To modulate alloreactivity after hematopoietic stem cell transplantation, suicide gene–expressing donor T cells can be administered with an allogeneic T-cell–depleted bone marrow graft. Immune competence of such cells is a critical issue. The impact of the ex vivo gene transfer protocol (12-day culture period including CD3/interleukin-2 [IL-2] activation, retroviral-mediated gene transfer, and G418-based selection) on the anti–Epstein-Barr virus (EBV) potential of gene-modified cells has been examined. Cytotoxic (pCTL) and helper (pTh) cell precursor limiting dilution assays, interferon-γ enzyme-linked immunospot, or fluorescence-activated cell sorter analysis after tetrameric HLA-A2/EBV peptide complexes revealed that the frequency of anti-EBV T cells was lower in gene-modified cells (GMCs) than in similarly cultured but untransduced T cells and was even lower than in fresh peripheral blood mononuclear cells, demonstrating both an effect of the culture and of the transduction or selection. The culture-dependent loss of EBV-reactive cells resulted from the preferential induction of activation-induced cell death in tetramer+ cells. Replacing the initial CD3/IL-2 activation by CD3/CD28/IL-2 partially restored the anti-EBV response of GMCs by reducing the initial activation-induced cell death and enhancing the proliferation of EBV-tetramer+cells. Moreover, the G418 selection, and not the transduction, was directly toxic to transduced tetramer+ cells. Replacing the G418 selection by an immunomagnetic selection significantly prevented the selection-dependent loss of EBV-specific cells. Overall, ex vivo gene modification of primary T cells can result in a significant reduction in EBV-reactive T cells through both culture-dependent and selection-dependent mechanisms. Improving immune functions of GMCs through modifications of the cell culture conditions and transduction/selection processes is critical for further clinical studies.
Introduction
Graft versus host (GVH) disease remains a major source of morbidity and mortality after allogeneic hematopoietic stem cell (HSC) transplantation. It results from the recognition by mature immunocompetent donor cells present in the graft of alloantigens expressed by the recipients. GVH disease can be efficiently prevented by T-cell depletion of the graft. However, donor T cells significantly contribute to important therapeutic aspects, such as control of graft rejection, increased graft versus leukemia effect, and antiviral immune responses.1 Thus, the separation of beneficial and harmful properties of donor T cells remains a major goal of allogeneic HSC transplantation.
In this setting, we have developed a new approach aimed at controlling donor T cells by administering, together with a T-cell–depleted bone marrow graft, donor T lymphocytes that have been modified by ex vivo transfer of the herpes simplex thymidine kinase (HS-tk) gene.2 The expression of such a “suicide” gene allows for the gene-modified cells (GMCs) to be sensitive to a prodrug, ganciclovir (GCV). If subsequent GVH disease were to occur, GCV injection should lead to the specific and selective in vivo depletion of donor alloreactive GMCs and leave unaltered the other cells. Thus, one could preserve the beneficial effects of the T cells on engraftment and tumor control early after transplantation and throughout the posttransplantation period for patients not experiencing severe GVH disease. In addition, the GCV-induced selective immunosuppression, restricted to proliferating donor mature GMCs infused with the HSC graft, should result in a weaker toxicity than the broad immunosuppressive agents presently used for GVH disease treatment.
Another major complication of HSC transplantation is the development of Epstein-Barr virus–associated lymphoproliferative disease (EBV-LPD) in the setting of the severe immunosuppressive status of patients receiving transplants and/or of T-cell depletion.3 Donor lymphocyte infusions (DLIs) of T cells remain actually the only efficient treatment of EBV-LPD.4,5 The use of HS-tk–expressing GMCs should also contribute to prevent or treat EBV-LPD when administered together with the HSC graft or when used as donor cells in DLIs.6
We have initiated a phase I/II clinical study aimed at evaluating the toxicity of HS-tk–expressing GMC infusion and the possibility of controlling GVH disease through GCV injection.7 In our first cohort of 12 patients receiving escalating amounts of HS-tk–expressing donor T cells with a bone marrow graft from an HLA-identical sibling, 3 developed an EBV-LPD.8 Although these patients were at high risk for EBV-LPD (recipient age, intensive conditioning regimen, low T-cell dose, use of cyclosporine and, in one patient, a second transplantation following ATG treatment8), an impaired potential of GMCs to control EBV-LPD could not be excluded. Thus, we evaluated the in vitro potential of GMCs, ie, cultured cells that have been transduced and selected, to respond to EBV-infected cells by comparing them with fresh peripheral blood mononuclear cells (PBMCs) or cultured, nontransduced, nonselected control cells. This allowed us, using different technical approaches (limiting dilution assays [LDAs], enzyme-linked immunospot [ELISPOT] assays, and then flow cytometry [FACS] analysis staining with tetrameric HLA-A2/EBV peptide complexes) to determine the impact of the cell culture, transduction, or selection steps on the frequency of anti-EBV cells in GMC products and on their potential to respond to EBV.
Patients, materials, and methods
Donors
Donor-derived EBV-transformed B-cell lines
PBMCs (10 × 106 cells) resuspended in 2.5 mL RPMI 1640 medium (BioWhittaker, Emerainville, France) and supplemented with 10% vol/vol fetal calf serum (Biowest, Nuaillé, France) were incubated with 2.5 mL of supernatant from the B95-8 EBV-producing cell line (ATCC, Manassas, VA) for 2 hours at 37°C. The cells (106/mL) were then cultured in RPMI 1640 plus 10% fetal calf serum in the presence of cyclosporine (0.5 μg/mL; Sandimmune, Novartis, Basel, Switzerland). Establishment of EBV-transformed B-cell (B-EBV) lines was evidenced by the appearance of clumps, usually after 3 weeks of culture. These lines were maintained in RPMI 1640 plus 10% fetal calf serum at a concentration of 0.3 × 106 to 1 × 106 cells per milliliter.
Retroviral vectors
Three amphotropic retroviral vectors were used in this study: the G1Tk1SvNa vector,9 provided by Genetic Therapy (Gaithersburg, MD), and the SFCMM39 and LNSN10vectors, provided by Pr C Bordignon (Milan, Italy). These 3 vectors encode, respectively, the HS-tk and neomycin phosphotransferase II (Neo-R), the HS-tk and truncated NGF receptor (ΔLNGFR), and, lastly, the ΔLNGFR and Neo-R genes, the first gene being downstream of the viral Moloney long terminal repeat promoter and the second one being downstream of the SV40 large T-antigen promoter.
Preparation of gene-modified T cells with the G1Tk1SvNa vector
Generation of gene-modified T cells required a 12-day culture period, as previously described.11 After isolation by centrifugation over Histopaque-1077 and washes, PBMCs were resuspended in culture medium consisting of RPMI 1640 medium (Biowhittaker), 10% vol/vol human serum (EFS Bourgogne/Franche-Comté, Besançon, France), and recombinant human interleukin-2 (IL-2) (Cetus, Rueil Malmaison, France) at a final concentration of 500 IU/mL. Cells were activated by 10 ng/mL soluble CD3 monoclonal antibody (mAb) (OKT3, Jansen-Cilag, Levallois Perret, France) or with CD3 plus CD28 (B-T3, Diaclone, Besançon, France) mAb-coated beads (4 × 106 beads per 106 cells; Dynal, Compiègne, France) and incubated at 37°C, 5% CO2. After a 3-day culture, the cells were counted and transferred for 24 hours into the retroviral vector–containing medium supplemented with IL-2 (1000 IU/mL) and protamin sulfate (5 μg/mL; Sanofi-Winthrop, Gentilly, France). A cell aliquot was cultured in parallel without the retroviral vector. Twenty-four hours after initiation of transduction, cells were centrifuged, resuspended in culture medium, and incubated for 24 hours at 37°C, 5% CO2. From day 5 to day 12, positive selection was performed by culturing the transduced cells in medium containing G418 (800 μg/mL; Sigma). In parallel, an aliquot of transduced cells was cultured without G418 (transduced, nonselected control cells). Nontransduced, selected cells and nontransduced, nonselected cells (Co cells) were cultured in parallel in medium with or without G418, respectively. At the end of selection (day 12), dead cells were removed by centrifugation over Histopaque-1077. Cell viability was assessed by the trypan blue dye exclusion assay. Viable cells were washed twice with phosphate-buffered saline (PBS; Biowhittaker), resuspended in RPMI 1640 medium, 10% vol/vol human serum, and either used immediately for experiments or cryopreserved with 8% vol/vol dimethylsulfoxide (Braun, Boulogne, France) in liquid nitrogen until use.
Preparation of gene-modified T cells with the SFCMM3 vector
Cells were activated by soluble CD3 mAb plus IL-2 and transduced as described above for G1Tk1SvNa vector. However, the G418-based selection was replaced by a positive magnetic-based selection at day 5 as follows: cells were stained with culture supernatant of antihuman NGFR mAb-secreting hybridoma (HB8737, clone 20.4, ATCC) and then incubated with goat anti–mouse immunoglobulin G (H+L) microbeads (Miltenyi Biotec, Bergisch Gladbach, Germany) and positively selected with magnetic-activated cell separation (Miltenyi Biotec), according to the manufacturer's instructions. Selected cells were cultured until day 12 in culture medium with IL-2 (500 IU/mL). Positively selected transduced cells are referred to as “ΔLNGFR+” GMCs.
Preparation of gene-modified T cells transduced with the LNSN vector
CD3 plus IL-2–activated cells were transduced from day 3 to day 5 by coculture with the LNSN packaging cell line. Transduced cells were either selected by G418 (800 μg/mL) from day 7 to day 14 or were sorted by immunomagnetic selection at day 7, as described above for SFCMM3-transduced cells, and then cultured until day 14 in the presence of IL-2 (500 IU/mL) with or without G418.
Quality controls
The sensitivity of GMCs to GCV was assessed as previously described11 and always demonstrated more than 80% inhibition of IL-2–induced proliferation at 1 μg/mL GCV. Transduction efficiency of G1Tk1SvNa-transduced cells, evaluated by quantitative Neo-R gene polymerase chain reaction as previously described,12 was 7.4% ± 1.6% (n = 10) after CD3/IL-2 activation and 11.6% ± 2.0% (n = 5) after activation with CD3/CD28 beads. Transduction efficiencies in SCFMM3- or LNSN-transduced cells, evaluated by indirect staining of transduced cells before magnetic-activated cell separation selection with the antihuman NGFR HB8737 mAb and fluorescein isothiocyanate (FITC)–labeled goat anti–mouse immunoglobulin G (Cappel, ICN Biomedicals, Orsay, France), were 3.6% ± 1.3% (n = 4) and 7.7% ± 2.1% (n = 3), respectively.
Limiting dilution assays
Sensitization of responder cells at day 0.
Responders cells (PBMCs, Co cells, GMCs) from EBV-seropositive or, as negative control, EBV-seronegative donors were plated out in RPMI 1640 medium, 10% vol/vol human serum, at a concentration ranging from 0 to 2 × 105 cells per well (24 replicates per input cell number, final volume 200 μL per well) in round-bottom plates (Sarstedt, Orsay, France) in the presence or absence of 105freshly irradiated (7.5 Gy) stimulator cells (autologous or allogeneic B-EBV cell lines).
Determination of pre–T-helper cell frequencies.
A total of 100 μL of CTLL-2 cell suspension was added to each well of a 96-well round-bottom plate (5 × 103 cells per well) containing 100 μL supernatant harvested on day 3 of the LDAs. Cells were incubated during 24 hours in a humidified 37°C, 5% CO2, incubator. One μCi (37 kBq) tritiated thymidine (3H-TdR, Nen Life, Le Blanc Mesnil, France) was added for the last 8 hours of the assay, and the 3H-TdR incorporation was counted by liquid scintillation. The wells exhibiting helper activity were scored as positive if 3H-TdR incorporation exceeded the average plus 3 SD of control wells (supernatant of LDA culture wells containing no responder cells). Frequency values were estimated at 37% of negative wells using the zero term of the Poisson equation.13 14
Determination of precytotoxic cell frequencies.
A total of 100 μL of supernatant was removed and replaced by RPMI 1640 medium, 10% vol/vol human serum, and IL-2 (20 IU/mL) at days 3, 6, and 9. On day 12, 10 000 51Cr-labeled (10 μCi [370 kBq] 51Cr per 106 cells; Cis Bio International, Saclay, France) target cells (autologous or allogeneic B-EBV) were added to cultured cells. The plates were spun at 2000 rpm for 2 minutes. After a 4-hour incubation at 37°C, 5% CO2, supernatants were harvested and transferred onto Skatron filters and counted in a gamma counter (Wallac 1470 Wizard, Evry, France). The wells exhibiting cytotoxic activity were scored as positive when the chromium release exceeded the mean release plus 3 SD of control wells (LDA culture wells containing no responder cells). Frequency values were estimated at which 37% of the wells were negative using the zero term of the Poisson equation.13 14
ELISPOT assay
The frequency of EBV-specific T cells was also determined with a human interferon-γ (IFN-γ) ELISPOT kit (Diaclone), according to the manufacturer's instructions. Briefly, a 96-well round-bottom plate was coated with a capture anti–IFN-γ antibody, incubated for 1 hour at 37°C, 5% CO2, and then washed 3 times with washing buffer. The plate was saturated with 2% bovine serum albumin (BSA; Sigma)/PBS (Biowhittaker) for 1 hour at 37°C to block nonspecific adsorption and then emptied. A total of 2 × 105responder cells (PBMCs, Co cells, GMCs) were seeded in the absence or presence of irradiated stimulator cells (autologous or allogeneic B-EBV cell lines) at a 2:1 ratio in 200 μL RPMI 1640 medium, 10% vol/vol human serum, and were incubated at 37°C, 5% CO2, for 24 hours. After washing, a biotinylated anti–IFN-γ antibody was incubated for 1 hour at 37°C. After 3 washes, streptavidin–alkaline phosphatase was added for 1 hour at 37°C. The plate was then washed, placed on an ice bath, and 1% agarose solution was added. Individual IFN-γ–producing cells were detected as blue spots and counted. Data are expressed as number of spots per 105 cells, according to the following formula: mean number of spots in stimulated wells − mean number of spots in unstimulated wells. An IL-4 ELISPOT was performed similarly with a human IL-4 ELISPOT kit (Diaclone). To demonstrate that the secretion of IFN-γ or IL-4 was specific of an anti-EBV response, stimulation of cells from EBV-seronegative donors with autologous B-EBV cell lines was used as negative controls.
Tetrameric HLA–peptide complex staining
Production of phycoerythrin (PE)-labeled tetrameric complexes of HLA-A2 proteins folded with the GLCTLVAML peptide (GLC peptide) from the EBV BMLF (BMFL) lytic protein1 has been previously described.15 A total of 5 × 105 to 10 × 105 cells (PBMCs, Co cells, GMCs) were incubated in 0.1% BSA/PBS at room temperature for 30 minutes with PE-labeled tetrameric complex at a 20 μg/mL final concentration and then labeled with PC5-labeled CD8 mAb (Immunotech, Marseille, France) at 4°C for 30 minutes. After 2 washes in 0.1% BSA/PBS, the cells were fixed in PBS containing 1% formaldehyde (Sigma). Samples were analyzed on a FACSCalibur flow cytometer (Becton Dickinson, Le Pont de Claix, France) using CellQuest software. Analysis was gated on CD8+lymphocytes. Cells obtained from HLA-A2 EBV-seronegative donors (PBMCs, Co cells, GMCs) were used as negative control with paired samples from EBV-seropositive donors, as previously described.16 The positivity threshold was set in order to get 0.05% positive cells with negative control samples.
Apoptosis determination
Dioc-6 staining.
A total of 0.1 μM Dioc-6 (Interchim, Montluçon, France) was incubated with 5 × 105 cells at the indicated times during 30 minutes at 37°C, before performing a membrane staining (tetrameric complex and PC5-CD8 mAb), as previously described. After staining, cells were washed in 0.1% BSA/PBS and were immediately analyzed by flow cytometry without being fixed in PBS/formaldehyde.
Annexin V staining.
After performing a membrane staining (tetrameric complex and antibody PC5-CD8), 1 × 106 cells were incubated with 5 μL annexin V–FITC (Immunotech kit, Marseille, France) at 4°C in 500 μL final volume of binding buffer, according to the manufacturer's recommendations. After incubation, the cells were immediately analyzed by flow cytometry without being washed or fixed.
Statistical analysis
Statistical analyses were performed with the SigmaStat software (Jandel Scientific, Erkrath, Germany). Biologic data were compared using the Student t test or Mann-Whitney rank sum test, depending on Gaussian or non-Gaussian distribution of values.
Results
Gene-modified T cells have a reduced frequency of anti-EBV cytotoxic and helper precursors
We first used LDAs, with irradiated autologous B-EBV cell lines as stimulatory cells, to evaluate the frequency of anti-EBV cytotoxic (pCTL) and helper (pTh) cell precursors in GMCs generated from EBV-seropositive individuals. GMCs (transduced and selected cells, cultured during 12 days) were compared with fresh PBMCs and control cells that had been cultured during 12 days but were nontransduced and nonselected (Co cells). As shown in Figure1, the frequencies of pCTL (A,C,E) and pTh (B,D,F) were lower in Co cells than in PBMCs, suggesting that the 12-day cell culture period was sufficient to affect the EBV-reactive cell frequency. Moreover, frequencies of EBV-specific pCTL and pTh were always lower in GMCs than in Co cells, demonstrating that the transduction and/or selection process further reduced the frequency of EBV-reactive cells. Indeed, anti-EBV pCTLs in Co cells were detectable in 6 of 7 experiments but only in 3 of 10 experiments for GMCs (Figure 2A). Similarly, pTh cells in Co cells were detectable in 3 of 3 experiments but in 2 of 4 experiments only for GMCs (Figure 2B). The observation that both pCTL and pTh were reduced suggests that the loss of EBV-reactive cells affected both CD4+ and CD8+T cells. Neither pCTL nor pTh frequencies were detectable when responder cells from the 2 EBV-seronegative donors were stimulated with autologous B-EBV cell lines (data not shown). In some experiments, irradiated allogeneic B-EBV cell lines were used in parallel as positive controls for stimulation. As shown in Figure 2, there was a trend for higher pCTL and pTh frequencies against allogeneic B-EBV cell lines than against autologous B-EBV cell lines. Similarly to the situation with autologous B-EBV cell lines, frequencies of pCTL (Figure 2C) and pTh (Figure 2D) reactive against allogeneic B-EBV cell lines were lower in Co cells than in PBMCs and were always further decreased in GMCs, suggesting that the decreased reactivity was not restricted to EBV-specific cells but also affected alloreactive cells.
Determination of EBV-specific cell frequencies in PBMCs, Co cells, and GMCs by LDAs.
The pCTL (left panels) and pTh (right panels) frequencies as determined by LDAs in PBMCs (A-B), Co cells (C-D), and GMCs (E-F). The indicated responder cells were cultured in the absence (closed circles) or the presence of irradiated autologous (open circles) or allogeneic (closed triangles) B-EBV cell lines during the sensitization phase. For pCTL determination, the target cells were the autologous (circles) or allogeneic (triangles) cell lines used for sensitization. The frequencies are indicated for each culture, in front of their respective regression curve. Data are from one experiment representative of those shown in Figure 2. ND indicates not detectable.
Determination of EBV-specific cell frequencies in PBMCs, Co cells, and GMCs by LDAs.
The pCTL (left panels) and pTh (right panels) frequencies as determined by LDAs in PBMCs (A-B), Co cells (C-D), and GMCs (E-F). The indicated responder cells were cultured in the absence (closed circles) or the presence of irradiated autologous (open circles) or allogeneic (closed triangles) B-EBV cell lines during the sensitization phase. For pCTL determination, the target cells were the autologous (circles) or allogeneic (triangles) cell lines used for sensitization. The frequencies are indicated for each culture, in front of their respective regression curve. Data are from one experiment representative of those shown in Figure 2. ND indicates not detectable.
Reduced frequencies of EBV-specific cells in GMCs, as assessed by LDAs.
Frequencies of pCTL (A,C) and pTh (B,D) in PBMCs, Co cells, and GMCs stimulated by autologous (A-B) or allogeneic (C-D) B-EBV cell lines. Three to 10 independent LDA experiments were performed with the EBV-seropositive donors listed in Table 1; pCTL and pTh were not detectable (< 0.01/105 cells) with PBMCs, Co cells, or GMCs from the EBV-seronegative donor no. 8 (not shown). $ indicatesP < .1 as compared with PBMCs; *, P < .05 as compared with PBMCs; †, P < .05 as compared with Co cells.
Reduced frequencies of EBV-specific cells in GMCs, as assessed by LDAs.
Frequencies of pCTL (A,C) and pTh (B,D) in PBMCs, Co cells, and GMCs stimulated by autologous (A-B) or allogeneic (C-D) B-EBV cell lines. Three to 10 independent LDA experiments were performed with the EBV-seropositive donors listed in Table 1; pCTL and pTh were not detectable (< 0.01/105 cells) with PBMCs, Co cells, or GMCs from the EBV-seronegative donor no. 8 (not shown). $ indicatesP < .1 as compared with PBMCs; *, P < .05 as compared with PBMCs; †, P < .05 as compared with Co cells.
Impaired anti-EBV function is confirmed by IFN-γ ELISPOT assay
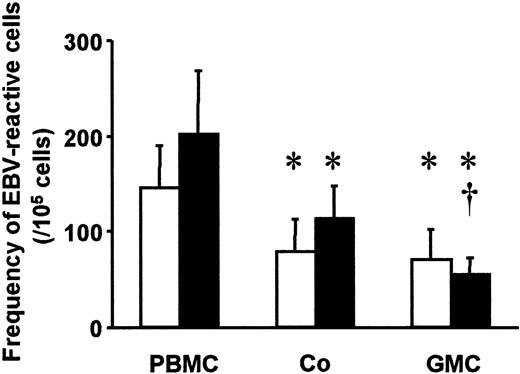
Production of GMCs required a 12-day culture, and the pCTL LDAs required 12 additional culture days. GMCs and Co cells had been cultured for 24 days at the time of the 51Cr release assay, versus only 12 days for PBMCs. The differences of frequency observed in LDAs could therefore be due at least in part to this longer period of culture. Thus, we compared the frequency of EBV-reactive cells in PBMCs, Co cells, and GMCs using an IFN-γ ELISPOT assay, which has the advantage of requiring only one day of culture. No spots were observed in the autologous setting when using cells from the 2 EBV-seronegative donors (data not shown). As reported in Figure3, IFN-γ–secreting cell frequencies in response to autologous B-EBV cell lines were lower in Co cells and in GMCs than in PBMCs. Similar results were obtained when allogeneic B-EBV cell lines were used as stimulators instead of autologous cells (Figure 3).
Reduced frequencies of EBV-specific cells in GMCs, as assessed by ELISPOT assay.
Median frequencies of EBV-reactive cells in PBMCs, Co cells, and GMCs from 6 donors, stimulated by autologous (white bars) or allogeneic (black bars) B-EBV cell lines in 8 independent ELISPOT assays. * indicates P < .05 as compared with PBMCs; †,P < .05 as compared with Co cells.
Reduced frequencies of EBV-specific cells in GMCs, as assessed by ELISPOT assay.
Median frequencies of EBV-reactive cells in PBMCs, Co cells, and GMCs from 6 donors, stimulated by autologous (white bars) or allogeneic (black bars) B-EBV cell lines in 8 independent ELISPOT assays. * indicates P < .05 as compared with PBMCs; †,P < .05 as compared with Co cells.
In 2 experiments, IFN-γ and IL-4 ELISPOT assays were performed in parallel to determine whether the decreased frequency of IFN-γ–secreting cells was compensated by an increased frequency of IL-4–producing cells. No IL-4–producing cells were detected (data not shown), demonstrating that a shift toward type 2 cells was not responsible for the lower frequency of EBV-reactive cells with the IFN-γ ELISPOT assay.
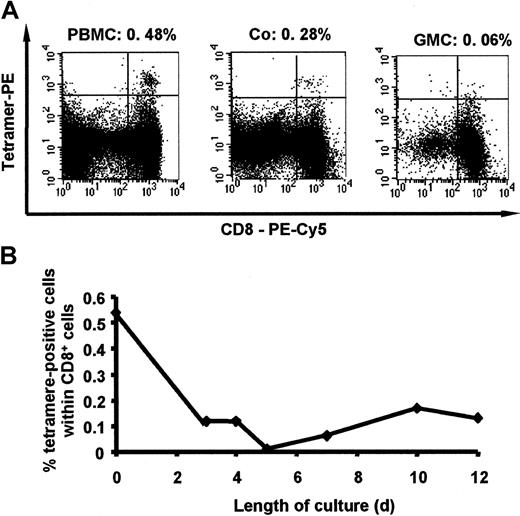
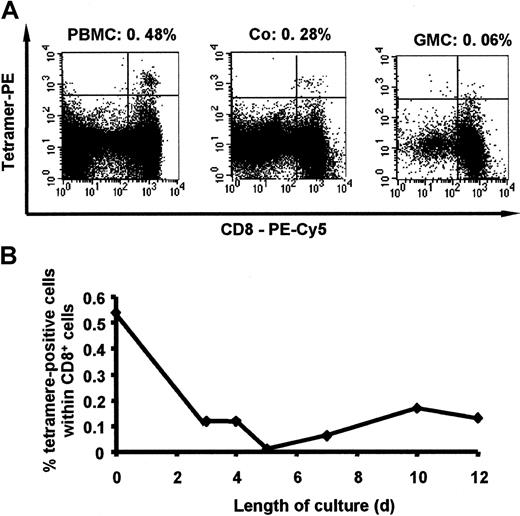
HLA-A2/GLC peptide tetramer staining demonstrates an early loss of EBV-reactive cells during GMC production
LDAs or ELISPOT assays examine T-cell functions. Thus, the frequency of cells expressing EBV-specific T-cell receptors (TCRs) might have been similar within PBMCs, Co cells, and GMCs, while a fraction of EBV-specific cells within Co cells and GMCs could have been anergized and, thus, undetectable in functional assays. The apparent decrease of anti-EBV cell frequency may also have resulted from an induction of activation-induced cell death (AICD) of EBV-reactive cells after B-EBV stimulation during these functional assays. We therefore used a cell phenotype assay based on the staining of EBV-specific T cells with HLA-A2 tetramers complexed with an EBV-derived peptide (GLC) and CD8 mAb. One representative staining is shown in Figure4A. In agreement with Tan et al,16 frequencies of EBV-reactive T cells in PBMCs were higher when using tetramer staining than with an ELISPOT assay and even higher than with LDAs. However, as observed when using LDAs or ELISPOT assays, the percentage of tetramer+ cells within the CD8 lymphocytes was lower in Co cells than in PBMCs and was even lower in GMCs (Figure 4A). These data demonstrate that the decrease of anti-EBV–reactive T-cell frequencies in Co cells and GMCs was due to a loss of anti-EBV cells during the production of GMCs, resulting in part from the 12-day culture (as assessed by the comparison between PBMCs and Co cells) and in part from the transduction and/or selection process itself (as assessed by the comparison between Co cells and GMCs).
Reduced frequencies of EBV-specific cells in GMCs, as assessed by tetramer staining.
(A) Representative FACS profile of PBMCs, Co cells, and GMCs (donor no. 2) after staining with a PE-labeled HLA-A2/GLC tetramer complex and PC5-CD8 mAb. The fraction of tetramer+ cells (upper right quadrant) within the CD8+ cells (upper and lower right quadrants) are indicated above each dot plot. PBMCs, Co cells, and GMCs generated from donor no. 8 (HLA-A2+, EBV-seronegative) were used to set up the positivity level (not shown). Similar profiles were obtained with 3 additional HLA-A2+ EBV-seropositive donors. (B) Kinetics of tetramer staining during cell culture. PBMCs activated by CD3/IL-2 were cultured in the presence of IL-2 until day 12. Data are from 1 of 4 representative experiments.
Reduced frequencies of EBV-specific cells in GMCs, as assessed by tetramer staining.
(A) Representative FACS profile of PBMCs, Co cells, and GMCs (donor no. 2) after staining with a PE-labeled HLA-A2/GLC tetramer complex and PC5-CD8 mAb. The fraction of tetramer+ cells (upper right quadrant) within the CD8+ cells (upper and lower right quadrants) are indicated above each dot plot. PBMCs, Co cells, and GMCs generated from donor no. 8 (HLA-A2+, EBV-seronegative) were used to set up the positivity level (not shown). Similar profiles were obtained with 3 additional HLA-A2+ EBV-seropositive donors. (B) Kinetics of tetramer staining during cell culture. PBMCs activated by CD3/IL-2 were cultured in the presence of IL-2 until day 12. Data are from 1 of 4 representative experiments.
Tetramer staining revealed that the cell loss occurred quickly after CD3/IL-2 activation, because the percentage of tetramer+CD8+ cells was minimal after 24 to 72 hours of culture and remained close to the detection limit by flow cytometry throughout the 12 days of culture (Figure 4B). Similar early reductions of anti-EBV T cells were observed with LDAs and ELISPOT assays (data not shown).
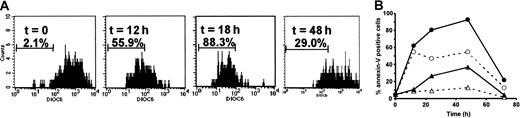
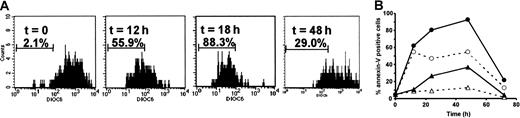
T-cell culture induces rapid early AICD of EBV-reactive cells
Because EBV-reactive T cells are mainly CD45RO+ memory T cells,17 we supposed that EBV-specific T cells present in the PBMC suspension were more sensitive to AICD than non–EBV-specific T cells and that they died preferentially from AICD during the first hours of culture, after CD3/IL-2 activation. Thus, we examined the kinetics of apoptosis from day 0 to day 4 by triple staining with Dioc-6, HLA-A2/GLC peptide tetramer, and PC5-CD8. The percentage of Dioc-6− (apoptotic) cells within CD8+ tetramer+ cells increased quickly after CD3/IL-2 activation (Figure 5A) and decreased at day 2. Additional studies, using annexin V–FITC staining, further confirmed the results obtained with Dioc-6. As shown in Figure5B, the fraction of annexin V+ (apoptotic) cells within tetramer+ CD8+ cells increased after activation, reached a maximum within a similar time frame to that with Dioc-6, ie, between 24 to 48 hours, and decreased thereafter. When CD3/IL-2–stimulated cells were compared with nonstimulated cells, the percentage of annexin V+ cells within tetramer+CD8+ cells was higher in CD3/IL-2–stimulated cultures than in nonstimulated cultures, demonstrating that the observed increase of apoptosis after CD3/IL-2 activation was due to AICD. Moreover, the percentage of apoptosis in the tetramer+ fraction was higher than in the tetramer− fraction of CD8+cells, both in nonactivated and activated cultures, demonstrating that EBV-specific CD8+ cells were more susceptible than other CD8+ cells to spontaneous apoptosis and AICD (Figure 5B). At day 12, less than 15% tetramer+ cells were annexin V+ (data not shown).
Induction of apoptosis in EBV-specific CD8+cells.
(A) PBMCs were activated by CD3/IL-2 and stained with Dioc-6, PE-labeled HLA-A2/GLC tetramer, and PC5-CD8 mAb. The percentage of apoptotic (Dioc-6−) cells, gated on CD8+tetramer+ cells, is indicated for each time of culture. (B) Nonstimulated (dashed lines, open symbols) or CD3/IL-2–activated (full lines, closed symbols) PBMCs were stained at the indicated time with FITC-labeled annexin V, PE-labeled HLA-A2/GLC tetramer, and PC5-CD8 mAb. The percentage of apoptotic (annexin V+) cells are shown in CD8+, tetramer+ (circles) and CD8+, tetramer− (triangles) subsets. Data are from 1 of 4 representative experiments.
Induction of apoptosis in EBV-specific CD8+cells.
(A) PBMCs were activated by CD3/IL-2 and stained with Dioc-6, PE-labeled HLA-A2/GLC tetramer, and PC5-CD8 mAb. The percentage of apoptotic (Dioc-6−) cells, gated on CD8+tetramer+ cells, is indicated for each time of culture. (B) Nonstimulated (dashed lines, open symbols) or CD3/IL-2–activated (full lines, closed symbols) PBMCs were stained at the indicated time with FITC-labeled annexin V, PE-labeled HLA-A2/GLC tetramer, and PC5-CD8 mAb. The percentage of apoptotic (annexin V+) cells are shown in CD8+, tetramer+ (circles) and CD8+, tetramer− (triangles) subsets. Data are from 1 of 4 representative experiments.
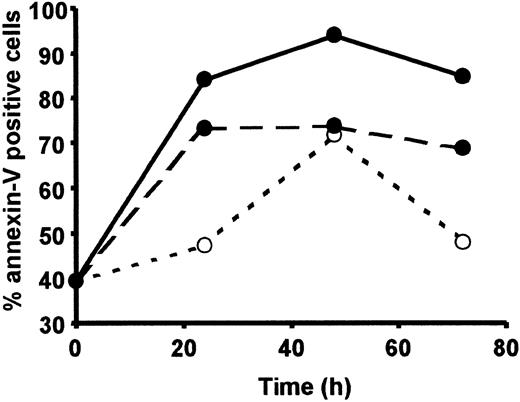
Loss of EBV-reactive cells can be prevented in part by an initial CD3/CD28/IL-2 activation
Our data point to the initial T-cell activation being an important event responsible for the loss of EBV-reactive cells. However, we have previously demonstrated that replacing the initial CD3/IL-2–induced activation by CD3/CD28 mAb-coated beads and IL-2 could prevent the occurrence of TCRBV repertoire alterations.18 Moreover, CD28 costimulation has been shown to reverse CD3 unresponsiveness19 and to exert antiapoptotic effects.20-22 Thus, we tested whether an initial activation by CD3/CD28 beads and IL-2 could limit the loss of EBV-reactive T cells. Induction of AICD after CD3/CD28/IL-2 activation was lower than after CD3/IL-2 activation, as assessed by the lower percentage of annexin V+ cells among tetramer+cells (Figure 6), leading to reduced loss of tetramer+ cells during the first 3 days of culture (Figure 7).
Activation-induced cell death of EBV-specific CD8+ cells after CD3/IL-2 versus CD3/CD28/IL-2 activation.
PBMCs were cultured for 3 days in the absence (dashed line, open symbol) or in the presence of CD3 /IL-2 (full line, closed symbol) or CD3/CD28/IL-2 (dashed line, closed symbol) activation. The percentage of annexin V+ cells is indicated for tetramer+CD8+ cells. Data are from 1 of 3 representative experiments.
Activation-induced cell death of EBV-specific CD8+ cells after CD3/IL-2 versus CD3/CD28/IL-2 activation.
PBMCs were cultured for 3 days in the absence (dashed line, open symbol) or in the presence of CD3 /IL-2 (full line, closed symbol) or CD3/CD28/IL-2 (dashed line, closed symbol) activation. The percentage of annexin V+ cells is indicated for tetramer+CD8+ cells. Data are from 1 of 3 representative experiments.
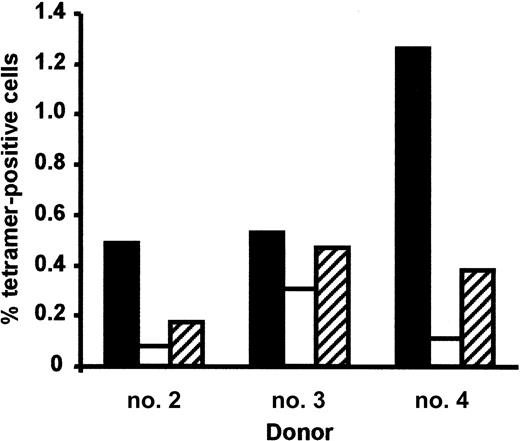
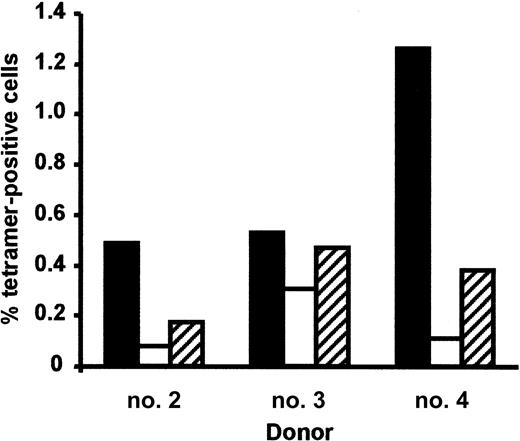
Prevention of EBV-specific CD8+ cell loss by CD28 costimulation after a 3-day culture.
Data are expressed as percentage of tetramer+ cells in CD8+ cells from fresh (black bars) or 3-day–cultured PBMCs after CD3/IL-2 (white bars) or CD3/CD28/IL-2 (hatched bars) activation.
Prevention of EBV-specific CD8+ cell loss by CD28 costimulation after a 3-day culture.
Data are expressed as percentage of tetramer+ cells in CD8+ cells from fresh (black bars) or 3-day–cultured PBMCs after CD3/IL-2 (white bars) or CD3/CD28/IL-2 (hatched bars) activation.
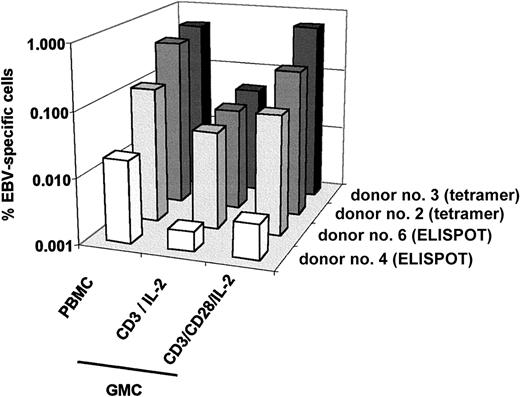
An additional effect of CD3/CD28 beads could be directly related to the proliferation of cells that escaped apoptosis. Thus, we calculated the cell growth of tetramer+ CD8+ T cells after CD3/IL-2 or CD3/CD28/IL-2 activation and compared it with the cell growth of tetramer− CD8+ T cells, within either Co cells or GMCs (Table 2). As expected from previous studies,11 the relative growth of Co cells was higher than for GMCs. In addition, the cell growth was higher for tetramer− CD8+ cells than for tetramer+ CD8+ cells, in GMCs and Co cells, confirming the decrease in the fraction of tetramer+ cell percentage during the culture. Moreover, replacing the initial CD3/IL-2 activation by a CD3/CD28/IL-2 activation improved cell proliferation, as reflected by the increased cell numbers in the latter situation. Interestingly, such improvement was more significant in the tetramer+ subset (1.9- to 8.9-fold increase) than in the tetramer− subset (0.3- to 2.3-fold increase), demonstrating that cell growth of EBV-specific cells was preferentially enhanced after CD3/CD28 activation (Table 2). Thus, we compared the frequency of EBV-reactive cells at day 12 in GMCs generated after CD3/IL-2 (GMCCD3/IL-2) or CD3/CD28/IL-2 activation (GMCCD3/CD28/IL-2). As shown in Figure8, the loss of EBV-specific T cells was partially prevented, as compared with PBMCs, when analyzed by tetramer staining or IFN-γ ELISPOT assay. However, the pCTL frequencies remained undetectable by LDAs both in GMCCD3/IL-2 and in GMCCD3/CD28/IL-2 cells (data not shown). When using beads coated with CD3 mAbs only, instead of CD3 plus CD28 mAbs, the frequency of tetramer+ cells was similar to that observed with soluble CD3 mAbs (data not shown), demonstrating that the beneficial effects of CD3/CD28 beads was due to CD28 mAb and not solely to CD3 mAb immobilization.
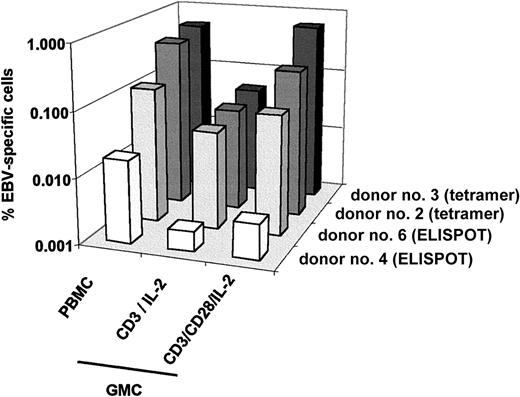
Prevention of EBV-specific CD8+ cell loss by CD28 costimulation after a 12-day culture.
Frequency of EBV-reactive cells from 4 donors, as assessed by HLA-A2/GLC peptide tetramer staining or by ELISPOT assay (after stimulation by an autologous B-EBV cell line), in PBMCs and GMCs generated after an initial PBMC activation by CD3/IL-2 or CD3/CD28/IL-2. Data are representative of 3 tetramer staining experiments and 4 ELISPOT experiments.
Prevention of EBV-specific CD8+ cell loss by CD28 costimulation after a 12-day culture.
Frequency of EBV-reactive cells from 4 donors, as assessed by HLA-A2/GLC peptide tetramer staining or by ELISPOT assay (after stimulation by an autologous B-EBV cell line), in PBMCs and GMCs generated after an initial PBMC activation by CD3/IL-2 or CD3/CD28/IL-2. Data are representative of 3 tetramer staining experiments and 4 ELISPOT experiments.
G418-based selection, and not the transduction per se, further impairs the EBV-reactive cell frequency
As reported above, the frequency of EBV-reactive cells was reproducibly lower in GMCs than in Co cells, demonstrating that, besides an effect of the cell culture itself, an additional effect of transduction and/or selection process accounted for this lower frequency. To further delineate between the effect of transduction and/or selection process on the anti-EBV cell frequency of GMCs, PBMCs were transduced with an HS-tk/ΔLNGFR-coding retroviral vector, SFCMM3, followed by immunomagnetic sorting of ΔLNGFR+GMCs. Both the ΔLNGFR+ and ΔLNGFR−fractions were compared with HS-tk/Neo-R–transduced, G418-selected GMCs and nontransduced Co control cells. As shown in Table3, the percentage of tetramer+ cells was higher in CD8+ΔLNGFR+ GMCs than in Co control cells, suggesting that the transduction per se is not deleterious. This also demonstrates that the expression of HS-tk gene per se is not deleterious to EBV-reactive T cells.
To further explore the mechanism of G418-induced loss of EBV-reactive cells, PBMCs were transduced with a vector coding for both the ΔLNGFR and Neo-R genes (LNSN vector). Transduced cells were either G418 selected or immunomagnetically selected. The ΔLNGFR+sorted cells were then further cultured either in the presence of IL-2 or with IL-2 and G418. As expected from the comparison of G1Tk1SvNa- versus SFCMM3-transduced cells, the percentage of tetramer+cells after LNSN transduction was higher in immunomagnetically selected GMCs than in Co control cells (P = .04), thus demonstrating that a direct, G418-independent effect of Neo-R expression per se can be excluded. Moreover, the G418-selected GMCs had a lower frequency of tetramer+ cells than ΔLNGFR+ GMCs (P = .05), suggesting that the G418-based selection is deleterious to EBV-reactive cells. Furthermore, when ΔLNGFR+ GMCs were cultured in the presence of IL-2 and G418, the percentage of tetramer+ cells was decreased, as compared with ΔLNGFR+ GMCs cultured in the presence of IL-2 but without G418 (P = 0.05; Figure9), further demonstrating that G418 directly affects EBV-reactive GMCs, despite the presence of the Neo-R transgene within GMCs. When T cells were transduced by the SFCMM3 or LNSN vectors, the percentage of tetramer+ cells was higher in the ΔLNGFR+ fraction than in the ΔLNGFR− fraction (P = .03; Table 3 and Figure 9), suggesting that EBV-reactive cells were preferentially transduced. This is further supported by the observation that the frequency of tetramer+ cells within nontransduced Co cells was usually intermediate between those observed in ΔLNGFR+ and ΔLNGFR− cells.
Comparison of G418 versus NGFR-selected GMCs.
Cells transduced with a ΔLNGFR/Neo-R–coding vector were selected at day 8, either by immunomagnetic sorting and were then cultured for 7 days in the presence of IL-2 or IL-2 plus G418, or were selected for 7 days in the presence of IL-2 plus G418.
Comparison of G418 versus NGFR-selected GMCs.
Cells transduced with a ΔLNGFR/Neo-R–coding vector were selected at day 8, either by immunomagnetic sorting and were then cultured for 7 days in the presence of IL-2 or IL-2 plus G418, or were selected for 7 days in the presence of IL-2 plus G418.
Discussion
Administration of donor T cells expressing the HS-tk gene with an HSC transplantation could allow, if GVH disease were to occur, a selective in vivo depletion of these T cells by the use of GCV.2 The administration of low numbers of HS-tk–expressing T cells early following an HLA-identical bone marrow transplantation is associated with no acute toxicity, persistent circulation of the GMCs, and GCV-sensitive GVH disease.8However, during our phase I/II clinical trial of GMC administration, we observed 3 cases of EBV-LPD.8 Although these patients were at high risk for EBV lymphoma (recipient age, intensive conditioning regimen, low T-cell dose, use of cyclosporine and, in one patient, a second transplantation following ATG treatment8) and despite the observation that one patient developed a complete response after delayed infusion of GMCs,8 we examined whether the process for ex vivo retroviral-based gene transfer could be a parameter affecting the antiviral potential of GMCs.
Using 3 different methods (LDAs, ELISPOT assay, and tetramer staining), we demonstrate that the gene transfer process significantly reduces the frequency of EBV-reactive T cells in GMCs as compared with PBMCs and Co cells. We have identified at least 2 critical events responsible for the loss of EBV-reactive cells during GMC production. The first one is a rapid, culture-dependent loss of EBV-specific cells, because Co cells that are activated and cultured for 12 days but are nontransduced and nonselected demonstrate a lower frequency of EBV-reactive cells than PBMCs. Our data demonstrate that the G418-based selection, and not the transduction per se, is the second event responsible for an additional loss of EBV-reactive cells among GMCs with, as a result, a reduced frequency of EBV-reactive T cells in G418-selected GMCs when compared with the Co cells.
Using HLA-A2/GLC peptide tetramer staining of CD8+cells, we show that the ex vivo culture-dependent loss results, at least for CD8+ cells, from a CD3/IL-2 activation-induced cell death. This AICD is preferentially restricted to tetramer+ (EBV-reactive) cells and is observed at a lower level in tetramer− (non–EBV-reactive) CD8+cells. Thus, the AICD results in a clonal deletion of tetramer+ cells, probably because of their memory-activated phenotype, as suggested by data from Janossy et al, who demonstrated that the CD45RO+-primed T cells preferentially die upon activation.23
The initial stimulus seems to be critical for preventing the loss of antigen-specific cells. Because of the known antiapoptotic effect of CD28 costimulation,20-22 we replaced the CD3/IL-2 activation by CD3/CD28 beads and IL-2. Activation with CD3/CD28/IL-2 induced less AICD of EBV-reactive cells than CD3/IL-2 activation and partially prevented the culture-induced cell loss of EBV-reactive cells. These results are in agreement with our observation that alterations of the TCRBV repertoire observed in GMC cultures are prevented by replacing the initial CD3/IL-2 activation by CD3/CD28 beads and IL-2.18 In addition, CD3/CD28/IL-2 activation may preferentially improve the proliferation of tetramer+cells (ie, memory EBV-specific cells24) over the tetramer− cells (which contain cells of both naive and memory phenotype). This is in agreement with data from Sallusto et al,25 which demonstrated that memory cells have higher proliferative responses than naive cells. Another effect of CD3/CD28/IL-2 activation could be an enhancement of EBV-reactive cell transduction efficiency of EBV-reactive cells. Indeed, we and others26 have observed an increased retroviral-mediated T-cell transduction efficiency after CD3/CD28/IL-2 costimulation when compared with CD3/IL-2 activation.
CD3/CD28/IL-2 activation prevents the loss of EBV-reactive cells in GMCs only when using short-term assays (ie, tetramer staining or ELISPOT) and not long-term assays (LDAs). This observation may be explained by the existence of 2 distinct memory T-cell subsets, called effector memory (Tem) and central memory (Tcm) cells.25 Such cells have also been described in persistent EBV infection.24 Although both subsets are detectable with tetramers, only Tem cells, which rapidly secrete IFN-γ upon activation25 (namely, after stimulation with the EBV-derived GLC peptide24) and terminally differentiate into effector cells, should be detectable in ELISPOT assays or LDAs. However, because Tem cells are expected to have a shorter lifespan than Tcm cells, as indicated by shorter telomere length,25 they could be lost during the LDA culture and nondetectable in LDAs despite being detectable in the ELISPOT assay.
The frequencies of EBV-reactive cells are reproducibly lower in GMCs than in Co cells, suggesting that, in addition to early events following T-cell activation, the transduction and/or the selection process may be another parameter responsible for EBV-specific T-cell loss.
Replacing the HS-tk/Neo-R vector (G1Tk1SvNa) by HS-tk/ΔLNGFR (SFCMM3) or ΔLNGFR/Neo-R (LNSN) vectors and performing an immunomagnetic selection of transduced cells allowed prevention of further loss of EBV-reactive cells. This demonstrates that the retroviral transduction is not toxic per se to EBV-reactive cells. On the contrary, these cells are preferentially transduced, as assessed by the observation that the percentage of tetramer+ cells was higher in the ΔLNGFR+ fraction than in the ΔLNGFR− one. Further studies are presently underway to explore how polyclonally stimulated EBV-reactive T cells can be preferentially retrovirally transduced. In addition, neither the HS-tk gene nor the Neo-R gene expression per se are toxic to EBV-reactive cells, because no further loss of EBV-reactive cells is observed with SFCMM3 or LNSN vectors after immunomagnetic selection. Rather, our data point to the G418 selection as a deleterious parameter toward EBV-reactive cells. This is further substantiated by the observation that ΔLNGFR/Neo-R–transduced cells have a high percentage of EBV-reactive cells when immunomagnetically selected (ΔLNGFR selection) but have low levels of EBV-reactive cells when directly selected by G418 or when ΔLNGFR+ cells are further cultured in the presence of G418 after immunomagnetic sorting. This last result clearly indicates that the deleterious effect of G418 selection results from a direct toxic effect of G418 on EBV-reactive transduced cells despite the presence of the Neo-R transgene in these cells. Importantly, non–G418-treated ΔLNGFR+ cells were maintained in IL-2 during 7 days before analysis, thus excluding cell culture per se as a cause for the additional G418-related loss in EBV reactive GMCs. The reasons for such a G418 sensitivity despite the presence of the Neo-R transgene remain unknown and are presently being investigated.
The observation that the reactivity of G1Tk1SvNa-transduced GMCs and Co cells against allogeneic EBV-transformed cell lines was lower than those of PBMCs is reminiscent of our study demonstrating that concanavalin A–activated, 12-day–cultured murine splenocytes exhibited a reduced alloreactivity in vivo, as evidenced by a delayed onset of GVH disease and a reduced GVH disease–related mortality when injected into mice that underwent allogeneic bone marrow transplantation.27 Whether this loss of alloreactivity results from the same mechanisms as those for the loss of EBV-reactive cells remains unknown. This issue needs to be evaluated in both minor and major histocompatibility settings because alloreactive cells are, at least in part, cross-reactive T cells with antiviral specificities, such as anti-HSV and anti-EBV T cells.28-30 Moreover, because most of the graft versus leukemia effect is apparently due to the recognition of leukemic cells by alloreactive cells31 rather than by tumor-specific T cells, the decreased alloreactivity of GMCs suggests that the graft versus leukemia potential of polyclonal gene-modified T cells might also be decreased when compared with fresh cells. Indeed, a lower than expected frequency of response rates in CML has been reported with DLIs using HS-tk–expressing donor T cells.32 In fact, the improvements we suggest in this paper to enhance the anti-EBV response of gene-modified T cells (use of CD3/CD28 costimulation; cell surface marker–based selection process) might also be beneficial for the antitumor potential of suicide gene–expressing T cells. However, further studies will have to confirm this possibility.
In conclusion, we have demonstrated that GMCs have an impaired anti-EBV potential, which may have implications for their ability to control EBV-LPD. The mechanisms involved in this decrease of anti-EBV reactivity involve both culture-dependent phenomena, such as clonal-restricted AICD, and selection-dependent mechanisms. Despite these results, complete response to delayed infusion of GMCs after EBV-LPD has been observed in our study8 and in the study by Bonini et al,6 thus suggesting that anti-EBV reactivity was not completely lost. However, finding ways to prepare GMCs while preserving their immune functions, such as by replacing the initial CD3/IL-2 activation by CD3/CD28/IL-2 activation and preferring a cell surface marker sorting process to Neo-R/G418–based selection, is essential to enhance the therapeutic potential of suicide gene–expressing donor T cells to modulate alloreactivity after HSC transplantation.
Supported by the Programme Hospitalier de Recherche Clinique (PHRC no. 950898), la Ligue Nationale contre le Cancer, l'Association Française contre la Myopathie and the Ministère de l'Enseignement Supérieur et de la Recherche (Centre Réseau de Développement des Thérapies Géniques), l'Association pour la Recherche sur le Cancer (no. 4350), Genetic Therapy, Novartis, and the European Community (Biomed contract no. CT97-2074).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Eric Robinet, Laboratoire de Thérapeutique Immuno-Moléculaire, INSERM E-0119/UPRES EA-2284, Etablissement Français du Sang— Bourgogne/Franche-Comté, 1, Bd Alexander Fleming, 25020 Besançon cedex, France; e-mail:eric.robinet@efs.sante.fr.