Abstract
The reported outcome of hematopoietic stem cell transplantation (HSCT) from HLA-mismatched family members has been inconsistent. The object of this study was to evaluate the true impact of HLA-mismatch by using recent data from a homogenous population, excluding HSCT procedures that used graft manipulations, and by considering genotypic matching. Clinical data of 2947 patients who underwent allogeneic HSCT for leukemia or myelodysplastic syndrome were extracted from the database of the Japan Society for Hematopoietic Cell Transplantation. The main outcome measures were survival and the incidence of graft-versus-host disease (GVHD). The presence of serologic HLA-mismatch, higher age, and high-risk disease were identified as independent risk factors for both shorter survival and the development of grade III to IV acute GVHD. The impact of HLA-mismatch on survival was more relevant in standard-risk patients. These findings persisted when we used genotypic HLA matching. Survival after one-locus–mismatched HSCT was equivalent to that after HLA-matched unrelated HSCT. We concluded that when a one-locus–mismatched family donor is available for high-risk patients, immediate HSCT using this donor is warranted. In standard-risk patients, however, survival after one-locus–mismatched HSCT is significantly shorter than that after HLA-matched HSCT, and the indications for HSCT should be considered carefully.
Introduction
Hematopoietic stem cell transplantation (HSCT) from HLA-identical siblings is an established treatment for hematologic malignancies. However, in most developed countries such donors are available for only approximately 30% of patients.1,2 Therefore, hematopoietic stem cell transplants from family members other than HLA-matched siblings or unrelated volunteers has been investigated. The advantages of family members over unrelated donors are immediate availability and the ability to collect additional donor cells for immunotherapy.
A mismatch in HLA antigens between the donor and recipient increases the risk of both graft rejection and graft-versus-host disease (GVHD) after HSCT. There have been several reports regarding the outcome of HSCT from family members other than HLA-matched siblings.3-10 Reports from Seattle showed that the probability of survival for patients who underwent one-locus–mismatched HSCT from family members was similar to that of patients who received grafts from HLA-identical siblings, because the increased risk of GVHD was counterbalanced by an increase in the graft-versus-leukemia effect.3,6 In contrast, in a large study from the International Bone Marrow Transplant Registry (IBMTR), leukemia-free survival for patients who received grafts from one-locus–mismatched family donors was significantly shorter than that for patients who received grafts from HLA-identical siblings.10 This discrepancy could be explained by the difference in the method for HLA typing. In the IBMTR report, matching at the HLA-DR locus was based exclusively on serologic data, whereas the Seattle group assigned HLA-D antigens by testing the donors, recipients, and available family members with homozygous typing cells.3,10 Therefore, some donor-recipient pairs that were considered to be mismatched for only one HLA locus in the IBMTR report might actually be more genetically disparate than those in the Seattle report.1
Recently, molecular techniques have made it possible to identify HLA alleles that cannot be identified serologically (genomic typing).11,12 Several groups have reported that a genotypic mismatch at DRB1 allele increased the risk of acute GVHD in HSCT from serologically HLA-matched unrelated donors.13,14 On the other hand, a Japanese study showed that genotypic incompatibility for class I HLA was more important than class II mismatch as a predictor of severe acute GVHD.15 These findings suggest the importance of genomic typing and the possibility that HLA mismatch may have different effects on the outcome of HSCT among ethnic groups. However, no previous studies have examined the outcome of HSCT using HLA-mismatched family donors considering genotypic HLA mismatches. Furthermore, studies based on registry data have included the outcome of HSCT from various countries as well as HSCT using ex vivo graft manipulation, including T-cell depletion or CD34+ cell selection, which can strongly affect the incidence of acute GVHD.
The object of this study was to evaluate the true impact of HLA mismatch by using recent data from a homogenous population, excluding HSCT procedures that used graft manipulations, and by considering data on genotypic HLA mismatch. We also aimed to clarify the impact of class I versus class II mismatch on the outcome of HSCT from HLA-partially mismatched family donors.
Patients and methods
Study population
A total of 3356 patients who underwent allogeneic HSCT from a family donor for the first time between 1991 and 2000 for chronic myelocytic leukemia (CML), acute myeloblastic leukemia (AML), acute lymphoblastic leukemia (ALL), or myelodysplastic syndrome (MDS) were reported to the Japan Society for Hematopoietic Cell Transplantation (JSHCT).16 Those younger than 16 year of age, those who received a graft from a syngeneic donor, those who received a manipulated graft, and those who received cord blood were excluded from the study. Finally, full serologic HLA datasets for HLA-A, -B, and -DR loci were available in 2947 patients.
After the completion of the following analyses regarding HSCT from a family donor, data of 1002 patients, who underwent HSCT from a serologically HLA-matched unrelated donor and fulfilled the conditions cited, were additionally extracted from the database of JSHCT. Unrelated HSCT exclusively used a bone marrow graft.
Transplantation procedure
The conditioning regimen before HSCT was mainly either a cyclophosphamide/total body irradiation (TBI)–based regimen (49%) or a busulfan/cyclophosphamide-based regimen (43%). Prophylaxis for GVHD mainly consisted of a combination of cyclosporine A and methotrexate (87%). Other prophylactic regimens were cyclosporine A with prednisolone (4%), tacrolimus with methotrexate (4%), and so on.
Histocompatibility
Data on serologic typing for HLA-A, -B, and -DR loci were obtained from reports from the institutions performing the transplantations. Genomic typing was performed at the discretion of the attending physicians at each institute. In pairs without data for genomic typing, we estimated genotype donor-recipient matching as follows.
Serologically HLA-matched sibling pairs were considered to be genotypically HLA-identical. In fact, 65 serologically HLA-matched sibling pairs underwent genomic typing of HLA-A, -B, and -DRB1 alleles, and all were completely matched. Another 302 serologically HLA-matched sibling pairs were tested only for DRB1 alleles and a mismatch was found in only one donor-recipient pair (1501 of 1501 versus 1501 of 1502).
In pairs other than serologically HLA-identical sibling pairs, loci that were serologically matched and were known to be associated with less than a 5% risk of genotype mismatch in the Japanese population were considered to be genotypically matched loci.17 On the other hand, loci that were serologically matched but were known to be associated with a 5% or greater risk of genotype mismatch (A2, A26, B13, B39, B61, B62, DR4, DR8, DR12, DR13, DR14, and DR15) were treated as ambiguous loci.17
HLA-mismatch in the graft-versus-host (GVH) vector was defined as when the recipient's antigens or alleles were not shared by the donor, whereas mismatch in the host-versus-graft (HVG) vector was defined as when the donor's antigens or alleles were not shared by the recipient.
Statistical considerations
The primary end point was survival after transplantation. Data for August 2001 were available in all 2947 patients. The incidence of grade III to IV acute GVHD, which was graded according to published criteria,18 was a secondary end point, and was analyzed in 2811 patients who achieved donor cell engraftment. The incidence of chronic GVHD was evaluated in 2150 patients who survived without relapse more than 100 days after HSCT. Engraftment failure was also analyzed with engraftment defined as a neutrophil count more than 500/mm3 for 3 consecutive days. Engraftment failure was diagnosed as when engraftment was not achieved at any time after transplantation.
The probability of survival and the cumulative incidence of acute GVHD were calculated using the Kaplan-Meier method. The cumulative incidence of relapse was calculated by the Gray method considering death without relapse as a competing risk.19 Univariate comparisons for dichotomous and time-to-event variables between groups were performed with the Fisher exact test and the log-rank test, respectively, and multivariate analyses were performed using logistic regression analysis and proportional hazards modeling, respectively. Potential confounding factors considered in the analysis were recipient age, sex, donor-recipient relationship (mother-child or not), disease status, stem cell source, and serologic/genotypic HLA mismatch. Acute leukemia in first or second remission, CML in first or second chronic phase, and MDS without leukemic transformation were considered standard-risk diseases, whereas others were considered high-risk diseases. Patients who received both bone marrow (BM) and peripheral blood stem cell (PBSC) grafts were included in the PBSC group. This study was approved by the Committee for Nationwide Survey Data Management of the Japan Society for Hematopoietic Cell Transplantation.
Results
Characteristics of the patients
The numbers of patients who received a graft from a serologically HLA-matched, one-locus–mismatched, and 2- or 3-loci–mismatched family donor were 2805, 112, and 30, respectively (Table 1). The HLA-mismatched group included significantly higher proportions of patients with high-risk disease and those who received PBSCs (P < .0001 for both comparisons). TBI-based conditioning regimens were preferentially used in HLA-mismatched group (P = .02) and high-risk group (P < .0001).
Patient characteristics
. | . | 1-locus mismatch . | . | . | |
|---|---|---|---|---|---|
. | Match . | Class I . | Class II . | 2-or 3-loci mismatch . | |
| n | 2805 | 70 | 42 | 30 | |
| Donor, n (%) | |||||
| Sibling | 2736 (98) | 39 (56) | 28 (67) | 9 (30) | |
| Others | 69 (2) | 31 (44) | 14 (33) | 21 (70) | |
| Sex, n (%) | |||||
| Male | 1711 (61) | 42 (60) | 21 (50) | 17 (57) | |
| Female | 1094 (39) | 28 (40) | 21 (50) | 13 (43) | |
| Age, n (%) | |||||
| Younger than 40 y | 1742 (62) | 45 (64) | 22 (52) | 14 (47) | |
| 40 y and older | 1063 (38) | 25 (36) | 20 (48) | 16 (53) | |
| Diagnosis, n (%) | |||||
| AML | 962 (34) | 21 (30) | 15 (36) | 10 (33) | |
| ALL | 672 (24) | 15 (21) | 13 (31) | 7 (23) | |
| CML | 804 (29) | 22 (31) | 11 (26) | 12 (40) | |
| MDS | 367 (13) | 12 (17) | 3 (7) | 1 (3) | |
| Disease risk, n (%) | |||||
| Standard | 2093 (75) | 41 (59) | 26 (62) | 7 (23) | |
| High | 712 (25) | 29 (41) | 16 (38) | 23 (77) | |
| Conditioning regimen, n (%) | |||||
| Non-TBI | 1126 (40) | 19 (27) | 15 (36) | 9 (30) | |
| TBI | 1679 (60) | 51 (73) | 27 (64) | 21 (70) | |
| Use of PBSCs, n (%) | |||||
| No | 2465 (88) | 54 (77) | 35 (83) | 14 (47) | |
| Yes | 340 (12) | 16 (23) | 7 (17) | 16 (53) | |
| Experienced engraftment failure, | |||||
| n (%) | 67 (2.4) | 6 (9) | 0 (0) | 3 (10) | |
| Number of genotype mismatches | |||||
| 0 | 2771 | 0 | 0 | 0 | |
| 1 | 3 | 22 | 20 | 0 | |
| 2 | 0 | 3 | 0 | 18 | |
| 3 | 0 | 0 | 0 | 8 | |
| ND | 31 | 45 | 22 | 4 | |
. | . | 1-locus mismatch . | . | . | |
|---|---|---|---|---|---|
. | Match . | Class I . | Class II . | 2-or 3-loci mismatch . | |
| n | 2805 | 70 | 42 | 30 | |
| Donor, n (%) | |||||
| Sibling | 2736 (98) | 39 (56) | 28 (67) | 9 (30) | |
| Others | 69 (2) | 31 (44) | 14 (33) | 21 (70) | |
| Sex, n (%) | |||||
| Male | 1711 (61) | 42 (60) | 21 (50) | 17 (57) | |
| Female | 1094 (39) | 28 (40) | 21 (50) | 13 (43) | |
| Age, n (%) | |||||
| Younger than 40 y | 1742 (62) | 45 (64) | 22 (52) | 14 (47) | |
| 40 y and older | 1063 (38) | 25 (36) | 20 (48) | 16 (53) | |
| Diagnosis, n (%) | |||||
| AML | 962 (34) | 21 (30) | 15 (36) | 10 (33) | |
| ALL | 672 (24) | 15 (21) | 13 (31) | 7 (23) | |
| CML | 804 (29) | 22 (31) | 11 (26) | 12 (40) | |
| MDS | 367 (13) | 12 (17) | 3 (7) | 1 (3) | |
| Disease risk, n (%) | |||||
| Standard | 2093 (75) | 41 (59) | 26 (62) | 7 (23) | |
| High | 712 (25) | 29 (41) | 16 (38) | 23 (77) | |
| Conditioning regimen, n (%) | |||||
| Non-TBI | 1126 (40) | 19 (27) | 15 (36) | 9 (30) | |
| TBI | 1679 (60) | 51 (73) | 27 (64) | 21 (70) | |
| Use of PBSCs, n (%) | |||||
| No | 2465 (88) | 54 (77) | 35 (83) | 14 (47) | |
| Yes | 340 (12) | 16 (23) | 7 (17) | 16 (53) | |
| Experienced engraftment failure, | |||||
| n (%) | 67 (2.4) | 6 (9) | 0 (0) | 3 (10) | |
| Number of genotype mismatches | |||||
| 0 | 2771 | 0 | 0 | 0 | |
| 1 | 3 | 22 | 20 | 0 | |
| 2 | 0 | 3 | 0 | 18 | |
| 3 | 0 | 0 | 0 | 8 | |
| ND | 31 | 45 | 22 | 4 | |
ND indicates not done (ambiguous loci).
We determined the number of genotypically mismatched loci in 2845 patients by the method described (see “Histocompatibility”) and the results are shown at the bottom of Table 1. An additional genotype mismatch was detected in 8 patients.
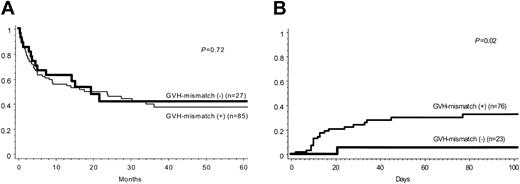
HLA-mismatch vector
Among the 112 patients who received a serologically one-locus–mismatched graft, 70 had a bidirectional mismatch, whereas 15 and 27 had a mismatch only in the GVH and HVG vectors, respectively. To evaluate the influence of mismatch in the GVH vector, we compared survival and the incidence of acute GVHD among patients who received serologically one-locus–mismatched grafts for those with and without mismatch in the GVH vector. Although the survival rate in the 2 groups was almost equivalent (P = .72), the incidence of grade III to IV acute GVHD was significantly higher in patients who underwent HSCT with a mismatch in the GVH vector (P = .02; Figure 1). Therefore, we used the overall number of mismatches in the survival analysis, whereas we used the number of mismatches in the GVH vector to compare the incidence of acute GVHD.
Impact of HLA mismatch in the GVH vector. Comparison of overall survival (A) and the incidence of grade III to IV acute GVHD (B) after serologically one-locus–mismatched HSCT between patient-donor pairs with or without an HLA mismatch in the GVH vector.
Impact of HLA mismatch in the GVH vector. Comparison of overall survival (A) and the incidence of grade III to IV acute GVHD (B) after serologically one-locus–mismatched HSCT between patient-donor pairs with or without an HLA mismatch in the GVH vector.
Engraftment failure
The incidence of engraftment failure was significantly higher in pairs with an HLA mismatch between the donor and recipient (2.4% in a serologically matched cohort versus 6.3% in a mismatched cohort; P = .01) and this difference was seen regardless of whether the HLA mismatch was analyzed at the serologic level or the DNA level and whether the mismatch was considered only in the HVG vector or in both vectors. Logistic regression analysis identified 2 independent risk factors for engraftment failure: HLA mismatch in the HVG vector (odds ratio, 2.28; 95% CI, 1.09-4.75; P = .028) and high-risk disease (odds ratio, 3.77; 95% CI, 2.36-6.02; P < .0001).
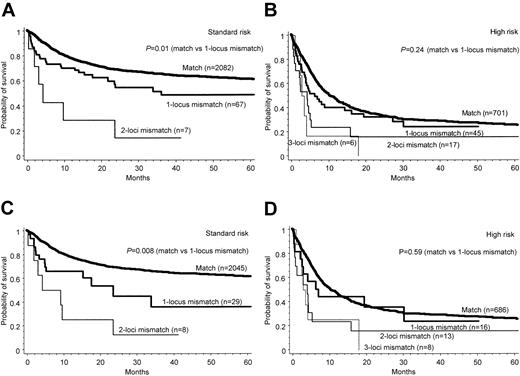
Survival
Overall survival in patients who underwent HSCT for standard-risk and high-risk diseases, grouped by the number of serologic HLA mismatches, is shown in Figure 2, panels A and B, respectively. A higher number of serologic HLA mismatches appeared to adversely affect survival. Among the potential confounding factors, higher age (≥ 40 years old), high-risk disease, and HLA mismatch were identified as independent predictive factors for shorter survival (Table 2). However, the impact of HLA mismatch on survival was smaller in high-risk patients and there was no statistically significant difference in survival between HLA-matched HSCT and one-locus–mismatched HSCT for high-risk disease (P = .24).
Overall survival based on mismatched loci. Overall survival after transplantation grouped according to the number of mismatched loci at the serologic level (A-B) and DNA level (C-D), and according to the disease status (A,C: standard-risk disease; B,D: high-risk disease). P values for the HLA-matched versus one-locus–mismatched group are shown.
Overall survival based on mismatched loci. Overall survival after transplantation grouped according to the number of mismatched loci at the serologic level (A-B) and DNA level (C-D), and according to the disease status (A,C: standard-risk disease; B,D: high-risk disease). P values for the HLA-matched versus one-locus–mismatched group are shown.
Results of proportional hazards modeling for overall survival
. | Relative risk (95% Cl) . | P . |
|---|---|---|
| Serologic matching | ||
| Age | ||
| Younger than 40 y | 1.00 | < .0001 |
| 40 y and older | 1.26 (1.13-1.41) | |
| HLA | ||
| Match | 1.00 | .014 |
| Mismatch | 1.38 (1.07-1.78) | |
| Disease | ||
| Standard risk | 1.00 | < .0001 |
| High risk | 2.82 (2.52-3.16) | |
| Genotypic matching | ||
| Age | ||
| Younger than 40 y | 1.00 | < .0001 |
| 40 y and older | 1.27 (1.14-1.43) | |
| HLA | ||
| Match | 1.00 | .036 |
| Mismatch | 1.53 (1.03-2.27) | |
| Disease | ||
| Standard risk | 1.00 | < .0001 |
| High risk | 2.83 (2.52-3.18) |
. | Relative risk (95% Cl) . | P . |
|---|---|---|
| Serologic matching | ||
| Age | ||
| Younger than 40 y | 1.00 | < .0001 |
| 40 y and older | 1.26 (1.13-1.41) | |
| HLA | ||
| Match | 1.00 | .014 |
| Mismatch | 1.38 (1.07-1.78) | |
| Disease | ||
| Standard risk | 1.00 | < .0001 |
| High risk | 2.82 (2.52-3.16) | |
| Genotypic matching | ||
| Age | ||
| Younger than 40 y | 1.00 | < .0001 |
| 40 y and older | 1.27 (1.14-1.43) | |
| HLA | ||
| Match | 1.00 | .036 |
| Mismatch | 1.53 (1.03-2.27) | |
| Disease | ||
| Standard risk | 1.00 | < .0001 |
| High risk | 2.83 (2.52-3.18) |
Two- or 3-loci—mismatched transplants were excluded.
We further analyzed the impact of genotypic HLA mismatch to exclude the influence of an unrecognized mismatch at the DNA level. As shown in Figure 2C-D, we observed a similar tendency toward a smaller impact of HLA mismatch on survival in patients with a high-risk disease, although the presence of genotypic HLA mismatch, along with an older age (≥ 40 years old), and high-risk disease, was identified as an independent risk factor for shorter survival (Table 2).
We compared the influence of class I versus class II mismatch on survival after serologically one-locus–mismatched HSCT, but the survival curves after HSCT with a class I mismatch and those after HSCT with a class II mismatch were superimposed (Figure 3A; P = .80). Furthermore, in an analysis at the DNA level, there was no statistically significant difference in survival after genotypically one-locus–mismatched HSCT between patients who received class I mismatched graft and those who received class II mismatched graft (Figure 3B; P = .98).
Overall survival based on mismatch locus. Overall survival after serologically (A) and genotypically (B) one-locus–mismatched HSCT in class I versus class II mismatch, stratified by the disease status. P values for class I versus class II mismatch are shown.
Overall survival based on mismatch locus. Overall survival after serologically (A) and genotypically (B) one-locus–mismatched HSCT in class I versus class II mismatch, stratified by the disease status. P values for class I versus class II mismatch are shown.
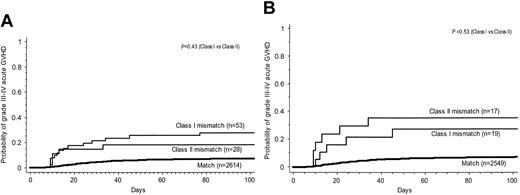
Acute and chronic GVHD
The incidence of grade III to IV acute GVHD after serologically one-locus–mismatched HSCT was 31%, which was significantly higher than that after serologically matched HSCT (9%; P < .0001). In addition, more than half the patients who developed grade III to IV acute GVHD did so between 10 and 20 days after HSCT (Figure 4A). Male sex, older age (≥40 years old), high-risk disease, the use of PBSCs, and the presence of HLA mismatch in the GVH vector were identified as independent risk factors for the development of grade III to IV acute GVHD (Table 3). The impact of one-locus mismatch on the incidence of grade III to IV acute GVHD was almost equivalent in BM transplantation (relative risk, 3.98; 95% CI, 2.25-7.04; P < .0001) and PBSC transplantation (relative risk, 2.29; 95% CI, 0.97-5.43; P = .059).
Incidence of grade III to IV acute GVHD. Cumulative incidence of grade III to IV acute GVHD after serologically (A) and genotypically (B) HLA-matched or one-locus–mismatched HSCT. P values for class I versus class II mismatch are shown.
Incidence of grade III to IV acute GVHD. Cumulative incidence of grade III to IV acute GVHD after serologically (A) and genotypically (B) HLA-matched or one-locus–mismatched HSCT. P values for class I versus class II mismatch are shown.
Results of proportional hazards modeling for the development of grade III to IV acute GVHD
. | Relative risk (95% CI) . | P . |
|---|---|---|
| Serologic matching | ||
| Age | ||
| Younger than 40 y | 1.00 | .027 |
| 40 y and older | 1.36 (1.04-1.79) | |
| Disease | ||
| Standard risk | 1.00 | .015 |
| High risk | 1.43 (1.07-1.92) | |
| Sex | ||
| Female | 1.00 | < .0001 |
| Male | 1.86 (1.37-2.53) | |
| Stem cell | ||
| BMT | 1.00 | < .0001 |
| PBSCT | 2.24 (1.63-3.08) | |
| HLA | ||
| GVH match | 1.00 | < .0001 |
| GVH mismatch | 2.67 (1.65-4.33) | |
| Genotypic matching | ||
| Age | ||
| Younger than 40 y | 1.00 | .041 |
| 40 y and older | 1.34 (1.01-1.78) | |
| Disease | ||
| Standard risk | 1.00 | .024 |
| High risk | 1.41 (1.01-1.90) | |
| Sex | ||
| Female | 1.00 | .0002 |
| Male | 1.81 (1.33-2.48) | |
| Stem cell | ||
| BMT | 1.00 | < .0001 |
| PBSCT | 2.47 (1.79-3.41) | |
| HLA | ||
| GVH match | 1.00 | < .0001 |
| GVH mismatch | 5.41 (2.93-10.0) |
. | Relative risk (95% CI) . | P . |
|---|---|---|
| Serologic matching | ||
| Age | ||
| Younger than 40 y | 1.00 | .027 |
| 40 y and older | 1.36 (1.04-1.79) | |
| Disease | ||
| Standard risk | 1.00 | .015 |
| High risk | 1.43 (1.07-1.92) | |
| Sex | ||
| Female | 1.00 | < .0001 |
| Male | 1.86 (1.37-2.53) | |
| Stem cell | ||
| BMT | 1.00 | < .0001 |
| PBSCT | 2.24 (1.63-3.08) | |
| HLA | ||
| GVH match | 1.00 | < .0001 |
| GVH mismatch | 2.67 (1.65-4.33) | |
| Genotypic matching | ||
| Age | ||
| Younger than 40 y | 1.00 | .041 |
| 40 y and older | 1.34 (1.01-1.78) | |
| Disease | ||
| Standard risk | 1.00 | .024 |
| High risk | 1.41 (1.01-1.90) | |
| Sex | ||
| Female | 1.00 | .0002 |
| Male | 1.81 (1.33-2.48) | |
| Stem cell | ||
| BMT | 1.00 | < .0001 |
| PBSCT | 2.47 (1.79-3.41) | |
| HLA | ||
| GVH match | 1.00 | < .0001 |
| GVH mismatch | 5.41 (2.93-10.0) |
Two- or 3-loci—mismatched transplants were excluded. BMT indicates bone marrow transplantation; PBSCT, peripheral blood stem cell transplantation.
We compared the influence of class I versus class II mismatch on the incidence of acute GVHD after serologically one-locus–mismatched HSCT and did not observe a significant difference between the groups (P = .23; Figure 4A). In an analysis of genotypic mismatch, the incidence of acute GVHD was almost the same between transplants with class I mismatch and those with class II mismatch (P = .70; Figure 4B).
The incidence of chronic GVHD in patients who received a serologically one-locus–mismatched graft was higher than that in patients who underwent HLA-matched HSCT, but this difference was not statistically significant (60% versus 47%; P = .11). Multivariate analysis revealed that male sex, higher age (≥ 40 years old), high-risk disease, and the use of PBSCs were independent risk factors for the development of chronic GVHD.
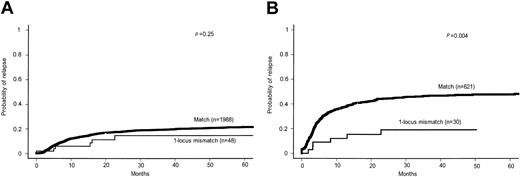
Relapse
Cumulative incidence of relapse was compared between HSCT with versus without a serologic mismatch in the GVH vector. It was 22% at 5 years after matched HSCT for standard-risk diseases, which was not significantly different from that after one-locus–mismatched HSCT (15%; P = .25; Figure 5A). In contrast, the incidence of relapse was dramatically decreased after one-locus–mismatched HSCT compared to matched HSCT for high-risk diseases (19% versus 47%; P = .004; Figure 5B).
Cumulative incidence of relapse after serologically HLA-matched or one-locus–mismatched HSCT. (A) Standard-risk disease. (B) High-risk disease.
Cumulative incidence of relapse after serologically HLA-matched or one-locus–mismatched HSCT. (A) Standard-risk disease. (B) High-risk disease.
Comparison between one-locus–mismatched related HSCT and matched unrelated HSCT
For patients with a high-risk disease, it appeared unnecessary to search a matched unrelated donor if the patient has a one-locus–mismatched family donor. However, for patients with a standard-risk disease, whether we should choose a one-locus–mismatched family donor or a matched unrelated donor is problematic. Therefore, we compared survival after matched related HSCT, one-locus–mismatched related HSCT, and HLA-matched unrelated HSCT. We excluded HSCT that was performed within 180 days after the diagnosis of underlying disease because the interval from diagnosis to HSCT was more than 180 days in 987 of 1002 unrelated HSCTs. Another difference in the characteristics of the patients between one-locus–mismatched group and matched unrelated group was the proportion of patients of older age (40% versus 25%; P = .0007). As shown in Figure 6, survival curves of one-locus–mismatched related HSCT and unrelated HSCT were superimposed both among standard-risk and high-risk patients, although the incidence of grade III to IV acute GVHD was significantly higher after one-locus–mismatched related HSCT (30% versus 16%; P = .0013). These findings did not change when we compared these curves without excluding patients who underwent HSCT that was performed within 180 days after the diagnosis of underlying disease (data not shown). In an analysis of genotypic mismatch, the 2 curves were also superimposed (data not shown).
Overall survival after transplantation grouped according to the type of donor and according to the disease status. (A) Standard-risk disease. (B) High-risk disease.
Overall survival after transplantation grouped according to the type of donor and according to the disease status. (A) Standard-risk disease. (B) High-risk disease.
We performed a multivariate analysis using proportional hazard modeling to adjust the difference between one-locus–mismatched HSCT and matched unrelated HSCT. Higher age (relative risk, 1.61; 95% CI, 1.34-1.94; P < .0001) and high-risk disease (relative risk, 2.48; 95% CI, 2.08-2.96; P < .0001) were identified as independent risk factors for shorter survival. Whether the use of a one-locus–mismatched related donor or a matched unrelated donor did not affect survival even adjusted for these factors (relative risk, 0.97; 95% CI, 0.71-1.20; P = .84).
Discussion
This study analyzed the outcome of HSCT from family donors over the last decade. Recent advances in genomic typing enabled us to evaluate the true influence of a single HLA mismatch. Previous studies did not use genotypic matching and therefore may have overlooked mismatches at the DNA level. Other advantages of this study are the exclusion of ex vivo manipulation of graft and the use of registry data from a homogenous population. These features allowed us to clearly evaluate the influence of HLA-mismatch on the incidence of GVHD and the probability of survival.
Higher age, high-risk disease, and the presence of HLA mismatch were identified as independent risk factors for both shorter survival and the development of grade III to IV acute GVHD. The adverse influence of HLA mismatch on survival was pronounced in patients with standard-risk disease. It is possible that the increased risk of acute GVHD was counterbalanced by a decrease in relapse in patients with high-risk disease, whereas the increased risk of transplant-related mortality did not balance the change in the relapse rate in standard-risk patients, because the risk of relapse is low in such patients.
Whereas the report from IBMTR showed a trend similar to ours, the Seattle group reported equivalent survival in HLA-matched and one-locus–mismatched HSCT, even in standard-risk patients.4,6,10 This discrepancy may have been due to the difference in the method used for HLA matching.1 The one-locus–mismatched group in the IBMTR study may have included a greater number of patients with another genotypic mismatch that could not be detected by serologic typing, compared to the Seattle study. However, in this study, we used genotypic matching, and thus it is very unlikely that patients in our one-locus–mismatched group in Figure 2C-D had another genotypic mismatch. Even this “true one-locus mismatch” was shown to adversely affect survival in standard-risk patients. The difference in the impact of HLA-mismatch among studies may be due to recent improvements in the outcome of standard-risk HSCT. The probability of survival at 5 years after HLA-matched standard-risk transplantation was approximately 40%, 60%, and 60% in the Seattle study, the IBMTR study, and this study, respectively, with a similar definition of standard-risk disease.4,10 The major difference was that the Seattle study included transplantations that were performed between 1975 and 1986, whereas the IBMTR study and this study included those performed between 1985 and 1991, and between 1991 and 2000, respectively. The outcome of HLA-matched transplantation in standard-risk patients might have been improved by advances in supportive treatments and possibly by more ready application of HSCT in standard-risk patients. On the other hand, the outcome of HLA-matched transplantation in high-risk patients has remained fairly constant at approximately 20% survival at 5 years in all 3 studies.
Our comparison of the impact of class I versus class II mismatch on the incidence of acute GVHD and survival is interesting because genotypic class I mismatch was a stronger risk factor than genotypic class II mismatch for the development of grade III to IV acute GVHD in serologically matched unrelated BM transplantation in Japan.15 However, there was no difference in the outcome of serologically class I mismatched HSCT versus serologically class II mismatched HSCT in this population. Although there were only a small number of patients with complete genotypic matching, whether the mismatch is in class I or class II appeared to be unimportant in one-locus–mismatched HSCT from family members.
The use of PBSCs as a graft was identified as an independent risk factor for the development of grade III to IV acute GVHD. However, in several randomized controlled trials that compared PBSC transplantation and BM transplantation from HLA-identical siblings, the incidence of acute GVHD did not significantly differ, except in a study by the European Group for Blood and Marrow Transplantation.20-25 In Japan, PBSCs tended to be used in patients with infection or low performance status until allogeneic PBSC transplantation became covered by health insurance in April 2000. Therefore, there might be biases that could not be detected in this dataset. We need a randomized controlled trial to address this issue in our own country.
After we found that the TBI-based regimens were preferentially used in HLA-mismatched group and high-risk patients, we evaluated the impact of the type of a conditioning regimen. However, the difference in the conditioning regimen did not affect any outcome measures. Conditioning regimens including antithymocyte globulin were used in 6 and 3 patients who underwent HLA-matched and one-locus–mismatched HSCT, respectively. However, exclusion of these 9 patients did not influence the outcome of this study (data not shown).
In conclusion, in high-risk patients, there appears to be no need to search for a matched unrelated donor when a one-locus–mismatched family donor is available, regardless of whether the mismatch is class I or class II, because we can expect an outcome similar to that after HSCT from an HLA-identical sibling. However, in standard-risk patients, the indications for allogeneic HSCT based on randomized controlled trials using HLA-identical sibling donors should not be extended to one-locus–mismatched HSCT, because there was a statistically significant difference in survival between HLA-matched and one-locus–mismatched HSCT. Therefore, we should reconsider the indication of HSCT, although there is no need to search for an unrelated donor when a one-locus–mismatched family donor is available. The outcome of 2- or 3-loci–mismatched HSCT without T-cell depletion was extremely poor.
Prepublished online as Blood First Edition Paper, April 24, 2003; DOI 10.1182/blood-2003-02-0430.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
This is a study from Working Group 3 of the Japanese Society for Hematopoietic Cell Transplantation.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal