Abstract
To draw the cytogenetic profile of childhood and adult acute megakaryoblastic leukemia (M7), the Groupe Français de Cytogénétique Hématologique collected 53 cases of M7 (30 children and 23 adults). Compared to other acute myeloid leukemias, M7 is characterized by a higher incidence of abnormalities, a higher complexity of karyotypes, and a different distribution of abnormalities among children and adults. Nine cytogenetic groups were identified: normal karyotypes (group 1), patients with Down syndrome (group 2), numerical abnormalities only (group 3), t(1;22)(p13;q13) orOTT-MAL transcript (group 4), t(9;22)(q34;q11) (group 5), 3q21q26 (group 6), −5/del(5q) or −7/del(7q) or both (group 7), i(12)(p10) (group 8), and other structural changes (group 9). Groups 1, 2, 3, and 4 were exclusively composed of children (except one adult in group 3), whereas groups 5, 6, 7, and 8 were mainly made up of adults. The main clinical and hematologic features of these groups were described. No new recurrent abnormality was identified, but mapping of all breakpoints allowed us to specify several possible hot spots of rearrangement: 17q22-23, 11q14-21, 21q21-22, and 16q21-22-23. Although 90.5% of cases had no documented antecedent hematologic disorder or exposure to chemotherapy or radiotherapy, the morphologic and the cytogenetic findings indicated that M7 might be a secondary leukemia more often than suggested by preceding history, particularly among adults. The concurrent analyses of morphologic and cytogenetic data also led us to assume that the initial precursor involved might be more immature in adult than in childhood M7.
Introduction
Few large series of acute megakaryoblastic leukemias, M7 according to the French-American-British (FAB) classification,1 have been reported, some having included only children2,3 and others mainly adults.4-6The only study comprising both childhood and adult M7 was that reported by Lu et al who reviewed all cases with documented cytogenetic data published before 1993.7 These previous studies revealed evidence for cytogenetic heterogeneity among cases with acute megakaryoblastic leukemia. In children, at least 2 entities have been recognized, M7 developing in patients with Down syndrome (DS) and M7 associated with t(1;22)(p13;q13) in early infancy. Strong associations have not been found among adults who are characterized by a larger diversity of chromosomal abnormalities including 3q21q26 changes, aberrations of chromosomes 5 and 7, and t(9;22)(q34;q11). However, the distribution of cytogenetic abnormalities in childhood and adult M7 has not been reported to date.
M7, the most frequent type of acute myeloid leukemia (AML) occurring in DS patients, is characterized in these young patients by unique features (for a review, see Lange8). It is often preceded by a transient myeloproliferative phase, is commonly associated with a concurrent involvement of erythroid precursors, and shows a remarkable responsiveness to AML therapy. The occurrence of t(1;22)(p13;q13) is restricted to acute megakaryoblastic leukemia and infancy.9,10 This translocation has seldom been detected in children older than 1 year and occasionally in DS patients.11,12 The genes implicated in 1p13 and 22q13 have recently been identified.13,14 The OTT (RBM15) gene located on 1p13 is fused to the MAL (MLK1) gene on chromosome 22 leading to theOTT-MAL (RBM15-MLK1) fusion gene on the derivative 22. The outcome of these patients is usually poor, but long-term survivors after intensive therapy have been reported.9,10 Other than poor prognosis, no specific features have been associated with M7 occurring in children without DS or t(1;22).3 Likewise, the outcome of adulthood M7 is extremely poor and has been primarily attributable to resistant disease.6 No specific association between outcome and chromosomal abnormalities has been established in this age group.
The aim of our study was to collect a significant number of megakaryoblastic leukemias with successful karyotype, to draw the cytogenetic profile of this rare myeloid malignancy. A morphologic review of all cases recorded was simultaneously undertaken by the Groupe Français d'Hématologie Cellulaire (GFHC) to ensure that megakaryoblasts were the sole or the major component of the malignant proliferation. Therefore, because of strict morphologic and immunophenotyping criteria used to validate an M7 diagnosis, we can expect that our study would reflect the cytogenetic features of megakaryoblastic proliferations among children and adults.
Materials and methods
A retrospective study of M7 leukemias (1988-1999) was carried out by the Groupe Français de Cytogénétique Hématologique (GFCH). The criteria required to include a case were both a successful karyotype reviewed by the GFCH and a validation of the morphologic and immunophenotyping data by the GFHC (chaired by 2 morphologists O.F. and E.D.).
Morphologic and immunophenotypic validation
To be eligible for the study, each patient had to fulfill the following criteria. The blast population had to represent more than 20% of cells in bone marrow aspirate according to the World Health Organization classification,15 and to be myeloperoxidase negative. Immunophenotypes were required when blasts could not be unequivocally classified as megakaryoblasts on morphologic criteria. The recommendations of the European Group for the Immunological Classification of Acute Leukemias (EGIL) were then applied to validate diagnosis, that is, negativity of lymphoid antigens together with either the positivity of 2 megakaryoblastic markers (CD41, CD42, or CD61) or the expression of one megakaryoblastic marker associated with CD36 positivity.16
Cytogenetics
Cytogenetic analysis was performed on bone marrow blasts in 44 cases and on peripheral blood in 9 others. In this multicenter study, different techniques were used. Short cultures (24 and 48 hours) were most frequently carried out (30 and 11 cases, respectively) and half of them were synchronized. Chromosomes were identified with the R-banding technique in 51 patients or G-banding technique in 6. The GFCH respected the usual cytogenetic criteria. A successful karyotype required at least 20 metaphases fully analyzed when karyotype was normal. Clonal abnormalities were identified on either the presence of 2 identical structural changes, or 2 identical extra chromosomes for chromosome gains, or loss of 3 identical chromosomes. Karyotypes were described according to International System for Human Cytogenetic Nomenclature (ISCN) 1995 nomenclature17 and, as a usual practice of the GFCH, were validated by 2 successive workshops, the first “subgroup meeting” for a thorough revision of all metaphases and the second, “central group meeting,” for the final validation.
Fluorescence in situ hybridization studies
Fluorescence in situ hybridization (FISH) analyses were performed with commercially available probes according to the manufacturer's instructions and methods previously described.18 Whole chromosome painting (wcp) was carried out in case 22 with chromosomes 1, 14, and 22 wcp; in case 23 with chromosomes 1 and 22 wcp; in case 42 with chromosomes 4, 5, 7, and 13 wcp; and in case 49 with chromosomes X, 7, and 22 wcp. In case 43, i(12)(p10) was studied using ETV6/TEL 50F4 cosmid concurrently with a centromeric probe of chromosome 12 (D12Z3) and in case 46, t(16;16) was analyzed by painting the short arm of chromosome 16 (Appligene Oncor, Gaithersburg, MD). Case 50 (21q21 breakpoint) was studied with an AML1 probe (LSI TEL-AML1 ES; Vysis, Downers Grove, IL) and cases 48 and 51 (16p12 and 16q21 breakpoints) with aCBFβ probe (LSI CBFB dual color; Vysis).
Reverse transcription–polymerase chain reaction analyses
In patients with a t(16;16)(p13;q22) and a t(16;21)(p11;q22) (cases 45 and 46), the CBFβ-MYH11 and theTLS/FUS-ERG fusion transcripts were studied according to described methods.19,20 Reverse transcription–polymerase chain reaction (RT-PCR) for detection of an OTT-MALtranscript using primers recently described21 was performed in infants without t(1;22) or DS (cases 1, 10, 13) and in one of the variant t(1;22) (case 23).
Statistical analyses
The numbers of patients with a given feature were compared using the χ2 test. Achievement of complete remission (CR) was assessed for the 26 children and the 16 adults who received therapy. Probabilities of event-free survival (EFS) and of survival were evaluated using the log-rank test.22
Results
Patients
This retrospective study included 30 children and 23 adults from 1 Swiss and 15 French centers (see list of participants in “”).
Clinical and hematologic data
A bimodal age distribution was observed with 2 peaks of frequency, M7 occurring in infancy and among the elderly. All children (except one 7-year-old patient) were younger than 3 (median age, 1 year; range, 0-7 years), and 43% of them were infants (< 1 year). Six were congenital leukemias (below 1 month). The median age of adults was 58 years (range, 19-79 years).
In 90.5% of patients, M7 was diagnosed as a de novo leukemia. In 3 adults, M7 occurred after a hematologic disorder: one chronic myeloid leukemia (case 24), one myelodysplastic syndrome (case 36), and one essential thrombocytemia (case 27); this latter patient also received hydroxyurea for several years. M7 might be secondary to a previous toxic exposure in 2 further cases: a patient with lymphoma treated with an intensive chemotherapy regimen (case 32), and a patient with breast cancer who underwent radiotherapy (case 34).
Hepatosplenomegaly was mostly found in children; splenomegaly was present in 70% of children and 26% of adults, whereas hepatomegaly was observed in 60% and 35%, respectively. Lymph node enlargement was rare in children (11%) and never observed in adults. Periostosis contributed to clinical diagnosis in 4 children. Other sites of disease included mediastinal mass (the 2 adults of group 8), kidney involvement (2 infants), chloroma (1 infant), and central nervous system (1 infant).
Children were treated according to either the European Organization for Research and Treatment of Cancer–Children Leukemia Cooperative Study Group 58872 (EORTC-CLCG58872)23 or the Leucémie Aigue Myéloblastique de l'Enfant 89/91 (LAME89/91) trials,24 except patients with DS who received low-dose cytarabine in 6 of 7 cases (the patient with congenital disease died at birth). The Bordeaux Grenoble Marseille Toulouse (BGMT87), BGMT91, or BGMT95 protocols25 were administered to the 16 adult patients who completed therapy. Children fared better than adults, achieving CR more easily (CR: 77% in children versus 33% in adults; P < .01) and having longer survivals (3-year survival probability, 36%; 95% CI, 20-56; median survival, 16 months) than adults (3-year survival probability, 0%; 95% CI, 2-24; median survival, 4 months; P < .01). All adults had a poor outcome, whereas among children, outcome differed according to karyotype. The longest survivals were observed in patients with DS (3-year EFS, 57%; 95% CI, 20-88; 3-year survival, 71%; 95% CI, 30-95). Patients with t(1;22) either died within a few days (before starting therapy in 3 cases) or were good responders to intensive therapies (chemotherapy alone or associated with allogeneic bone marrow transplantation [BMT] or autologous BMT). Their 3-year EFS probability was 50% (95% CI, 20-80). Outcome was poor in all children without DS or t(1;22) (3-year EFS, 8%; 95% CI: 0-38).
Peripheral white blood cell (WBC) counts were more elevated in children (median WBC count, 14.4 × 109/L) than in adults (median WBC count, 4.6 × 109/L; P < .05), whereas hemoglobin and platelet counts were low in both age groups. Bone marrow biopsy showed reticulin myelofibrosis in 9 of 13 documented cases.
The GFHC classified M7 into 3 morphologic categories according to the degree of maturation displayed by blasts. In the first category, megakaryocytic lineage involvement was unequivocally evoked by morphologic features of the nuclei and cytoplasm. Category 1 was then subdivided into 2 subgroups (1A and 1B) according to blast size, chromatin density, and cytoplasm abundance and shape. Category 2 was characterized by coexistence of blasts with typical megakaryocytic attributes (as in category 1) with a population of undifferentiated blasts. Category 3 was composed solely of morphologically undifferentiated blasts. In all cases, the presence of abnormal megakaryocytic maturation, mainly characterized by the presence of micromegakaryocytes, was also assessed. Micromegakaryocytes, quoted as “m” in the morphologic classification were only observed in categories 1 and 2 (Table1).
Age, sex, morphologic classification, survival, and karyotype of the 53 patients
| Cases . | Morphologic categories . | Age* . | Sex . | Survival (mo) . | Karyotype . | |
|---|---|---|---|---|---|---|
| y . | mo . | |||||
| Group 1: Normal karyotypes | ||||||
| 1 | 1 A | 8 | M | 7 | 46,XY[40] | |
| Group 2: Down syndrome | ||||||
| 2 | 2 m | 1 | M | 0.1 | 47,XY,+ 21c[30] | |
| 3 | 2 | 2 | F | 57† | 47,XX,der(15;21)(q10;q10),+ 21c[15] | |
| 4 | 1 B | 2 | F | 67† | 47,XX,add(13)(q33),+ 21c[10]/47,XX,+ 21c[9] | |
| 5 | 2 | 3 | F | 65† | 50,XX,t(1;21)(q31.3;q21.1)c,+ 11,+ 14,+ 21c,+ der(21)t(1;21)[19]/47,XX,t(1;21)(q31.3;q21.1)c,+ 21c[1] | |
| 6 | 2 m | 16 | F | 46† | 51,XY,+ 14,+ 19,+ 21c,+ 21,+ 22[10] | |
| 7 | 1 B | 2 | M | 98† | 46,XY,del(6)(q21q25),− 7,+ 21c[10]/47,XY,+ 21c[3] | |
| 8 | 1 A | 17 | M | 21 | 44,XY,t(9;15)(p11;q11),dup(11)(q11q13),− 13,− 15,− 16,der(17)t(16;17)(q11;p11),+ 21c,der(21)t(13;21) (q21;p11)[9]/46,XY[18] | |
| Group 3: Numerical abnormalities | ||||||
| 9 | 1 B | 2 | F | 24 | 47,XX,+ 3[4]/46,XX[21] | |
| 10 | 1 B m | 1 | M | 0.1 | 47,XY,+ 21[30]/94,idem x 2[3] | |
| 11 | 1 B | 18 | M | 8 | 48,XY,+ 8,+ 21[17]/46,XY[3] | |
| 12 | 2 m | 68 | M | 0.1 | 49,XY,+ 8,+ 12,+ 19[11]/49,XY,+ 9,+ 12,+ 13[5]/46,XY[34] | |
| Group 4: t(1;22)(p13;q13) or OTT-MAL transcript | ||||||
| 13 | 1 B m | 3 | M | 71† | 46,XY[27]/OTT-MAL fusion transcript positive | |
| 14 | 1 B m | 1 | M | 0.6 | 46,XY,t(1;22)(p13;q13)[4]/46,XY[24] | |
| 15 | 2 m | 1 | F | 0.8 | 46,XX,t(1;22)(p13;q13)[16]/46,XX[1] | |
| 16 | 2 m | 1 | F | 1.4 | 46,XX,t(1;22)(p13;q13)[9]/46,XX[15] | |
| 17 | 2 m | 2 | F | 29† | 46,XX,t(1;22)(p13;q13)[14]/46,XX[13] | |
| 18 | 1 B m | 6 | F | 33† | 46,XX,t(1;22)(p13;q13)[22] | |
| 19 | 1 A m | 1 | F | 68† | 46,XX,t(1;22)(p13;q13)[5]/46,XX[16] | |
| 20 | 2 m | 3 | F | 3 | 46,XX,t(1;22)(p13;q13)[1]/46,idem,del(11)(q22q24)[1]/46,idem,del(11)(q22q24),del(17)(q22)[15]/46,XX[28] | |
| 21 | 2 m | 21 | M | 59† | ‡54,XY,t(1;22)(p13;q13),+ der(1)t(1;22),+ 2,+ 4,+ 6,+ 9,+ 10,+ 19,+ 21[11]/46,XY[16] | |
| 22 | 1 B m | 2 | F | 0.1 | 46,XX,t(1;22;14)(p13;q13;q31)[25] | |
| 23 | 2 m | 9 | M | 23† | ‡46,XY,t(1;22;4)(p13;q13;q35)[9]/46,XY[60] | |
| Group 5: t(9;22)(q34;q11) | ||||||
| 24 | 1 A m | 57 | M | 0.8 | 46,XY,t(9;22)(q34;q11)[8]/45,idem,− 7,der(17)t(7;17)(q22;q23)[16]/46,XY[1] | |
| 25 | 2 m | 72 | F | 27 | 46,XX,t(9;22)(q34;q11)[12]/〈4n〉92,XXXX,t(9;22)x2[10]/〈8n〉184,XXXXXXXX,t(9;22)x4[4] | |
| 26 | 1 B | 51 | F | 27 | 46,XX,t(9;22)(q34;q11)[25] | |
| Group 6: 3q21q26 changes | ||||||
| 27 | 3 | 67 | F | 6.9 | 46,XX,t(3;12)(q26;p13)[20] | |
| 28 | 1 B | 44 | F | 1.9 | ‡46,XX,inv(3)(q21q26)[4]/46,idem,t(9;22)(q34;q11)[15] | |
| 29 | 1 A m | 26 | M | 6.3 | 46,XY,inv(3)(q21q26),t(4;19)(p16;?),del(5)(q23q34)[1]/45,XY,inv(3)(q21q26),del(5)(q23q34),dic(11;17) (p14;p13)[20] | |
| 30 | 1 A m | 12 | M | 21.1 | 47,XY,del(3)(q21q25-26),+ del(6)(q12q21),t(11;17)(p15;q23)[14]/46,XY[8] | |
| 31 | 1 A | 2 | M | 23 | 46,XY,add(2)(q37),ins(3;?)(q21;?),del(5)(q13q33),− 7,− 9,add(16)(q23),+ min,+ mar[18]/46,idem,add (11)(q23)[2] | |
| 32 | 1 A | 58 | M | 2 | 46,XY,− 3,− 5,del(7)(q21q23),der(20)t(3;20)(q21;q12),+ 21,+ 22[2]/88,XYY,− X,+ Y,− 4,− 5,− 5,+ 6, − 7,+ 8,− 9,− 9,del(12)(p12),+ 13,− 14,− 16,− 17,− 18,+ 19,+ 19,der(20)t(3;20)(q21;q12)x2,+ 21, + 21[18] | |
| Group 7: − 5/del(5q) − 7/del(7q) | ||||||
| 33 | 3 | 69 | M | 38 | 46,XY,− 7,+ der(1;7)(q10;p10)[22]/46,XY[3] | |
| 34 | 1 B m | 71 | F | 4.3 | 45,XX,− 1,− 7,+ der(1;7)(q10;p10),del(5)(q15q34),der(6)t(6;13)(p22;q14),− 13,+ mar[12] | |
| 35 | 3 | 68 | F | 9.5 | 46,XX,del(7)(q31q35)[10]/92,idemx2[3]/46,XX[10] | |
| 36 | 1 B m | 70 | F | 14 | 46,XX,del(5)(q23q33)[15] | |
| 37 | 1 B m | 78 | M | 3 | 46,XY,del(5)(q22q34),t(14;21)(q24;q22)[5]/46,XY[15] | |
| 38 | 2 | 25 | M | 14 | 48,XY,dic(1;15)(p11;p11)x2,t(2;7)(p16;p14),del(5)(q21q34),+ 8,− 11,− 19,+ 22[21]/46,XY[2] | |
| 39 | 1 B m | 67 | M | 1.7 | 48,XY,− 3,inv(4)(p15.3q11),del(5)(q21q34),− 7,− 14,add(17)(p11),+ mar1,+ mar2x2,+ mar3x2[18]/48, idem,der(Y)t(Y;?)(q12;?)[5] | |
| 40 | 1 A m | 79 | F | 4.4 | 48,XX,− 5,?der(7)t(7;9)(q11;q13),add(9)(q33),− 17,add(19)(p13),+ 20,+ 4mar[3]/46,XX[20] | |
| 41 | 3 | 57 | M | 5.7 | 45,XY,t(1;9;2)(q21;q13-21;q36),del(5)(q13q34),i(7)(q10),+ der(7)t(7;17)(q11;q11),+ 8,− 11,− 13,− 16, − 17,r(?;?11)[11]/54-60,idem,+ der(1)t(1;9;2),+ 6,+ 11,+ 16,+ 19,+ 20,+ 21,− ring,+ mar[7]/81-89,idemx2[5] | |
| 42 | 1 A | 47 | F | 0.6 | 45,XX,der(4)(4p16→4q21::5::?::7::13),del(5)(q12),der(7)t(7;4)(q21;q23),der(7)t(?;7)(?;q10),− 13,− 16, del(17)(p11),− 21,− 22[18] | |
| Group 8: i(12)(p10) | ||||||
| 43 | 2 m | 23 | M | 1.2 | 60-64〈3n〉,XX,− Y,− 2,− 4,− 5,del(6)(q21q24),add(6)(p22-25),del(7)(q32q35),− 8,− 9,der(11)t(4;11) (q28;q22),i(12)(p10)x2,der(13)t(8;13)(q13;p11),− 15,− 16,− 18,− 21,+ 4mar[19]/46,XY[2] | |
| 44 | 1 A m | 19 | M | 4.6 | 71-76〈3n〉,XYY,+ add(1)(q11),+ add(1)(q23),i(2)(q10),add(3)(p12),− 4,+ add(8)(p12),− 9,+ der(10) i(10)(q10)t(5;10)(q11;q26),− 11,i(12)(p10),− 13,− 17,+ 19x2,+ 20,+ 21,+ mar[7]/72-76,XYY,+ 1, der(1;2)(p10;q10),add(3)(p12),− 4,+ 8,− 9,+ der(10),− 11,i(12)(p10),− 13,+ 19,+ 21x2,+ mar[4] | |
| Group 9: Other structural changes | ||||||
| 45 | 2 m | 41 | M | 13 | 46,XY,t(16;21)(p11;q22)[20] | |
| 46 | 3 | 33 | M | 53 | ‡46,XY,t(16;16)(p13;q22)[13]/46,idem,del(7)(q33q36)[3]/46,XY[4] | |
| 47 | 1 A | 2 | F | 15 | 46,XX,del(13)(q13q32)[17]/46,XX[11] | |
| 48 | 1 A | 13 | M | 14 | 46,t(X;16)(q28;p12),Y[2]/46,XY[16] | |
| 49 | 1 A m | 7 | F | 13 | 46,X,add(X)(q12),der(7)t(X;7)(q12;p13),add(22)(q12)[3]/46,idem,del(6)(q21q26)[2]/46,XX[4] | |
| 50 | 1 A | 22 | F | 5.3 | 46,XX,del(9)(p21)[1]/46,X,t(X;21)(q24;q21),del(9)(p21),+ 19[19] | |
| 51 | 1 A | 12 | F | 10 | 47,XX,t(5;17)(p13;q22),t(16;17)(q21;q22),+ 19[14]/46,XX[6] | |
| 52 | 2 m | 2 | M | 21.5 | 46,XY,t(11;21)(q14;q22),del(22)(q13)[25]/46,XY[1] | |
| 53 | 3 | 66 | F | 0.1 | 47,XX,+ 5,del(6)(q15-16q26),add(11)(q22),− 22,+ mar[14]/46,XX[2] | |
| Cases . | Morphologic categories . | Age* . | Sex . | Survival (mo) . | Karyotype . | |
|---|---|---|---|---|---|---|
| y . | mo . | |||||
| Group 1: Normal karyotypes | ||||||
| 1 | 1 A | 8 | M | 7 | 46,XY[40] | |
| Group 2: Down syndrome | ||||||
| 2 | 2 m | 1 | M | 0.1 | 47,XY,+ 21c[30] | |
| 3 | 2 | 2 | F | 57† | 47,XX,der(15;21)(q10;q10),+ 21c[15] | |
| 4 | 1 B | 2 | F | 67† | 47,XX,add(13)(q33),+ 21c[10]/47,XX,+ 21c[9] | |
| 5 | 2 | 3 | F | 65† | 50,XX,t(1;21)(q31.3;q21.1)c,+ 11,+ 14,+ 21c,+ der(21)t(1;21)[19]/47,XX,t(1;21)(q31.3;q21.1)c,+ 21c[1] | |
| 6 | 2 m | 16 | F | 46† | 51,XY,+ 14,+ 19,+ 21c,+ 21,+ 22[10] | |
| 7 | 1 B | 2 | M | 98† | 46,XY,del(6)(q21q25),− 7,+ 21c[10]/47,XY,+ 21c[3] | |
| 8 | 1 A | 17 | M | 21 | 44,XY,t(9;15)(p11;q11),dup(11)(q11q13),− 13,− 15,− 16,der(17)t(16;17)(q11;p11),+ 21c,der(21)t(13;21) (q21;p11)[9]/46,XY[18] | |
| Group 3: Numerical abnormalities | ||||||
| 9 | 1 B | 2 | F | 24 | 47,XX,+ 3[4]/46,XX[21] | |
| 10 | 1 B m | 1 | M | 0.1 | 47,XY,+ 21[30]/94,idem x 2[3] | |
| 11 | 1 B | 18 | M | 8 | 48,XY,+ 8,+ 21[17]/46,XY[3] | |
| 12 | 2 m | 68 | M | 0.1 | 49,XY,+ 8,+ 12,+ 19[11]/49,XY,+ 9,+ 12,+ 13[5]/46,XY[34] | |
| Group 4: t(1;22)(p13;q13) or OTT-MAL transcript | ||||||
| 13 | 1 B m | 3 | M | 71† | 46,XY[27]/OTT-MAL fusion transcript positive | |
| 14 | 1 B m | 1 | M | 0.6 | 46,XY,t(1;22)(p13;q13)[4]/46,XY[24] | |
| 15 | 2 m | 1 | F | 0.8 | 46,XX,t(1;22)(p13;q13)[16]/46,XX[1] | |
| 16 | 2 m | 1 | F | 1.4 | 46,XX,t(1;22)(p13;q13)[9]/46,XX[15] | |
| 17 | 2 m | 2 | F | 29† | 46,XX,t(1;22)(p13;q13)[14]/46,XX[13] | |
| 18 | 1 B m | 6 | F | 33† | 46,XX,t(1;22)(p13;q13)[22] | |
| 19 | 1 A m | 1 | F | 68† | 46,XX,t(1;22)(p13;q13)[5]/46,XX[16] | |
| 20 | 2 m | 3 | F | 3 | 46,XX,t(1;22)(p13;q13)[1]/46,idem,del(11)(q22q24)[1]/46,idem,del(11)(q22q24),del(17)(q22)[15]/46,XX[28] | |
| 21 | 2 m | 21 | M | 59† | ‡54,XY,t(1;22)(p13;q13),+ der(1)t(1;22),+ 2,+ 4,+ 6,+ 9,+ 10,+ 19,+ 21[11]/46,XY[16] | |
| 22 | 1 B m | 2 | F | 0.1 | 46,XX,t(1;22;14)(p13;q13;q31)[25] | |
| 23 | 2 m | 9 | M | 23† | ‡46,XY,t(1;22;4)(p13;q13;q35)[9]/46,XY[60] | |
| Group 5: t(9;22)(q34;q11) | ||||||
| 24 | 1 A m | 57 | M | 0.8 | 46,XY,t(9;22)(q34;q11)[8]/45,idem,− 7,der(17)t(7;17)(q22;q23)[16]/46,XY[1] | |
| 25 | 2 m | 72 | F | 27 | 46,XX,t(9;22)(q34;q11)[12]/〈4n〉92,XXXX,t(9;22)x2[10]/〈8n〉184,XXXXXXXX,t(9;22)x4[4] | |
| 26 | 1 B | 51 | F | 27 | 46,XX,t(9;22)(q34;q11)[25] | |
| Group 6: 3q21q26 changes | ||||||
| 27 | 3 | 67 | F | 6.9 | 46,XX,t(3;12)(q26;p13)[20] | |
| 28 | 1 B | 44 | F | 1.9 | ‡46,XX,inv(3)(q21q26)[4]/46,idem,t(9;22)(q34;q11)[15] | |
| 29 | 1 A m | 26 | M | 6.3 | 46,XY,inv(3)(q21q26),t(4;19)(p16;?),del(5)(q23q34)[1]/45,XY,inv(3)(q21q26),del(5)(q23q34),dic(11;17) (p14;p13)[20] | |
| 30 | 1 A m | 12 | M | 21.1 | 47,XY,del(3)(q21q25-26),+ del(6)(q12q21),t(11;17)(p15;q23)[14]/46,XY[8] | |
| 31 | 1 A | 2 | M | 23 | 46,XY,add(2)(q37),ins(3;?)(q21;?),del(5)(q13q33),− 7,− 9,add(16)(q23),+ min,+ mar[18]/46,idem,add (11)(q23)[2] | |
| 32 | 1 A | 58 | M | 2 | 46,XY,− 3,− 5,del(7)(q21q23),der(20)t(3;20)(q21;q12),+ 21,+ 22[2]/88,XYY,− X,+ Y,− 4,− 5,− 5,+ 6, − 7,+ 8,− 9,− 9,del(12)(p12),+ 13,− 14,− 16,− 17,− 18,+ 19,+ 19,der(20)t(3;20)(q21;q12)x2,+ 21, + 21[18] | |
| Group 7: − 5/del(5q) − 7/del(7q) | ||||||
| 33 | 3 | 69 | M | 38 | 46,XY,− 7,+ der(1;7)(q10;p10)[22]/46,XY[3] | |
| 34 | 1 B m | 71 | F | 4.3 | 45,XX,− 1,− 7,+ der(1;7)(q10;p10),del(5)(q15q34),der(6)t(6;13)(p22;q14),− 13,+ mar[12] | |
| 35 | 3 | 68 | F | 9.5 | 46,XX,del(7)(q31q35)[10]/92,idemx2[3]/46,XX[10] | |
| 36 | 1 B m | 70 | F | 14 | 46,XX,del(5)(q23q33)[15] | |
| 37 | 1 B m | 78 | M | 3 | 46,XY,del(5)(q22q34),t(14;21)(q24;q22)[5]/46,XY[15] | |
| 38 | 2 | 25 | M | 14 | 48,XY,dic(1;15)(p11;p11)x2,t(2;7)(p16;p14),del(5)(q21q34),+ 8,− 11,− 19,+ 22[21]/46,XY[2] | |
| 39 | 1 B m | 67 | M | 1.7 | 48,XY,− 3,inv(4)(p15.3q11),del(5)(q21q34),− 7,− 14,add(17)(p11),+ mar1,+ mar2x2,+ mar3x2[18]/48, idem,der(Y)t(Y;?)(q12;?)[5] | |
| 40 | 1 A m | 79 | F | 4.4 | 48,XX,− 5,?der(7)t(7;9)(q11;q13),add(9)(q33),− 17,add(19)(p13),+ 20,+ 4mar[3]/46,XX[20] | |
| 41 | 3 | 57 | M | 5.7 | 45,XY,t(1;9;2)(q21;q13-21;q36),del(5)(q13q34),i(7)(q10),+ der(7)t(7;17)(q11;q11),+ 8,− 11,− 13,− 16, − 17,r(?;?11)[11]/54-60,idem,+ der(1)t(1;9;2),+ 6,+ 11,+ 16,+ 19,+ 20,+ 21,− ring,+ mar[7]/81-89,idemx2[5] | |
| 42 | 1 A | 47 | F | 0.6 | 45,XX,der(4)(4p16→4q21::5::?::7::13),del(5)(q12),der(7)t(7;4)(q21;q23),der(7)t(?;7)(?;q10),− 13,− 16, del(17)(p11),− 21,− 22[18] | |
| Group 8: i(12)(p10) | ||||||
| 43 | 2 m | 23 | M | 1.2 | 60-64〈3n〉,XX,− Y,− 2,− 4,− 5,del(6)(q21q24),add(6)(p22-25),del(7)(q32q35),− 8,− 9,der(11)t(4;11) (q28;q22),i(12)(p10)x2,der(13)t(8;13)(q13;p11),− 15,− 16,− 18,− 21,+ 4mar[19]/46,XY[2] | |
| 44 | 1 A m | 19 | M | 4.6 | 71-76〈3n〉,XYY,+ add(1)(q11),+ add(1)(q23),i(2)(q10),add(3)(p12),− 4,+ add(8)(p12),− 9,+ der(10) i(10)(q10)t(5;10)(q11;q26),− 11,i(12)(p10),− 13,− 17,+ 19x2,+ 20,+ 21,+ mar[7]/72-76,XYY,+ 1, der(1;2)(p10;q10),add(3)(p12),− 4,+ 8,− 9,+ der(10),− 11,i(12)(p10),− 13,+ 19,+ 21x2,+ mar[4] | |
| Group 9: Other structural changes | ||||||
| 45 | 2 m | 41 | M | 13 | 46,XY,t(16;21)(p11;q22)[20] | |
| 46 | 3 | 33 | M | 53 | ‡46,XY,t(16;16)(p13;q22)[13]/46,idem,del(7)(q33q36)[3]/46,XY[4] | |
| 47 | 1 A | 2 | F | 15 | 46,XX,del(13)(q13q32)[17]/46,XX[11] | |
| 48 | 1 A | 13 | M | 14 | 46,t(X;16)(q28;p12),Y[2]/46,XY[16] | |
| 49 | 1 A m | 7 | F | 13 | 46,X,add(X)(q12),der(7)t(X;7)(q12;p13),add(22)(q12)[3]/46,idem,del(6)(q21q26)[2]/46,XX[4] | |
| 50 | 1 A | 22 | F | 5.3 | 46,XX,del(9)(p21)[1]/46,X,t(X;21)(q24;q21),del(9)(p21),+ 19[19] | |
| 51 | 1 A | 12 | F | 10 | 47,XX,t(5;17)(p13;q22),t(16;17)(q21;q22),+ 19[14]/46,XX[6] | |
| 52 | 2 m | 2 | M | 21.5 | 46,XY,t(11;21)(q14;q22),del(22)(q13)[25]/46,XY[1] | |
| 53 | 3 | 66 | F | 0.1 | 47,XX,+ 5,del(6)(q15-16q26),add(11)(q22),− 22,+ mar[14]/46,XX[2] | |
In karyotype column, the lower case c indicates constitutional abnormality.
Age is indicated in months for patients under age 2 years.
Patients alive.
Case previously reported.
Several cases submitted were rejected by the morphoimmunologic validation procedure. The most frequent reason for rejection was mixed leukemias with a major component of myeloblasts in addition to megakaryoblasts. However, 6 patients with mixed proliferations were kept: 3 with a minor proerythroblastic (cases 5, 9, 47) and 3 with a minor myeloblastic component of blasts (< 10% of blasts; cases 26, 43, 45).
The GFHC also assessed cases for myelodysplastic features of the erythroid and granulocytic lineages when the number of residual cells allowed this evaluation. Dysgranulopoiesis was never observed among children and was present in 35% of adults. Dyserythropoiesis was found in 23% of children and in 22% of adults. Only one adult (case 40) presented with features of trilineage dysplasia.
Cytogenetic data
Constitutional karyotype was checked in 11 cases and the only constitutional chromosomal abnormality found was trisomy 21. One of the patients with DS also had a constitutional translocation (case 5). In one case of DS with trisomy 21 in mosaicism (case 8), the acquired clonal aberrations occurred in the clone +21c. Constitutional karyotype was normal in 2 patients with an acquired trisomy 21 (cases 10 and 11).
In 3 patients, including one with DS, no acquired abnormality was present. These karyotypes were classified as normal (NN). Clonal changes were observed in 94% karyotypes, either with normal cells (AN in 34 patients) or without (AA in 16 patients).
Distribution of the ploidy groups showed that karyotypes were mostly pseudodiploid (60% in children and 43% in adults). Hyperdiploidy was present in 26% of children and 35% of adults. In the hyperdiploid group, modal numbers ranged from 47 to 54 with a clear predominance of 47 and 48 modal numbers in children and in adults. Triploidy and tetraploidy were rare (3 cases) and only found in adults. Hypodiploidy was more common in adults (22%) than in children (only one case).
Complexity was assessed according to the number of unrelated abnormalities (≥ 3 unrelated abnormalities). The percentage of simple karyotypes (1 or 2 unrelated abnormalities) was higher in children (61.5%) than in adults (41.5%). The degree of complexity was lower in children than in adults (< 5 changes in most children and > 5 changes in most adults).
Most of the karyotypes (70%) were composed of unbalanced abnormalities, either with numerical (6 cases) or with both numerical and structural changes (44 cases).
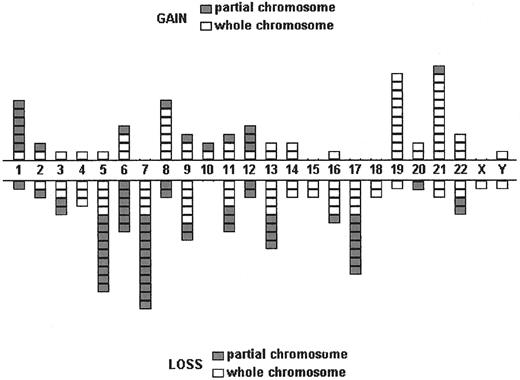
Chromosome gains and losses are shown in Figures1 and 2. Gains involved mainly chromosomes 8, 19, and 21, and partial trisomy 1q. Chromosomes implicated in losses were chromosomes 5, 6, 7, 9, 11, 13, 16, and 17. For chromosomes 5 and 7, partial deletions of the long arm were more frequent than losses of the whole chromosome. Five partial deletions of the short arm of chromosome 17 and 5 deletions of the long arm of chromosome 6 were observed.
Distribution of chromosome gains and losses among the 30 children and 23 adults.
Gains are shown in the upper part of the scheme with partial trisomies in gray and whole chromosome gains in white. Losses are shown in the lower part of the scheme with partial deletions in gray and whole chromosome losses in white. Each chromosome gain or loss is represented by a box.
Distribution of chromosome gains and losses among the 30 children and 23 adults.
Gains are shown in the upper part of the scheme with partial trisomies in gray and whole chromosome gains in white. Losses are shown in the lower part of the scheme with partial deletions in gray and whole chromosome losses in white. Each chromosome gain or loss is represented by a box.
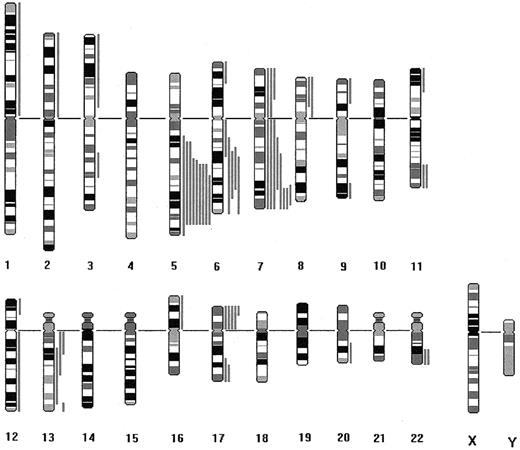
Schematic representation of the partial deletions observed among the 30 children and 23 adults.
Vertical solid bars located on the right of each chromosome (R-band diagram) represent the size of each deletion.
Schematic representation of the partial deletions observed among the 30 children and 23 adults.
Vertical solid bars located on the right of each chromosome (R-band diagram) represent the size of each deletion.
Abnormalities found as sole changes were either balanced: t(X;16)(q28;p12), t(1;22)(p13;q13), t(9;22)(q34;q11), t(3;12)(q26;p13), t(16;16)(p13;q22), t(16;21)(p11;q22), inv(3)(q21q26) or unbalanced: +3,+21, der(1;7)(q10;p10), del(7)(q31q35), del(5)(q23q33), add(13)(q33), del(13)(q13q32) (Table1).
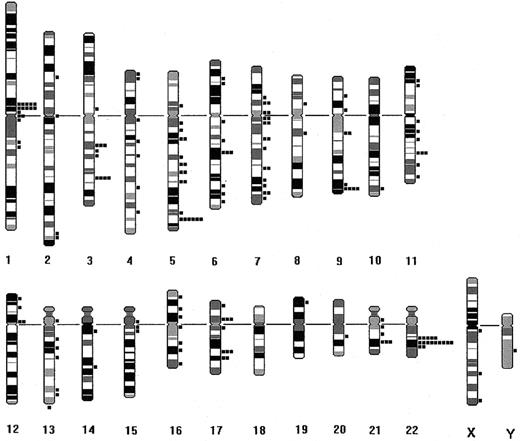
All the breakpoints are shown in the diagram of Figure3. The chromosomal regions most often disrupted were 5q (n = 18), 22q (n = 16), 7q (n = 14), 1p (n = 11), 3q (n = 9), 6q (n = 8), 11q (n = 8), and 9q (n = 7). The breaks in 1p, 22q, and 9q mostly resulted from t(9;22)(q34;q11) and t(1;22)(p13;q13). The breaks delineating the deletions accounted for the frequent involvement of 5q, 7q, and 6q. However, other clusters of breaks not involved in these known changes were also identified. A possible hot spot was 17q22-23 involved in 5 translocations, t(5;17)(p13;q22), t(16;17)(q21;q22), t(11;17)(p15;q23), t(7;17)(q22;q23), and a deletion, del(17)(q22). The 11q14-22 bands were implicated in 4 cases: 3 translocations, t(11;21)(q14;q22), t(4;11)(q28;q22), add(11)(q22) and a deletion del(11)(q22q24). Another cluster of breaks was observed in 21q21-22 rearranged in 4 translocations: t(X;21)(q24;q21), t(16;21)(p11;q22), t(11;21)(q14;q22), t(14;21)(q24;q22). The long arm of chromosome 16 was implicated in 3 changes involving the region 16q21-22-23: t(16;17)(q21;q22), t(16;16)(p13;q22), and add(16)(q23).
Distribution of the breakpoints observed among the 30 children and 23 adults.
All breakpoints including those resulting from deletions are represented on the right side of each chromosome (R-band diagram).
Distribution of the breakpoints observed among the 30 children and 23 adults.
All breakpoints including those resulting from deletions are represented on the right side of each chromosome (R-band diagram).
Karyotypes were then classified according to the presence of a recurrent change. In this classification, the DS were kept together as a group whatever their acquired changes. When 2 recurrent changes were observed, the most probable primary change determined the inclusion in a given group. Nine groups were identified (Table 1).
FISH and molecular results
No rearrangements of AML1 (case 50) andCBFβ (cases 48 and 51) genes were detected with FISH analyses. In cases 48 and 51, these results allowed us to rule out a cryptic inv(16)(p13q22).
In cases 1 and 10, no OTT-MAL fusion transcript was found. However, in case 13 with a normal karyotype, a strongly expressedOTT-MAL transcript was detected. No material was available to check the presence of the fusion gene with FISH. The t(1;22;4) also showed an OTT-MAL transcript (case previously reported by Mercher et al13)
In case 46, FISH analysis confirmed the t(16;16)(p13;q22) and RT-PCR detected a G-type CBFβ/MYH11 fusion transcript. In case 45, with a t(16;21)(p11;q22), a TLS/FUS-ERG transcript was found and the specificity of amplification was further confirmed by nucleotide sequence analysis, which showed an in-frame fusion ofTLS exon 7 to ERG exon 9.
Lack of correlation between the cytogenetic groups and the morphologic classification
No relationship could be established between the cytogenetic and the morphologic features because all morphologic aspects (categories 1, 2, and 3) were observed in each cytogenetic group (Table 1). The 3 morphologic categories were evenly distributed in the 2 age cohorts except for category 3, which was only found among adults.
Characteristics of the 9 cytogenetic groups
Group 1 (normal karyotypes) initially included 2 infants. However, one of them (case 13) showed an OTT-MAL fusion transcript and was therefore included in the t(1;22)(p13;q13) group (group 4). The only infant in group 1 had a relapse early after allogeneic BMT.
Group 2 (DS) had a median age of 2 years and low leukocytoses (median, 5 × 109/L) and platelet counts (median, 20 × 109/L). No preceding transient myeloproliferative phases or myelodysplastic syndromes were observed and 2 patients had a minor population of proerythroblasts. This group had a favorable outcome (see “Clinical and hematologic data”) because only 2 patients had relapses (cases 6 and 8). Case 8 with a complex karyotype died in relapse, whereas case 6 achieved second CR. Prognosis was not impaired by the presence of −7 in case 7.
Group 3 (numerical abnormalities not associated with structural changes) contained only trisomies. No OTT-MAL transcript was detected in the infant (case 10) analyzed by RT-PCR. Prognosis was poor in all cases.
Group 4, made up of patients with t(1;22) or with an OTT-MALtranscript, showed a prevalence of infant and congenital leukemias, female preponderance, and propensity to hepatosplenomegaly. Morphologically, the unifying feature of these patients was the constant presence of micromegakaryocytes in addition to blasts. In the 2 variant translocations identified, t(1;22;4)(p13;q13;q35) and t(1;22;14)(p13;q13;q31), the derivative 22 was of identical appearance to cases with the classical t(1;22) and the derivative 1 displayed the translocated portions of chromosomes 4 and 14. This group experienced an intermediate outcome and some patients proved to be good responders to intensive therapy (see “Clinical and hematologic data”).
The Philadelphia (Ph) chromosomes included in group 5 were found in both de novo M7 (cases 25 and 26) and a blastic phase of chronic myeloid leukemia (CML) (case 24). A fourth t(9;22) (case 28), found as a secondary change, was included in group 6. Outcome was poor for all patients but survivals were shorter when Ph chromosome was associated with inv(3) or −7.
Group 6, 3q21q26, was made up of patients with only 3q21 (cases 31, 32), only 3q26 (case 27), or both 3q21 and 3q26 (cases 28, 29, 30) breakpoints. Micromegakaryocytes were observed in only 2 patients and platelet counts were low except in case 28, which had a normal platelet count. Complete or partial deletions of chromosomes 5 and 7 were frequently associated and prognosis of this 3q21q26 group was very poor (median survival, 4.8 months) although the 2 children experienced longer survivals (21 and 23 months).
Group 7, composed of −5/del(5q) or −7/del(7q) or both, was characterized by an elevated median age (68 years), complex karyotypes, and a poor outcome (median survival, 5.8 months).
The patients of group 8, characterized by an isochromosome 12p, were young adults with a mediastinal mass and elevated serum markers (α-fetoprotein in both cases, neuron specific enolase in one and β-human chorionic gonadotrophin in the other) when the diagnosis of M7 was made in the bone marrow. The i(12)(p10) was found in both cases in a near-triploid karyotype (hypotriploid and hypertriploid). The course of the disease was extremely aggressive in both patients.
Among the miscellaneous changes found in group 9 there were recurrent and rare abnormalities. One of the recurrent changes was a t(16;16)(p13;q22) with a CBFβ-MYH11 fusion transcript (case 46). The patient had no eosinophils in the bone marrow and had the longest survival of all adults (4.4 years). Another recurrent change, t(16;21)(p11;q22) displayed the TLS/FUS-ERGtranscript. The rare translocations included in this group were mainly found in children with simple karyotypes and were associated with a poor outcome.
Discussion
The 53 cases of M7 collected in the current study allowed us to describe the spectrum of cytogenetic abnormalities found in this malignancy with their respective frequencies among children and adults, to analyze the features characterizing the main cytogenetic groups and to make assumptions on the origin of this acute leukemia (either de novo or secondary) and on the possible precursors involved.
To describe the cytogenetic features of M7, frequencies of the different cytogenetic abnormalities were compared with those of large series of de novo and secondary AMLs, which have included all FAB types from M1 to M7. We could establish these comparisons because our series was only composed of M7, whereas M7 represented less than 5% of cases in large published series of AML. This approach enabled us to better define the similarities and the discrepancies of M7 as compared to other acute myeloid proliferations and to specify the incidence of different changes in children and adult M7.
The high percentage of abnormal karyotypes (94%) found in our series showed that the percentage of abnormal karyotypes is higher in M7 than in de novo AMLs in which abnormal karyotypes represent approximately 80% of cases in children26-28 and 50% to 60% of cases in adults.29,30 In our study, karyotypes were complex in 39% of children and 52.5% of adults with a higher degree of complexity in adults than in children. These findings show that there are more complex karyotypes in M7 than in de novo AMLs in which the complex karyotypes represent 10% of cases in pediatric series31 and 34% of cases in adults (> 55 years).29
M7 presented similarities with other AMLs. The distribution of the ploidy groups and the cytogenetic profile of chromosome gains and losses were comparable to those observed in de novo AML, as exemplified by the most frequent trisomies (+8,+19,+21) and monosomies (−5, −7, −13, −16, −17). As in other AMLs, trisomies were usually complete, whereas monosomies were often partial and involved the long arms of chromosomes 5, 7, and 13 and the short arm of chromosome 17. However, an acquired trisomy 21 has also been assumed to be a cytogenetic feature of childhood M7, reported in 18% and 23% of patients with M7 (DS excluded) in the Lu et al7 and Ribeiro et al2 series, respectively. In our study, an acquired trisomy 21 was found in 20% of children (including acquired trisomies 21 in patients with DS) and 8% of adults. All these data suggest that an acquired trisomy 21 has a higher incidence in childhood M7 than in other childhood de novo AMLs (6% in the Grimwade et al30and 1.5% in the Raimondi et al28 series) and is probably one of the characteristics of childhood M7 (including DS).
Other features uncommonly found in de novo AMLs, characterized our M7 series: partial trisomies for the long arm of chromosome 1, partial deletion of chromosome 6q, trisomy 6, and deletion of chromosome 9 and of chromosome 11 (complete or involving 11q). Trisomy 6 was found in 6% of cases in Lu et al's series.7
No new recurrent abnormality was identified and the diversity of changes observed in our study illustrated the cytogenetic heterogeneity of M7. By classifying karyotypes according to the most probable recurrent abnormalities, we described 9 cytogenetic groups that probably comprised diseases presenting an M7 morphology. These groups were differently distributed among young and old patients.
In our study, t(1;22) was the most frequent abnormality among children (33%). This frequency was higher than in the Lu et al7(20%) and Athale et al3 (2.5%) studies, but it was in agreement with previous reports estimating that t(1;22) represents approximately one third of childhood M7.9,26,27 The finding of an OTT-MAL transcript in a patient with a normal karyotype suggests that the frequency of this group is still probably underestimated. The t(1;22) might be cryptic but it might also be undetected because it is often present in minor clones as attested by the frequently low numbers of blasts and of abnormal metaphases in these patients. The percentage of DS among our young patients (23%) is more in agreement with the frequency reported by Ribeiro et al2 (21%) and Athale et al3 (15%) than with that reported by Lu et al7 (54% of the children). In our study, 43% of children (13 patients) presented with normal karyotypes (2 patients), simple numerical changes (3 patients), complex karyotypes including 3q, 5q−, and −7 (2 patients), or with rare structural abnormalities (6 cases). The frequency of this category of childhood M7, without +21c or t(1;22), has varied considerably between previous reports.
Among adults, group 7, −5/del5q or −7/del(7q), or both, which represented 43% of cases in this age cohort, was the most frequent cytogenetic group. Actually, if we take into account cases in which chromosomes 5 and 7 abnormalities were associated with 3q changes or t(9;22), this incidence was even higher (56%). The corresponding frequencies reported by Cuneo et al4 and Ohyashiki et al5 in M7 series mainly made up of adults were lower (33% and 25%, respectively). However, all these estimations (current study and literature) were more elevated than those reported in de novo AMLs30 in which −5/del(5q), −7/del(7q) represented approximately 10% of patients, and closer to those reported in elderly de novo AMLs and in therapy-related AMLs where they can reach 30%.32-34 In our study, the 3q21q26 abnormalities were observed in 17% of adults. This frequency is in agreement with prior reports indicating incidences of 16%, 19%, and 25% in adult M7.4,5,7 The incidence of 3q aberrations in M7 is higher than in de novo AMLs (2%) and secondary AMLs (5%).30 Ph chromosome was as frequent as 3q abnormalities, representing 17% of adult M7. In previous reports, the incidence of t(9;22) in M7 has widely varied from 0% in Lu et al's, to 16% in Cuneo et al's and 66% in Ohyashiki et al's studies.4,5,7 This variability might reflect registration bias, that is, inclusion or noninclusion of blastic phases of CML. Even if its genuine incidence is difficult to assess in M7, t(9;22) is probably more frequent in this subgroup than in de novo AML as a whole, in which approximately 1% of patients are Ph+.29,30 Isochromosome 12p was the fourth most frequent change in our adult M7 (9%). This abnormality has occasionally been associated with megakaryoblastic leukemias35 but never reported in other series of M7.
Most of the features characterizing the 9 cytogenetic groups were in agreement with previous studies. However, some divergent or new specific data need to be emphasized. In patients with DS, we did not observe either the frequently reported transient myeloproliferative phase, or the trisomy 1q and trisomy 8 in karyotypes. In patients with t(1;22), the constant presence of micromegakaryocytes in addition to low percentages of blasts appeared as a new specific feature of this cytogenetic entity. These features were also observed in the patient with a normal karyotype and an OTT-MAL fusion transcript. The cytogenetic presentation of the 2 complex variants suggested that the derivative 22 is the critical chromosome. This assumption was reinforced by the recent description of the OTT-MAL fusion located on the derivative 22.13 Only one other variant has been previously reported.36 In group 6, 3q21q26, as opposed to the dysmegakaryocytopoiesis and the high platelet counts reported in myeloid malignancies with 3q abnormalities,37,38 micromegakaryocytes were rarely observed and platelet counts were low. The patients of group 8 (isochromosome 12p) presented with the features expected in the syndrome associating a mediastinal germ cell tumor (MGCT) and a hematologic malignancy (M7 in one third of cases).35 In addition to the typical clinical and biologic presentation, the near-triploid karyotypes displayed the chromosome gains and losses frequently observed in germ cell tumors, that is, the 2 patients shared losses of chromosomes 4 and 9, whereas chromosome 13 was lost in one patient and rearranged in the other. Coexistence of a triploid karyotype with a mediastinal mass in young adults with M7 should lead to a systematic search of i(12)(p10), which might be difficult to identify in complex karyotypes. In group 9 (miscellaneous changes), we observed a t(16;16)(p13;q22) with a CBFβ-MYH11transcript, which has been considered the diagnostic hallmark of AML M4 with abnormal eosinophils. The association M7/inv(16) might be nonrandom because 3 other cases have been reported2,4,39(case 46 has been reported by Costello et al19). Another recurrent change, t(16;21) (p11;q22) generating aTLS/FUS-ERG transcript, has been found in all subtypes of AML (except M3) and in several cases of M7.20 40 We can therefore confirm that this translocation belongs to the spectrum of cytogenetic abnormalities of M7. None of the rare translocations included in group 9 has been reported in the literature. They contributed to the identification of the possible hot spots of rearrangement found in this study.
Primary changes of a tumor, strongly related to the development of malignant proliferation, are sole and balanced structural abnormalities in the vast majority of cases.41 In our series, among the single abnormalities, t(1;22) has closely been related to M7, whereas most of the others (see list in “Results”) have been mainly related to other myeloproliferative, myelodysplastic malignancies or acute leukemias and occasionally published in M7. Conversely, the t(X;16)(q28;p12), which has not been previously reported, and trisomy 3, which is a very rare numerical change in AML, were both observed as sole abnormalities, thereby emerging as possible primary changes in M7.
In addition to frequent breakpoints resulting from known recurrent changes, our study revealed several clusters of more uncommon breakpoint regions, located on 17q22-23, 11q14-21, 21q21-22, and 16q21-22-23. Because these breaks were mostly generated by rare translocations in simple karyotypes (not associated with changes previously related to M7), we can assume that they might pinpoint hot spots of rearrangements frequently involved in M7. Among the genes mapped in these regions, only CBFA2 (AML1) located in 21q22, has proved to be involved in megakaryopoiesis.42 No rearrangement of AML1gene was detected in our study but only 1 of the 4 patients with a 21q21-22 breakpoint could be analyzed using molecular methods.
Despite the absence of a suggestive history among 90.5% of patients in our series, several cytogenetic and morphologic features argued in favor of the occurrence of M7 as a secondary leukemia.
In adults, this assumption was supported by the high incidence of complex karyotypes, of unbalanced changes, of −5/del(5q), −7/del(7q), 3q21q26, and abnormalities such as dic(1;15)(p11;p11), inv(4)(p15q11), t(14;21)(q24;q22), der(7)t(7;17)(q11;q11) and t(6;13)(p22;q14) already reported in myelodysplasia and secondary leukemia,43-46 and also by the presence of dysgranulopoiesis found in one third of patients. In patients without such a history, it is possible that a number of cases of M7 had arisen from a previously undiagnosed myelodysplastic phase. However, the elevated age of patients might also have contributed to this presentation because de novo AMLs arising in elderly individuals are often cytogenetically and morphologically very similar to leukemias developing after aggressive therapy, occupational exposure, or myelodysplastic syndrome.
In contrast to adults, there was little evidence to suggest that childhood M7 typically arises as a secondary leukemia, because no dysgranulopoiesis and few of the “hallmark” chromosomal abnormalities were observed. In contrast with a recent series of childhood M7, which reported that 15% occurred after prior therapy for acute lymphoblastic leukemia with a frequent involvement of 11q23,3 no prior toxic exposure was identified in the children of our study and the only 11q23 breakpoint was found in one patient who also presented with the classical combination of 3q, −7, and 5q abnormalities consistent with a secondary leukemia (case 31). This raises the question as to whether this patient was subject to an unidentified prenatal or perinatal exposure. This may also apply to patients with t(1;22) who invariably develop leukemia in early infancy.
The morphologic and cytogenetic features also led us to hypothesize on the precursors involved in M7. Although the megakaryocytic commitment of blasts was unequivocal in all cases, the initial precursor involved seemed to be more immature in adults than in children as evidenced by the high frequency of 3q21q26, t(9;22), −7, and 5q abnormalities reported to involve multipotent stem cells, by the detection of dysgranulopoiesis and dyserythropoiesis in 35% and 22% of adult patients and by the presence of morphologically undifferentiated megakaryoblasts (category 3 of the morphologic classification) only among adults. An even earlier precursor was probably implicated in patients with i(12p) because it has been assumed that in M7 developing concurrently with MGCT, blasts derive from a common ancestor, reminiscent of the first stem cells in the yolk sac.47Conversely, because chromosomal abnormalities evoking a stem cell involvement were rare among children, and also because only the erythroid and megakaryocytic lineages were affected, it might be assumed that a more mature precursor is involved in childhood M7. However, this assumption needs to be corroborated by further ultrastructural and functional evidence as it has been previously demonstrated for M7 occurring in patients with DS.48
This study on 53 patients with acute megakaryoblastic leukemia validated by a review of morphologic and immunophenotyping data is the largest comprehensive series with cytogenetic data including children and adults reported to date. It allowed us to display the spectrum of recurrent changes observed in M7, to assess their frequencies and to emphasize the differences between M7 developing in infancy and adulthood. The diversity of chromosomal abnormalities and their frequent association in complex karyotypes account for the difficulty in understanding the primary molecular rearrangements.
We thank David Grimwade for his most valuable suggestions and Mariana Titorov for her editorial assistance.
The lists the name of the institute, with the center and number of cases in parentheses, followed by the names of other participants. Institut Paoli Calmettes (Marseille; n = 16): Jean Albert Gastaut, Didier Blaise, Christine Arnoulet, Danielle Sainty; CHU Toulouse (Toulouse; n = 9): Emilienne Kuhlein, Alain Robert, Françoise Huguet; Hôpital Debrousse (Lyon; n = 7): Anne Marie Manel, Claire Galambrun, Emmanuelle Homolle; Hôpital Necker (Paris; n = 4): Françoise Valensi, Pierre Quartier; CHU Nantes (Nantes; n = 3): Hervé Avet-Loiseau, Richard Garand, Françoise Mechinaud; Hôpital Robert Debré (Paris; n = 2): Etienne Vilmer; Hôpital Bicêtre (Paris; n = 2): Danielle Feneux, Anne Beauchamp-Nicoud; CHU Caen (Caen; n = 2): Michèle Malet, Patrick Boutard; Hôpital Haut Lévêque (Bordeaux; n = 1): Jean-Philippe Vial, Francis Lacombe, Jean-Michel Boiron, Philippe Bernard; Hôpital Universitaire de Genève (Genève, Suisse; n = 1): Pierre Wacker, Jacqueline Schmid; CHU La Timone (Marseille; n = 1): Chantal Fossat, Gerard Michel; CHU Reims (Reims) (n = 1): Sylvie Daliphard, Catherine Behar; CHU Brest (Brest; n = 1): Marie Chantal Leglise, Christian Berthou; CHU Dijon (Dijon; n = 1): Isabelle Luquet, Bernardine Favre, Marc Maynaide, Gérard Couillault; Hôpital Saint Antoine (Paris; n = 1): Mircea Adam, Judith Landman-Parker, Guy Leverger; and CHU Montpellier (Montpellier; n = 1): Jacques Taib, Geneviève Margueritte. Paola Ballerini (Hôpital Trousseau-Paris) and Florence Nguyen-Khac (Groupe Hospitalier Pitié-Salpétrière-Paris) performed the molecular analyses of OTT-MAL and FUS-ERG transcripts. Anna Aventin (Hopital San Pau-Barcelona) contributed to FISH studies.
Prepublished online as Blood First Edition Paper April 17, 2002; DOI 10.1182/blood-2001-12-0241.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Nicole Dastugue, Laboratoire d'Hématologie, Génétique des Hémopathies, Hôpital Purpan, Place du Dr Baylac, 31059 Toulouse Cedex, France; e-mail:dastugue.n@chu-toulouse.fr.