Abstract
The excess risk of second malignancy after Hodgkin disease is an increasing problem. In light of the long-term data, guidelines for follow-up of survivors of Hodgkin disease need to be redefined. In this study we attempt to analyze the long-term risks and temporal trends, identify patient- and treatment-related risk factors, and determine the prognosis of patients who develop a second malignancy after radiation treatment with or without chemotherapy for Hodgkin disease. Among 1319 patients with clinical stage I-IV Hodgkin disease, 181 second malignancies and 18 third malignancies were observed. With a median follow-up of 12 years, the relative risk (RR) and absolute excess risk of second malignancy were 4.6 and 89.3/10 000 person-years. The RR was significantly higher with combined chemotherapy and radiation therapy (6.1) than with radiation therapy alone (4.0, P = .015). The risk increased with increasing radiation field size (P = .03) in patients who received combined modality therapy, and with time after Hodgkin disease. After 15 and 20 years, there was a 2.3% and 4.0% excess risk of second malignancy per person per year. The 5-year survival after development of a second malignancy was 38.1%, with the worst prognosis seen after acute leukemia and lung cancer. The excess risk of second malignancy after Hodgkin disease continues to be increased after 15 to 20 years, and there does not appear to be a plateau. Our analysis suggests that the risk may be reduced with smaller radiation fields, as are used in current trials of abbreviated chemotherapy and limited-field radiation therapy.
Introduction
Second malignancy after Hodgkin disease was first recognized as a problem in the early 1970s.1-3 Our understanding of this serious late effect has evolved over time. Many early studies reported an increased risk of acute leukemia, which has a shorter latency and is associated with the use of alkylating chemotherapy.1,2,4-11 In more recent years, solid tumors, often taking 15 or more years to develop, have emerged as the most significant subtype of second malignancy and account for the majority of cases.12-19 Increasing attention is being directed to the more common individual tumor types, including lung cancer20-23 and breast cancer,24-27 in an attempt to better understand and perhaps modify the risk and impact of the different specific malignancies.
A number of studies have shown that second malignancy represents the leading cause of excess mortality in survivors of Hodgkin disease.28-32 As follow-up time increases, as the number of survivors accumulates, and as the treatment for Hodgkin disease changes, continued efforts to further our knowledge about the magnitude of the risk, temporal trend, and outcome of patients after a second malignancy are important. Understanding the treatment-related risk factors and time to development of second tumors may have important implications for the design of future trials for treatment, for the follow-up of patients, and for the identification of a high-risk population that might benefit from more intensive screening and preventative programs.
We previously published results from our institution on second malignancy after Hodgkin disease in 794 patients with pathologic stage I-III disease.33 We have now expanded the study to include patients of all clinical and pathologic stages treated over a longer period. This updated report contains twice the number of person-years of follow-up of our last publication. In this study, we focus on the types, temporal trends, risk factors, and prognosis of second malignancy after Hodgkin disease, with particular attention on very late effects. The patients in the current study were drawn predominantly from those seen in consultation at the Departments of Radiation Oncology at the Brigham and Women's Hospital, Dana-Farber Cancer Institute, Children's Hospital, and Beth Israel Deaconess Medical Center, Boston, MA; the majority initially presented with early-stage disease, and most received radiation therapy alone or combined chemotherapy and radiation therapy. The number of patients who received chemotherapy alone was relatively small, and such patients were thus excluded from the study.
Patients, materials, and methods
Patient characteristics, staging, and treatment
Between April 1969 and December 1997, 1319 patients with clinical stage IA-IVB Hodgkin disease were treated at one of the following Harvard-affiliated hospitals: Brigham and Women's Hospital, Dana-Farber Cancer Institute, Children's Hospital, or Beth Israel Deaconess Medical Center. Patient characteristics are described in Table 1. Fifty-five percent of patients were male. Median age at presentation was 25 years. Histologic classification for all patients was confirmed by hematopathologists at the treating hospital. All patients underwent clinical staging with history and physical examination, chest radiography, complete blood counts, and chemistry. The choice of studies in the staging work-up was influenced by the development of new studies (computed tomography,26 gallium scans), phasing out of old studies (lymphangiography), and a gradual change in recommendations for staging over time (less frequent staging laparotomy and fewer bone marrow biopsies for early-stage disease). In this study, 85% of patients presented with clinical stage I-II disease. Among the 964 patients (73%) who underwent staging laparotomy, 77% had pathologic stage I-II disease and 23% had pathologic stage III-IV disease. In the analysis of surgical staging versus clinical staging, only the 961 patients with more than 10 years of potential follow-up were included, to minimize the differences in lengths of follow-up time between the 2 cohorts of patients.
Patient characteristics of all 1319 patients
| . | No. . | (%) . |
|---|---|---|
| Age at diagnosis (y) | ||
| Mean | 28 | |
| Median | 25 | |
| Range | 3-93 | |
| Younger than 20 | 380 | (28.8) |
| 20 to 50 | 832 | (63.1) |
| Older than 50 | 107 | (8.1) |
| Sex | ||
| Male | 728 | (55.2) |
| Female | 591 | (44.8) |
| Clinical stage | ||
| I | 321 | (24.3) |
| II | 807 | (61.2) |
| III | 138 | (10.5) |
| IV | 53 | (4.0) |
| Laparotomy | ||
| Yes | 964 | (73.1) |
| No | 355 | (26.9) |
| . | No. . | (%) . |
|---|---|---|
| Age at diagnosis (y) | ||
| Mean | 28 | |
| Median | 25 | |
| Range | 3-93 | |
| Younger than 20 | 380 | (28.8) |
| 20 to 50 | 832 | (63.1) |
| Older than 50 | 107 | (8.1) |
| Sex | ||
| Male | 728 | (55.2) |
| Female | 591 | (44.8) |
| Clinical stage | ||
| I | 321 | (24.3) |
| II | 807 | (61.2) |
| III | 138 | (10.5) |
| IV | 53 | (4.0) |
| Laparotomy | ||
| Yes | 964 | (73.1) |
| No | 355 | (26.9) |
Initial treatment choices also evolved over time, with earlier patients treated predominantly with radiation therapy alone, and more recent patients treated with combined modality therapy (CMT). As in the analysis of staging methods, only the 961 patients with more than 10 years of potential follow-up were included in the analysis of treatment parameters. Among these 961 patients, initial treatment included radiation therapy alone in 665 patients and CMT in 296 patients. The radiation fields included total nodal irradiation (TNI) in 13% of patients, mantle and paraaortic (MPA) in 66%, mantle alone in 17%, and pelvic and paraaortic (PPA) in 3%. The median dose to the mantle field was 3605 cGy, with a boost to bulk disease to a median total dose of 4000 cGy. Daily fractions ranged from 150 cGy to 200 cGy, 5 days per week. Technical factors included the use of individualized divergent blocks, equal treatment from anterior and posterior fields, the addition of a larynx block at 2000 cGy, and the addition of a posterior cervical spine block at 3000 cGy. Among the 296 patients who received CMT, chemotherapy included mechlorethamine, vincristine, procarbazine, and prednisone (MOPP) in 253 patients (85%); doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) in 15 patients (5%); alternating or hybrid MOPP/ABVD in 4 patients (1%); chlorambucil, vinblastine, procarbazine, and prednisone (ChlVPP) in 7 patients (2%); cyclophosphamide, vincristine, procarbazine, and prednisone (COPP) or cyclophosphamide, vinblastine, procarbazine, and prednisone (CVPP) in 6 patients (2%); and other chemotherapy regimens in 11 patients (4%). A total of 213 patients developed a relapse and received further salvage therapy, with 173 patients relapsing after initial radiation therapy alone and 40 patients after initial CMT. Treatment at first relapse included MOPP in 99 patients (46%), ABVD in 33 (15%), etoposide, vinblastine, and doxorubicin (EVA) in 11 (5%), other chemotherapy alone in 32 (15%), CMT in 22 (10%), radiation therapy alone in 11 (5%), high-dose therapy with stem cell rescue in 3 (2%), and unknown in 2 patients (1%).
Follow-up data on disease status, second and third malignancies, and causes of death were ascertained through review of medical records, contact of physicians following the patients, and contact of patients or family members. Information obtained from patients and family members was verified by review of relevant medical reports.
Statistical analysis
Relative risks (RRs; ratio of observed to expected number of cases) were analyzed by sex, age at diagnosis, treatment, and time interval since treatment. RRs were estimated based on the assumption that the observed number of second cancers followed a Poisson distribution. Confidence intervals for RR were obtained using exact Poisson probabilities. Chi-square tests were used to compare the RR of second malignancy between groups. All P values are 2-sided. Absolute excess risk (AR) was calculated by dividing observed minus expected numbers of cases by the person-years at risk. The result was multiplied by 10 000 and expressed as the excess number of cases of second malignancy per 10 000 person-years. Dividing the AR by 100 gives the average percent excess second malignancy risk per year per patient. To obtain the expected number of second malignancies, age- and sex-specific incidence rates from Surveillance Epidemiology and End Results (SEER) data were multiplied by corresponding person-years of observation. Person-years of observation began at the end of initial treatment for Hodgkin disease and continued until death or last day of follow-up. In the analyses of RR and AR of second malignancy by staging methods and by treatment exposure, only patients with more than 10 years of potential follow-up were included.
Survival curves for the time to the development of a second tumor were calculated by the Kaplan-Meier method. The cumulative incidence of observed second malignancies was estimated using Gray's method,34 while the cumulative risk function for the expected number of second malignancies was determined using the life-table method.35
Results
At the time of this analysis, the median follow-up time among survivors was 12 years, with 416 patients (32%) having more than 15 years and 229 patients (17%) having more than 20 years of follow-up. The total number of person-years of follow-up was 15 910. Only 45 patients (3.4%) were lost to follow-up. Patient characteristics are described in Table 1.
The 15- and 20-year cumulative incidence rates of second malignancy were 14% and 23%, respectively. Figure1 shows the overall cumulative incidence of second malignancy in the study population and the expected cumulative incidence in an age- and sex-matched population over time. A total of 181 second malignancies were observed (excluding nonmelanoma skin cancers and carcinoma in situ of the cervix). Twenty-three patients developed acute leukemia, 24 had non-Hodgkin lymphoma, 3 developed multiple myeloma, and 131 developed solid tumors. The median times to development of leukemia, non-Hodgkin lymphoma, and solid tumors were 5.3, 7.1, and 13.8 years, respectively, among patients who developed these second tumors.
Cumulative incidence of observed second tumors in survivors of Hodgkin disease and expected tumors in a matched population.
Cumulative incidence of observed second tumors in survivors of Hodgkin disease and expected tumors in a matched population.
The RR and AR of second malignancy were 4.6 and 89.3/10 000 person years (9% excess risk per person per decade of follow-up), respectively. Table 2 shows the RR and AR of second malignancy by sites. The RR of acute leukemia, non-Hodgkin lymphoma, and solid tumors was significantly elevated at 82.5, 16.5, and 3.5, respectively. The corresponding AR was 14.3, 14.2, and 59.1/10 000 person-years, respectively. Because of the low background risk of leukemia, the RR was high despite the relatively low AR. In contrast, because of the higher background risk of solid tumor, only a modest RR was observed, but the AR was high. The 5 most common malignancies after Hodgkin disease were breast cancer, lung cancer, acute leukemia, non-Hodgkin lymphoma, and gastrointestinal cancer. Other tumors with significantly increased RR included sarcoma, head and neck cancer, melanoma, thyroid cancer, and multiple myeloma.
RR and AR of second malignancies by sites in all 1319 patients
| Second malignancy . | O . | E . | RR . | (95% CI) . | AR . |
|---|---|---|---|---|---|
| All sites | 181 | 38.97 | 4.6 | (4.0, 5.4) | 89.3 |
| Acute leukemia | 23 | 0.28 | 82.5 | (53.5, 122.2) | 14.3 |
| Non-Hodgkin lymphoma | 24 | 1.46 | 16.5 | (10.2, 23.8) | 14.2 |
| Multiple myeloma | 3 | 0.32 | 9.4 | (1.9, 27.4) | 1.7 |
| Solid tumors | 131 | 36.91 | 3.5 | (3.0, 4.2) | 59.1 |
| Breast | 39 | 5.83 | 6.7 | (4.8, 8.9) | 20.8 |
| Lung | 22 | 4.53 | 4.9 | (3.0, 7.1) | 11.0 |
| Gastrointestinal | 24 | 5.96 | 4.0 | (2.5, 5.8) | 11.3 |
| Sarcoma | 11 | 0.41 | 26.6 | (13.3, 47.6) | 6.7 |
| Genitourinary | 11 | 6.07 | 1.8 | (0.9, 3.2) | 3.1 |
| Head and neck | 7 | 1.75 | 4.0 | (1.6, 8.2) | 3.3 |
| Melanoma | 7 | 2.14 | 3.3 | (1.3, 6.7) | 3.1 |
| Thyroid | 5 | 0.89 | 5.6 | (1.8, 13.0) | 2.6 |
| Gynecological | 4 | 8.58 | 0.5 | (0.1, 1.2) | − 2.9 |
| Central nervous system | 1 | 0.74 | 1.4 | (0.04, 7.5) | 0.2 |
| Second malignancy . | O . | E . | RR . | (95% CI) . | AR . |
|---|---|---|---|---|---|
| All sites | 181 | 38.97 | 4.6 | (4.0, 5.4) | 89.3 |
| Acute leukemia | 23 | 0.28 | 82.5 | (53.5, 122.2) | 14.3 |
| Non-Hodgkin lymphoma | 24 | 1.46 | 16.5 | (10.2, 23.8) | 14.2 |
| Multiple myeloma | 3 | 0.32 | 9.4 | (1.9, 27.4) | 1.7 |
| Solid tumors | 131 | 36.91 | 3.5 | (3.0, 4.2) | 59.1 |
| Breast | 39 | 5.83 | 6.7 | (4.8, 8.9) | 20.8 |
| Lung | 22 | 4.53 | 4.9 | (3.0, 7.1) | 11.0 |
| Gastrointestinal | 24 | 5.96 | 4.0 | (2.5, 5.8) | 11.3 |
| Sarcoma | 11 | 0.41 | 26.6 | (13.3, 47.6) | 6.7 |
| Genitourinary | 11 | 6.07 | 1.8 | (0.9, 3.2) | 3.1 |
| Head and neck | 7 | 1.75 | 4.0 | (1.6, 8.2) | 3.3 |
| Melanoma | 7 | 2.14 | 3.3 | (1.3, 6.7) | 3.1 |
| Thyroid | 5 | 0.89 | 5.6 | (1.8, 13.0) | 2.6 |
| Gynecological | 4 | 8.58 | 0.5 | (0.1, 1.2) | − 2.9 |
| Central nervous system | 1 | 0.74 | 1.4 | (0.04, 7.5) | 0.2 |
O indicates observed; E, expected; RR, relative risk; CI, confidence interval; AR, absolute excess risk.
Table 3 shows the excess risk of second malignancy by sex and age at diagnosis of Hodgkin disease. The difference in RR of second malignancy was not significantly different according to sex (P = .68). The RR of developing a second malignancy decreased significantly with age at diagnosis from 10.7 (< 20 years old) to 4.9 (20 to 50 years old) to 2.4 (> 50 years old) (P < .0001). However, the AR for the 3 age groups increased with increasing age and were 71.0, 88.5, and 211.0/10 000 person-years, respectively. This is because of the higher expected incidence of cancer with increasing age. The excess risk of breast cancer by age was also examined separately (Table4). There was a continuous downward trend in the RR of breast cancer as age at diagnosis of Hodgkin disease increased. The RR of breast cancer was significantly increased in women diagnosed with Hodgkin disease when younger than 30 years of age. The increase in RR of breast cancer was of borderline significance in women diagnosed between age 30 and 35 years. After age 35, the RR was not significantly increased.
RR and AR of second malignancy by age and sex in all 1319 patients
| . | No. . | Person-years . | O . | E . | RR . | (95% CI) . | AR . |
|---|---|---|---|---|---|---|---|
| Age at diagnosis | |||||||
| Younger than 20 | 380 | 5112 | 40 | 3.7 | 10.7 | (7.8, 14.4) | 71.0 |
| 20-50 | 832 | 9964 | 111 | 22.8 | 4.9 | (4.0, 5.9) | 88.5 |
| Older than 50 | 107 | 834 | 30 | 12.4 | 2.4 | (1.6, 3.4) | 211.0 |
| Sex | |||||||
| Female | 591 | 7118 | 102 | 21.3 | 4.8 | (4.0, 5.8) | 113.4 |
| Male | 728 | 8792 | 79 | 17.7 | 4.5 | (3.6, 5.6) | 70.0 |
| . | No. . | Person-years . | O . | E . | RR . | (95% CI) . | AR . |
|---|---|---|---|---|---|---|---|
| Age at diagnosis | |||||||
| Younger than 20 | 380 | 5112 | 40 | 3.7 | 10.7 | (7.8, 14.4) | 71.0 |
| 20-50 | 832 | 9964 | 111 | 22.8 | 4.9 | (4.0, 5.9) | 88.5 |
| Older than 50 | 107 | 834 | 30 | 12.4 | 2.4 | (1.6, 3.4) | 211.0 |
| Sex | |||||||
| Female | 591 | 7118 | 102 | 21.3 | 4.8 | (4.0, 5.8) | 113.4 |
| Male | 728 | 8792 | 79 | 17.7 | 4.5 | (3.6, 5.6) | 70.0 |
O indicates observed; E, expected; RR, relative risk; CI, confidence interval; AR, absolute excess risk.
RR and AR of breast cancer by age at diagnosis of Hodgkin disease
| Age at diagnosis . | Person-years . | O . | E . | RR . | (95% CI) . | AR . |
|---|---|---|---|---|---|---|
| Younger than 15 | 604 | 5 | 0.04 | 111.8 | (36.2, 261.0) | 82.1 |
| 15-19 | 1498 | 9 | 0.28 | 32.0 | (14.6, 60.7) | 58.2 |
| 20-25 | 1781 | 10 | 0.60 | 16.6 | (8.0, 30.6) | 52.8 |
| 26-29 | 1232 | 8 | 0.96 | 8.4 | (3.6, 16.5) | 57.2 |
| 30-35 | 950 | 4 | 1.07 | 3.7 | (1.0, 9.5) | 30.8 |
| 36-40 | 355 | 2 | 0.60 | 3.4 | (0.4, 12.1) | 39.6 |
| Older than 40 | 699 | 1 | 2.23 | 0.4 | (0.01, 2.5) | − 17.7 |
| Age at diagnosis . | Person-years . | O . | E . | RR . | (95% CI) . | AR . |
|---|---|---|---|---|---|---|
| Younger than 15 | 604 | 5 | 0.04 | 111.8 | (36.2, 261.0) | 82.1 |
| 15-19 | 1498 | 9 | 0.28 | 32.0 | (14.6, 60.7) | 58.2 |
| 20-25 | 1781 | 10 | 0.60 | 16.6 | (8.0, 30.6) | 52.8 |
| 26-29 | 1232 | 8 | 0.96 | 8.4 | (3.6, 16.5) | 57.2 |
| 30-35 | 950 | 4 | 1.07 | 3.7 | (1.0, 9.5) | 30.8 |
| 36-40 | 355 | 2 | 0.60 | 3.4 | (0.4, 12.1) | 39.6 |
| Older than 40 | 699 | 1 | 2.23 | 0.4 | (0.01, 2.5) | − 17.7 |
O indicates observed; E, expected; RR, relative risk; CI, confidence interval; AR, absolute excess risk.
Table 5 shows the RR and AR by 5-year intervals of follow-up of all malignancies, of the 3 major subtypes (acute leukemia, non-Hodgkin lymphoma, and solid tumors), and of the most common subtypes of solid tumors. For all second malignancies combined, the RR was significantly elevated in each time interval considered, and both the RR and AR increased with increasing follow-up time. For acute leukemia, the majority of the cases were observed in the first 10 years, although 2 of the cases occurred after 20 years. No clear pattern emerged in terms of length of follow-up in the excess risk of non-Hodgkin lymphoma, but its RR remained significantly increased more than 20 years after diagnosis of Hodgkin disease. In the first 10 years, approximately half of the cases of second malignancies were solid tumors. However, after 10 years, 85% of second malignancies observed were solid tumors. For lung cancer, the RR was significantly increased after 5 years of follow-up. For breast cancer, the RR was significantly increased after a latency of 10 to 15 years, with the greatest increases seen after 15 years. The RR of gastrointestinal cancer became significantly increased after 15 years of follow-up. Breast cancer was the most common second malignancy in our cohort of patients, with the excess risk being the highest among women diagnosed with and irradiated for Hodgkin disease at a younger age. To focus on this higher risk group, we analyzed the RR and AR of breast cancer by follow-up interval, limiting the analysis to only the 397 women treated with radiation therapy (mantle, MPA, or TNI) at or before age 30. The results are displayed in Table 6. A trend similar to that found in the whole group was noted in this subgroup, with increasing excess risk with increasing follow-up time. However, the increase in RR of breast cancer in this group of patients did not reach significance until after 15 years.
RR and AR of second malignancy by follow-up interval in all 1319 patients
| Intervals . | Person-years . | O . | E . | RR . | (95% CI) . | AR . |
|---|---|---|---|---|---|---|
| All sites | ||||||
| 0-5 | 5846 | 24 | 11.0 | 2.2 | (1.4, 3.1) | 22.2 |
| 5-10 | 4303 | 33 | 9.7 | 3.4 | (2.4, 4.7) | 54.2 |
| 10-15 | 3002 | 33 | 8.2 | 4.0 | (2.8, 5.5) | 82.5 |
| 15-20 | 1751 | 46 | 5.9 | 7.8 | (5.8, 10.3) | 229.2 |
| 20+ | 1009 | 45 | 4.1 | 10.9 | (7.8, 14.2) | 404.7 |
| Acute leukemia | ||||||
| 0-5 | 5846 | 11 | 0.09 | 128.0 | (63.9, 229.0) | 18.7 |
| 5-10 | 4303 | 7 | 0.07 | 100.3 | (40.3, 206.6) | 16.1 |
| 10-15 | 3002 | 3 | 0.06 | 52.8 | (10.9, 154.3) | 9.8 |
| 15-20 | 1751 | 0 | 0.04 | 0 | (0.0, 93.8) | − 0.2 |
| 20+ | 1009 | 2 | 0.03 | 74.8 | (9.0, 269.9) | 19.5 |
| NHL | ||||||
| 0-5 | 5846 | 5 | 0.41 | 12.2 | (4.0, 28.5) | 7.9 |
| 5-10 | 4303 | 8 | 0.35 | 22.5 | (9.7, 44.4) | 17.8 |
| 10-15 | 3002 | 2 | 0.31 | 6.4 | (0.8, 23.3) | 5.6 |
| 15-20 | 1751 | 2 | 0.22 | 8.9 | (1.7, 32.2) | 10.1 |
| 20+ | 1009 | 7 | 0.16 | 44.3 | (17.8, 91.3) | 67.8 |
| Solid tumors | ||||||
| 0-5 | 5846 | 7 | 10.5 | 0.7 | (0.3, 1.4) | − 5.9 |
| 5-10 | 4303 | 18 | 9.17 | 2.0 | (1.2, 3.1) | 20.5 |
| 10-15 | 3002 | 27 | 7.81 | 3.5 | (2.3, 4.9) | 63.9 |
| 15-20 | 1751 | 43 | 5.55 | 7.7 | (5.7, 10.3) | 213.9 |
| 20+ | 1009 | 36 | 3.92 | 9.2 | (6.5, 12.4) | 317.8 |
| Breast cancer (females only) | ||||||
| 0-5 | 2640 | 0 | 1.43 | 0 | (0.0, 2.6) | − 5.4 |
| 5-10 | 1962 | 3 | 1.32 | 2.3 | (0.5, 6.6) | 8.5 |
| 10-15 | 1342 | 5 | 1.29 | 3.9 | (1.3, 9.1) | 27.7 |
| 15-20 | 754 | 16 | 1.0 | 16.1 | (9.2, 26.1) | 198.9 |
| 20+ | 421 | 15 | 0.75 | 20.1 | (11.3, 33.2) | 338.4 |
| Lung cancer | ||||||
| 0-5 | 5846 | 0 | 1.19 | 0 | (0.0, 3.1) | − 2.0 |
| 5-10 | 4303 | 4 | 1.04 | 3.8 | (1.0, 9.8) | 6.9 |
| 10-15 | 3002 | 5 | 0.95 | 5.2 | (1.7, 12.2) | 13.5 |
| 15-20 | 1751 | 6 | 0.75 | 8.0 | (2.9, 17.3) | 30.0 |
| 20+ | 1009 | 7 | 0.59 | 11.9 | (4.8, 24.5) | 63.5 |
| GI cancer | ||||||
| 0-5 | 5846 | 4 | 1.62 | 2.5 | (0.7, 6.4) | 4.1 |
| 5-10 | 4303 | 4 | 1.39 | 2.9 | (0.8, 7.4) | 6.1 |
| 10-15 | 3002 | 3 | 1.27 | 2.4 | (0.5, 6.9) | 5.8 |
| 15-20 | 1751 | 7 | 0.97 | 7.2 | (2.9, 14.9) | 34.4 |
| 20+ | 1009 | 6 | 0.72 | 8.3 | (3.1, 18.1) | 52.3 |
| Intervals . | Person-years . | O . | E . | RR . | (95% CI) . | AR . |
|---|---|---|---|---|---|---|
| All sites | ||||||
| 0-5 | 5846 | 24 | 11.0 | 2.2 | (1.4, 3.1) | 22.2 |
| 5-10 | 4303 | 33 | 9.7 | 3.4 | (2.4, 4.7) | 54.2 |
| 10-15 | 3002 | 33 | 8.2 | 4.0 | (2.8, 5.5) | 82.5 |
| 15-20 | 1751 | 46 | 5.9 | 7.8 | (5.8, 10.3) | 229.2 |
| 20+ | 1009 | 45 | 4.1 | 10.9 | (7.8, 14.2) | 404.7 |
| Acute leukemia | ||||||
| 0-5 | 5846 | 11 | 0.09 | 128.0 | (63.9, 229.0) | 18.7 |
| 5-10 | 4303 | 7 | 0.07 | 100.3 | (40.3, 206.6) | 16.1 |
| 10-15 | 3002 | 3 | 0.06 | 52.8 | (10.9, 154.3) | 9.8 |
| 15-20 | 1751 | 0 | 0.04 | 0 | (0.0, 93.8) | − 0.2 |
| 20+ | 1009 | 2 | 0.03 | 74.8 | (9.0, 269.9) | 19.5 |
| NHL | ||||||
| 0-5 | 5846 | 5 | 0.41 | 12.2 | (4.0, 28.5) | 7.9 |
| 5-10 | 4303 | 8 | 0.35 | 22.5 | (9.7, 44.4) | 17.8 |
| 10-15 | 3002 | 2 | 0.31 | 6.4 | (0.8, 23.3) | 5.6 |
| 15-20 | 1751 | 2 | 0.22 | 8.9 | (1.7, 32.2) | 10.1 |
| 20+ | 1009 | 7 | 0.16 | 44.3 | (17.8, 91.3) | 67.8 |
| Solid tumors | ||||||
| 0-5 | 5846 | 7 | 10.5 | 0.7 | (0.3, 1.4) | − 5.9 |
| 5-10 | 4303 | 18 | 9.17 | 2.0 | (1.2, 3.1) | 20.5 |
| 10-15 | 3002 | 27 | 7.81 | 3.5 | (2.3, 4.9) | 63.9 |
| 15-20 | 1751 | 43 | 5.55 | 7.7 | (5.7, 10.3) | 213.9 |
| 20+ | 1009 | 36 | 3.92 | 9.2 | (6.5, 12.4) | 317.8 |
| Breast cancer (females only) | ||||||
| 0-5 | 2640 | 0 | 1.43 | 0 | (0.0, 2.6) | − 5.4 |
| 5-10 | 1962 | 3 | 1.32 | 2.3 | (0.5, 6.6) | 8.5 |
| 10-15 | 1342 | 5 | 1.29 | 3.9 | (1.3, 9.1) | 27.7 |
| 15-20 | 754 | 16 | 1.0 | 16.1 | (9.2, 26.1) | 198.9 |
| 20+ | 421 | 15 | 0.75 | 20.1 | (11.3, 33.2) | 338.4 |
| Lung cancer | ||||||
| 0-5 | 5846 | 0 | 1.19 | 0 | (0.0, 3.1) | − 2.0 |
| 5-10 | 4303 | 4 | 1.04 | 3.8 | (1.0, 9.8) | 6.9 |
| 10-15 | 3002 | 5 | 0.95 | 5.2 | (1.7, 12.2) | 13.5 |
| 15-20 | 1751 | 6 | 0.75 | 8.0 | (2.9, 17.3) | 30.0 |
| 20+ | 1009 | 7 | 0.59 | 11.9 | (4.8, 24.5) | 63.5 |
| GI cancer | ||||||
| 0-5 | 5846 | 4 | 1.62 | 2.5 | (0.7, 6.4) | 4.1 |
| 5-10 | 4303 | 4 | 1.39 | 2.9 | (0.8, 7.4) | 6.1 |
| 10-15 | 3002 | 3 | 1.27 | 2.4 | (0.5, 6.9) | 5.8 |
| 15-20 | 1751 | 7 | 0.97 | 7.2 | (2.9, 14.9) | 34.4 |
| 20+ | 1009 | 6 | 0.72 | 8.3 | (3.1, 18.1) | 52.3 |
O indicates observed; E, expected; RR, relative risk; CI, confidence interval; AR, absolute excess risk; NHL, non-Hodgkin lymphoma; GI, gastrointestinal.
RR and AR of breast cancer by follow-up interval among women who received mantle, MPA, or TNI at age 30 years or younger
| Intervals . | Person-years . | O . | E . | RR . | (95% CI) . | AR . |
|---|---|---|---|---|---|---|
| Overall | 5231 | 32 | 2.0 | 15.9 | (10.6, 22.0) | 57.3 |
| 0-5 | 1800 | 0 | 0.1 | 0.0 | (0.0, 30.0) | − 0.7 |
| 5-10 | 1443 | 2 | 0.3 | 6.8 | (0.8, 24.7) | 11.8 |
| 10-15 | 1026 | 2 | 0.5 | 4.1 | (0.5, 14.9) | 14.8 |
| 15-20 | 598 | 14 | 0.5 | 25.8 | (14.1, 43.3) | 225.0 |
| 20+ | 365 | 14 | 0.6 | 24.5 | (13.4, 41.1) | 368.2 |
| Intervals . | Person-years . | O . | E . | RR . | (95% CI) . | AR . |
|---|---|---|---|---|---|---|
| Overall | 5231 | 32 | 2.0 | 15.9 | (10.6, 22.0) | 57.3 |
| 0-5 | 1800 | 0 | 0.1 | 0.0 | (0.0, 30.0) | − 0.7 |
| 5-10 | 1443 | 2 | 0.3 | 6.8 | (0.8, 24.7) | 11.8 |
| 10-15 | 1026 | 2 | 0.5 | 4.1 | (0.5, 14.9) | 14.8 |
| 15-20 | 598 | 14 | 0.5 | 25.8 | (14.1, 43.3) | 225.0 |
| 20+ | 365 | 14 | 0.6 | 24.5 | (13.4, 41.1) | 368.2 |
RR indicates relative risk; AR, absolute excess risk; MPA, mantle and paraaortic; TNI, total nodal irradiation; O, observed; E, expected; CI, confidence interval.
In the analysis of the excess risks of second malignancy according to whether or not staging laparotomy was performed (Table7), treatment exposure based on radiation therapy with or without chemotherapy (Table8), and radiation field size (Table9), only the 961 patients with 10 or more years of follow-up were included.
RR and AR of second malignancy by staging in the 961 patients with more than 10 years of potential follow-up
| Staging laparotomy . | Person-years . | O . | E . | RR . | (95% CI) . | AR . |
|---|---|---|---|---|---|---|
| No | 1 480 | 18 | 6.4 | 2.8 | (1.7, 4.5) | 78.6 |
| Yes | 12 868 | 144 | 29.2 | 4.9 | (4.2, 5.8) | 89.2 |
| Staging laparotomy . | Person-years . | O . | E . | RR . | (95% CI) . | AR . |
|---|---|---|---|---|---|---|
| No | 1 480 | 18 | 6.4 | 2.8 | (1.7, 4.5) | 78.6 |
| Yes | 12 868 | 144 | 29.2 | 4.9 | (4.2, 5.8) | 89.2 |
O indicates observed; E, expected; CI, confidence interval; AR, absolute excess risk.
RR and AR of second malignancy by overall treatment exposure in 961 patients with more than 10 years of potential follow-up
| Initial therapy . | No. . | PY . | O . | E . | RR . | (95% CI) . | AR . |
|---|---|---|---|---|---|---|---|
| All patients | |||||||
| CMT8-150 | 296 | 4 046 | 53 | 8.6 | 6.18-151 | (4.7, 8.0) | 109.7 |
| RT | 665 | 10 302 | 109 | 26.9 | 4.08-151 | (3.4, 4.9) | 79.6 |
| Nonrelapsed cases | |||||||
| CMT | 256 | 3 739 | 48 | 8.2 | 5.98-152 | (4.2, 7.7) | 106.5 |
| RT | 492 | 7 997 | 79 | 21.2 | 3.78-152 | (3.0, 4.6) | 72.3 |
| Relapsed cases | |||||||
| Relapsed after CMT | 40 | 307 | 5 | 0.4 | 11.38-153 | (3.7, 26.3) | 148.2 |
| Relapsed after RT | 173 | 2 305 | 30 | 5.8 | 5.28-153 | (3.5, 7.2) | 105.1 |
| Initial therapy . | No. . | PY . | O . | E . | RR . | (95% CI) . | AR . |
|---|---|---|---|---|---|---|---|
| All patients | |||||||
| CMT8-150 | 296 | 4 046 | 53 | 8.6 | 6.18-151 | (4.7, 8.0) | 109.7 |
| RT | 665 | 10 302 | 109 | 26.9 | 4.08-151 | (3.4, 4.9) | 79.6 |
| Nonrelapsed cases | |||||||
| CMT | 256 | 3 739 | 48 | 8.2 | 5.98-152 | (4.2, 7.7) | 106.5 |
| RT | 492 | 7 997 | 79 | 21.2 | 3.78-152 | (3.0, 4.6) | 72.3 |
| Relapsed cases | |||||||
| Relapsed after CMT | 40 | 307 | 5 | 0.4 | 11.38-153 | (3.7, 26.3) | 148.2 |
| Relapsed after RT | 173 | 2 305 | 30 | 5.8 | 5.28-153 | (3.5, 7.2) | 105.1 |
PY indicates person-years; O, observed; E, expected; RR, relative risk; CI, confidence interval; AR, absolute excess risk; CMT, combined modality therapy; RT, radiation therapy.
90% of patients who received CMT were treated with alkylating agent–containing regimens.
P = .015.
P = .016.
P = .19.
RR and AR of second malignancy by initial radiation field (+/− chemotherapy) in 961 patients with more than 10 years of potential follow-up
| . | No. . | PY . | O . | E . | RR . | (95% CI) . | AR . | P . |
|---|---|---|---|---|---|---|---|---|
| Mantle alone | 45 | 541 | 6 | 2.9 | 2.1 | (0.8, 4.6) | 58.1 | .25 |
| MPA/PPA alone | 542 | 8573 | 89 | 21.3 | 4.2 | (3.4, 5.1) | 78.9 | |
| TNI alone9-150 | 78 | 1188 | 14 | 2.8 | 5.1 | (2.8, 8.5) | 94.7 | |
| CT + mantle | 121 | 1346 | 13 | 2.8 | 4.7 | (2.5, 8.0) | 76.0 | .03 |
| CT + MPA/PPA | 128 | 1904 | 27 | 4.6 | 5.9 | (3.9, 8.4) | 117.9 | |
| CT + TNI9-150 | 46 | 776 | 12 | 0.9 | 13.5 | (7.0, 23.5) | 143.1 |
| . | No. . | PY . | O . | E . | RR . | (95% CI) . | AR . | P . |
|---|---|---|---|---|---|---|---|---|
| Mantle alone | 45 | 541 | 6 | 2.9 | 2.1 | (0.8, 4.6) | 58.1 | .25 |
| MPA/PPA alone | 542 | 8573 | 89 | 21.3 | 4.2 | (3.4, 5.1) | 78.9 | |
| TNI alone9-150 | 78 | 1188 | 14 | 2.8 | 5.1 | (2.8, 8.5) | 94.7 | |
| CT + mantle | 121 | 1346 | 13 | 2.8 | 4.7 | (2.5, 8.0) | 76.0 | .03 |
| CT + MPA/PPA | 128 | 1904 | 27 | 4.6 | 5.9 | (3.9, 8.4) | 117.9 | |
| CT + TNI9-150 | 46 | 776 | 12 | 0.9 | 13.5 | (7.0, 23.5) | 143.1 |
One patient who received combined modality therapy received whole brain radiation therapy and was excluded from the analysis.
PY indicates person-years; O, observed; E, expected; RR, relative risk; CI, confidence interval; AR, absolute excess risk; MPA/PPA, mantle and paraaortics/paraaortics and pelvc; TNI, total nodal irradiation; CT, chemotherapy.
P = .019.
Table 7 shows the RR and AR of second malignancy according to whether or not staging laparotomy was performed. Patients who underwent surgical staging and splenectomy had a significantly higher RR of developing a second malignancy than did patients who underwent clinical staging (4.9 vs 2.8, P = .03). The corresponding ARs were 89.2 and 78.6, respectively.
Table 8 summarizes the excess risk of second malignancy by treatment modality. The RR was significantly higher in the CMT group compared with the radiation therapy alone group (P = .015). When broken down into nonrelapsed versus relapsed cases, the RR of second malignancy was the highest among patients who relapsed after CMT and received further salvage therapy. The RR of second malignancy in patients who relapsed after radiation therapy alone and received further salvage therapy was of similar magnitude to patients who received initial CMT but who never relapsed.
The excess risks of second malignancy by radiation field size, with or without chemotherapy, are summarized in Table 9. The RR and AR of second malignancy increased with increasing radiation field size. For patients treated with radiation therapy alone, the RRs of a second malignancy after mantle alone, subtotal nodal irradiation, and total nodal irradiation were 2.1, 4.2, and 5.1, respectively. Within each radiation field, the addition of chemotherapy further increased the RR of a second malignancy, although the increase was statistically significant only among patients who received total nodal irradiation (5.1 vs 13.5, P = .019). For patients treated with combined chemotherapy and radiation therapy, the RR of a second malignancy in patients treated to a mantle, subtotal nodal, and total nodal field were 4.7, 5.9, and 13.5, respectively, and the difference was statistically significant (P = .03).
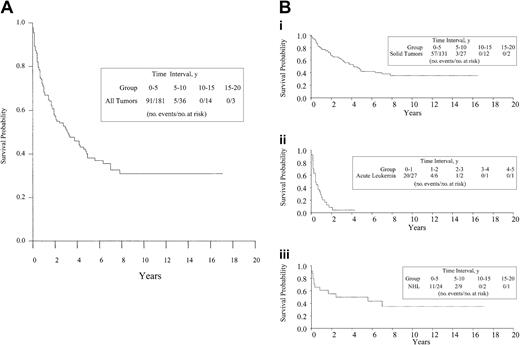
The median follow-up time after the diagnosis of a second malignancy was 3 years among survivors. The 5-year overall survival rate after second malignancy was 38.1%, and the median survival time was 3 years for all sites of second tumors. Survival following development of acute leukemia was poor, with a 5-year overall survival estimate of only 4.9%, and a median survival time of 0.4 years. Seventeen of the 23 patients who developed acute leukemia died within 1 year of diagnosis. The 5-year overall survival rates after diagnosis of second malignancy for patients who developed solid tumors and non-Hodgkin lymphoma were 42.1% and 49.6%, respectively. The corresponding median survival times were 4.3 years and 2.4 years, respectively. The survival curves after the development of any second malignancy are shown in Figure 2A, and survival curves after the development of solid tumors, leukemia, and non-Hodgkin lymphoma are shown in Figure 2B. Among the solid tumors, prognosis was the poorest in patients who developed lung cancer, with a median survival time of only 1 year. The 5-year survival estimate after development of a gastrointestinal cancer was 12.4%, and the median survival time was 1.9 years. In patients who developed breast cancer, the 5-year overall survival estimate was more favorable at 76.1%, and the median survival time has not yet been reached. The survival outcome by type of second malignancy is summarized in Table10.
Survival after second malignancy.
(A) Survival after second malignancy in patients treated for Hodgkin disease. (B) Survival after solid tumors, acute leukemia, and non-Hodgkin lymphoma in patients treated for Hodgkin disease.
Survival after second malignancy.
(A) Survival after second malignancy in patients treated for Hodgkin disease. (B) Survival after solid tumors, acute leukemia, and non-Hodgkin lymphoma in patients treated for Hodgkin disease.
Survival outcome after a second malignancy
| Second malignancy . | No. . | 5-year survival estimate (%) . | 95% CI . | Median survival, y . |
|---|---|---|---|---|
| All sites | 181 | 38.1 | (29.7-46.5) | 3.2 |
| Acute leukemia | 23 | 4.9 | (0.0-14.2) | 0.4 |
| Non-Hodgkin lymphoma | 24 | 49.6 | (28.0, 71.2) | 2.4 |
| Solid tumors | 131 | 42.1 | (31.6, 52.5) | 4.3 |
| Breast | 39 | 76.1 | (57.4-94.8) | Not yet reached |
| Lung | 22 | 0.0 | — | 1.0 |
| Gastrointestinal | 24 | 12.4 | (0-28.1) | 1.9 |
| Sarcoma | 11 | 14.4 | (0-40.2) | 4.3 |
| Genitourinary | 11 | 81.8 | (59.0-100.0) | Not yet reached |
| Head and neck | 7 | 38.1 | (0-77.2) | 2.9 |
| Melanoma | 7 | 80.0 | (44.9-100) | Not yet reached |
| Thyroid | 5 | 100.0 | — | Not yet reached |
| Gynecological | 4 | 50.0 | (1.0-99.0) | 1.4 |
| Second malignancy . | No. . | 5-year survival estimate (%) . | 95% CI . | Median survival, y . |
|---|---|---|---|---|
| All sites | 181 | 38.1 | (29.7-46.5) | 3.2 |
| Acute leukemia | 23 | 4.9 | (0.0-14.2) | 0.4 |
| Non-Hodgkin lymphoma | 24 | 49.6 | (28.0, 71.2) | 2.4 |
| Solid tumors | 131 | 42.1 | (31.6, 52.5) | 4.3 |
| Breast | 39 | 76.1 | (57.4-94.8) | Not yet reached |
| Lung | 22 | 0.0 | — | 1.0 |
| Gastrointestinal | 24 | 12.4 | (0-28.1) | 1.9 |
| Sarcoma | 11 | 14.4 | (0-40.2) | 4.3 |
| Genitourinary | 11 | 81.8 | (59.0-100.0) | Not yet reached |
| Head and neck | 7 | 38.1 | (0-77.2) | 2.9 |
| Melanoma | 7 | 80.0 | (44.9-100) | Not yet reached |
| Thyroid | 5 | 100.0 | — | Not yet reached |
| Gynecological | 4 | 50.0 | (1.0-99.0) | 1.4 |
CI indicates confidence interval.
Of the 181 patients with a second malignancy, 18 developed a third malignancy, including 1 case of acute leukemia, 1 case of non-Hodgkin lymphoma, 6 cases of breast cancers, 3 cases of lung cancers, 1 case of gastrointestinal cancer, 3 cases of genitourinary cancers, 1 case of melanoma, 1 case of mesothelioma, and 1 case of vulvar cancer. The median time between the second and third malignancy was 34 months (range, 0-203 months).
Discussion
In this study, the long-term risk of second malignancy after Hodgkin disease therapy was analyzed for 1319 patients treated over almost 30 years at a single institution. With 15 910 person-years of follow-up and with only 3.4% of patients lost to follow-up, this represents one of the largest and most complete single-institution studies on the subject. A total of 181 second malignancies and 18 additional third malignancies were observed, with solid tumors accounting for nearly three quarters of all cases. Overall, this translates to a 4.6-fold risk of developing a cancer compared with the general population, and an almost 1% excess risk per person per year. The excess risk increased with follow-up time, and after 20 years, the RR was 10.9 and the AR reached 405/10 000 person-years or 4.0% per person per year. However, it should be noted that in this study, 85% of the patients presented with early-stage disease. Therefore, the results may not be completely generalizeable to patient groups with a more typical stage distribution.
The literature on second malignancy after Hodgkin disease has grown considerably in recent years. Given that Hodgkin disease is a relatively uncommon diagnosis and a second malignancy is typically associated with a long latency, a large number of patients with long follow-up time is crucial for a full appreciation of this life-threatening consequence of Hodgkin disease therapy. The completeness of the follow-up data for the entire cohort of patients is also critical. By minimizing the number of patients lost to follow-up, ascertainment bias, which may result in overestimation or underestimation of the risk of second malignancy, can be decreased. Finally, although a multi-institutional study allows for the assessment of more patients, a single-institutional study has the advantages of uniformity of staging and treatment in each time period and availability of more detailed and accurate patient-, disease-, and treatment-related information.
The relationship between age at diagnosis and risk of second malignancy after Hodgkin disease is subject to debate.12,17,19,36-41The conflicting results reported in the literature may be due to differences in the type of second malignancy and the age group of the patient population under consideration. Also, the way in which the risks are calculated and reported may influence the results and conclusions. Because of the increasing background risk of cancer with increasing age, RR tends to decrease with increasing age, while measurements such as AR and cumulative incidence tend to increase. One consistent finding, however, is the increased risk of breast cancer for females treated for Hodgkin disease at a young age.17,18,25,26 In this study, we separated out a group of 397 women at high risk for breast cancer, namely, those who received radiation therapy to the chest region prior to age 30 years. In this group, the excess risk was especially striking 15 to 20 years and beyond 20 years after treatment, with an excess risk of 2.3% to 3.7% per person per year, respectively. Prior to 15 years, the excess risk was low (0%-0.15% per person per year). Other studies have also found a similar delay in the occurrence of breast cancer, with median time to development ranging from 15 to 18 years.24,26,27,42Because of the substantial risk, recommendations and programs dealing with breast cancer after Hodgkin disease are beginning to be implemented or studied, including early screening with mammography. Investigators are also looking into screening with breast magnetic resonance imaging and chemoprevention with tamoxifen, borrowing from data on other high-risk groups.43-46 It remains to be seen whether such efforts will reduce the risk and improve the prognosis of breast cancer after Hodgkin disease.
In this study, a significantly higher risk of second malignancy was found in patients who underwent staging laparotomy compared with those who were clinically staged. The finding of an increased risk of second cancer after surgical staging and splenectomy has also been noted by other investigators.39,40 47 Although staging laparotomy for Hodgkin disease has largely been abandoned by most institutions and practices, these findings may still have implications in the follow-up of patients who underwent the procedure. However, in our study, the numbers of patients and person-years of follow-up were relatively small for the no-laparotomy cohort. As the number of clinically staged patients increases and as their follow-up time lengthens, it will become more apparent whether the difference will persist.
We also investigated the association between treatment modality and extent, and the risk of second malignancy after Hodgkin disease. In our study, in which solid tumors accounted for 72% of all cases of second tumors, the RR of a second malignancy was found to be significantly higher in patients who received initial CMT than in patients who received radiation therapy alone. Other studies, in which solid tumors also made up the majority of the second malignancies, have found an association between overall treatment delivered and the risk of a second tumor. In a study from the Netherlands Cancer Institute by van Leeuwen et al,18 a significantly increased risk of nonbreast solid cancer in patients who received salvage chemotherapy or CMT was noted among 1253 young adults treated for Hodgkin disease. Swerdlow et al from the British National Lymphoma Investigation reported on 5519 patients with Hodgkin disease17 and found that the risk of second malignancy (in particular, that of gastrointestinal cancer) was highest among patients who received initial CMT. In a study from Munich on 1120 patients from 6 participating institutions, the cumulative intensity of chemotherapy and radiation therapy was found to correlate with the risk of second malignancy after Hodgkin disease.40 However, it is important to note that in our study, as in most of the above studies, the majority of the patients (90%) who received chemotherapy were treated with alkylating agents. In addition, 60% of patients who underwent CMT received extended-field irradiation (MPA, PPA, or TNI). It is quite plausible that the increased risk of second malignancy associated with CMT may not hold true with ABVD chemotherapy and more limited field radiation treatment. Early data clearly show no significantly increased leukemia risk with the modern regimens.48-50 However, longer follow-up time is needed to determine the long-term solid tumor risk, which is associated with a longer latency.
In this study, we noted a significant correlation between radiation field size and the risk of second malignancy. Similar findings have also been reported by others. Biti et al of the University of Florence found that the 15-year cumulative probability of developing a solid tumor was 5.1% among patients treated with involved field/mantle radiation therapy,12 compared to 11.6% among patients treated with subtotal or total nodal irradiation. Results from the International Database for Hodgkin Disease showed a 1.84-fold higher risk of solid tumor in patients who received subtotal or total nodal irradiation compared with local radiation therapy.37 Not all studies, however, have demonstrated a relationship between radiation field size and second tumor risks.8 39 The best data will come from the randomized trials comparing different radiation field sizes when these studies become fully mature. Most of the ongoing trials employ involved-field radiation therapy, which treats an even smaller volume than a mantle field. In this study, we did not attempt to evaluate the radiation dose received at the site of second tumor development. Because of the long latency to second malignancy and changes in body habitus of patients over time, especially among pediatric patients, it would be difficult to reliably correlate the recreated radiation dose distribution of the original treatment with the location of the second malignancy.
The findings of the increasing RR and AR of second malignancy with increasing follow-up time also have been noted in other reports. In the study by Swerdlow et al,17 although the RR of second malignancy remained relatively constant over time, the AR increased with length of follow-up and was up to 102.6/10 000 person-years after 15 years. Van Leeuwen et al reported an increase in RR over time up to 15 to 19 years, but after 20 years, the RR appeared to decrease. The AR of second malignancy, however, continued to increase with time, reaching 201/10 000 person-years after 20 years.18 Our observed AR beyond 20 years of 449/10 000 person-years is higher than that found in the study by Van Leeuwen et al. The difference may be due to the fact that the patient population in the van Leeuwen study was limited to adolescents and young adults, who have a lower background cancer risk.
In our study, a persistently increased excess risk over time was found for acute leukemia, non-Hodgkin lymphoma, and solid tumors. It is noteworthy that earlier studies on second malignancy after Hodgkin disease had suggested that the leukemia risk after Hodgkin disease appears to be limited to the first 10 years after treatment.4,5,7,9,10,18,51,52 However, in the current study, 2 cases were observed beyond 20 years. Nevertheless, it is clear that the increased excess risk of second malignancy in the later years is predominantly driven by solid tumors, in particular, breast cancer. The long latency emphasizes the importance of allowing adequate follow-up time before the long-term safety of the new regimens for Hodgkin disease can be confirmed. In addition, there may be some uncertainty associated with the estimate of the median time to solid tumor development, given the long latency, which extended well beyond the median follow-up of this study. Longer follow-up time is needed to further confirm the timing of the various types of solid tumors following Hodgkin disease. Because of the high cure rate of Hodgkin disease and its occurrence in predominantly younger patients, a significant number of survivors of the disease who received various forms of treatment over the years are currently alive and are in need of proper follow-up care. In this study, we found a dramatic increase in second tumor risk with time; 15 to 20 years or more after initial therapy, survivors of Hodgkin disease on average are faced with a 2.3% to 4.0% excess risk of second malignancy per person per year. This clearly represents a substantial risk in a group of patients who have long been cured of their original cancer diagnosis and may no longer feel the need for vigilance. Primary care physicians, who may be the main source of long-term care for survivors of Hodgkin disease, should be made aware of these risks. Whether the magnitude of the risk and the poor prognosis associated with some of the second malignancies, including lung and gastrointestinal cancers, justify more comprehensive screening strategies, such as yearly body CAT scan or use of the newer, potentially more sensitive imaging techniques such as positron emission tomography,53 needs to be explored. Researchers have also attempted to identify potential molecular markers that may be associated with increased risk for a second malignancy, although results have been unrevealing thus far.54 55 However, such research efforts should continue in order to better define high-risk groups for more intensive surveillance and interventional programs tailored to their specific risk profile.
Prepublished online as Blood First Edition Paper, June 7, 2002; DOI 10.1182/blood-2002-02-0634.
Supported by funding from the Suzanne L. Chute Lymphoma Clinical Research Program and a Joint Center for Radiation Therapy Foundation grant.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Peter M. Mauch, Department of Radiation Oncology, Brigham and Women's Hospital, 75 Francis St, ASB1-L2, Boston, MA 02115; e-mail: pmauch@lroc.harvard.edu.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal