We have previously shown that the infusion of donor lymphocytes expressing the herpes simplex virus thymidine kinase(HSV-tk) gene is an efficient tool for controlling graft-versus-host disease (GVHD) while preserving the graft-versus-leukemia (GVL) effect. In addition to the GVL effect, the administration of donor HSV-tk+ cells could have a clinical impact in promoting immune reconstitution after T-cell–depleted stem cell transplantation (SCT). To explore this hypothesis, we have investigated whether in vitro polyclonal activation, retroviral transduction, immunoselection, and expansion affect the immune competence of donor T cells. We have observed that, after appropriate in vitro manipulation, T cells specific for antigens relevant in the context of SCT are preserved in terms of frequency, expression of T-cell receptor, proliferation, cytokine secretion, and lytic activity. A reduction in the frequency of allospecific T-cell precursors is observed after prolonged T-cell culture, suggesting that cell manipulation protocols involving a short culture time and high transduction efficiency are needed. Finally, the long-term persistence of HSV-tk+ cells was observed in a patient treated in the GVL clinical trial, and a reversion of the phenotype of HSV-tk+ cells from CD45RO+ to CD45RA+ was documented more than 2 years after the infusion. Based on all this evidence, we propose a clinical study of preemptive infusions of donor HSV-tk+ T cells after SCT from haploidentical donors to provide early immune reconstitution against infection and potential immune protection against disease recurrence.
Introduction
In allogeneic stem cell transplantation (allo-SCT), delayed donor lymphocyte infusion (DLI) plays a crucial therapeutic role in promoting an antitumor effect.1-3 However, the efficacy of DLI is limited by the development of graft-versus-host disease (GVHD).2,4 We and others have previously shown that GVHD can be selectively treated by the transfer of theHSV-tk gene into donor lymphocytes to confer ganciclovir (GCV) sensitivity.5,6 In these clinical trials, the antitumor activity of transduced lymphocytes was observed in a significant number of patients, resulting in complete and durable clinical remission6-8 (F.C. et al, manuscript in preparation). In addition to the above clinical context, the early administration of donor lymphocytes genetically engineered for the expression of a suicide phenotype could have a clinical impact in promoting immune reconstitution after SCT from haploidentical donors (haplo-SCT). In this context the intensive T-cell depletion required to avoid lethal GVHD has been associated with a delayed immune recovery of CD3+ cells to 7 to 9 months after transplantation and a prolonged risk for infection after transplantation.9 10The early infusion of HSV-tk–transduced donor lymphocytes could provide a rapid reconstitution of a wide T-cell repertoire while providing a tool for the selective control of GVHD.
We and others previously demonstrated that human lymphocytes can be efficiently transduced by retroviral vectors after the induction of active cell proliferation.11,12 The cell manipulation protocol proposed consists of polyclonal T-cell activation and culture in the presence of recombinant human interleukin-2 (rhIL-2). This protocol allows the transduction of a polyclonal T-cell population, potentially representative of all T-cell precursors circulating in healthy donors.7,13 However, the variability in response to activation stimuli, activation-induced cell death (AICD), exposure to rhIL-2, and proliferation-induced T-cell exhaustion could alter the immune potential of donor T cells. Indeed, other investigators previously reported that some gene transfer protocols skew the Vβ cell repertoire to oligoclonality and that this modification is attributed more appropriately to ex vivo culture than to gene transfer.14,15 Ex vivo culture required for gene transfer and selection also reduced the alloreactive potential of transduced cells into a murine GVHD model.16 Recently, the same group reported that reduced Epstein-Barr virus (EBV)–specific immune reactivity is observed on transduced lymphocytes after activation and drug selection17 and suggested that appropriate activation and immune selection could significantly spare EBV-specific lymphocytes. In this study, we extensively investigated the immune competence of transduced and selected lymphocytes. Because noncultured, nontransduced, nonselected peripheral blood lymphocytes (PBLs) from healthy donors have by definition retained immune activity and are to date the standard therapy for disease relapse after SCT, PBLs were regarded as the appropriate experimental control. To account for interindividual heterogeneity of T-cell responses, experiments were performed by comparing genetically modified donor T cells with PBLs from the same donor. Our results suggest that, after appropriate in vitro manipulation, T cells maintain the ability to recognize, proliferate, and kill cells expressing antigens relevant in SCT. Based on this evidence, we propose a clinical study of preemptive infusions of HSV-tk+ donor T cells after T-cell–depleted SCT to confer early immune reconstitution against infection and potential immune protection against disease recurrence.
Materials and methods
Transduction and selection of human lymphocytes with retroviral vectors
Primary human lymphocytes were transduced with a replication-competent retrovirus (RCR)–free Am-12–derived packaging clone encoding for the SFCMM-3 vector (clone 35). The SFCMM-3 vector13 encodes for HSV-tk as the suicide gene and for a truncated form of the low-affinity receptor for nerve growth factor (ΔLNGFR) as a cell surface marker.12 Briefly, PBLs were isolated from healthy donors by leukapheresis and Ficoll-Hypaque gradient separation (Lymphoprep Nycomed; Pharma AS, Oslo, Norway) and activated with 2 μg/mL phytohemagglutinin (PHA) (Boehringer Mannheim-Roche GmbH, Germany). When different activation signals were compared, 30 ng/mL anti-CD3 monoclonal antibody (mAb) (OKT3) (Orthoclone, Milan, Italy) and 30 ng/mL anti-CD3 plus 1 μg/mL anti-CD28 mAb (PharMingen, San Diego, CA) were used. Activated T cells were cultured at 1 × 106 cells/mL, in RPMI 1640 supplemented with 5% autologous serum in the presence of 100 U/mL rhIL-2 (EuroCetus Italia S.r.l., Milan, Italy). Culture medium was changed every 3 to 4 days. Transduction was performed by 2 cycles of 2-hour centrifugation starting 2 days after stimulation in the presence of polybrene (8 μg/mL). The same supernatant batch was used at a multiplicity of infection (MOI) of 3:1. Some experiments were repeated with cells transduced by 72-hour cocultivation with semiconfluent lethally irradiated packaging cells (100 Gy; GIL RAD, Gilardoni, Mandello, Italy) on the day of stimulation in the presence of polybrene (8 μg/mL). Retrovirally transduced cells were analyzed for ΔLNGFR expression on day 5 from activation by fluorescence-activated cell sorter (FACS) and were immunoselected on the same day as previously described12 13 with a mouse antihuman LNGFR mAb (Boehringer Mannheim-Roche, Basel, Switzerland) and goat antimouse immunoglobulin G1 (IgG1)–coated magnetic beads (Dynabeads M-450; Dynal AS, Oslo, Norway) to obtain a greater than 95% pure population of transduced cells. Transduced and immunoselected donor T cells were expanded in the culture conditions described above for 14 days after initial activation and subsequently frozen. Transduced, immunoselected, cultured cells will be referred to as RV cells throughout the rest of this report. PBLs from the same donors isolated by leukapheresis and gradient separation were used as controls.
Flow cytometric analysis of genetically engineered T cells
RV cells and PBLs from the same donors were characterized by cell surface staining with fluorescein isothiocyanate (FITC)– and phycoerythrin (PE)–conjugated antibodies to CD2, CD3, CD4, CD8, CD56, CD19 (Becton Dickinson, Mountain View, CA), CD62L, CD28, and CD95 (PharMingen Biosciences, San Diego, CA) and with FITC- and PE-conjugated isotype controls. Activation of T cells was evaluated by staining with FITC- and PE-conjugated antibodies to CD25, HLA-DR, CD69, CD45RA, and CD45RO (Becton Dickinson).
Transduced cells were detected in vitro and ex vivo by staining with the mouse antihuman LNGFR monoclonal antibody (mAb) followed by FITC-conjugated goat antimouse antibody (DAKO, Glostrup, Denmark). Analysis of the T-cell receptor (TCR)–Vβ repertoire was performed by staining PBL and RV cells with a panel of mouse antihuman Vβ antibodies (Vβ2(a), Vβ5(a), Vβ5(b), Vβ5.1, Vβ5.2, Vβ5.3, Vβ8(a), Vβ12.1, Vβ 13.1, Vβ14, Vβ16, Vβ17, Vβ18, and Vβ22; Immunotech, Marseilles, France) followed by FITC-conjugated goat antimouse antibody. For LNGFR/CD45RA/CD45RO triple fluorescence, cells were stained with a biotinylated anti-LNGFR mAb (Boehringer Mannheim-Roche) followed by streptavidin conjugated to tricolor, FITC-conjugated, anti-CD45RA and PE-conjugated anti-CD45RO antibodies (Caltag, Burlingame, CA). Isotype controls from the same manufacturers were used, and quadrant markers were positioned to include 95% of stained cells. Samples were analyzed on FACScalibur (Becton Dickinson, Milan, Italy) using Cell Quest software (BD Biosciences, Milan, Italy).
Intracytoplasmic staining for cytokine production
To determine the cytokine production profile, intracellular cytokines were quantified by flow cytometry as described,18 with some modifications. Pairs of RV cells and PBLs from the same donors (1 × 106/mL) were stimulated with 10 μg/mL immobilized OKT3 and 10 ng/mL phorbol myristate acetate (TPA). After 3 hours of activation, 1 ng/mL brefeldin A (Sigma Chemical, Milan, Italy) was added. After 6 hours of activation, T cells were washed in phosphate-buffered saline (PBS), stained with anti-CD4 and anti-CD8 mAbs, and fixed in 2% formaldehyde for 20 minutes at 20°C. After fixation, T cells were permeabilized in PBS supplemented with 2% fetal calf serum (FCS) and 0.5% saponin (Sigma). T cells were incubated with PE-labeled anti–hIL-4, anti–hIL-2, or anti–hIL-10 and FITC-coupled anti–interferon γ (IFN-γ) (PharMingen). After washing, cells were analyzed on FACScalibur.
Analysis of antigen-specific T-cell frequency on genetically engineered T cells and PBLs using peptide–major histocompatibility complex tetramers
The nonapeptide pp65495-503, derived from the structural protein pp65 of cytomegalovirus (CMV), which binds HLA-A0201,19 was synthesized. Tetramers were made according to the protocol of Altman et al.20 In brief, human β2-microglobulin and the soluble domain of the HLA-A0201 heavy chain linked at its COOH terminus to BirA substrate peptide and β2-microglobulin subunits were solubilized and refolded in the presence of the peptide. Folded material was biotinylated by BirA enzyme. HLA-A0201–peptide complexes were purified on gel filtration and ion exchange columns. Tetrameric complexes of biotinylated HLA-A0201 peptide were produced by mixing purified, biotinylated heterodimer with NeutrAvidin-PE (Molecular Probes) at a molar ratio of 4:1. To compare the frequency of antigen-specific T cells on RV cells and PBLs, 1 × 106 cells were stained with PE-conjugated pp65-tetramer, anti-CD8–Quantum Red (1/60) and anti-CD3–FITC (1/60) antibodies for 30 minutes at 4°C. The frequency of pp65-specific cytotoxic T lymphocytes (CTLs) is presented as a fraction of tetramer-positive, CD3+/CD8+ lymphocytes over the total of CD3+/CD8+ lymphocytes.
Induction of EBV-specific cytotoxic T lymphocytes
For the induction of CTLs specific to EBV, EBV IgG-seropositive healthy donors were used. Autologous EBV cells lines (EBV-LCL) were obtained by infecting PBLs with the B95-8 EBV strain for 3 hours.21 To compare RV cells with PBLs for the ability to lyse autologous EBV-LCL, CD8+ cells were obtained by positive separation using anti-CD8 magnetic-activated cell separation (MACS) microbeads (Miltenyi Biotec GmbH) according to the manufacturer's recommendations. CD8+ RV cells (1.5 × 106) and the same number of CD8+ PBLs were stimulated in vitro with 5 × 105 previously irradiated (100 Gy) autologous EBV-LCL, in Iscove modified Dulbecco medium (IMDM) supplemented with 10% human serum, glutamine, and antibiotics in the presence of 50 U/mL rhIL-2 (mixed lymphocyte reaction [MLR] medium). Effector cells were tested against autologous EBV-LCL in a standard cytotoxicity assay 10 days later. As negative controls, effectors were tested against autologous PHA-activated lymphocytes. As a control for specific cytotoxic activity, cold inhibition assay was used adding unlabeled K562 cells in 30 times excess to chromium Cr 51–labeled target cells. As described elsewhere,22 this proportion of K562 cells resulted in complete inhibition of nonspecific natural killer/lymphokine-activated killer cell (NK/LAK) activity.
Induction of CMV-specific cytotoxic T lymphocytes
To isolate specific CTLs against CMV, autologous fibroblasts from IgG CMV-positive healthy donors were infected with AD169 strain CMV for 4 hours. RV cells (2 × 106) and the same number of PBLs chosen for a similar CD4+/CD8+ ratio were cultured in the presence of 5 × 104 autologous CMV-infected fibroblasts and 1 × 106 autologous peripheral blood mononuclear cells (PBMCs) previously irradiated at 60 Gy in MLR medium. Cells were restimulated at day 7 using the same culture conditions. Effector cells were tested after 7 to 10 days against autologous CMV-infected fibroblasts in a cold inhibition cytotoxicity assay. Autologous mock-infected fibroblasts were used as a negative control. To determine the target of the anti-CMV immune response, autologous EBV-LCLs were infected for 8 to 12 hours with recombinant vaccinia virus (rVV) encoding the CMV matrix proteins pp65, pp150, and pp72 at an MOI of 10:1. Infected EBV-LCLs were then used as targets of a cold inhibition cytotoxicity assay. Autologous EBV-LCLs infected with an irrelevant rVV were used as a negative control.
Induction of flu-specific cytotoxic T lymphocytes
To isolate flu-specific cytotoxic T lymphocytes, 5.6 × 106 PHA-activated lymphocytes from HLA-A0201 donors were pulsed with 50 μM class 1 HLA-A0201–restricted M58-66 peptide derived from the flu matrix protein (Neosystem Laboratoire, Strasburg, France) in 1 mL IMDM in the presence of 2 μg/mL β2-microglobulin (Sigma) and 100 U/mL rhIL-2 for 4 hours at room temperature. Cells were then irradiated at 60 Gy, washed, and cultured with CD8+ RV cells or CD8+ PBLs at a responder-to-stimulator ratio of 1.5:1. Effector cells were tested 7 to 10 days later in a cold inhibition cytotoxicity assay as described. To this purpose, M58-66-pulsed HLA-A0201 TAP-deficient T2 cells23 were labeled with 51Cr and were used as targets. Unpulsed T2 cells were used as negative controls. Because M58-66 flu peptide is usually recognized in HLA-A0201–positive patients by Vβ17-TCR+ T cells, staining with a Vβ17 antibody was used to monitor the expansion of Vβ17+ cells by flow cytometry.
Cytotoxic T-lymphocyte precursors frequency against HLA-mismatched target cells
To isolate cytotoxic T lymphocytes specific for allogeneic cells, 1.5 × 106 CD8+ RV cells and CD8+ PBLs from the same donor were stimulated in MLR against 1 × 106 60-Gy–irradiated, fully allogeneic PBMCs in MLR medium. Effector cells were tested against PHA-activated lymphocytes from the same donor in a standard cytotoxicity assay performed in cold inhibition 10 days later. Autologous PHA-activated lymphocytes were used as negative controls. To establish the frequency of antiallogeneic cytotoxic T precursor (CTLp), CD8+ RV cells and CD8+ PBLs from the same donor were plated in limiting dilution at 50 × 103, 40 × 103, 30 × 103, 20 × 103, 10 × 103, 5 × 103, 2.5 × 103, and 1.25 × 103 cells per well (96-well plate) with 30 × 103 fully mismatched PBMCs as stimulators and 30 × 103 autologous PBMCs as feeder cells; both types were 60 Gy irradiated in MLR medium. Twenty wells were plated for each dilution of responders. Medium was replaced on day 7, and cells were tested in a cold inhibition cytotoxicity assay on day 10. As negative controls, effectors were tested against autologous PHA-derived lymphocytes. Statistical analysis was performed with the χ2 Poisson distribution method.
Results
Human lymphocytes activated with different stimuli can be efficiently transduced by cell-free, retroviral-containing supernatant
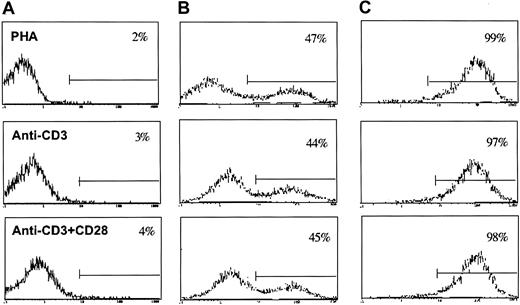
To identify the protocol of T-cell activation resulting in the highest transduction efficiency, different activation signals, such as PHA, anti-CD3 mAb, and the combination of anti-CD3 mAb and anti-CD28 mAb, were compared. Cells were transduced 48 hours after stimulation by 2 cycles of 2-hour centrifugation in the presence of cell-free retroviral supernatant. All the activation signals tested resulted in efficient and similar transduction efficiency (Figure1B). In 3 independent experiments performed with cells from different donors, the difference in transduction efficiency observed with the 3 activation protocols was less than 5%. No differences in gene transfer efficiency were observed if transduction was delayed by 24 hours (data not shown). Such gene transfer efficiency is similar to the efficiency obtained by coculture of T cells with irradiated packaging cell lines.13However, the use of a cell-free supernatant is more suitable to clinical use.
Different activation signals such as PHA, anti-CD3, and anti-CD3 plus anti-CD28 antibodies result in similar transduction efficiency and identical level of transgene expression.
(A) Autofluorescence of transduced cells stained with FITC-conjugated goat antimouse antibody. (B) Transduction efficiency measured by cytofluorometric analysis for ΔLNGFR expression after cell-free, supernatant-mediated transduction. (C) ΔLNGFR expression of the same subpopulation of lymphocytes after immune selection and 14-day culture from initial activation.
Different activation signals such as PHA, anti-CD3, and anti-CD3 plus anti-CD28 antibodies result in similar transduction efficiency and identical level of transgene expression.
(A) Autofluorescence of transduced cells stained with FITC-conjugated goat antimouse antibody. (B) Transduction efficiency measured by cytofluorometric analysis for ΔLNGFR expression after cell-free, supernatant-mediated transduction. (C) ΔLNGFR expression of the same subpopulation of lymphocytes after immune selection and 14-day culture from initial activation.
Retrovirally transduced cells were immunoselected for ΔLNGFR expression, as previously described,12 to obtain a greater than 95% pure population of transduced cells. All the activation protocols resulted in the same level of transgene expression, which was maintained throughout the 14 days of culture (Figure 1C).
Transduction/selection procedure results in T cells with a mixed activation phenotype
To analyze the effects of cell manipulation on different cell subsets, 3 pairs of PBLs and RV cells were analyzed for the expression of surface markers. As shown in Table 1, most RV cells expressed the panlymphocytic CD2 marker. Although most RV cells were represented by T lymphocytes (CD3+ cells), a variable number of cells (ranging from 3% to 19%) showed an NK phenotype (CD2+CD3−CD56+). Among CD3+ T cells, an inversion of the CD4+/CD8+ ratio was usually observed in RV cells, whereas B lymphocytes (CD19+) were lost during culture. Interestingly, the inversion of the CD4+/CD8+ ratio was not caused by the preferential transduction of CD8+ cells but by culture conditions because it was seen also in cultured nontransduced cells. Different activation signals resulted in a similar CD4+/CD8+ ratio. Polyclonality of transduced cells was verified by immunophenotyping for TCR Vβ repertoire. All TCR analyses were represented in RV cells, and comparative analysis of RV cells and autologous PBLs revealed no gross alterations of the TCR repertoire.
Phenotypic and activation surface markers of PBLs and RV cells on 3 representative donors
| Surface marker . | Donor 1 . | Donor 2 . | Donor 3 . | |||
|---|---|---|---|---|---|---|
| PBLs % . | RV cells % . | PBLs % . | RV cells % . | PBLs % . | RV cells % . | |
| CD2 | 90 | 97 | 79 | 99 | 77 | 100 |
| CD3 | 84 | 97 | 64 | 82 | 76 | 97 |
| CD4 | 65 | 45 | 45 | 22 | 55 | 36 |
| CD8 | 25 | 58 | 23 | 55 | 29 | 56 |
| CD56 | 8 | 12 | 27 | 19 | 20 | 9 |
| CD19 | 8 | 0 | 12 | 0 | 4 | 5 |
| CD25 | 1 | 2 | 3 | 1 | 4 | 7 |
| HLA-DR | 25 | 85 | 37 | 87 | 24 | 92 |
| CD69 | 12 | 21 | 30 | 65 | 16 | 54 |
| CD95 | 10 | 72 | 14 | 94 | 40 | 99 |
| CD45RA | 42 | 5 | 43 | 1 | 43 | 6 |
| CD45RO | 40 | 91 | 56 | 99 | 57 | 97 |
| CD62L | 74 | 56 | 46 | 27 | 67 | 51 |
| CD28 | 67 | 51 | 68 | 33 | 68 | 33 |
| Surface marker . | Donor 1 . | Donor 2 . | Donor 3 . | |||
|---|---|---|---|---|---|---|
| PBLs % . | RV cells % . | PBLs % . | RV cells % . | PBLs % . | RV cells % . | |
| CD2 | 90 | 97 | 79 | 99 | 77 | 100 |
| CD3 | 84 | 97 | 64 | 82 | 76 | 97 |
| CD4 | 65 | 45 | 45 | 22 | 55 | 36 |
| CD8 | 25 | 58 | 23 | 55 | 29 | 56 |
| CD56 | 8 | 12 | 27 | 19 | 20 | 9 |
| CD19 | 8 | 0 | 12 | 0 | 4 | 5 |
| CD25 | 1 | 2 | 3 | 1 | 4 | 7 |
| HLA-DR | 25 | 85 | 37 | 87 | 24 | 92 |
| CD69 | 12 | 21 | 30 | 65 | 16 | 54 |
| CD95 | 10 | 72 | 14 | 94 | 40 | 99 |
| CD45RA | 42 | 5 | 43 | 1 | 43 | 6 |
| CD45RO | 40 | 91 | 56 | 99 | 57 | 97 |
| CD62L | 74 | 56 | 46 | 27 | 67 | 51 |
| CD28 | 67 | 51 | 68 | 33 | 68 | 33 |
The in vitro stimulation required for transduction induces polyclonal activation of T cells. To characterize the level of cell activation in RV cells, the expression of activation molecules such as CD25, HLA-DR, CD69, CD95, CD45RA, CD45RO, and CD28 was investigated. More than 91% of RV cells had an antigen-experienced phenotype (CD45RA−CD45RO+). This phenotype was maintained for more than 28 days of culture, suggesting a memory function for RV cells. Most cells still expressed HLA-DR and CD95 but had already lost the expression of CD25 and, in some cases, of CD69, suggesting that RV cells were reaching a new resting phase.
To obtain the in vivo induction of an effective immune response, T cells are supposed to travel to T-cell areas of secondary lymphoid organs to find antigen presented by professional antigen-presenting cells (APCs).24,25 A substantial proportion of RV cells expressed CD62L, a crucial molecule for lymphocyte migration to lymph nodes,25 suggesting that the in vitro manipulation does not interfere with homing abilities. Finally, a variable but consistent proportion of T cells maintained expression of CD28 after in vitro manipulation. Because CD28 engagement in CD28+ T cells recruits membrane microdomains containing kinases and adapters to the triggered TCR, allowing the activation threshold to be reached more rapidly and at lower doses of antigen,26 the maintained expression of this molecule should facilitate the activation of RV cells. Interestingly, the same results were observed using untransduced cells stimulated and cultured in the same conditions (data not shown), suggesting that the in vitro culture conditions and not the transduction/selection procedures were responsible for the alterations in cell phenotype.
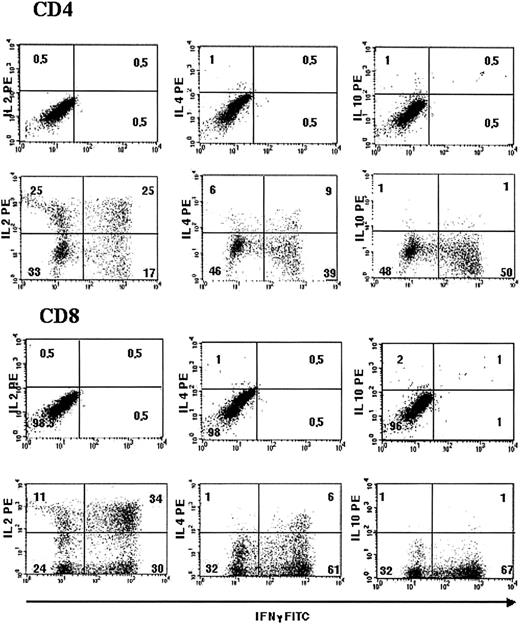
Transduction/selection procedure results mainly in TC1 and TH1 subsets
To determine whether the gene transfer procedure skews toward different T-cell subsets, CD4+ and CD8+ RV cells from 3 different donors were analyzed for intracytoplasmic cytokine production. IL-2 and interferon (IFN)–γ were chosen as representative of helper T-cell/cytotoxic T-cell (TH1/TC1) subsets, and IL-4 and IL-10 were used to detect, respectively, TH2/TC2 and regulatory T cells.18,27 All cytokines were detected, though in different amounts. Analysis performed on RV cells obtained from 3 different donors showed a higher proportion of CD4+/IL-2+/TH1 (41%-50%) and CD4+/IFN-γ+/TH1 (37%-51%) than CD4+/IL-4+/TH2 (12%-19%) subsets and a higher proportion of CD8+/IL-2+/TC1 (44%-46%) and CD8+/IFN-γ+/TC1 (64%-70%) than CD8+/IL-4+/TC2 (7%-13%) cells. Less than 3% IL-10+ regulatory cells were detected in RV cells (Figure 2). These results suggest a more rapid and increased production of type 1 and type 2 cytokines than peripheral blood mononuclear cells and a preferential skewing toward CD4+TH1 and CD8+TC1,28 probably because of culture in the presence of rhIL-2.
Activation, transduction, and selection procedures result mainly in IL-2 and IFN-γ–producing T cells, documenting a preferential skewing toward CD4+ TH1 and CD8+ TC1 phenotypes.
Intracytoplasmic staining of RV cells for IFN-γ (FITC; x axes, all panels), IL-2 (PE; y axes, left panels), IL-4 (PE; y axes, central panels), and IL-10 (PE; y axes, right panels) is shown. Results were analyzed gating CD4+ (upper panels) and CD8+ (lower panels). Quadrant markers were positioned to include 95% of stained, unstimulated cells in the lower left square (upper panel of each series). Results from 1 of 3 representative experiments are shown.
Activation, transduction, and selection procedures result mainly in IL-2 and IFN-γ–producing T cells, documenting a preferential skewing toward CD4+ TH1 and CD8+ TC1 phenotypes.
Intracytoplasmic staining of RV cells for IFN-γ (FITC; x axes, all panels), IL-2 (PE; y axes, left panels), IL-4 (PE; y axes, central panels), and IL-10 (PE; y axes, right panels) is shown. Results were analyzed gating CD4+ (upper panels) and CD8+ (lower panels). Quadrant markers were positioned to include 95% of stained, unstimulated cells in the lower left square (upper panel of each series). Results from 1 of 3 representative experiments are shown.
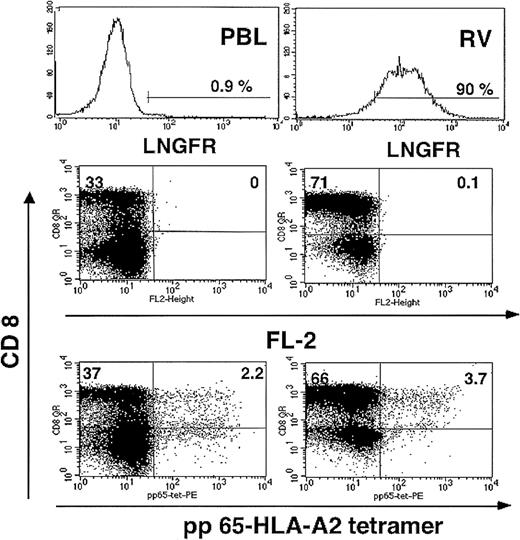
Cytotoxic T cells specific for CMV antigens are preserved after gene transfer and selection
Immune competence of RV cells was studied using antigens relevant in allogeneic stem cell transplantation. In particular CMV, a significant cause of illness and death after SCT,29 was used as a model antigen. To determine whether the gene transfer/selection procedure resulted in a reduced frequency of CTLs specific for CMV, pairs of RV cells and PBLs were stained with a PE-conjugated tetramer specific for the immunodominant HLA-A0201–restricted CMV pp65495-503 peptide. The frequency of CD8+ pp65 tetramer-binding cells in PBLs (ΔLNGFR−) was preserved in RV cells (ΔLNGFR+) (Figure 3). The high level of circulating tetramer+ cells shown in Figure 3is suggestive of a recent CMV infection and T-cell activation. To evaluate whether resting memory T cells specific for pp65 are preserved after gene manipulation, cells from 2 CMV-seropositive donors with a lower frequency of circulating tetramer+ cells were studied. A similar frequency of CD8+ pp65 tetramer-binding cells in PBLs and RV cells (0.59% vs 0.56% of total CD3+/CD8+ cells in donor 2; 0.3% vs 0.5% in donor 3) was observed. In spite of interindividual differences highlighting the heterogeneity of T-cell responses, these results suggest that CTLs specific for pp65 are preserved in terms of frequency and level of TCR expression after in vitro manipulation.
CTLs specific for CMV pp65 are preserved in RV cells.
T cells specific for the immunodominant HLA-A0201–restricted pp65495-503 peptide derived from the matrix protein pp65 of CMV were detected by staining with a QR-conjugated CD8 and a PE-conjugated pp65 tetramer followed by cytofluorometric analysis. Upper panels show the expression of ΔLNGFR in PBLs (upper left panel) and RV cells (upper right panel). Middle panels show FL-2 autofluorescence of cells stained with QR-conjugated CD8 antibody and FITC-ΔLNGFR antibody. Lower panels show the percentage of QR-CD8+/PE-pp65-tetramer+ T cells in PBLs.
CTLs specific for CMV pp65 are preserved in RV cells.
T cells specific for the immunodominant HLA-A0201–restricted pp65495-503 peptide derived from the matrix protein pp65 of CMV were detected by staining with a QR-conjugated CD8 and a PE-conjugated pp65 tetramer followed by cytofluorometric analysis. Upper panels show the expression of ΔLNGFR in PBLs (upper left panel) and RV cells (upper right panel). Middle panels show FL-2 autofluorescence of cells stained with QR-conjugated CD8 antibody and FITC-ΔLNGFR antibody. Lower panels show the percentage of QR-CD8+/PE-pp65-tetramer+ T cells in PBLs.
Because the polyclonal T-cell activation required for gene transfer could potentially result in a refractory phase of nonresponse to additional stimuli or in AICD secondary to TCR religation,30 experiments were designed to assess the ability of RV cells to recognize and lyse cells expressing antigens relevant in the SCT setting.
Immune response to viral antigens is preserved after gene transfer and selection
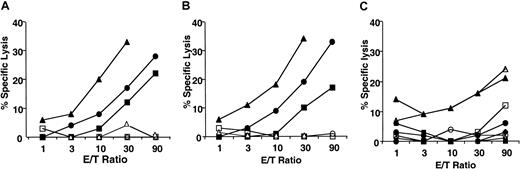
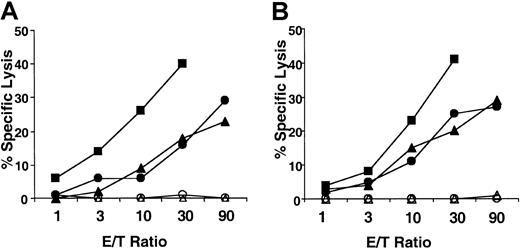
To evaluate the reactivity of RV cells to viral antigens, EBV, CMV, and influenza virus were used. RV CD8+ cells and PBL CD8+ cells were stimulated either against autologous EBV-LCLs or autologous fibroblasts infected with CMVs, and specific lytic activity was tested in a cold cytotoxic inhibition assay. RV cells (Figure 4B) were always as efficient as PBLs (Figure 4A) in lysing viral-infected autologous targets.
RV cells are as efficient as PBLs in generating viral-specific cytotoxic effectors.
PBLs (A) and RV cells (B) were stimulated against autologous irradiated EBV-LCL (triangles) or CMV-infected fibroblasts (circles and squares). Cytolytic activity was measured in a cold inhibition cytotoxic assay at different effector/target (E/T) ratios against the same targets (closed symbols). As negative control, cytolytic activity against autologous PHA-derived lymphocytes (experiments with EBV-LCL) and autologous noninfected fibroblasts (experiments with CMV) was measured (open symbols). (C) Specific lysis of PBLs (open symbols) and RV cells (closed symbols) stimulated with autologous irradiated CMV-infected fibroblasts against autologous EBV-LCL infected with rVV-pp150 (triangles), rVV-pp65 (squares), or rVV-pp72 (circles) is shown.
RV cells are as efficient as PBLs in generating viral-specific cytotoxic effectors.
PBLs (A) and RV cells (B) were stimulated against autologous irradiated EBV-LCL (triangles) or CMV-infected fibroblasts (circles and squares). Cytolytic activity was measured in a cold inhibition cytotoxic assay at different effector/target (E/T) ratios against the same targets (closed symbols). As negative control, cytolytic activity against autologous PHA-derived lymphocytes (experiments with EBV-LCL) and autologous noninfected fibroblasts (experiments with CMV) was measured (open symbols). (C) Specific lysis of PBLs (open symbols) and RV cells (closed symbols) stimulated with autologous irradiated CMV-infected fibroblasts against autologous EBV-LCL infected with rVV-pp150 (triangles), rVV-pp65 (squares), or rVV-pp72 (circles) is shown.
To identify potential modifications in the CMV-specific T-cell repertoire induced by in vitro manipulation, immunity against single CMV-derived proteins was studied. To this purpose, autologous EBV-LCLs were infected with rVV coding for pp65, pp150, and pp72 CMV proteins. Infected cells were used in a cytotoxic assay as targets of the CMV-specific T-cell lines. Autologous EBV-LCLs infected with rVV coding for green fluorescent protein (GFP) were used as a negative control. Stimulation of PBLs and RV cells resulted in the expansion of CTLs specific for the same CMV antigen, most frequently a pp65-derived peptide for HLA-A2+ donors (data not shown) or a pp150-derived peptide for HLA-A3+ donors (Figure 4C).
To better correlate proliferation of specific viral CTLs with cytolytic activity, immune response to the M58-66 matrix flu peptide was investigated. Because the M58-66 peptide is presented by HLA-A0201 molecules to cytotoxic effectors Vβ17+ TCR chain,31 this model allows evaluation of the level of proliferation of antigen-specific T cells and their killing activity. RV CD8+ cells and PBL CD8+ cells from the same HLA-A0201+ donor were stimulated against autologous PHA lymphocytes pulsed with the M58-66 peptide. After one round of in vitro stimulation, specific cytotoxic activity against HLA-A0201+ T2 cells pulsed with the M58-66peptide was similar in RV cells and PBLs (Figure5A). Similarly, RV cells were as good as PBLs in expanding 2- to 5-fold Vβ17 TCR+ cells when stimulated with the M58-66 peptide (Figure 5B-C). These results suggest that effective T cells specific for viral antigens relevant in the context of allo-SCT are preserved and functional after gene transfer and immunoselection.
RV cells specific for a viral-derived peptide are as efficient as PBLs in proliferating and lysing cells pulsed with the peptide.
(A) PBL CD8+ (open symbols) and RV CD8+ cells (closed symbols) were stimulated with the M58-66 Flu peptide and tested in a cold inhibition cytotoxic assay against T2 cells pulsed (triangle) or not (circle) with the same M58-66 peptide. The proportion of Vβ17 TCR on PBLs or RV CD8+ cells stimulated with autologous cells in the absence (C) or in the presence (D) of the M58-66 peptide is measured by cytofluorometric analysis. (B) Autofluorescence of PBLs and RV cells stained with FITC-conjugated goat antimouse antibody is shown. Results from 1 of 3 representative experiments are shown. Horizontal bars indicate % of Vβ17 in panels C and D and % GAM-FITC in panel B.
RV cells specific for a viral-derived peptide are as efficient as PBLs in proliferating and lysing cells pulsed with the peptide.
(A) PBL CD8+ (open symbols) and RV CD8+ cells (closed symbols) were stimulated with the M58-66 Flu peptide and tested in a cold inhibition cytotoxic assay against T2 cells pulsed (triangle) or not (circle) with the same M58-66 peptide. The proportion of Vβ17 TCR on PBLs or RV CD8+ cells stimulated with autologous cells in the absence (C) or in the presence (D) of the M58-66 peptide is measured by cytofluorometric analysis. (B) Autofluorescence of PBLs and RV cells stained with FITC-conjugated goat antimouse antibody is shown. Results from 1 of 3 representative experiments are shown. Horizontal bars indicate % of Vβ17 in panels C and D and % GAM-FITC in panel B.
RV lymphocytes maintain an antiallogeneic immune repertoire
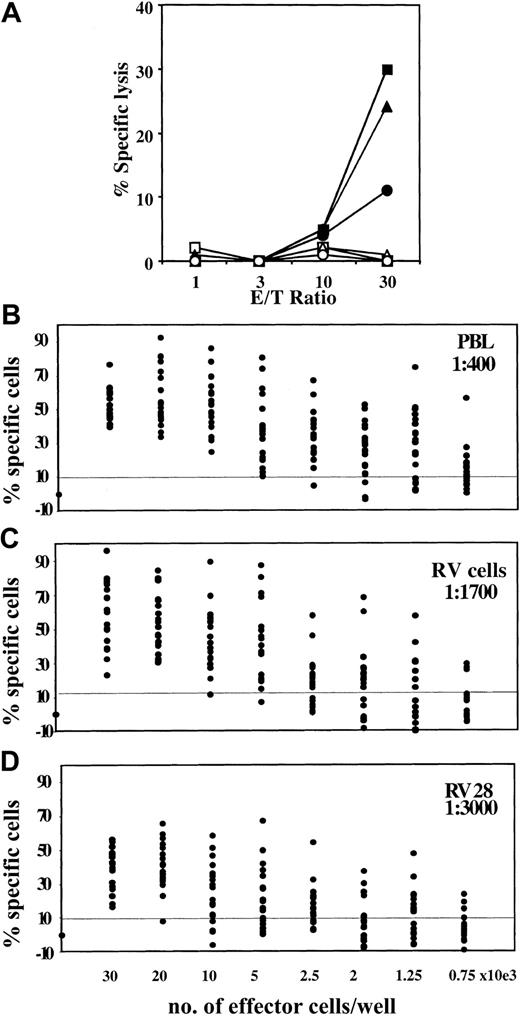
The immune reactivity of genetically modified donor T cells against allogeneic targets was used to further characterize the immune potential of cultured cells. Repeat MLRs confirmed that RV cells have the same lytic activity as PBLs against mismatched target (Figure6). To investigate whether prolonged in vitro manipulation results in alterations of the immune repertoire with a reduction of antiallogeneic effector cells—in addition to PBLs and RV cells transduced with the standard 14-day culture protocol—genetically modified cells obtained by prolonging the culture time to a total of 28 days were tested as source of effectors (RV 28). An MLR was set by stimulating PBLs, RV cells, and RV 28 cells with fully HLA-mismatched irradiated PBMCs. On stimulation, PBL and RV cell effectors exhibited a similar amount of specific lysis, whereas RV 28–derived effectors showed a significant reduction in lytic activity (Figure 7A). To precisely quantify the loss in antiallogeneic precursors induced by prolonged T-cell culture, a more sensitive and quantitative assay, the cytotoxic T-lymphocyte precursor frequency assay (CTLp) was used. Although the frequency of antiallogeneic precursors was already 3- to 4-fold reduced in RV cells (Figure 7C) compared with PBLs (Figure 7B), a more pronounced reduction in the CTLp frequency was observed in RV 28 cells (Figure 7D).
RV cells are as efficient as PBLs in generating antiallogeneic-specific cytotoxic effectors.
PBLs (A) and RV cells (B) were stimulated against fully mismatched irradiated PBMCs. Cytolytic activity was measured in a cold inhibition cytotoxic assay at different E/T ratios against PHA-derived lymphocytes from the same targets (closed symbols). As negative control, cytolytic activity against autologous PHA-derived lymphocytes (open symbols) was measured. Results from 3 experiments are shown.
RV cells are as efficient as PBLs in generating antiallogeneic-specific cytotoxic effectors.
PBLs (A) and RV cells (B) were stimulated against fully mismatched irradiated PBMCs. Cytolytic activity was measured in a cold inhibition cytotoxic assay at different E/T ratios against PHA-derived lymphocytes from the same targets (closed symbols). As negative control, cytolytic activity against autologous PHA-derived lymphocytes (open symbols) was measured. Results from 3 experiments are shown.
Frequency of allospecific CTL precursors is affected by the culture time-span.
(A) MLR of PBLs (squares), standard 14-day cultured RV cells (triangles), and 28-day cultured RV cells (circles; RV 28) against fully mismatched PBMCs was performed. After 1 round of in vitro stimulation, effector cells were tested against the same allogeneic target (closed symbols) and autologous PHA-derived lymphocytes (open symbols) in a standard cytotoxicity assay, performed in cold inhibition. The frequency of CD8+ T-cell precursors elicited in PBLs (B), RV cells (C), and RV 28 cells (D) with 1 round of stimulation with fully mismatched PBMCs was measured by stimulating the effectors in limiting dilution numbers and by performing a cytotoxic assay. Regression curves were interpolated, and precursor frequencies were determined according to Poisson statistics. Precursor frequencies are shown.
Frequency of allospecific CTL precursors is affected by the culture time-span.
(A) MLR of PBLs (squares), standard 14-day cultured RV cells (triangles), and 28-day cultured RV cells (circles; RV 28) against fully mismatched PBMCs was performed. After 1 round of in vitro stimulation, effector cells were tested against the same allogeneic target (closed symbols) and autologous PHA-derived lymphocytes (open symbols) in a standard cytotoxicity assay, performed in cold inhibition. The frequency of CD8+ T-cell precursors elicited in PBLs (B), RV cells (C), and RV 28 cells (D) with 1 round of stimulation with fully mismatched PBMCs was measured by stimulating the effectors in limiting dilution numbers and by performing a cytotoxic assay. Regression curves were interpolated, and precursor frequencies were determined according to Poisson statistics. Precursor frequencies are shown.
The moderate difference in antiallogeneic precursor frequency observed between RV cells and PBLs by the CTLp assay, and not by the MLR assay, probably reflects the different level of sensitivity of the 2 methods. The profound reduction in the CTLp frequency observed using RV 28, detectable already in the MLR assay, suggests that prolonged T-cell culture results in skewing of the antiallogeneic immune repertoire toward oligoclonality.
Ex vivo detection of circulating CD45RA+/LNGFR+ T cells long term after infusion
In a clinical study designed to take advantage of the graft-versus-leukemia (GVL) activity of HSV-tk–transduced donor T cells while controlling GVHD, we have shown that the infusion of donor lymphocytes expressing HSV-tk allows efficient control of GVHD while preserving antitumor potential7 (F.C. et al, manuscript in preparation). In this trial, GVHD did not develop in a significant number of patients, and they did not require GCV-mediated elimination of transduced cells. Some of these patients developed immunity against genetically modified cells, resulting in the elimination of circulating HSV-tk cells7,13 (C.T. et al, manuscript in preparation). However, in patients in whom an immune response against HSV-tk did not develop, long-term persistence of genetically modified cells (more than 60 months) could be documented. Circulating genetically modified T cells were detected at low levels long term after infusion by PCR for HSV-tk, and, when the number of circulating transduced donor lymphocytes reached the levels of FACS sensitivity, characterization of LNGFR+ cells was performed.7 In one patient of this series, characterization of LNGFR+ cells was possible up to 28 months after the last infusion, showing that circulating LNGFR+ T cells were usually CD45RA+ (Figure8). This observation suggests that HSV-tk donor T cells produced under the described manipulation conditions and almost exclusively represented by memory CD45RO+ T cells (Table 1) can persist long term and can revert to a phenotype of terminally differentiated CD45RA+ effectors in vivo. This antigen-dependent differentiation and proliferation process25 32 suggests that genetically modified cells are able to persist long term and to properly react to antigens in vivo. Future studies will be conducted to estimate the frequency and the clinical relevance of this phenomenon.
Ex vivo detection of circulating CD45RA+/ΔLNGFR+ T cells long term after infusion of genetically modified donor cells.
Cytofluorometric analysis of PBLs derived from patient UPN-87 28 months after the last infusion of genetically modified donor lymphocytes. Cells were tested for the coexpression of CD45RA+-FITC /ΔLNGFR+-TC (A, right panel) and CD45RO+-PE/ΔLNGFR+-TC (B, right panel). Appropriate isotypic controls are shown in the left panels.
Ex vivo detection of circulating CD45RA+/ΔLNGFR+ T cells long term after infusion of genetically modified donor cells.
Cytofluorometric analysis of PBLs derived from patient UPN-87 28 months after the last infusion of genetically modified donor lymphocytes. Cells were tested for the coexpression of CD45RA+-FITC /ΔLNGFR+-TC (A, right panel) and CD45RO+-PE/ΔLNGFR+-TC (B, right panel). Appropriate isotypic controls are shown in the left panels.
Discussion
The possibility of exploiting the different kinetics of GVL and GVHD and selectively treating GVHD makes HSV-tk+ donor lymphocytes a potential tool for controlling GVHD while preserving GVL.4,6 Administration of HSV-tk+ donor lymphocytes could have a clinical impact in promoting early immune reconstitution after T-depleted transplantation from a haploidentical donor.10,33 As an alternative strategy to provide immune reconstitution and to reduce the risk for GVHD, T cells specific for viral antigens, such as EBV34,35 or CMV,29have been successfully infused in patients who have undergone transplantation. In contrast to these approaches, the HSV-tk-DLI approach aims at providing immunity against a wide range of pathogens, and potentially neoplastic cells, while controlling GVHD. Moreover, the HSV-tk-DLI approach relies on a faster and easier manipulation method than approaches based on antigen-specific T cells.
Some limitations intrinsic to HSV-tk led to recent investigations of novel, less immunogenic suicide genes such as dimerized Fas36 and CD20.37 However, the HSV-tk/GCV suicide strategy is to date the only suicide switch that reached clinical trials, proving safety and efficacy in controlling GVHD. Given that the infusion of donor lymphocytes after haplo-SCT may require an efficient killing system and may not benefit from a nonimmunogenic protein because of the immune incompetence of recipients, HSV-tk+ RV cells were used to evaluate the immune function of RV cells in this study. However, some of the experiments described in this report were repeated with lymphocytes expressing an alternative suicide gene, resulting in similar findings. To completely exploit the use of RV cells, protocols of in vitro manipulation able to fully preserve T-cell potential are required. In this work, we investigated whether the polyclonal activation, retroviral transduction, immune selection, and expansion in the presence of rhIL-2 affects the immune reactivity of donor CD3+ T cells. The main concerns were AICD, which could skew the immune repertoire,38 and the 14 days of culture in the presence of rhIL-2, which could alter the T-cell repertoire, lead to T-cell exhaustion, or affect the proliferative and effector machinery of T cells.14,39 To reduce the level of AICD, different activation signals were compared. We observed that costimulation with anti-CD3 alone or with anti-CD3 plus anti-CD28 is as efficient as PHA in inducing T-cell proliferation and transduction. In contrast to the findings of Pollock et al,40 we observed no differences in the level of transgene expression after transduction following different stimulation signals. These different results could be attributed to the use of soluble instead of immobilized forms of antibodies, to the different promoters used in the 2 studies, or, less likely, to fibronectin, used by Pollock et al.40 Recent studies reported that AICD could be partially prevented by CD28 engagement through Bcl-Xl up-regulation in activated T cells.26,40 Indeed, results obtained with Annexin V showed that stimulation with anti-CD3 plus anti-CD28 mAb induce a lower level of AICD than PHA (data not shown). Furthermore, because CD28 costimulation provides T cells with signals that prevent the induction of anergy and that promote IL-2 production and clonal expansion,41 42 anti-CD3 in combination with anti-CD28 mAb is to date the ideal activation signal.
Although antigen-specific cytotoxic CD8+ T cells may be the principal effectors for most antitumor and antiviral immune responses, CD4+ cells provide crucial helper functions required to sustain the CD8+ response.43 Even though the CD4/CD8 ratio is inverted in RV cells, both T cell populations are present after gene transfer. Furthermore, RV cells proved to have a broad cytokine secretion pattern with a preferential skew toward TH1/TC1, the T-cell subsets most likely responsible for GVL.44
An efficient T-cell–mediated immune response relies on the presence of a sufficient number of antigen-specific T cells and on the ability of T cells to be specifically activated by exposure to the antigen. Tetramers of the peptide–MHC complex20,45 were used to directly analyze the frequency of T cells of a defined specificity. Furthermore, antigens relevant in allo-SCT were used to evaluate the proliferative and lytic activities of RV cells. Anti-CMV and -EBV immunity were investigated because CMV and EBV cause significant illness and death after SCT46,47 and because viral reactivation can be efficiently treated by donor T cells.29,34 35 Results of this work showed that CTLs specific for viral antigens are preserved after in vitro manipulation, in terms of frequency and level of TCR expression and in terms of ability to proliferate and to kill antigen-expressing cells with the same efficiency and kinetics of PBLs.
Among the antigens relevant in allo-SCT, allogeneic targets are particularly important because they are involved in GVHD,48,49 in the conversion to full donor chimerism,50 and in the prevention and treatment of disease relapse.1,2,34,51 Quantitative assays measuring the frequency of antigen-specific T-lymphocyte precursors by limiting dilution analyses showed a moderate reduction in the frequency of allospecific T cells in RV cells compared with unmodified lymphocytes. The reduction became more relevant when cells were kept in culture for longer times (RV 28). Because no additional stimulation was performed between RV cells and RV 28, AICD should not be implicated in this phenomenon. Conversely, this is probably because of the preferential growth advantage of some clones, resulting in progressive skewing toward oligoclonality.14 However, we cannot exclude that the reduced alloreactivity observed by prolonging the T-cell culture to 28 days could also occur in vivo. Indeed, in a murine model, Drobyski et al39 observed reduced alloreactivity and GVHD potential in transduced lymphocytes compared with unmodified cells. Based on this possibility and in addition to further improvements in gene transfer efficiency and cell manipulation methods, future clinical protocols will ideally involve the use of alternative gene transfer technologies that do not require cell proliferation, such as lentiviral vectors.52
Taken together, these results suggest that a cell manipulation protocol consisting of appropriate cell activation, high transduction efficiency, and short culture results in the preservation of human T cells specific for antigens relevant in the context of allo-SCT. However, the clinical relevance of these observations can only be evaluated by analysis of the in vivo behavior of genetically modified cells. Indeed, in a series of patients who received RV donor lymphocytes to treat disease relapse after SCT,7 we documented the long-term persistence of RV cells. In one patient we could characterize LNGFR+ cells long after infusion and could observe the reversion of the phenotype of infused cells from a “memory” CD45RO phenotype to a CD45RA phenotype. This phenomenon was already observed in HIV+ patients 10 weeks after the infusion of genetically marked T cells from their syngeneic twins.53,54 Antigen-experienced T cells with a CD45RA phenotype have been described,32 and phenotypic and functional analyses have characterized this T-cell subset as terminally differentiated effector T cells.25 In our study, ΔLNGFR+/CD45RA+ cells could be demonstrated in one patient 28 months after the infusion, and transduced circulating cells could be detected at a low level for more than 60 months. Because effector CD45RA+ T cells are generated through an antigen-dependent differentiation and proliferation process, these data suggest the immune competence of RV cells persisting in vivo. A larger number of patients will be studied to confirm this observation and to reveal its clinical relevance. Based on this study, we cannot rule out the possibility that a small proportion of ΔLNGFR+/naive T cells with a CD45RA phenotype has preferentially survived in vivo. Indeed, different investigators reported that naive T cells could be expanded55 and potentially transduced56 in vitro. Although this event is supposed to be quantitatively irrelevant after in vitro polyclonal activation, it could become more visible after challenge in vivo. The long-term persistence of transduced lymphocytes with a naive phenotype could represent a relevant observation for the SCT field and for other gene therapy clinical applications. This will be further investigated and pursued by the development of protocols for lentiviral-mediated T-cell transduction not requiring T-cell activation.
Based on these results and on our previous experience in terms of safety and efficacy of the HSV-tk/GCV strategy,5,7 we propose the use of HSV-tk genetically engineered donor lymphocytes to promote early immune reconstitution after T-cell–depleted SCT from haploidentical donors. The possibility of selectively eliminating cells expressing HSV-tk with GCV could allow the anticipation of immune reconstitution and improvement of the GVL effect by an early infusion of genetically modified cells, potentially in association with immune modulators such as IL-2.57
We thank the physicians and nurses of the Bone Marrow Transplantation Unit, Istituto Scientifico San Raffaele, for patient care, and we thank all the patients and marrow donors who participated in the clinical study. We thank Dr A. Aiuti for helpful discussion and D. Maggioni and E. Zino for excellent technical assistance.
Prepublished online as Blood First Edition Paper, October 3, 2002; DOI 10.1182/blood-2002-08-2351.
Supported by the European Commission (Biomed contract BMH4-CT97-2760, BMH4-CT97-2074, and QLK3-CT-2001-01265); the Italian Association for Cancer Research (AIRC), Milan, Italy; and the Cancer Research Institute, New York, NY.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Chiara Bonini, Cancer Immunotherapy and Gene Therapy Program, Istituto Scientifico H. S. Raffaele, via Olgettina 58, 20132, Milan, Italy; e-mail:bonini.chiara@hsr.it.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal