Protein kinase D (PKD, also known as PKCμ) is closely related to the protein kinase C superfamily but is differentially regulated and has a distinct catalytic domain that shares homology with Ca2+-dependent protein kinases. PKD is highly expressed in hematopoietic cells and undergoes rapid and sustained activation upon stimulation of immune receptors. PKD is regulated through phosphorylation by protein kinase C (PKC). In the present study, we show that PKD is expressed in human platelets and that it is rapidly activated by receptors coupled to heterotrimeric G-proteins or tyrosine kinases. Activation of PKD is mediated downstream of PKC. Strong agonists such as convulxin, which acts on GPVI, and thrombin cause sustained activation of PKC and PKD, whereas the thromboxane mimetic U46619 gives rise to transient activation of PKC and PKD. Activation of PKD by submaximal concentrations of phospholipase C–coupled receptor agonists is potentiated by Gi-coupled receptors (eg, adenosine diphosphate and epinephrine). This study shows that PKD is rapidly activated by a wide variety of platelet agonists through a PKC-dependent pathway. Activation of PKD enables phosphorylation of a distinct set of substrates to those targeted by PKC in platelets.
Introduction
Protein kinase C (PKC) is a family of serine/threonine kinases implicated in the signal transduction of a variety of extracellular stimuli such as hormones and growth factors.1-4 The extended PKC family involves 11 isozymes with structural similarities,5-7 which are divided into subgroups on the basis of structural, enzymatic and regulatory differences.8 The PKC family members are known to have distinct mechanisms of activation, patterns of expression, and subcellular localization in different cell types.8 The conventional PKCs are regulated by Ca2+, sn-1,2-diacylglycerol (DAG), and phospholipids. The novel PKCs lack a Ca2+ binding domain but are regulated by DAG and phospholipids. The atypical PKCs are not known to be regulated by Ca2+ or DAG.9 All of these subgroups have a highly conserved catalytic domain and pseudosubstrate region.3,9,10 PKD (also known as PKCμ) was initially identified as a member of the PKC family,11 creating a new subdivision of PKC.
PKD has similarities to other PKCs in that it has a domain that is homologous to the DAG binding domain of other PKCs, but it lacks the C2 domain responsible for Ca2+ sensitivity of the conventional PKC subgroup.11,12 In contrast to other PKC isoforms, PKD has a putative pleckstrin homology (PH) domain that is reminiscent of those found in the protein kinase B family and is important for regulating PKD's enzyme activity.13,14 Unlike other PKC isoforms that have a highly conserved catalytic domain, PKD's catalytic domain shows a higher degree of homology to the Ca2+-calmodulin–regulated kinases,13 giving it a unique substrate specificity.15,16 These differences and the identification of 2 further PKD isotypes17,18 have made it difficult to classify PKD. It is currently regarded as a member of the PKC family by some groups and has recently been classified as a new novel subgroup of the AGC family of serine/threonine kinases.19
PKD is highly expressed in hematopoietic cells11,15 and is rapidly activated through a phosphorylation-dependent mechanism.20 A variety of stimuli, including phorbol esters and G protein–coupled receptor and tyrosine kinase–linked receptor agonists,21 all lead to sustained PKD activation. Several lines of evidence suggest that this activation is mediated through a PKC-dependent signal transduction pathway.12,20Residues Ser744 and Ser748 in the activation loop of PKD have been shown to be critical sites of phosphorylation that lead to PKD activation and subsequent autophosphorylation at other residues, such as Ser916.22,23 The degree of phosphorylation of Ser916 has been used as a measure of PKD activation using phosphospecific antisera.22-26
In platelets, many receptor agonists lead to activation of PKC via the phosphoinositide second-messenger pathway.27 This involves activation of phospholipase C (PLC), which cleaves phosphatidyl inositol 4,5-bisphosphate, generating the second messengers inositol 1,4,5-trisphosphate (IP3) and DAG. IP3mobilizes Ca2+ from intracellular stores and DAG activates certain isoforms of PKC. Several studies have shown a role for PKC activation in aggregation and dense granular secretion28,29 in response to a variety of agonists. This has been supported by studies that show a correlation between serotonin release from dense granules and phosphorylation of pleckstrin (a marker for PKC activation in platelets).30,31 PKC has also been implicated in platelet adhesion to collagen32 and has been shown to have a direct role in aggregation that is independent of secretion from dense granules.33 In spite of PKC's being implicated in multiple functions during platelet signaling, the role of individual isoforms is still poorly characterized. Purification studies and the use of isoform-specific antibodies have shown that platelets express several isoforms of PKC.34-36 Recent studies in platelets37 have implicated PKCθ in the regulation of Bruton tyrosine kinase. In addition, PKCδ associates with phosphatidylinositol 3-kinase (PI 3–kinase)/γ85 in platelets stimulated with platelet-activating factor.38 There are many other examples, and it is likely that there will be many further examples of PKC isotype-specific functions in platelets in the future.
The objective of the current study was to investigate the regulation of PKD in human platelets. The results provide the first demonstration that PKD is present in platelets and that it is activated by G protein–coupled and tyrosine kinase–linked receptor agonists in these cells. Unusually, activation of PKD in response to some agonists is transient, and we show that PKD activation is dependent on sustained PKC activity. We also demonstrate synergistic activation between submaximal concentrations of agonists that activate PLC by both G protein and tyrosine kinase pathways and agonists that stimulate Gi/z-dependent signaling pathways in platelets.
Materials and methods
Materials
Agonists, inhibitors, and reagents.
Adenosine diphosphate (ADP), apyrase, A3P5P (adenosine 3′-phosphate 5′-phosphate), BAPTA-am (1,2-bis(2-aminophenoxy)ethane-N, N, N, N′, N′-tetraacetic acid), epinephrine, fibrinogen, and wortmannin were obtained from Sigma (Poole, United Kingdom). LY294002 (2-[4-morpholoinyl]-8-phenyl-1[4H]-benzopyran-4-one), phorbol-12-myristate-13-acetate (PMA), and U46619 (9,11-dideoxy-11α,9α.-epoxymethano-prostaglandin F2γ) were from Calbiochem-Novabiochem (Nottingham, United Kingdom). Purified convulxin isolated from the venom of Crotalus durissus terrificus was a gift from Drs M. Leduc and C. Bon (Unite des Venens, Institut Pasteur, Paris, France). Ro 31-8220 (3-[1-(-amidinothio)propyl-1H-indo-3-yl]-3-(1-methyl-1H-indol-3-yl)maleimide, bisindolyl maleimide IX, methanesulfonate) was a gift from Roche Pharmaceuticals (Dr J. Nixon, Welwyn Gardens, United Kingdom) and AR-C67085 (2-propylthio-D-β,γ-dichloromethylene adenosine 5′-trisphosphate) was a gift from AstraZeneca Charnwood (Mr R. Humphries, Loughborough, United Kingdom). Other reagents were from previously described sources.39
Antibodies and substrates.
Rabbit antibodies (Santa Cruz Biotechnology, Santa Cruz, CA) were used for PKD detection. The first (sc639) was raised against a synthetic peptide with an amino acid sequence corresponding to amino acids 899-918 of murine PKD, and the second (sc937) was raised against a peptide mapping to 893-912 of the carboxy terminus of human PKD. PA-1 antiserum, pS916 and syntide-2 were gifts from Dr Doreen Cantrell (Cancer Research UK, London, United Kingdom). The PA-1 antiserum was raised against the synthetic peptide EEREMKALSERVSIL, a sequence from the carboxy terminus of PKD.12 PS916 is a phosphospecific antibody directed against phosphoserine 916 of PKD.23Syntide-2 (PLARTLSVAGLPGKK) is a peptide based on phosphorylation site 2 of glycogen synthase and acts as a substrate for PKD.12,16 20
Methods
Preparation of platelets.
Blood was drawn on the day of the experiment from aspirin-free volunteers into acid citrate dextrose (ACD) as anticoagulant. Studies were carried out with ethical approval from the Central Oxford Research Committee (Ref: C00:203). Washed platelets were prepared essentially as described previously by Gear.40 In brief, platelet-rich plasma (PRP) was obtained by centrifugation at 200g for 20 minutes. Platelets were isolated from PRP by centrifugation at 450g for 15 minutes in the presence of 5% (vol/vol) ACD, 5 U/mL apyrase, 80 nM prostacyclin, and 2.8 μM indomethacin. The pellet was then resuspended in ACD containing 5 U/mL apyrase and 2.8 μM indomethacin and recentrifuged at 450gfor 15 minutes. Platelets were resuspended to a cell density of 1 × 109/mL in HEPES (N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid )–buffered Tyrodes (140 mM NaCl, 5 mM KCl, 15 mM HEPES, 5 mM glucose, 0.4 mM NaH2PO4, 11.9 mM NaHCO3, and 1 mM MgCl2). Platelets were incubated for at least 1 hour at room temperature and just before experimentation 1 mM CaCl2and 0.2 mg/mL fibrinogen were added. All experiments were performed in the presence of the cycloxygenase inhibitor indomethacin (10 μM) to eliminate positive feedback from thromboxanes, with the exception of studies using the thromboxane mimetic U46619. For synergy experiments, where epinephrine was used, inhibition of ADP activity was achieved with the ADP scavenging enzyme apyrase (2 U/mL).
The following drugs were added prior to stimulation of platelets: Ro 31-8220 (1 μM) for 3 minutes; apyrase (2 U/mL) for 1 minute; A3P5P (1 mM) for 1 minute; AR-C67 085 (1 μM) for 1 minute; LY294 002 (20 μM) for 15 minutes; wortmannin (100 nM) for 15 minutes; BAPTA-am (20 μM) for 10 minutes; PP1 (an Src kinase inhibitor; 10 μM) for 10 minutes.
Western blot analysis.
After stimulation, cells were lysed in 2 × Laemmli sample buffer analyzed by 8% sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to polyvinylidene difluoride (PVDF) membranes (Millipore, Bedford, MA). Immunodetection was performed with different antibodies. The Santa Cruz antibodies sc937 and sc639 and the pS916 antisera were used at 1:500 dilution, and the PA-1 antiserum was diluted to 1:100. Immunoreactive bands were visualized by enhanced chemiluminescence.
Immunoprecipitation and in vitro kinase assays.
After stimulation, cells were lysed at 4°C in lysis buffer (50 mM Tris/HCl, pH 7.6; 2 mM EGTA [ethyleneglycoltetraacetic acid]; 2 mM EDTA [ethylenediaminetetraacetic acid]; 2 mM dithiothreitol; protease inhibitors aprotinin (10 μg/mL), leupeptin (100 μg/mL), and pepstatin (0.7 μg/mL); and 1 mM 4-(2-aminoethyl)-benzenesulfonyl fluoride hydrochloride, 2 mM sodium orthovanadate, 1 mM sodium fluoride, 40 mM β-glycero-phosphate, and 1% Triton X-100). Lysates were then centrifuged at 3000gfor 10 minutes at 4°C. PKD was immunoprecipitated from whole cell lysates with the sc937 antibody and recovered with protein A sepharose. PKD immunocomplexes were then washed twice in lysis buffer. Samples were fractioned by SDS-PAGE following transfer to PVDF membrane for Western blotting. For in vitro kinase assays, the immunoprecipitates were washed additionally in 1 mL kinase buffer (30 mM Tris/HCl, pH 7.4; 30 mM MgCl2). The kinase activity of PKD was determined as described previously.24
Phosphatidic acid and pleckstrin phosphorylation.
Phosphatidic acid production was measured as described previously.41 Washed platelets were labeled with32P-orthophosphoric acid (0.5 mCi/mL [18.5 × 106 Bq]) for 1 hour at 37°C. After stimulation, cells were lysed in 2 × Laemmli sample buffer and analyzed by 10% SDS-PAGE, stained with Coomassie blue, destained, and dried down. They were then exposed to hyperfilm overnight. Pleckstrin bands were then excised from the gel and analyzed by scintillation counting.
Data analysis.
Each experiment was performed at least 3 times. Results are expressed as the mean ± SEM and were analyzed by an unpaired Studentt test with P < .05 taken as the minimum value to indicate statistical significance.
Results
PKD is expressed in human platelets
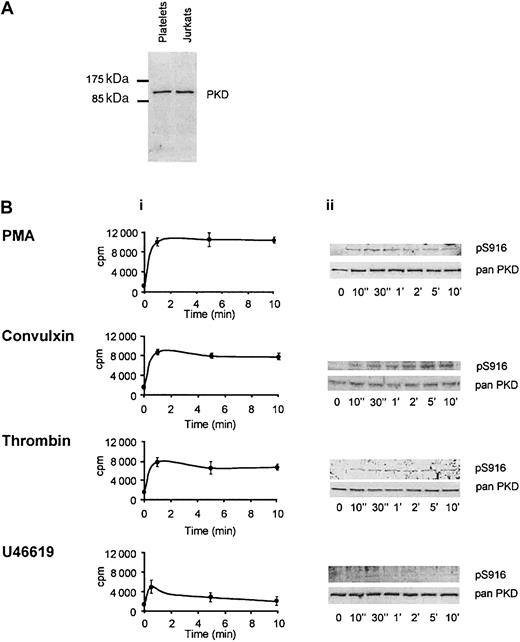
In order to determine the presence of PKD in human platelets, whole cell lysates were analyzed by Western blotting, using 3 separate antibodies that recognize different parts of the COOH-terminal region of this kinase. These antibodies all interact with a protein of 115 kDa, corresponding to the molecular mass of PKD in other cells. An example of the results obtained with one of these antibodies is shown in Figure 1A along with whole cell lysates of Jurkat cells (known to express high levels of PKD) as a control. This demonstrates the presence of PKD in human platelets.
PKD is expressed in human platelets and is activated by PMA, convulxin, thrombin, and U46619.
Washed platelets were treated with indomethacin (10 μM) and apyrase (2 U/mL), with the exception of those activated by U46619, which were treated with apyrase alone. (A) Whole cell lysates from platelets (12.5 × 106 cells) and Jurkat T cells (12.5 × 105 cells) were subjected to SDS-PAGE, transferred to PVDF membrane, immunoblotted with PA-1 antiserum, and visualized by chemiluminescence. Similar results were obtained using 2 other anti-PKD antibodies, sc639 and sc937 (data not shown). One experiment representative of 3 is shown. (B) Time courses of PKD activation were obtained using PMA (30 nM), convulxin (12 nM), thrombin (0.1 U/mL), and U46619 (3 μM). (i) Platelets were lysed and immunoprecipitated with the sc937 antiserum and PKD activity was determined by an in vitro kinase assay using peptide syntide-2 as substrate. Results are shown as the mean ± SEM and are representative of 3 independent experiments, each in duplicate. (ii) Lysates were analyzed by SDS-PAGE and Western blotting with the pS916 antibody, and the Western blots were reprobed with a pan–C-terminal PKD antibody (pan sc639). One experiment representative of 3 independent experiments is shown.
PKD is expressed in human platelets and is activated by PMA, convulxin, thrombin, and U46619.
Washed platelets were treated with indomethacin (10 μM) and apyrase (2 U/mL), with the exception of those activated by U46619, which were treated with apyrase alone. (A) Whole cell lysates from platelets (12.5 × 106 cells) and Jurkat T cells (12.5 × 105 cells) were subjected to SDS-PAGE, transferred to PVDF membrane, immunoblotted with PA-1 antiserum, and visualized by chemiluminescence. Similar results were obtained using 2 other anti-PKD antibodies, sc639 and sc937 (data not shown). One experiment representative of 3 is shown. (B) Time courses of PKD activation were obtained using PMA (30 nM), convulxin (12 nM), thrombin (0.1 U/mL), and U46619 (3 μM). (i) Platelets were lysed and immunoprecipitated with the sc937 antiserum and PKD activity was determined by an in vitro kinase assay using peptide syntide-2 as substrate. Results are shown as the mean ± SEM and are representative of 3 independent experiments, each in duplicate. (ii) Lysates were analyzed by SDS-PAGE and Western blotting with the pS916 antibody, and the Western blots were reprobed with a pan–C-terminal PKD antibody (pan sc639). One experiment representative of 3 independent experiments is shown.
PKD is activated in response to PMA in human platelets
Previous studies have shown that in other cell types PKD is activated downstream of PKC activation, induced by the phorbol ester PMA.42-44 Studies were performed to determine whether PMA could activate PKD in human platelets. Platelets were treated with PMA over a period of 10 minutes and activation of PKD was monitored by an in vitro kinase assay of immunoprecipitated PKD, using syntide-2 as the substrate. Results show a rapid increase in PKD activity as determined by an approximately 5-fold increase in syntide-2 phosphorylation, compared with nonstimulated samples (Figure 1B). This increase was sustained for 10 minutes. Activation of PKD was confirmed by Western blot analysis, using pS916 antisera specific for the phosphorylated, active form (Figure 1B). These 2 separate measures of PKD activity show that in platelets, as in other cells, PKC activation alone (by PMA) is sufficient to stimulate PKD activity.
PKD is activated in response to the platelet agonists convulxin, thrombin, and U46619
Three platelet agonists were tested for their ability to activate PKD. Convulxin selectively activates the tyrosine kinase–coupled collagen receptor glycoprotein VI (GPVI), and thrombin activates protease-activated receptor (PAR) receptors coupled to heterotrimeric Gq and G12/13 proteins. The thromboxane A2 (TxA2) mimetic, U46619, activates platelets through the Gq- and G12/13-coupled thromboxane prostanoid TP receptor. All 3 of these agonists lead to PKC activation via PLC-mediated generation of DAG.45 46 Convulxin and thrombin stimulated a rapid 4- to 5-fold increase in PKD catalytic activity as assessed by an in vitro kinase assay (Figure 1B). PKD activity reached a maximum after one minute of activation by either agonist and was maintained for 10 minutes. Similarly, Western blot analysis using the pS916 antiserum showed phosphorylation of PKD after 10 seconds, which was sustained for at least 10 minutes for convulxin and thrombin (Figure 1B). These results suggest PKD activation as an early event in convulxin and thrombin signaling during platelet activation. PKD was also activated by U46619, but, in contrast to convulxin and thrombin, activation was shown to be weak and transient (Figure 1B).
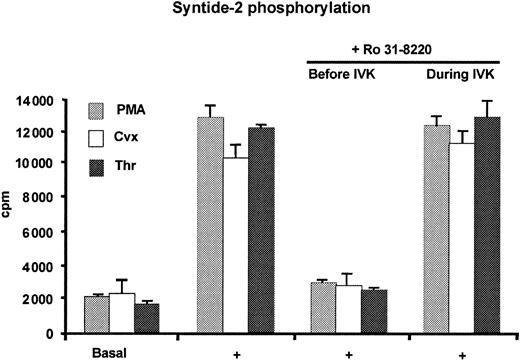
PKD activation is regulated by a PKC-dependent signal transduction pathway in human platelets
In all cells studied so far PKD activation has been shown to be dependent on an active PKC. The next consideration was to assess the role PKC has in the regulation of PKD by receptor stimuli in platelets. Prior to stimulation platelets were preincubated with Ro 31-8220, a potent inhibitor of PKC47 but not PKD.20 21Preincubating platelets with Ro 31-8220 blocked PKD activation induced by PMA, convulxin, and thrombin (Figure2). However, addition of the PKC inhibitor directly to PKD during the in vitro kinase assay did not effect the catalytic activity of PKD itself. These results show that receptor activation of PKD is regulated by a PKC-dependent signaling pathway in platelets. These data also show that in spite of each agonist's having a different mechanism of activation, PKD is a common downstream signaling target during platelet activation.
PKD activity is dependent on a PKC signaling pathway.
Washed human platelets (1 × 109/mL) were treated with indomethacin (10 μM) and apyrase (2 U/mL) and then stimulated (+) with PMA (30 nM), convulxin (12 nM), and thrombin (0.1 U/mL). PKD was then immunoprecipitated from lysed platelets using the sc937 antiserum. PKD activity was determined by in vitro kinase assay (IVK). As indicated, Ro 31-8220 (1 μM) was either added to the platelets prior to treatment with agonist (IVK) or added directly to the IVK assay. PKD activity in the immunocomplexes was measured by syntide-2 phosphorylation. Results are the average of 3 experiments (each in duplicate) and show the mean ± SEM for each agonist.
PKD activity is dependent on a PKC signaling pathway.
Washed human platelets (1 × 109/mL) were treated with indomethacin (10 μM) and apyrase (2 U/mL) and then stimulated (+) with PMA (30 nM), convulxin (12 nM), and thrombin (0.1 U/mL). PKD was then immunoprecipitated from lysed platelets using the sc937 antiserum. PKD activity was determined by in vitro kinase assay (IVK). As indicated, Ro 31-8220 (1 μM) was either added to the platelets prior to treatment with agonist (IVK) or added directly to the IVK assay. PKD activity in the immunocomplexes was measured by syntide-2 phosphorylation. Results are the average of 3 experiments (each in duplicate) and show the mean ± SEM for each agonist.
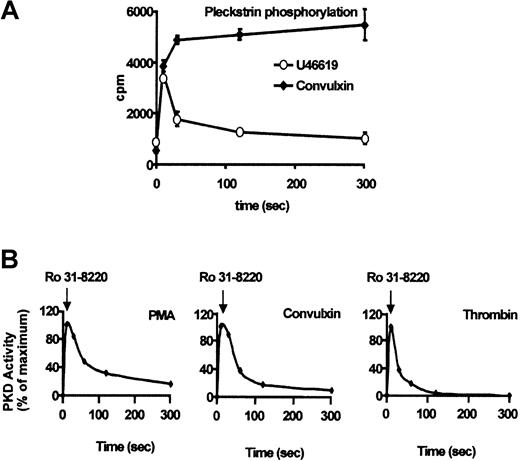
U46619 induces transient activation of PKC
Owing to the transient nature of PKD activation induced by U46619, experiments were designed to assess whether prolonged PKC activation is required to maintain PKD activity. Studies were carried out to observe the activity of PKC by measuring pleckstrin phosphorylation. Results show that convulxin-induced PKC activation was increased 5-fold compared with basal activation and was maintained for 5 minutes (Figure3A). Similar results were observed for thrombin (Figure 4) and PMA (not shown). However, a maximum concentration of U46619 induced a 3-fold increase in pleckstrin phosphorylation (Figure 3A) within 10 seconds of stimulation. This phosphorylation rapidly decreased by approximately 60% after 30 seconds and continued to decrease to less than 10% after 5 minutes. These data show that U46619 is able to transiently activate PKC.
U46619 induces transient activation of PKC.
Platelets were labeled with 32P-orthophosphate for 1 hour prior to stimulation with 12 nM convulxin (as a control) and 3 μM U41669. (A) At various time intervals samples were removed to determine the degree of pleckstrin phosphorylation, as described in “Materials and methods.” Results are shown as the mean ± SEM of 3 independent experiments. (B) Washed platelets were stimulated with PMA (30 nM), convulxin (12 nM), or thrombin (0.1 U/mL) for 10 seconds in the presence of indomethacin and apyrase. A sample was removed and platelets were then treated with Ro 31-8220 (1 μM), with further samples being removed for up to 5 minutes (as indicated). After lysis, platelet whole cell lysates were analyzed by Western blotting (not shown) using the pS916 antiserum, and results were analyzed using densitometry to observe active PKD. Results are expressed as the mean ± SEM of 3 separate experiments.
U46619 induces transient activation of PKC.
Platelets were labeled with 32P-orthophosphate for 1 hour prior to stimulation with 12 nM convulxin (as a control) and 3 μM U41669. (A) At various time intervals samples were removed to determine the degree of pleckstrin phosphorylation, as described in “Materials and methods.” Results are shown as the mean ± SEM of 3 independent experiments. (B) Washed platelets were stimulated with PMA (30 nM), convulxin (12 nM), or thrombin (0.1 U/mL) for 10 seconds in the presence of indomethacin and apyrase. A sample was removed and platelets were then treated with Ro 31-8220 (1 μM), with further samples being removed for up to 5 minutes (as indicated). After lysis, platelet whole cell lysates were analyzed by Western blotting (not shown) using the pS916 antiserum, and results were analyzed using densitometry to observe active PKD. Results are expressed as the mean ± SEM of 3 separate experiments.
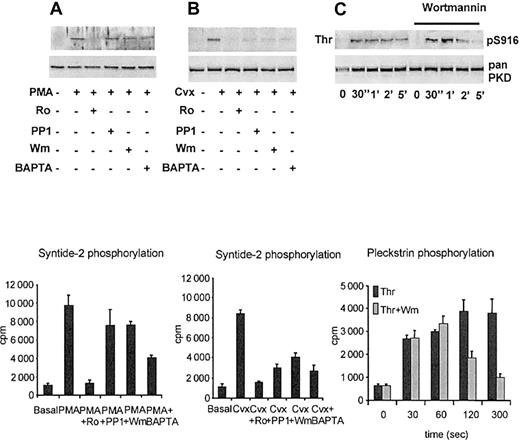
Signaling components involved in PKD activation.
Washed human platelets (1 × 109/mL) were pretreated with 1 μM Ro 31-8220 (Ro), 10 μM PP1, 100 nM wortmannin (Wm), and 20 μM BAPTA-am (BAPTA), prior to activation with 30 nM PMA (panel A) or 12 nM convulxin (Cvx; panel B), for 1 minute at 37°C. Samples from whole cell lysates were analyzed by Western blotting using pS916 following lysis of the cells with 2 × sample buffer. Results are representative of the mean ± SEM of 3 experiments. The remaining cells were lysed and immunoprecipitated using the pan sc937 antibody. PKD activity immunoprecipitated from whole cell lysates was measured by in vitro kinase assay using syntide-2 as substrate. Results shown are the mean ± SEM of 3 independent experiments with duplicate samples from each. (C) Platelets were lysed and analyzed by SDS-PAGE and Western blotting with the pS916 antibody and the Western blots were reprobed with a pan–C-terminal PKD antibody (pan sc639). One experiment representative of 3 independent experiments is shown. Platelets were labeled with 32P-orthophosphate for 1 hour prior to stimulation with 0.1 U/mL thrombin (Thr) or 0.1 U/mL thrombin preincubated with 100 nM wortmannin (Wm). At various time intervals samples were removed to determine the degree of pleckstrin phosphorylation, as described in “Materials and methods.” Results are shown as the mean ± SEM of 3 independent experiments.
Signaling components involved in PKD activation.
Washed human platelets (1 × 109/mL) were pretreated with 1 μM Ro 31-8220 (Ro), 10 μM PP1, 100 nM wortmannin (Wm), and 20 μM BAPTA-am (BAPTA), prior to activation with 30 nM PMA (panel A) or 12 nM convulxin (Cvx; panel B), for 1 minute at 37°C. Samples from whole cell lysates were analyzed by Western blotting using pS916 following lysis of the cells with 2 × sample buffer. Results are representative of the mean ± SEM of 3 experiments. The remaining cells were lysed and immunoprecipitated using the pan sc937 antibody. PKD activity immunoprecipitated from whole cell lysates was measured by in vitro kinase assay using syntide-2 as substrate. Results shown are the mean ± SEM of 3 independent experiments with duplicate samples from each. (C) Platelets were lysed and analyzed by SDS-PAGE and Western blotting with the pS916 antibody and the Western blots were reprobed with a pan–C-terminal PKD antibody (pan sc639). One experiment representative of 3 independent experiments is shown. Platelets were labeled with 32P-orthophosphate for 1 hour prior to stimulation with 0.1 U/mL thrombin (Thr) or 0.1 U/mL thrombin preincubated with 100 nM wortmannin (Wm). At various time intervals samples were removed to determine the degree of pleckstrin phosphorylation, as described in “Materials and methods.” Results are shown as the mean ± SEM of 3 independent experiments.
To investigate this further, studies were carried out to observe the activity of PKD upon PKC inhibition. Ro31-8220 was added to platelets 10 seconds after stimulation by PMA, convulxin, or thrombin, and the level of PKD autophosphorylation was measured using the antiphosphoserine antibody p5916. The bands on the resulting autorad were quantified using densitometry and were plotted versus time (Figure3B). The phosphorylated state of PKD decreased with time for all 3 stimuli, showing that PKC must remain active to maintain PKD activity. These results suggest that PKD activation is regulated by a PKC-dependent signaling pathway and that continued PKC activity is necessary for sustained PKD activation in platelets. It is therefore clear that transient PKD activation in response to U46619 is the result of transient PKC activation induced by this agonist.
Other signaling pathways that contribute to PKD activation
Other components of the signaling pathway leading to PKD activation by PMA and convulxin were investigated by determining the effects of preincubating platelets with the Src kinase inhibitor PP1, the PI 3-kinase inhibitors LY294002 (not shown) and wortmannin, and the calcium chelator BAPTA-am (Figure 4). For the phorbol ester, PMA (Figure 4A), there was a small but not significant decrease in PKD activation in the presence of inhibitors of PI3-kinase or Src kinases. There was also approximately 50% inhibition of PKD activation in the presence of the Ca2+ chelator BAPTA-am, consistent with a role for the cation in the activation of PKC. Convulxin-induced PKD activation (Figure 4B) was inhibited to almost basal levels in the presence of Src kinase inhibition or calcium chelation, whereas PI 3–kinase inhibition decreased PKD activation by more than 60%. This is not surprising, because activation of PLCγ2, by GPVI, is critically dependent on Src kinases48,49 and is modified in part via PI 3–kinase.39
Thrombin-induced PKD activation was shown to be dependent on PI 3–kinase and Ca2+ with more than 60% attenuation of PKD activation in the presence of wortmannin or BAPTA-am after 2 minutes (Figure 4 and not shown). A time course of the effects of wortmannin on thrombin-induced PKD activation was compared with thrombin-induced PKC activation (pleckstrin phosphorylation). The results (Figure 4C) show that PKD activation is maintained for 1 minute and is attenuated significantly after 2 minutes, returning to basal levels after 5 minutes. This suggests a role for PI 3–kinase or its products in later stages of PKD regulation. The same pattern of regulation was observed for PKC activation and correlates well with published data50 51 showing a role for PI 3–kinase in the later stages (after 2 minutes) of pleckstrin phosphorylation downstream of the thrombin PAR receptors (Figure 4C).
Gi/Gz involvement in activation of PKD
Previous work has suggested synergistic activation of platelets by submaximal concentrations of agonists that activate Gq- and Gi/z-dependent signaling pathways.52-56 The pathways activated by Gi/z are not defined but are likely to include PI 3–kinase.39 57 To test this possibility, PKD activation by epinephrine (which activates both Gi- and Gz-linked pathways via the α2A-adrenoceptor) and ADP (which activates both Gq-[via the P2Y1 receptor] and Gi-[via the P2Y12 receptor] coupled pathways) was determined. Epinephrine was unable to activate PKD even at high concentrations (Figure 5A-Bi). However, a submaximal concentration of U46619, which was unable to cause PKD activation alone, stimulates a 4-fold increase in PKD activation in the presence of epinephrine (Figure 5A-Bi). Similar experiments carried out with a high concentration of ADP (Figure 5A-Bii) show that activation of Gq and Gi/z-coupled ADP receptors is required for PKD activation. In the presence of selective ADP receptor antagonists A3P5P (which blocks P2Y1) or AR-C67085 (which blocks P2Y12), there was no activation of PKD. These results reveal that signals from Gi/z- and Gq-coupled receptors can act together to activate PKD.
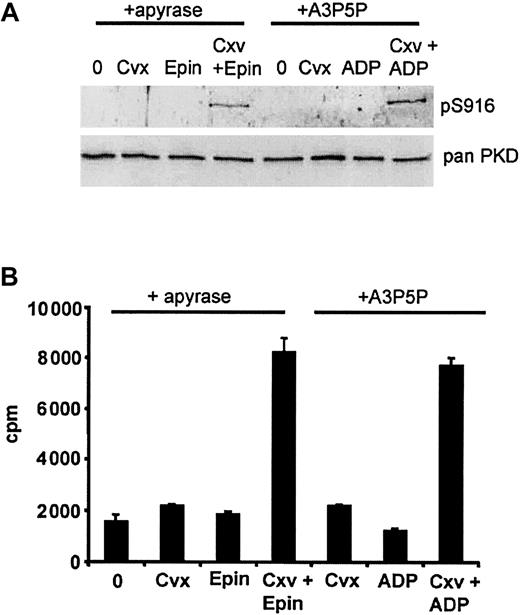
Synergy between GPVI and Gi/z leads to PKD activation
Previous work has shown synergy between the tyrosine kinase pathway activated by GPVI and a Gi/z-coupled pathway during platelet aggregation,33,58 59 and so the possibility of synergy between these signaling pathways to activate PKC and thereafter PKD was monitored. A submaximal concentration of convulxin, which on its own stimulated a small increase in PKD activation, was potentiated 4-fold in the presence of ADP (+A3P5P) or epinephrine, as determined by Western blot analysis and in vitro kinase assays (Figure6). These results demonstrate that concomitant signals from Gi/z-coupled receptors and GPVI can act together to stimulate PKD activation.
Synergy between Gq- and Gi-coupled receptors to activate PKD.
(A) Washed platelets were resuspended to a concentration of 1 × 109/mL. Those activated with ADP or ADP receptor antagonists were treated with the cyclooxygenase (COX) inhibitor indomethacin (10 μM) and those stimulated with U46619 or epinephrine were treated with the ADP scavenging enzyme apyrase (2 U/mL). Platelets were stimulated with threshold concentrations of (i) U46619 (0.1 μM), epinephrine (10 μM), and both agonists together, or maximum concentrations of (ii) ADP (20 μM)+ 1 μM AR-C67085 (ARC), ADP (20 μM)+ 1 mM A3P5P (A3P) and ADP (20 μM) alone for 1 minute. Western blot analysis was performed using pS916 following lysis of cells with 2 × sample buffer. Lysates from cells stimulated for 1 minute with 30 nM PMA were used as a positive control. Results show the mean ± SEM of results from 3 different donors. (B) Platelets were lysed and PKD activity was assayed by in vitro kinase assay (as described in “Materials and methods”). Results are the mean ± SEM of 3 separate experiments, and each sample was in duplicate.
Synergy between Gq- and Gi-coupled receptors to activate PKD.
(A) Washed platelets were resuspended to a concentration of 1 × 109/mL. Those activated with ADP or ADP receptor antagonists were treated with the cyclooxygenase (COX) inhibitor indomethacin (10 μM) and those stimulated with U46619 or epinephrine were treated with the ADP scavenging enzyme apyrase (2 U/mL). Platelets were stimulated with threshold concentrations of (i) U46619 (0.1 μM), epinephrine (10 μM), and both agonists together, or maximum concentrations of (ii) ADP (20 μM)+ 1 μM AR-C67085 (ARC), ADP (20 μM)+ 1 mM A3P5P (A3P) and ADP (20 μM) alone for 1 minute. Western blot analysis was performed using pS916 following lysis of cells with 2 × sample buffer. Lysates from cells stimulated for 1 minute with 30 nM PMA were used as a positive control. Results show the mean ± SEM of results from 3 different donors. (B) Platelets were lysed and PKD activity was assayed by in vitro kinase assay (as described in “Materials and methods”). Results are the mean ± SEM of 3 separate experiments, and each sample was in duplicate.
Synergy between GPVI and Gi leading to PKD activation.
Indomethacin (10 μM)–treated platelets were resuspended to a density of 1 × 109/mL. These were then split into 2, and half were pretreated with apyrase (2 U/mL). (A) Platelets minus apyrase were then stimulated with threshold concentrations of convulxin (cvx; 2 nM) or ADP (1 μM) in the presence of the P2Y1 receptor antagonist (1 mM A3P5P) and the agonist combination. Similarly, platelets treated with apyrase were activated by threshold concentrations of convulxin (Cvx; 2 nM) or epinephrine (Epin; 10 μM) and both together. Aliquots were removed from each sample after 1 minute and subjected to Western blot analysis using pS916 antisera to determine PKD activity. One experiment representative of 3 is shown. (B) In parallel, PKD was immunoprecipitated from the remaining sample for an in vitro kinase assay to observe syntide-2 phosphorylation. Results are the mean ± SEM of 3 independent experiments, carried out in duplicate.
Synergy between GPVI and Gi leading to PKD activation.
Indomethacin (10 μM)–treated platelets were resuspended to a density of 1 × 109/mL. These were then split into 2, and half were pretreated with apyrase (2 U/mL). (A) Platelets minus apyrase were then stimulated with threshold concentrations of convulxin (cvx; 2 nM) or ADP (1 μM) in the presence of the P2Y1 receptor antagonist (1 mM A3P5P) and the agonist combination. Similarly, platelets treated with apyrase were activated by threshold concentrations of convulxin (Cvx; 2 nM) or epinephrine (Epin; 10 μM) and both together. Aliquots were removed from each sample after 1 minute and subjected to Western blot analysis using pS916 antisera to determine PKD activity. One experiment representative of 3 is shown. (B) In parallel, PKD was immunoprecipitated from the remaining sample for an in vitro kinase assay to observe syntide-2 phosphorylation. Results are the mean ± SEM of 3 independent experiments, carried out in duplicate.
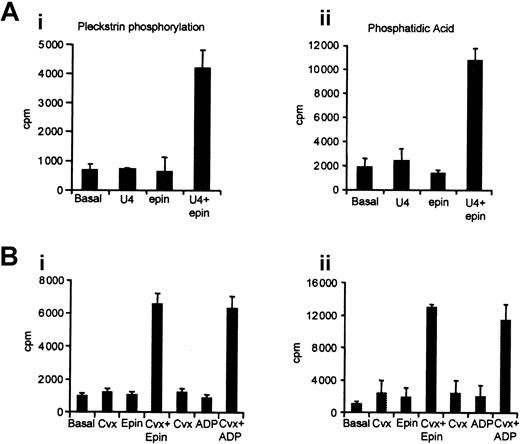
Synergistic activation of PKD is at the level of PKC activity
The signals from Gi/z that synergize with Gq- or tyrosine kinase (TK)–linked signaling pathways to activate PKD either could be at the level of PKC activation or could represent a separate input directly into PKD activation. To explore these possibilities, PKC activation was assessed by pleckstrin phosphorylation and PLC activity by phosphatidic acid (PA) production. PA is generated in cells by phosphorylation of DAG and so can be used as an indirect measure of DAG levels or PLC activation.60In both cases a marked potentiation was seen between submaximal concentrations of convulxin or U46619 and epinephrine, at the level of both pleckstrin phosphorylation and phosphatidic acid production (Figure 7). The same results were found when using ADP in the presence of A3P5P, rather than epinephrine, as a selective Gi/z agonist. Thus, activation of Gi/z leads to potentiation of PLC activation by Gq- and TK-linked pathways, which subsequently leads to PKC, then PKD, activation.
Synergistic activation of pleckstrin phosphorylation and phosphatidic acid production.
Platelets were labeled with 32P-orthophosphate for 1 hour prior to stimulation with submaximal concentrations of 0.1 μM U46619, 10 μM epinephrine (Epin), or both together (panel A) or 2 nM convulxin (Cvx), 10 μM epinephrine (Epin), or both together (panel B). Samples were harvested after 1 minute to determine the degree of pleckstrin phosphorylation (i) or phosphatidic acid production (ii), as described in “Materials and methods.” Results are the mean ± SEM of 3 independent experiments.
Synergistic activation of pleckstrin phosphorylation and phosphatidic acid production.
Platelets were labeled with 32P-orthophosphate for 1 hour prior to stimulation with submaximal concentrations of 0.1 μM U46619, 10 μM epinephrine (Epin), or both together (panel A) or 2 nM convulxin (Cvx), 10 μM epinephrine (Epin), or both together (panel B). Samples were harvested after 1 minute to determine the degree of pleckstrin phosphorylation (i) or phosphatidic acid production (ii), as described in “Materials and methods.” Results are the mean ± SEM of 3 independent experiments.
Discussion
Identifying potential kinases activated downstream of platelet receptor stimulation allows a greater understanding of platelet signal transduction. This study implicates PKD as a signaling molecule in the regulation of platelet function. PKD was initially identified as a member of the PKC superfamily but can be distinguished from other PKC isoforms because of differences in its catalytic domain structure, giving it unique substrate specificity.2467 Most important, PKD activation is mediated by phosphorylation by other members of the PKC family, rather than by direct interaction with DAG.62 63 The magnitude and duration of PKD activation by maximal concentrations of PMA, convulxin, and thrombin is more or less identical. Also, all 3 stimulate PKD activation via PKC. This shows PKD as a common point of signal amplification downstream of tyrosine kinase– and Gq-coupled receptors.
Convulxin-induced PKD activation was partially dependent on PI 3–kinase and entirely dependent on the Src kinases.48,64Because activation of PLCγ2 downstream of GPVI has similarly been shown to be dependent on these activities, this presumably reflects the degree of PKC activation in the presence of these inhibitors. Thrombin-induced PKD activation was also attenuated by the presence of the structurally different65 PI 3–kinase inhibitors LY294002 and wortmannin after 2 minutes of activation. This is consistent with previous reports of a role for PI 3–kinase in later stages of regulation of PKC by thrombin as shown by measurements of phosphorylation of pleckstrin.51
PKD activation is transient in response to weak platelet agonists U46619 (present study) and ADP (data not shown). This is likely to be the result of these agonists' activating PKC only temporarily, as sustained PKC activity is required to maintain PKD activation. After treatment with convulxin, thrombin, and PMA, a subsequent addition of Ro 31-8220 led to a loss of PKD activity, suggesting that a phosphatase is active in platelets that can reverse PKD activation unless the PKC stimulus remains. Transient PKC activation was confirmed by measurements of phosphorylation of pleckstrin, an alternative PKC substrate in platelets. This transient regulation of PKD activation in response to weak agonists is unusual, as in other systems PKD activation is sustained.62 66
It is well established that synergy between signaling pathways can lead to platelet activation.55,58 Therefore, investigations were undertaken to identify whether synergy between signals from 2 separate receptors can activate PKD. The results presented here identify synergy through Gi/z and Gq and between Gi/z and GPVI leading to PLC and PKD activation in platelets. This synergy was also apparent when investigating PKD activation in response to ADP. Results show that activating either the P2Y1 receptor coupled to Gq or the P2Y12 receptor coupled to Gi/z was unable to activate PKD alone. This is different from the results observed for other Gq-coupled receptor agonists in this study (thrombin, U46619) and is likely to be due to the low number of P2Y1receptors on the platelet surface. Previous studies have implied that PI 3–kinase is an important component of the synergy between Gi/z and Gq in the regulation of platelet aggregation,55,58 65 and this may also be the case for synergy at the level of PKC/PKD activation.
These studies demonstrate activation of PKD downstream of GPVI and thrombin-dependent Gq signaling, in a PKC-dependent manner. PKD is a novel PKC substrate in platelets that phosphorylates a different recognition motif from that phosphorylated by PKC, enabling regulation of a different set of proteins from those targeted by PKC in platelets. A number of pathways that have been previously ascribed to PKC could in fact be regulated via PKD, because activation of PKC always leads to PKD activation. This could potentially include all of the roles involving PKC where the functional mechanisms remain ill-defined, such as aggregation and adhesion. Presently, however, there are no tools, such as selective inhibitors or mutant mice, to enable determination of the role of PKD function compared with the role of PKC in platelets. Future studies need to be performed to investigate whether PKC or PKD is responsible for a number of the effects downstream of PLC activation in platelets.
We are grateful to Dr Doreen Cantrell for pS916 and syntide-2, and for lots of helpful advice; to Ben Atkinson, who helped with the earlier studies; and to Dr Ulrica Marklund for lots of support and excellent advice.
Prepublished online as Blood First Edition Paper, October 10, 2002; DOI 10.1182/blood-2002-08-2384.
Supported by a British Heart Foundation (BHF) Studentship (M.J.S.) and a BHF Senior Research Fellowship (S.P.W.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Margaret J. Stafford, Department of Biochemistry, University of Oxford, South Parks Road, Oxford, OX1 3QU, United Kingdom; e-mail: margaret@bioch.ox.ac.uk.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal