During the past decade it became evident that shear stress in the vasculature modulates gene expression of endothelial cells and thus the endothelial phenotype. The observed changes included adhesion molecules and chemokines involved in the recruitment of leukocytes.1 The differential gene expression under various shear rate conditions offered an explanation for why some sites in the vasculature may be more suited for leukocyte extravasations and why atherosclerotic lesions develop mainly in the regions of disturbed flow.2 The as-yetunidentified mechanotransducing receptors were proposed to be either integrins3 or stretch-activated calcium channels.4 FIG1
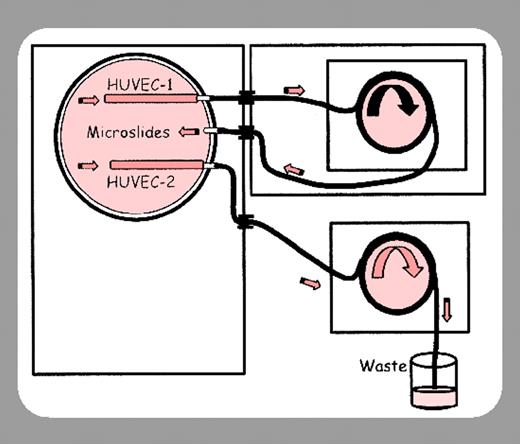
Sheikh and colleagues (page 2828) provide yet another twist to the shearmediated modulation of endothelium. They demonstrate that the extent of endothelial response to the proinflammatory cytokine tumor necrosis factor α (TNF-α) also depends on shear stress. This indicates that the reaction to the same inflammatory stimulus can be locally regulated not only by the effects of surrounding tissues and basement membrane components but also by mechanical forces tugging at the endothelial cells. The authors plated first-passage human umbilical vein endothelial cells in identical tubes and exposed these to shear stress conditions that would be encountered in postcapillary venules, where leukocytes tend to extravasate, or in arteries, where leukocyte adhesion is rare. The endothelial response to TNF-α was incrementally reduced with both increased duration and strength of shear exposure. The high shear rates lowered the production of mRNAs for E-selectin and the CXC-chemokines interleukin 8 (IL-8) and growth-related oncogene α (GRO-α), whereas the expression of TNF receptors apparently was not affected. The adhesion receptor E-selectin is important for both leukocyte and platelet rolling5 on inflamed endothelium. The biologic potency of the TNF-α–treated endothelium in neutrophil adhesion and transmigration was also determined and both parameters were reduced in TNF-α–treated endothelium grown under high–shear rate conditions. Thus, the study by Sheikh and colleagues explains why leukocyte and platelet rolling are up-regulated in venules but remain infrequent in arterioles when TNF-α is produced in inflammation.
How could shear modulate TNF-α signaling? There are many possibilities. The distribution/availability of the TNF receptors in the endothelial cell could be modified; conformational change in the receptors could be induced by the high shear rate, rendering them less active. Alternatively, the expression of a signaling component downstream of the TNF receptors may be affected, or, finally, cosignaling of TNF receptors with a mechanotransducing receptor could have produced the observed dampening effect. These possibilities need to be addressed in future studies. It will also be important to establish whether the effect of shear on the TNF-α signaling is specific to this pathway or whether signaling by other endothelial receptors is modulated by shear stress.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal