The 2 lymphotoxin subunits LTα (also called tumor necrosis factor β [TNF-β]) and LTβ belong to the family of TNF-related cytokines. They form either a soluble homotrimeric ligand (LTα3) that binds to and signals through CD120a/b (TNFRp55 and TNFRp75), or a membrane-associated heterotrimeric ligand (LTα1β2) that binds to and signals through the LTβ receptor (LTβR). In mice, LTβR signaling is critical for the maintenance of peripheral lymphoid tissues and optimal immune responses, and its down-regulation results in immunodeficiency. To determine the possible relationship between LT-mediated immunodeficiency and the immunosuppressive effects of cyclosporin A (CsA), we tested the effects of CsA on the expression of LTα and LTβ in human peripheral blood mononuclear cells (PBMCs). When PBMCs were stimulated with phorbol myristate acetate/ionomycin or with anti-CD3/anti-CD28, the accumulation of LTα both at mRNA and protein levels was markedly inhibited by CsA. This inhibition is likely due to CsA's effect on the nuclear factor of activated T cell (NFAT) proteins binding to a novel NFAT-binding element at position −490 relative to LTα transcription start. LTβ showed a distinct expression pattern and was insensitive to CsA. Thus, in addition to its effects on the expression of other TNF family members, such as TNFα, CD40-L, and CD95-L, CsA can block expression of surface LT complex by selectively inhibiting the expression of the LTα subunit. We propose that LT dysfunction and its downstream effects may contribute to immunosuppressive effects of CsA.
Introduction
Members of the tumor necrosis factor (TNF) cytokine family are critically involved in immune responses associated with inflammation, tissue homeostasis, and innate immunity,1-3as well as in organogenesis and maintenance of functional lymphoid tissues.4 Most of the cytokines of this family, consisting of about 20 members, are type II transmembrane glycoproteins, which can form homotrimers and heterotrimers.5 Lymphotoxin α (LTα) is unique among these cytokines in that it lacks the transmembrane region,6 and the membrane-associated form of LTα depends on its membrane-bound partner, LTβ.7,8LTα complexes function in 2 major trimeric forms: (1) as a soluble LTα3 homotrimeric ligand through TNF receptor CD120a (TNFRp55) and (2) as a membrane-bound LTα1β2 heterotrimer, through LTβ receptor (LTβR),9 and are believed to be expressed mainly on activated lymphocytes and natural killer (NK) cells.10 The role of LTα→TNFRp75 signaling in vivo and the significance of the third minor complex, LTα2β1, are not completely understood.
Much of the current knowledge concerning the functions of LT results from experiments in the murine system, including knockout and transgenic mice.4 Mice deficient in LTα and LTβ display major defects in the architecture of peripheral lymphoid organs, demonstrate an impaired ability to produce antigen-specific IgG in either primary or secondary responses, and are IgA deficient.11-13 Experiments using soluble LTβR-Ig fusion proteins revealed that disruption of the signaling through LTβR affects the normal development of peripheral lymphoid tissue.14-16 TNFR-Ig administration resulted in less severe defects.17 Other studies demonstrated that inhibition of membrane-bound LTα/β heterotrimer signaling by anti-LTβ antibodies, or by an excess of soluble LTβR-Ig, resulted in the disappearance of multiple markers on follicular dendritic cells (FDCs) within one day.18 19 Taken together, these studies established that LT-mediated signaling is important for (1) the development and maintenance of peripheral lymphoid tissue architecture, (2) B-cell maturation, and (3) antibody class switch during immune responses.
The link between human LT genes and immunodeficiency was suggested by a genetic study of a large human family with the inherited IgA deficiency (IgAD) and common variable immunodeficiency (CVID). The susceptibility locus for the disease was mapped between major histocompatibility complex (MHC) class III markers, a region containing 21 identified genes that include TNF, LTA, andLTB.20
Based on all these considerations, it is conceivable that in humans the disruption of LT signaling by pharmacologic agents may dramatically affect the development of FDC networks and interfere with proper development of germinal centers, class switch, and antibody response. Deficient immune responses in humans are consistently observed in patients undergoing allograft transplantation and subsequent immunosuppressive treatment with cyclosporin A (CsA).
In this paper we report that LTα and LTβ, the 2 components of the surface LT, display different expression patterns in human peripheral blood mononuclear cells (PBMCs) and respond differently to CsA. We demonstrate that expression of LTα is markedly down-regulated by CsA and that this effect may be mediated by a novel regulatory site in the LTα upstream promoter region. Our data imply that CsA may inhibit LTβR signaling by suppressing production of LTα, and this mechanism may contribute to the overall immunosuppression.
Materials and methods
PBMCs and cell culture
Human PBMCs were isolated from buffy coats prepared from healthy donors by Ficoll-Hypaque gradient centrifugation. Approval was obtained from the Institutional Review Board for these studies, informed consent was provided according to the Declaration of Helsinki. For PBMC isolation, a buffy coat (50-80 mL) was added to 1 mL heparin solution in phosphate-buffered saline (PBS; 1:10 Liquemin N10 000, Hoffmann-La Roche, Basel, Switzerland) and TC199 medium (Cytogen, Berlin, Germany) or Dulbecco modified Eagle medium (DMEM; Gibco BRL/Life Technologies, Gaithersburg, MD) was added to a final volume of 100 mL. Each third of this solution was carefully layered on 10 mL 1.077 g/mL Ficoll solution (Sigma, St Louis, MO) in a 50-mL plastic tube and centrifuged at 400g for 30 minutes at room temperature. Cells at the interface were collected and washed twice in TC199 or DMEM. Freshly isolated PBMCs (107/mL) were suspended in RPMI 1640 medium (Gibco BRL/Life Technologies) supplemented with 0.5% fetal bovine serum (FBS), and preincubated with 400 nM CsA (from 2 μM stock in dimethyl sulfoxide [DMSO]), or DMSO as a control, for 30 minutes. Cells were then induced with either 100 ng/mL or 20 ng/mL phorbol myristate acetate (PMA) and 2 μM ionomycin in the presence or absence of the indicated agents prepared as 1000-fold stock solutions in DMSO. A DMSO concentration of 0.2% (vol/vol), unless otherwise indicated, was maintained at all time points measured. In some experiments 5 μg/mL mouse monoclonal anti-CD3 antibodies (clone UCHT1) and anti-CD28 antibodies (clone ANC28.1/5D10; Calbiochem, La Jolla, CA) were used for PBMC activation. CsA was a gift from Dr U. Christians (Institute for Pharmacology, Hannover Medical School) or was purchased from Calbiochem (San Diego, California). After treatment of cells, total RNA or whole cell extracts were prepared for further analyses.
RNA isolation and Northern blotting
Our protocols for RNA isolation and Northern blotting essentially followed standard procedures21,22 and have been previously described.23 Northern analysis was performed using 10 μg total RNA per sample and the following hybridization probes: 1.4 kb BamHI-EcoRI fragment of human LTA gene24 containing all 3 coding exons 2-4, or a 0.5-kb fragment of human LTBgene8 containing exon 4 (Figure 1B). Images of radioactive blots were obtained either on x-ray film (X-Omat, Kodak, Rochester, NY) or using PhosphorImager plates (Fuji Photo Film, Tokyo, Japan).
Regulation of LTα and LTβ transcription in primary human cells.
(A) Northern blot analyses of LTα and LTβ mRNA levels in human PBMC. (B) Location of LTα and LTβ hybridization probes within the human TNF-α locus. Cells were treated with 20 ng/mL PMA plus 2 μM ionomycin (P/I) in presence (+) or absence (−) of CsA (400 nM), as indicated. CsA was added 30 minutes prior to activation. No act indicates nonactivated control. RNA (10μg) from 5 to 10 × 106 cells taken at indicated time points was used for Northern analysis. Ethidium bromide staining of 18S RNA at the bottom panel is shown as RNA loading control.
Regulation of LTα and LTβ transcription in primary human cells.
(A) Northern blot analyses of LTα and LTβ mRNA levels in human PBMC. (B) Location of LTα and LTβ hybridization probes within the human TNF-α locus. Cells were treated with 20 ng/mL PMA plus 2 μM ionomycin (P/I) in presence (+) or absence (−) of CsA (400 nM), as indicated. CsA was added 30 minutes prior to activation. No act indicates nonactivated control. RNA (10μg) from 5 to 10 × 106 cells taken at indicated time points was used for Northern analysis. Ethidium bromide staining of 18S RNA at the bottom panel is shown as RNA loading control.
Immunoprecipitation and antibodies
Immunoprecipitation was performed essentially as described.23 To block LTα secretion, treatment of cells was done in the presence of 10 μg/mL protein secretion inhibitor Brefeldin A (Calbiochem, San Diego, CA). The cells (108) were lysed in the lysis buffer containing 50 mM Tris (tris(hydroxymethyl)aminomethane), pH 7.7, 250 mM NaCl, 5 mM EDTA (ethylenediaminetetraacetic acid), 2% NP-40, 50 mM NaF, 5 mM Na4P2O7, 10 mM sodium glycerophosphate, 2 μM microcystin-LR (Alexis, Gruenberg, Germany), and cocktail of protease inhibitors. Then 40 μL protein-G-Sepharose (Pharmacia, Uppsala, Sweden) and 20 μL anti-LTα polyclonal rabbit antiserum no. 3236 against KLH-conjugated synthetic peptide LPGVGLTPSAAQTARQHPKC (single-letter amino acid codes) spanning amino acids 1-19 of the secreted form of human LTα23 were added to lysate precleared by centrifugation and incubated overnight with continuous rotation at 4°C. The immune complexes were washed 4 times with lysis buffer, boiled in 2 times sodium dodecyl sulfate (SDS) gel-loading buffer, and subjected to Western blotting. The Chinese hamster ovary (CHO) cell line stably transfected with LTα/LTβ expression construct (kindly provided by Dr J. Browning) and untransfected CHO cell line were used as positive and negative controls, respectively.
Western blotting
Transfer to nitrocellulose membranes (Optitran BA-S 85, Schleicher and Schuell, Dassel, Germany) was performed under semidry conditions in transfer buffer (50 mM Tris, 40 mM glycine, 375 mg/L SDS, 20% [vol/vol] MeOH) for 2 hours at 0.8 mA/cm2. Membranes were blocked with 5% (wt/vol) nonfat dry milk in TBST (20 mM Tris-HCl, pH 8.0, 0.9% NaCl, 0.05% [vol/vol] Tween20) for 1 hour. Proteins were incubated with the anti-LTα rabbit polyclonal antiserum no. 323623 in 5% (wt/vol) nonfat dry milk/TBST for 12 hours at 4°C. Membranes were then washed 3 times in TBST for 5 minutes and incubated for 1 hour with secondary horseradish peroxidase-conjugated goat anti–rabbit IgG antibody (Amersham, Braunschweig, Germany) in 5% (wt/vol) nonfat dry milk/TBST and developed with the enhanced chemiluminescence (ECL) reagents (Amersham).
LTα promoter analysis and oligonucleotide probes
Analysis of nucleotide sequence of human LTα promoter using MatInspector site prediction program and weight matrices from Transfac database (http://transfac.gbf.de/) revealed a number of potential NFAT-binding sites within the proximal 0.7-kb (Figure 4A). The following double-stranded oligonucleotide probes were synthesized, each encompassing one of the potential NFAT sites together with the flanking regions (heterologous sequences at the end of the probes not present in the promoter are shown in lower case): NFAT3 5′-gaa ttC CCT GAC CCG ACT CCC TTT CCC AGA; NFAT4 5′-gaa ttC GAT GGG CTG GAA AGT CCG TAT ACT; NFAT5 5′-gaa ttC CCT TTG TAG AAA ACT TTG GAA GGT; A-NFAT 5′-CTC CTA GGC CTC AGC CTT TCC TGC CTT TGA CTG AAA; B-NFAT 5′-GGA CAG GGG TAC AAG AGA AGG AAA TGG GCA AAG AGA; kB 5′-cat gCA ACA GAG GGG ACT TTC CGA GAG Gca tg; LTAKB 5′-gaa ttG CCC TGG GGG CTT CCC CGG GCC CCA. Probes were labeled either with [α-32P]dATP (deoxyadenosine triphosphate) by Klenow fragment (NFAT3-5) or with [γ-32P]dATP by bacteriophage T4 polynucleotide kinase (A-NFAT and B-NFAT) using standard procedures.25
Nuclear extracts and electrophoretic mobility shift assay
For nuclear extract preparation, freshly isolated human PBMCs were collected, washed, and resuspended in RPMI 1640 medium supplemented with 0.5% FBS as described above. Freshly isolated PBMCs (1-3 × 107/mL) were preincubated with 400 nM CsA (or with DMSO as control) for 1 hour. Cells were stimulated with 100 ng/mL PMA and 2 μM ionomycin for 10 or 30 minutes. After treatment cells were washed once with ice-cold PBS, resuspended in 1 mL buffer A (10 mM HEPES [N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid], pH 7.9, 10 mM KCl, 0.1 mM EDTA, 0.1 mM EGTA [ethyleneglycoltetraacetic acid], 1 mM DTT [dichlorodiphenyltrichloroethane], 0.5 mM PMSF [phenylmethylsulfonyl fluoride], Complete protease inhibitor cocktail [Boehringer Mannheim]) and incubated on ice for 15 minutes. After adding of 1/15 vol/vol 10% NP-40 and rigorous vortexing, samples were left on ice for 3 minutes and then centrifuged. Nuclei were resuspended in 100 μL buffer C (20 mM HEPES, pH 7.9, 400 mM NaCl, 1 mM EDTA, 1 mM EGTA, 1 mM DTT, 0.5 mM PMSF, Complete protease inhibitor cocktail [Boehringer Mannheim]) and incubated on ice for 10 to 15 minutes. Nuclear extracts were centrifuged, aliquoted, and snap-frozen in liquid nitrogen. Protein concentration of nuclear extracts was determined by Bradford assay and 4 μL of each nuclear extract (approximately 10 μg) was incubated with 20 to 50 fmol labeled probe (10 000-20 000 cpm) in the binding buffer (12.5 mM HEPES, pH 7.8, 6% glycerol, 0.5 mM EDTA, 0.5 mM EGTA, 0.125 μg/μL poly-dIdC (polydeoxyinosinic-deoxycytidylic acid; Sigma) and 3% fetal calf serum [FCS]) in 10 μL total reaction volume for 5 minutes at room temperature. Where indicated, the reaction was further incubated with 0.5 μL polyclonal rabbit anti-NFAT serum no. 79626 or anti-NFκB1 serum no. 114127 for 10 minutes at room temperature. Complexes were resolved on a 5% polyacrylamide gel in Tris-borate buffer (45 mM Tris, pH 8.0, 45 mM boric acid, 0.5 mM EDTA) as previously described.28 The gels were dried and visualized on Cyclone phosporimaging system (Packard Bioscience, Meriden, CT).
Results
The LTα/LTβ membrane complex constitutes a unique signaling ligand whose biologic function depends on the coexpression of both its subunits. In this study we focused on the regulation of the LTα gene in primary human cells with special emphasis on the effects mediated by CsA.
LTα and LTβ differ in their basal expression levels in primary human blood cells
In unstimulated PBMCs no basal RNA expression of the LTα gene can be detected by Northern blot analysis, regardless of CsA pretreatment (Figure 1A, lanes 1 and 2). In contrast, the LTβ gene is expressed with significant mRNA levels in these cells when they were freshly isolated from donor blood (Figure1A, lane 1; see also Browning et al8 and Millet and Ruddle29). This level of basal LTβ expression was unaffected by treatment of these cells with CsA (Figure 1A, lane 2). This comparison identifies a distinct difference in the mRNA expression levels of the 2 LT subunits, LTα and LTβ, in human PBMCs.
Activation of LTα expression in PBMCs is sensitive to CsA
When PBMCs were stimulated with the phorbol ester PMA plus the Ca++-ionophore ionomycin, significant LTα mRNA levels were detected by Northern blot analysis after 4 hours (Figure 1A, lane 3). Prior treatment of the PBMC population with CsA effectively prevented LTα up-regulation by PMA plus ionomycin (lanes 4 and 6). We then investigated whether the CsA prevented LTα induction using stimuli that mimic physiologic activation of T cells. PBMCs were activated with anti-CD3 and anti-CD28 monoclonal antibodies via a T-cell receptor (TCR)–mediated and costimulatory mechanism. The combination of both signals activated PBMCs considerably more strongly than either anti-CD3 or anti-CD28 alone (Figure2, compare lanes 3 and 5 to lane 7). In this case, CsA treatment reduced the level of CD3/CD28-induced LTα message by at least 80% at both the 5-hour and 9-hour time points (Figure 2, lanes 7 and 9, and 8 and 10), suggesting that the effects of CsA on PBMCs may be relevant to the mechanisms acting in vivo.
CsA inhibits LTα mRNA levels in anti-CD3 or anti-CD28 activated PBMCs.
PBMCs were treated with 5 ng/mL anti-CD3 antibodies (aCD3), 5 ng/mL anti-CD28 antibodies (aCD28), or 5 ng/mL anti-CD3 plus 5 ng/mL anti-CD28 antibodies in the presence (+) or absence (−) of CsA (400 nM), as indicated. CsA was added 30 minutes prior to activation. See Figure 1 and “Materials and methods” for details.
CsA inhibits LTα mRNA levels in anti-CD3 or anti-CD28 activated PBMCs.
PBMCs were treated with 5 ng/mL anti-CD3 antibodies (aCD3), 5 ng/mL anti-CD28 antibodies (aCD28), or 5 ng/mL anti-CD3 plus 5 ng/mL anti-CD28 antibodies in the presence (+) or absence (−) of CsA (400 nM), as indicated. CsA was added 30 minutes prior to activation. See Figure 1 and “Materials and methods” for details.
PMA/ionomycin down-regulates the basal LTβ level of expression in PBMCs
Basal RNA levels of LTβ are high in freshly prepared PBMCs (Figure 1A, lane 1). Unexpectedly, this high basal level was drastically reduced on treatment of cells with PMA plus ionomycin for 4 or 8 hours (Figure 1A, lanes 3 and 5, approximately 3 times and 5 times reduction, respectively, compared with lane 1), but not by incubation in cultural medium without activation (data not shown). Additional treatment with CsA had no effect on this down-regulation by PMA/ionomycin (lanes 4 and 6). Thus, the 2 genes, LTα and LTβ, have distinct patterns of regulation. In contrast to LTα transcription, PMA/ionomycin treatment resulted in down-regulation of LTβ transcripts in PBMCs.
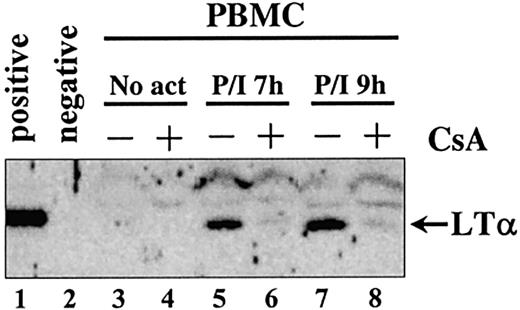
CsA inhibits induced LTα protein expression in PBMCs
To determine whether the RNA expression patterns paralleled protein expression levels in these primary human blood cells, immunoprecipitations were performed with extracts from PBMCs activated with PMA/ionomycin in the presence or absence of CsA. Antipeptide polyclonal serum no. 323623 directed against LTα was used for the immunoprecipitations using whole cell lysates. The protein secretion inhibitor Brefeldin A was used during cell activation to block LTα protein secretion. Precipitates subjected to Western analysis revealed that LTα protein levels paralleled mRNA levels (compare Figure 1A and Figure 3). No LTα expression was seen in untreated PBMCs, whereas treatment with PMA/ionomycin induced LTα protein expression (Figure 3, lanes 5 and 7). As for mRNA, LTα protein induction by PMA/ionomycin was almost completely blocked by CsA (Figure 3, lanes 6 and 8). Immunoprecipitation of LTβ protein from PBMC extracts revealed constant LTβ protein levels not sensitive to PMA/ionomycin or CsA (data not shown).
CsA inhibits LTα protein expression in PBMCs.
Cells were treated with 20 ng/mL PMA plus 2 μM ionomycin (P/I) in the presence (+) or absence (−) of 400 nM CsA for the indicated time in hours (h). CsA was added 30 minutes prior to activation. For each time point extracts from 108 cells were immunoprecipitated with antipeptide rabbit polyclonal serum no. 3236. Proteins were detected by subsequent Western blotting with the same antiserum. Extracts from CHO cells stably transfected with LTα and LTβ expression construct were used as positive control; untransfected CHO cells were used as negative control.
CsA inhibits LTα protein expression in PBMCs.
Cells were treated with 20 ng/mL PMA plus 2 μM ionomycin (P/I) in the presence (+) or absence (−) of 400 nM CsA for the indicated time in hours (h). CsA was added 30 minutes prior to activation. For each time point extracts from 108 cells were immunoprecipitated with antipeptide rabbit polyclonal serum no. 3236. Proteins were detected by subsequent Western blotting with the same antiserum. Extracts from CHO cells stably transfected with LTα and LTβ expression construct were used as positive control; untransfected CHO cells were used as negative control.
We concluded from these expression measurements that the 2 components of the surface LT complex in PBMCs, LTα and LTβ, are differently regulated at the mRNA and protein levels. Because LTα was the limiting component in this system, its activation appeared to be a crucial and regulatory step in the formation of heterotrimeric lymphotoxin surface complexes in PBMCs. LTα, and not LTβ, appeared to be the target of inhibition by the immunosuppressant CsA both at the RNA and the protein levels.
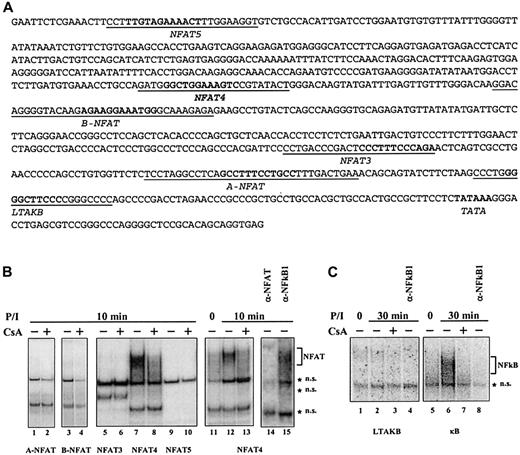
Identification of a novel NFAT site in human LTα promoter
To determine the molecular mechanisms of CsA action, we examined binding of nuclear proteins to the promoter region of human LTα gene using MatInspector site prediction program.30 Five regions within the proximal 700 nucleotides proximal to the transcription start matched consensus binding sequence for NFAT (Figure4A), the most likely candidate for the downstream target of CsA effects (for a review, see Kiani et al31). In addition, our analysis pointed to an NFκB site 90 nucleotides upstream of the transcription start, which we termed LTAKB (Figure 4A). Binding of NFκB proteins is sensitive to CsA,32,33 and the role of this particular NFκB binding sequence in LTα transcriptional activation in T-cell lines in response to LTα3 or to human T-cell lymphotropic virus (HTLV) tax has been reported previously.34-37
PMA/ionomycin-inducible and CsA-sensitive NFAT binding in human LTα promoter.
(A) Sequence of human LTα promoter. Predicted NFAT and NFκB sites are in bold, sequences of the corresponding oligonucleotide probes are underlined. (B) Binding to NFAT probes. PBMCs were treated with 100 ng PMA and 2 μM ionomycin for 10 minutes (P/I) in the presence (+) or absence (−) of 400 nM CsA. CsA was added 30 minutes prior to activation. Nuclear extracts from 1 to 3 × 107/mL PBMCs were analyzed in EMSA with different predicted NFAT-binding probes from human LTα promoter. Specificity of PMA/ionomycin-inducible and CsA-sensitive NFAT binding to NFAT4 site was confirmed by abolishing the binding with anti-NFAT, but not anti-NFκB1 sera. (C) NFκB binding. Brackets indicate the location of NFAT (B) or NFκB (C) complexes. *NS indicates nonspecific bands.
PMA/ionomycin-inducible and CsA-sensitive NFAT binding in human LTα promoter.
(A) Sequence of human LTα promoter. Predicted NFAT and NFκB sites are in bold, sequences of the corresponding oligonucleotide probes are underlined. (B) Binding to NFAT probes. PBMCs were treated with 100 ng PMA and 2 μM ionomycin for 10 minutes (P/I) in the presence (+) or absence (−) of 400 nM CsA. CsA was added 30 minutes prior to activation. Nuclear extracts from 1 to 3 × 107/mL PBMCs were analyzed in EMSA with different predicted NFAT-binding probes from human LTα promoter. Specificity of PMA/ionomycin-inducible and CsA-sensitive NFAT binding to NFAT4 site was confirmed by abolishing the binding with anti-NFAT, but not anti-NFκB1 sera. (C) NFκB binding. Brackets indicate the location of NFAT (B) or NFκB (C) complexes. *NS indicates nonspecific bands.
Binding assays using nuclear extracts from PBMCs treated with PMA/ionomycin with or without CsA revealed characteristic NFAT binding to a distinct NFAT site, termed NFAT4 and located 490 nucleotides upstream of the transcription start site (Figure 4B, lanes 7, 8, and 11-15). The specificity of the binding was confirmed by disruption of binding by specific antiserum (Figure 4B, lanes 14 and 15) and by competition with nonlabeled probe (data not shown). None of the other 4 sites identified by computer analysis demonstrated any detectable specific binding (Figure 4B, lanes 1-6, 9, 10, and data not shown). Importantly, binding to NFAT4 site was inducible by PMA/ionomycin and at least 80% of this binding could be inhibited by CsA (Figure 4B, lanes 7, 8, and 11-13).
No detectable NFκB binding to LTAKB probe was observed, either in nonactivated cells (Figure 4C, lane 1) or 30 minutes after activation with PMA/ionomycin (Figure 4C, lane 2). This lack of NFκB binding appears to be the property of the specific sequence of the κB site from LTα promoter, because control κB oligonucleotide showed strong PMA/ionomycin-inducible binding in the same nuclear extracts (Figure 4C, lanes 5 and 6). The control NFκB activity was strongly inhibited by CsA (Figure 4C, lane 7) and was completely abolished by anti-NFκB1 antibody (Figure 4C, lane 8).
Our data strongly suggest that the previously unrecognized NFAT-binding element in human LTα promoter mediates transcriptional activation of the LTα gene by NFAT. The same site may be responsible for the suppressive effects of CsA on LTα transcription. NFκB factors, even though strongly inducible in PBMCs by PMA/ionomycin and CsA sensitive, did not bind to the κB site from LTα promoter and therefore did not appear to be important for the LTα transcriptional regulation in this particular system.
Discussion
In this study we addressed 2 previously unresolved issues regarding the regulation of LT components in primary human cells: (1) whether in primary human blood cells the expression of either of the 2 components was sensitive to the action of the immunosuppressant CsA and (2) whether these 2 components are regulated concordantly.
The molecular mechanisms of CsA immunosuppressive effects have been elucidated and largely attributed to inhibition of the phosphatase calcineurin,38 which regulates, among other targets, the transcription factor NFAT.39 CsA suppresses the activity of many genes,40 including 3 members of the TNF family, TNFα, CD40L, and CD95L.41 Although CsA-mediated effects on the LTα mRNA levels have been previously reported,42 43 the molecular mechanisms of this suppression were not addressed in detail.
First of all, we found that expression of LTα, but not LTβ, is inducible in PBMCs. We then investigated the effects of Ca++- and protein kinase C (PKC)–stimulated signaling, as induced by ionomycin and PMA, respectively, on the expression of LTα. Our data show that simultaneous activation of PBMCs with PMA/ionomycin caused induction of LTα at both the mRNA and protein levels. The finding that LTα expression is modulated by CsA is in agreement with the earlier observations made using Northern hybridization,42,43 and apoptosis-based bioassays,44,45 as well as with recent data obtained with DNA array technology.40 Importantly, we have demonstrated that LTα protein levels follow CsA-mediated down-regulation of LTα mRNA synthesis, implying relatively short protein half-life for LTα.
Contrary to LTα, LTβ mRNA was expressed constitutively in human PBMCs (see also Browning et al8 and Millet and Ruddle29) and, surprisingly, PMA/ionomycin treatment down-regulated LTβ message levels (Figure 1A and data not shown). The fact that LTβ protein can be detected in whole cell extracts prepared from resting PBMCs (V.E.B., unpublished observation, May 1999), but could not be detected on the cell surface,9 supports the notion that LTβ cannot be transported to the membrane surface without LTα. Taken together, these data suggest that activation of LTα transcription may be the rate-limiting step in the overall process of surface expression of LTα/β complexes on PMA/ionomycin-activated PBMCs. It is worth noting that LTβ expression in established human T-cell lines, such as MOLT-4 and Jurkat, shows an expression pattern different from that observed here for PBMCs,23 thus implying deregulation of intracellular signaling pathways affecting LTβ expression in established T-cell lines. Therefore, established cell lines may have serious limitations as model systems to study cytokine gene transcription.
To evaluate the physiologic relevance of our initial finding concerning activated LTα expression, we performed PBMC activation using anti-CD3 and anti-CD28 antibodies, which mimic physiologic activation of T cells. As expected, we found that receptor cross-linking with these 2 antibodies acted synergistically to activate LTα expression in PBMCs, and that this activation was effectively blocked by CsA (Figure 2). These findings suggest that triggering TCR and CD28 in PBMCs can activate the LTα gene in T lymphocytes in a calcium-dependent manner and that intracellular calcium balance critically controls the expression of cell-bound LT heterotrimers and therefore subsequent signaling mediated by LTβR.
The promoter regions of the LTA and LTB genes have been previously characterized35,46-49 and both are known to contain functional NFκB sites.35,48-50Sensitivity to CsA of transcriptional induction of LTα strongly suggests a possible role of NFAT transcription factors, known to be regulated via the phosphatase calcineurin.39 Indeed, we have identified a novel NFAT-binding site position −490 in the human LTα promoter and demonstrated by electrophoretic mobility shift assay CsA-sensitive PMA/ionomycin-inducible DNA binding (Figure 4B). NFAT4 appears to be the predominant NFAT-binding sequence within the human LTα promoter and, as such, is the primary candidate as the CsA-responsive element in the LTα transcription mechanism. Further studies will be necessary to assess the role of the NFAT4 site in the context of the complete LTα promoter on LTα transcription. Several distinct functional elements within the LTα promoter have been previously identified in studies using T cells35,48 and B cells.50 Most likely, the specificity of LTα transcriptional activation in PBMCs, including CsA dependence, relies on the unique combination of several transcriptional factors, similar to other genes such as interleukin 2 (IL-2).51
Previous studies of LTα transcription in T-cell lines suggested a general role for NFκB in LTα transcriptional regulation.34-37 However, we did not observe any appreciable binding to the NFκB site from the LTα promoter in our experimental system (Figure 4C), arguing against the involvement of NFκB into the regulation of CsA-sensitive LTα transcription in PMBCs. On the other hand, we cannot rule out the possibility that NFκB may play a role via association with other transcription factors.
Another potential mechanism may act at the posttranscriptional level through the AU-rich motif found in the 3′ untranslated regions (UTRs) of many short-lived mRNAs.46,52,53 This motif is present in the 3′-UTRs of the TNFA and LTA genes but is lacking in the LTB gene.8,29 54 It was reported that CsA can destabilize IL-3 mRNA acting through the AU-rich motif from the IL-3 3′-UTR52 by unknown mechanism, but presumably by regulating expression of AU-RNA–binding proteins. It is conceivable that in addition to the effects on transcriptional initiation, CsA may contribute to down-regulation of LTα mRNA through the 3′-UTR.
In conclusion, our data on the CsA sensitivity of LTα synthesis suggest that the downstream effects mediated by LTβR signaling may constitute a previously unrecognized component of immunosuppression in patients undergoing treatment after organ transplantation. Supporting this notion is the observation that injection of mice with CsA, in addition to drastic effects on the thymus, results in reduction of germinal centers, histologic abnormalities in spleen and lymph nodes and reduction of antigen-specific IgG responses without gross effect on the overall Ig responses.55 Even though the effects of CsA in spleen may be partly mediated by CD40 inhibition, some of these features are reminiscent of the effects caused by biochemical inactivation of membrane LT signaling.14 15
We are grateful to Drs J. Browning (Biogen, Cambridge, MA) and U. Christians (Institute for Pharmacology, Hannover Medical School) for generous gift of reagents. We thank Drs J. J. Oppenheim, W. J. Murphy (NCI Frederick), H.-G. Rammensee (University of Tübingen), B. Ryffel (CNRI, Orleans, France), and M. A. Lagarkova (Moscow State University) for critically reading this manuscript.
Supported by the VW Foundation (Hanover, Germany). This project has been funded in part with federal funds from the National Cancer Institute, National Institutes of Health (contract no. N01-CO-124000) and by Russian State Program “Human Genome.” S.A.N. is an International Research Scholar of the Howard Hughes Research Institute.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Sergei Nedospasov, Engelhardt Institute of Molecular Biology, 32 Vavilov St, 119991, Moscow, Russia; e-mail:snedos@online.ru.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal