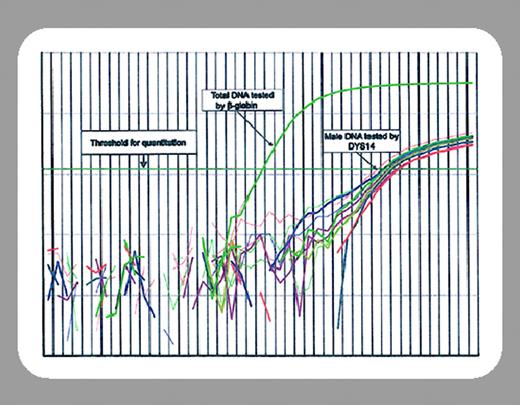
Fetal microchimerism (FMc) describes the persistence of low numbers of fetal cells in the mother after a pregnancy. A number of recent studies suggests FMc may play a role in the etiology of some autoimmune diseases.1 Remarkably, FMc has been demonstrated to persist for up to 38 years after pregnancy and has been found in multiple lymphocyte subsets and in early lymphoid precursors.2 In a single patient, FMc was demonstrated in CD34+ cells, suggesting that FMc may result from the engraftment of a long-term repopulating or stem cell.3 In this issue of Blood, Adams and colleagues (page 3845) have taken the next step and evaluated female hematopoietic cell (HC) transplant donors for the presence of Y chromosome-specific DNA. Strikingly, Y chromosome DNA could be detected in more than one third of peripheral blood stem cell (PBSC) collections and nearly one half of the CD34+ selected cell fractions from these female donors. Since the use of multiparous female donors is associated with a higher propensity of graft-versus-host disease (GVHD),4 the authors speculate that major histocompatibility complex (MHC)-mismatched fetal cells transferred during HC transplantation (HCT) could participate in the induction of GVHD. Unfortunately, a number of factors are lacking from this dataset to completely address such questions. For instance, parity information is not available for most donors, and the assay used detects only male DNA; thus, the actual incidence of FMc in hematopoietic stem cell factions may be significantly higher than is estimated by this analysis. Likewise, it is not known whether female donors with demonstrable FMc induced a greater incidence of GVHD than other donors in this series.FIG1
Despite this, and like all good science, this work raises more questions than it answers. For instance, virtually nothing is known about the circumstances that allow FMc to occur. Other important questions include what role do such cells play in the pathogenesis of either acute or chronic GVHD. If the hypothesis by Adams et al is correct, then it may be possible to detect the presence of transferred fetal cells in the host after HCT (possibly in GVHD target tissues). To date there have been no reports of chimerism analysis after HCT demonstrating a party other than the donor or recipient, but the studies by Adams et al may prompt such reports.
Not only have fetal cells been detected in the mother, but also maternal cells in the fetus.5 Such microchimerism might not be all bad for patients requiring HCT, since it might aid, or even enhance, donor selection. This is because a potential sibling donor (with maternal microchimerism) may be tolerant of noninherited maternal antigens, allowing for less rigorous typing of maternal alleles. Similarly, mothers who have had multiple pregnancies (and hence FMc from more than one child) may be tolerant of paternal antigens. Such parents may be ideal donors for their children. In fact, Shimazaki et al have reported a technique of donor selection based on microchimerism analysis to perform haploidentical, 2 to 3 antigen mismatched, non-T-cell-depleted HCT.6 In this series of 5 patients the incidence of severe (grades 3-4) GVHD was remarkably low (1 of 5 patients). Thus, it is hopeful that the findings by Adams et al may be useful in the understanding of FMc and how (or if) it relates to the pathogenesis of GVHD and whether such information may assist in the selection of HC transplant donors.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal