In the fourth act of Shakespeare's darkest tragedy, the Scottish thane Macbeth—lately elevated to the national throne upon Duncan's betrayal and murder—enters a remote cave in order to consult 3 witches regarding his ultimate fate. To assist their divination, these “weird sisters” brew up a fantastic potion in a seething cauldron, a double-boiled concoction embracing several rather exotic ingredients:
Eye of newt and toe of frog, Wool of bat and tongue of dog, Adder's fork and blind-worm's sting, Lizard's leg and howler's wing, For a charm of pow'rful trouble, Like a hell-broth boil and bubble.1
After more than a century of research and nearly 4 decades of clinical use, the animal-derived antilymphocyte sera (antilymphocyte globulin [ALG] and antithymocyte globulin [ATG]) are still viewed by some as retaining traces of the baffling aura of a witch's stew. The great Russian immunologist Élie Metchnikoff is credited with being first (in 1899) to have had the idea to grind up rat spleens and inject fragments into guinea pigs in order to produce a hyperimmune serum.2 Metchnikoff found that this serum was able to agglutinate and destroy rat leukocytes—first the mononuclear cells, followed by the polymorphonuclear cells—and he used this evidence to support his long-standing contention about the primacy of phagocytes in the immune response.3 Manufacturing practices have advanced considerably since the late Victorian era, and the antilymphocyte/antithymocyte immunoglobulin preparations now available for clinical use in the US (Pfizer's equine ATGAM [New York, NY] and Sangstat-Genzyme's rabbit-derived Thymoglobulin [Cambridge, MA]) are, of course, sterile and purified of contaminants, with quality carefully controlled. Yet just how these agents actually work remains nearly as opaque as the uncanny supernatural aptitude of those 11th-century Scottish witches.
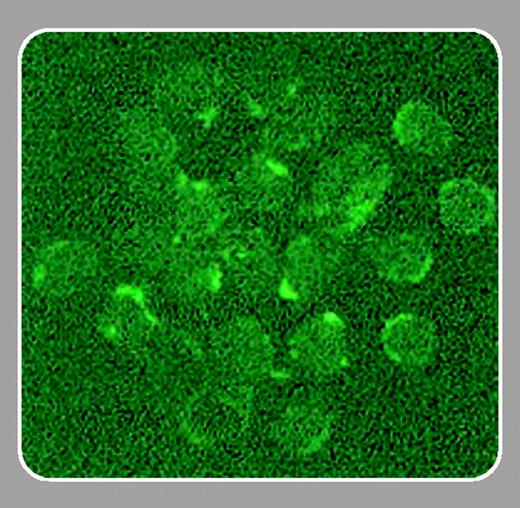
There can be no argument about the fact that ALG and ATG do work. ALG was a key element underpinning the early success of solid organ transplantation in the 1960s and 1970s, and just as it began to yield ground to cyclosporin A and monoclonal anti-T-cell antibodies in the early 1980s, it found new roles combating graft-versus-host disease (GVHD) in the bone marrow transplant unit and treating aplastic anemia. Recently, there have been reports that ATG also benefits some patients with myelodysplastic syndrome,4 although work continues toward defining just who among that needy group are most likely to enjoy a drug response5 ; unfortunately, our predictions there are not yet as eerily accurate as the sooth-saying of Macbeth's witches.FIG1
In this issue of Blood, Michallet and colleagues (page 3719) extend previous observations concerning ATG-associated T-cell apoptosis and report new evidence for the release of cathepsin B into the lymphocyte cytoplasm after ATG exposure. The latter finding is novel and interesting, and may open a new line of investigation into the drug's mechanism. To a lymphocyte, having active cathepsin B spill into the cytoplasm is as lethal as Lady Macbeth's ambitions—though the ultimate outcome in this case is cellular suicide instead of homicide.
Some might despair of ever precisely defining the mechanism of ATG—one group of investigators has reported that rabbit ATG has 23 different major antibody specificities6 —and batch-to-batch variability in preparation potency and product properties continue to be problematic. But the report by Michallet and colleagues is certainly a strong step toward achieving a better molecular understanding of these strange sera— and banishing any lingering airs of witchcraft.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal