen. In agreement with previous studies44 showing that actin reorganization is required for p60src cytoskeletal association, fibrinogen-induced inhibition of the cytoskeletal association of p60src could be a consequence of its inhibitory role in actin polymerization in human platelets.
In summary, we have shown that fibrinogen binding to the integrin αIIbβ3 inhibits SMCE in human platelets activated by submaximal concentrations of agonists, an action that may be mediated by modulating the reorganization of the actin cytoskeleton and by subsequent translocation of the protein tyrosine kinase p60src to the platelet cytoskeleton. The regulatory role of the integrin αIIbβ3 occurs when fibrinogen is present at the moment of activation but not when fibrinogen is added after platelet activation. The inhibitory effect of the integrin αIIbβ3 on SMCE might be involved in the intrinsic negative feedback that prevents further activation of platelets subjected to low-level stimuli in the circulation. Furthermore, our results indicate platelet aggregation may act as a mechanism that in part suppresses further Ca++influx-dependent activation of platelets incorporated into a thrombus. This inhibition may protect against the adverse effects of high [Ca++]i. Our data imply that platelet-fibrinogen interaction has 2 apparently opposing effects. On the one hand, it is the mechanism by which the hemostatic plug assembles. On the other hand, further platelet activation is down-regulated by fibrinogen binding. This down-regulation is greatly reduced or absent in platelets from patients with Glanzmann thrombasthenia because of reduced interaction with fibrinogen. This compensatory effect may explain the lack of a tendency to bleed severely, observed in many Glanzmann patients.
Supported in part by The Wellcome Trust (grant 046115) and by grants from the Junta de Extremadura, Spain (J.A.R.) and The Dr Saal van Zwanenbergstichting (E.M.Y.M.).
J.A.R. and E.M.Y.M. contributed equally to this work.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Stewart O. Sage, Dept of Physiology, University of Cambridge, Downing St, Cambridge CB2 3EG, United Kingdom; e-mail:sos10@cam.ac.uk.

![Fig. 1. Fibrinogen inhibits ADP-evoked elevations in [Ca++]i. / (A) Fura-2–loaded human platelets suspended in an HBS containing 1 mM Ca++ were stimulated with ADP (5 μM) in the absence (Control) or presence of various concentrations of fibrinogen (FG; 0.1-1 mg/mL). [Ca++]i was monitored as described in “Materials and methods.” (B, C) Human platelets were stimulated with ADP (5 μM) in the absence (Control) or presence of either fibrinogen alone (FG; 1 mg/mL) or fibrinogen (1 mg/mL) in combination with RGDS (100 μM) (FG + RGDS; B) or abciximab (5 μg/mL) (ReoPro; FG + Ab; C). Traces shown are representative of 5 independent experiments.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/97/9/10.1182_blood.v97.9.2648/6/m_h80910986001.jpeg?Expires=1766411749&Signature=b1NQMQh48g3MLOW2gefx7a6D9uASTANxVNFQmKscQU1Bwl5uyOMiKtnigHR1Imsn96u-1VxySbC5i7idYfQj8h~eF3XvAWoYoG8zBTTAYrTFpjZtUYS0kwpJISftMyuzSyrK6zSJh5EOpCo7ZOZ~Tqli7HvMB8rgLSvxncd8lgI8UG5InwrRgdAJczEZvW84LjIVXsZRNBAHXKCza7DBEFmDZTyU8ZDDN6h-Hi15Fq1WstyB34sNcSpRZFyC5i~cA4taDNcmYyVUBUPxVx46BstgXMezbDid7akdlNY0-cc7vISelCPDlSETYzv5umzcoFk03tk0vImqPaH0XwPM7A__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 2. Fibrinogen inhibits thrombin-evoked elevations in [Ca++]i. / (A) Fura-2–loaded human platelets were stimulated with thrombin (0.1 U/mL) in the absence (Control) or presence of either fibrinogen alone (FG; 1 mg/mL) or fibrinogen after the addition of 100 μM RGDS (FG + RGDS). Traces are representative of 7 separate experiments.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/97/9/10.1182_blood.v97.9.2648/6/m_h80910986002.jpeg?Expires=1766411749&Signature=SKCn3sG0KG9O8spmnV3TSpF7qpFTfwlLVHCzb1lIYqVu~VlPJLitqWVzoc9Feb8UDTIRiBVirW5kPUxqI~FmOjkLzgGmHnF6mnMGMFffLlbSE0cQ7~ReqGY8azBLnbHLJt3mGHO24f4zysEBPrAQwgY4J50giuE8yhLk3YmMhbNUwYORrtcgDcR2Z9Wq5VqHHrrcg~07y8fVifaNNdJEChZhNUavIzagggn2NyxLfiRo0EMYpVt9-JusmYDiSXs6cf0LVybrLIhc9YS7a6fjmXi5fc4YWlid0VNY2-ybdCAdG5yGrFuGhTLh5i5KB9527LmuMwWBcYDYJqWaj67PMA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 5. Effect of fibrinogen on the maintenance of Ca++ entry. / (A) Fura-2–loaded human platelets suspended in HBS containing 1 mM Ca++ were stimulated with ADP (5 μM) (Control). Fibrinogen (1 mg/mL) was added 10 seconds later (FG), as shown by the arrow, or 45 seconds before the addition of ADP (FG [control]). (B) Human platelets suspended in HBS containing 1 mM Ca++ were stimulated with TG (200 nM) (Control). The addition of fibrinogen (FG; 1 mg/mL) was made 1½ minutes after the addition of TG, as shown by the arrow. (C) Human platelets were stimulated in a Ca++-free medium (100 μM EGTA) with ΤG (200 nM). Three minutes later, CaCl2 (final concentration, 300 μM) was added to the medium to initiate Ca++ entry (Control). The addition of fibrinogen (FG; 1 mg/mL) or lanthanum chloride (LaCl3; 100 μg/mL) was made 2 minutes after the addition of Ca++, as shown by the arrow. Traces shown are representative of 6 independent experiments.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/97/9/10.1182_blood.v97.9.2648/6/m_h80910986005.jpeg?Expires=1766411749&Signature=paSzTz2QC7Ekrs-kQ6RXL397qYop51dxsg3UqfAmRUog5EtkMoL8N7sC61HSL2C4Xnz157-r3jVq0xnGGddRHXiWFYmlWpdxOmLqax8yRneHMqQJOGGIPzndjk6xU3gDFerCWib0JifMUQxoWzQxvTaqhR1q4Y07xj3BuDBXsXCUi~R9KRC-IHir5GoyGEf-bnvXrB7MDrvUvVbqH3Us0phrHrvnUOPUs2fFzKptODnGqjxIkJDfYYEoYcBS5Rl9y517sKrD5dI5NoBXmjWKfmajGmlGBgtjiN7vhRlVOmW7~5amEaQXw2EIUiqU6YQpbuA80o8ud5z5UxNbi49jFg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)


![Fig. 1. Fibrinogen inhibits ADP-evoked elevations in [Ca++]i. / (A) Fura-2–loaded human platelets suspended in an HBS containing 1 mM Ca++ were stimulated with ADP (5 μM) in the absence (Control) or presence of various concentrations of fibrinogen (FG; 0.1-1 mg/mL). [Ca++]i was monitored as described in “Materials and methods.” (B, C) Human platelets were stimulated with ADP (5 μM) in the absence (Control) or presence of either fibrinogen alone (FG; 1 mg/mL) or fibrinogen (1 mg/mL) in combination with RGDS (100 μM) (FG + RGDS; B) or abciximab (5 μg/mL) (ReoPro; FG + Ab; C). Traces shown are representative of 5 independent experiments.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/97/9/10.1182_blood.v97.9.2648/6/m_h80910986001.jpeg?Expires=1766560046&Signature=LdMx5BtO2byAO59m3xtolP72hyZNFefymxPkn7ZjBboLaQHUVEtlIthd3JHdzcbBy6laM5ZJZ5gFZyddkpvwCdjM2Dt~wKjHLQGPsRCESKqYBz47zmM0zROlWbM4I-4DbhCy5X35RjkmuZlx44GX49o5hqk~T1ukZIGACIHEeZLqW2joWkv4VjpGJpULo5bcrEZdllhlIN9tsR8RdbNE6KgWDWoUa~GH-FOIJCWKmESHFYg86QeuGUP8acGLA57MuGOm51qe7mcgGr7rj4fBhJ3dy5B5wy1UqVMPs3V7zQ53VW7R~rXt4v50Y1xgKVB71P~TvGJHAei4EXQnsnCjxQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 2. Fibrinogen inhibits thrombin-evoked elevations in [Ca++]i. / (A) Fura-2–loaded human platelets were stimulated with thrombin (0.1 U/mL) in the absence (Control) or presence of either fibrinogen alone (FG; 1 mg/mL) or fibrinogen after the addition of 100 μM RGDS (FG + RGDS). Traces are representative of 7 separate experiments.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/97/9/10.1182_blood.v97.9.2648/6/m_h80910986002.jpeg?Expires=1766560046&Signature=zQ3x-ArSkJ3F0WdWgxGKNukj1WjeHasP9FcfvJ4K2x2GZJ-KyQ3fLn9ZLEQF66bc-muo01yrfVK8vjq2rjeXN9iElydmQH-cB4Qc-083uow~2yVtazayxK7bWZ1LOkXRBOGPFr3Xrx4~Hom8m6ffmuIbmeHnCuxJbg66csraNiyGLAxCdXt9Qp950lCKr6QCs1XrfLLdXfCojAxGZe-i6SzoTlkYFq~CekT07LYM-HYm8za4~agbPlZwHBlxMbqNg9xELMq09Mg3B-aAlbLL9gEw-OZ1h7qVGvlLLOSF3KTWvCGMPUDmoeRVWtcNE6N7k~ucC4viU~riqPISM-Zeag__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Fig. 5. Effect of fibrinogen on the maintenance of Ca++ entry. / (A) Fura-2–loaded human platelets suspended in HBS containing 1 mM Ca++ were stimulated with ADP (5 μM) (Control). Fibrinogen (1 mg/mL) was added 10 seconds later (FG), as shown by the arrow, or 45 seconds before the addition of ADP (FG [control]). (B) Human platelets suspended in HBS containing 1 mM Ca++ were stimulated with TG (200 nM) (Control). The addition of fibrinogen (FG; 1 mg/mL) was made 1½ minutes after the addition of TG, as shown by the arrow. (C) Human platelets were stimulated in a Ca++-free medium (100 μM EGTA) with ΤG (200 nM). Three minutes later, CaCl2 (final concentration, 300 μM) was added to the medium to initiate Ca++ entry (Control). The addition of fibrinogen (FG; 1 mg/mL) or lanthanum chloride (LaCl3; 100 μg/mL) was made 2 minutes after the addition of Ca++, as shown by the arrow. Traces shown are representative of 6 independent experiments.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/97/9/10.1182_blood.v97.9.2648/6/m_h80910986005.jpeg?Expires=1766560046&Signature=UK-ir~uawoHyMsVfXYdei2JLQtzF7c9yEBY9RPtA3b~0JuYHS3b-vOlecTePCl0ejGz-1HJnoKbZB5kKtDDlsE35UvUe69DOhig~y-C4H-eeB9WURySIgZvxlD7vksBjz86WCHeqR2RmX5rB~SlsdesVyFHLnSACfP0-TCx0k8-WqXM6WxdeRTpIuWtTVYvm5bNTSxgRcXvDDUkZdOi8Iru62-~HsRGV23lXOQaPtunrNYT~UPSFSfVuDpzyo2dGFVMJpzzciFKlRjSLpjnLCC3mwkExIxb2HGW8IODSIN97Ywa4xlEhcWioFhZ3vEkkkcC56tTiH8Hh4kUv4JVTFw__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)