Abstract
A survey of directors of adult and pediatric hematology/oncology subspecialty training programs in the United States and Canada was conducted to assess the environment in which recruitment and training is conducted in these medical disciplines. A total of 107 program directors responded to the survey, representing 66% of internal medicine and 47% of pediatric subspecialty programs in hematology or hematology/oncology. Specific areas covered in the web-based questionnaire included the type and demographics of the training program, profile of the training program director, characteristics of the applicant pool and existing trainee recruits, characteristics of the training program environment and curricula, research productivity of trainees, and the career pathways taken by recent training program graduates (including dominant areas of clinical interest). The results of this survey show considerable heterogeneity in the recruiting practices and the environment in which subspecialty training occurs, leading the authors to recommend improvements in or a heightened attention to issues, including recruitment of minority trainees, flexibility to recruit international medical school graduates, timing of trainee acceptance, maintaining the financial support of Medicare graduation medical education (GME), training of physician scientists, organization of the continuity clinic experience, visibility of nonmalignant hematology as a career path, and level of training program director support. (Blood. 2004;103:4383-4388)
Introduction
Training in the fields of hematology and medical oncology is generally conducted in subspecialty units of departments of internal medicine or pediatrics. Whereas the disciplines of hematology and oncology are considered to be distinct within the context of internal medicine, with separate Accreditation Council for Graduate Medical Education (ACGME)1 Residency Review Committee (RRC)-sanctioned subspecialty curricula (2 years for each discipline) and American Board of Internal Medicine certifying examinations, the fields are often taught in combined 3-year hematology/oncology training programs, which is also the norm in pediatrics (which has a single curriculum and certifying examination). The major mission of subspecialty training in hematology and medical oncology is to prepare trainees to achieve clinical competency in these disciplines through curricula that include didactic teaching and practical “hands-on” experience as taught by subspecialists who have already achieved these competencies.
In addition to teaching clinical competency, the RRC requirements that govern both internal medicine and pediatric disciplines mandate training in research, but they do not quantify the extent of such training.1 Certain training programs that are based primarily at academic centers may place a higher priority on the quantity or quality of the research experience that occurs during the training curriculum. These programs may seek National Institutes of Health (NIH) support to help fund the research experience of their fellowship trainees, and the ability of these training programs to compete for federal funding depends on their success in training graduates who accept positions in academic medicine and achieve financial independence as investigators.
How units of hematology and/or medical oncology in departments of internal medicine and pediatrics achieve the goal of promoting the clinical and research competencies of their trainees is a “black box.” Except for a few reports that have focused on specific aspects of the training curriculum,2,3 there has been no systematic analysis of the environment in which the disciplines of hematology and oncology are taught by training programs in North America in the past 25 years. To gain insight into this process, the Committee on Training Programs of the American Society of Hematology (ASH) conducted a web-based survey of directors of both internal medicine and pediatric hematology or hematology/oncology training programs. Whereas the proportion of training program directors responding to this survey was 54% (107 programs), these respondents reflect a fairly representative sampling of the entire group (196 programs). Included in this survey were questions pertaining to (1) the characteristics of the training program and the profile of the director, (2) the profile of the applicant pool, (3) the profile of the existing trainee group, (4) sources of funding for training, (5) features of the clinical and research curricula, (6) research productivity of trainees, and (7) professional fate of trainee graduates. The results of this survey disclosed considerable heterogeneity in recruiting practices and the environment in which hematology and oncology subspecialty training occurs, and they provided important insights about the factors that influence the career decisions of subspecialty trainees.
Methods
With the assistance of Alan Newman Research (Richmond, VA), the authors developed a 51-question questionnaire to determine the environment in which hematology or hematology/oncology fellowship training is conducted among U.S. and Canadian internal medicine and pediatric training programs. The questionnaire consisted of a web-based survey that was conducted from July through September 2003. One hundred ninety-six training program directors (122 directors of adult programs, 57 directors of pediatric programs, 17 directors of training programs of undetermined focus) were invited to participate, based on the listing of these programs in the ACGME Training Program Database. An initial invitation by e-mail was sent on July 15, 2003, with follow-up reminder e-mails sent on July 24 and September 3. By October 1, 2003, 107 training program directors (99 in the United States and 8 in Canada) responded to the survey, including 80 directors of adult programs and 27 directors of pediatric programs. The overall response rate was 54%. Among the 179 programs with a clear training focus, 80 of 122 adult program directors responded (66% response rate) and 27 of 57 pediatric program directors responded (47% response rate). The survey was designed as a descriptive study and, consequently, is not suitable for statistical analysis.
Results
Director and program profiles
Among the 107 respondents to this survey, 75% direct programs in adult hematology (14%) or adult combined hematology/oncology (61%) programs; 25% direct pediatric hematology/oncology programs. Forty-two percent of training program directors have held this responsibility for more than 6 years with 37% serving in this capacity for less than or equal to 3 years. The majority (72%) of training program directors devote 20% to 40% of their professional effort to supervising their programs, with directors of pediatric programs on average spending somewhat less effort in program direction than their adult program counterparts: 50% of directors of adult programs spend more than 30% effort, whereas only 25% of pediatric program directors describe a commitment of this magnitude. Directors of adult training programs are more likely to receive either full (16%) or partial (38%) funding for their effort as training program directors, whereas the majority (74%) of pediatric training program directors receives no institutional salary support.
Sixty-two percent of these programs are based at academic medical centers, described as being based at a medical school (38%), at a university National Cancer Institute (NCI)-designated cancer center (21%), or at a free-standing NCI-designated cancer center (3%). Thirty-four percent of the training programs are affiliated either with a medical school or with an NCI-designated cancer center; 6% of the responding programs are based at community or regional medical centers.
Recruitment of trainees
Two thirds of training programs admit 3 or fewer trainees each year (64% of adult training programs and 74% of pediatric programs). Thirty-seven percent of adult training programs are larger (> 4 trainees admitted each year) as compared with 26% of pediatric programs, with most of these programs admitting 4 to 6 trainees per year. Not surprisingly, adult training programs receive significantly more applications than pediatric training programs (the majority of the latter receiving < 75 applications per year). Eighty-four percent of adult programs receive more than 75 applications per year. Approximately three fourths (76%) of adult training programs report an increase in the number of applicants over the preceding 5 years, with less than half (45%) of pediatric programs observing such increases. Among the applications received, the majority of training programs (89%) select their trainees from a pool of less than 24 applicants who are interviewed, with adult programs interviewing more candidates than pediatric programs. More than half of the programs (56%) recruit their trainees from a national pool of applicants, whereas 30% recruit most of their trainees either regionally (22%) or from the home institution (8%). Fourteen percent of programs recruit most of their trainees from applications originating from outside North America. With respect to gender and ethnic origin, women constitute approximately 43% of the total applicants (51% for pediatric programs and 41% for adult programs). Slightly more than 13.1% are from underrepresented minorities (URMs), including African Americans (6.5%), Hispanics (5.3%), American Indians (0.3%), and Pacific Islanders (1.0%). A somewhat greater proportion of applicants to adult training programs are African Americans (7.2%) as compared with pediatric programs (4.8%). Forty-three percent of the total applicant pool received undergraduate medical training at either U.S. or Canadian allopathic or osteopathic schools (35% of applicants to adult training programs; 65% of applicants to pediatric programs). Ninety percent of applicants to adult training programs received residency training at U.S. or Canadian programs.
Among existing trainees (over the past 3 years), training program directors report that 43% of their trainees are recruited from a national pool of applicants, whereas 26% come from the region in which the program resides. Twenty-two percent of trainees are from the home institution, whereas 9% are from countries outside North America. Two thirds of directors report that at least 75% of their existing trainees are either U.S. citizens or resident aliens (with 26% of programs claiming that 100% of their trainees fall into this category). Conversely, 10% of training program directors report fewer than 25% of their existing trainees are either U.S. citizens or resident aliens. Fifty-five percent of existing trainees in adult programs received their undergraduate medical education at U.S. or Canadian allopathic or osteopathic schools (as compared with 71% of existing trainees in pediatric programs); 95% of existing trainees in adult programs were recruited from U.S. or Canadian internal medicine residency programs.
More than 46% of existing trainees of adult and pediatric programs are women, and 8% overall are members of underrepresented minorities with a higher proportion of URM trainees in adult programs as compared with pediatric programs (Table 1). Among these URMs, more African-Americans and Hispanics are recruited to adult programs as compared with pediatric programs. Nine of 10 training programs do not apply specific strategies to recruit URM applicants, but most programs that do use these recruiting strategies are adult training programs (10% of adult programs versus 4% of pediatric programs). Both adult and pediatric programs report an increase in the number of women trainees over the past 5 years (51% for adult programs and 33% for pediatric programs). Fewer programs report increases in URM applicants (17% for adult programs and 11% for pediatric programs). In fact, 11% of pediatric programs report a decline in URM trainees (as compared with 4% of adult programs).
Gender and ethnic origin of trainees over the past 3 years
. | Total, % (n = 103) . | Adult, % (n = 78) . | Pediatric, % (n = 25) . |
|---|---|---|---|
| Women | 46.2 | 41.8 | 60.0 |
| African American | 4.0 | 4.7 | 1.8 |
| Hispanic | 2.9 | 3.5 | 1.2 |
| American Indian | 0.1 | 0.1 | 0.1 |
| Pacific Islander | 1.0 | 0.9 | 1.1 |
. | Total, % (n = 103) . | Adult, % (n = 78) . | Pediatric, % (n = 25) . |
|---|---|---|---|
| Women | 46.2 | 41.8 | 60.0 |
| African American | 4.0 | 4.7 | 1.8 |
| Hispanic | 2.9 | 3.5 | 1.2 |
| American Indian | 0.1 | 0.1 | 0.1 |
| Pacific Islander | 1.0 | 0.9 | 1.1 |
Percentages indicate the mean percentage of trainees (as reported by training program directors) in each of the indicated categories.
Somewhat more than one third of programs (37%) have recruited trainees of whom 50% or more had prior research experience (as defined by authorship of one or more published abstracts, peer-reviewed or non-peer-reviewed publications). Another one third of programs recruited trainees of whom 25% to 49% had prior research experience.
Although pediatric hematology/oncology has a match for trainee recruitment, one does not exist for adult programs. When queried, slightly less than 50% of adult program directors support the reinstitution of a match for fellowship. In contrast, almost three fourths (73%) of adult training program directors support a uniform acceptance date of trainee applicants. In addition, a significant majority of both adult training program directors (83%) and pediatric program directors (78%) support a proposal to move the recruiting calendar to later in the second house officer year or early in the third year to allow applicants more time to make career decisions. Among the greatest challenges reported by training program directors is recruiting trainees to their programs: 1 of 5 directors is challenged by attracting a competitive applicant pool (21%), whereas 19% are challenged by recruiting from a competitive pool; 27% report challenges with both aspects of the recruiting process.
Training program support
Training program directors report 2 primary sources of funding for the clinical component of their training programs: for 72% of training programs, the clinical component receives support from hospital or Medicare funds; for 59%, funding is provided by a division or departmental source. Other significant sources include Veterans Administration (VA) funding (33%), industry-based funding (25%), other federal funding (20%), and funding from private foundations (18%). The research component of training programs, however, has more diverse sources of support. Nearly 3 of 5 training programs receive funding for the research component of their program through a division or department source. Two of 5 depend on either industry funding or mentors' grant funding. More than one third (36%) receive funding through an NIH training grant (29% of adult programs, 56% of pediatric programs, and 44% of programs of either type based at academic centers). Other sources of support include nondepartment or nondivisional institutional funding (27%), private funding (19%), other federal funding (18%), and VA funding (14% of adult programs).
Research training
With respect to a training curriculum that is supportive of research, 35% of training programs report an environment in which at least 50% of the total training experience is devoted to trainee research efforts. Thirty-seven percent of programs set aside 25% to 49% of the training experience for research, and 28% of programs set aside less than 25% for research. Pediatric programs in general provide a greater opportunity for research with 85% allocating more than 50% of the training program experience to trainee research efforts (as compared with a corresponding 18% of adult programs). Programs based in academic centers allocate somewhat more training time to research than do programs with academic affiliations or programs based at regional centers. With respect to the type of research that trainees pursue (Table 2), less than one fourth of trainees in adult programs pursue bench laboratory research as compared with two thirds of pediatric trainees. Conversely, a greater proportion of adult trainees pursue clinical trials research as compared with pediatric trainees. Smaller subsets of trainees pursue health services outcomes research and other forms of clinical research such as epidemiology. In support of clinical research training, 56% of programs use a formal didactic curriculum with specific training in clinical protocol design, biostatistical methods, regulatory policies, research ethics, etc. Among the programs with a formal clinical track or clinical research curriculum (n = 60), 95% require a mentor-supervised research project with a minority of programs (28%) requiring a laboratory experience. One half of training program directors who subscribe to a clinical track or clinical research curriculum (n = 60) describe this curriculum as a course for trainees from multiple disciplines. One of 4 indicates that their curriculum is a tailored course for their trainees alone. The remaining one fourth use a curriculum based on a series of courses given elsewhere in the university or center. Only 1 of 6 directors indicates that the trainees can receive academic credit toward a graduate degree when they complete the formal research curriculum. When academic credit is offered, in about half of the programs (47%) the trainees are expected to complete the academic requirement for a master's or doctoral degree.
Research focus of trainees over the past 3 years
. | Total, % (n = 102) . | Adult, % (n = 77) . | Pediatric, % (n = 25) . |
|---|---|---|---|
| Bench laboratory research | 35.3 | 24.9 | 67.1 |
| Clinical trials research | 46.0 | 53.0 | 23.5 |
| Health services/outcomes research | 6.1 | 6.3 | 5.5 |
| Other clinical research (eg, epidemiology) | 9.0 | 10.1 | 5.4 |
. | Total, % (n = 102) . | Adult, % (n = 77) . | Pediatric, % (n = 25) . |
|---|---|---|---|
| Bench laboratory research | 35.3 | 24.9 | 67.1 |
| Clinical trials research | 46.0 | 53.0 | 23.5 |
| Health services/outcomes research | 6.1 | 6.3 | 5.5 |
| Other clinical research (eg, epidemiology) | 9.0 | 10.1 | 5.4 |
Percentages indicate the mean percentage of trainees (as reported by training program directors) who pursued the indicated categories of research.
With respect to the academic productivity of fellowship trainees, an average of 62% author a published abstract at a national meeting, 49.5% author a peer-reviewed publication, 35.8% author a non-peer-reviewed publication, 48.3% give a poster or oral presentation at a national meeting, and 34.2% design a clinical trial. Authorship of an abstract or peer-reviewed publication and presentation at a national meeting are somewhat higher for pediatric trainees than their adult counterparts (with no major difference in these major indexes of scientific productivity between programs that are based at academic centers versus those that are not). Clinical trial design is more prevalent in the adult trainee group.
Among faculty who mentor fellowship trainees, two thirds of an average faculty pool of 19 are described as active research investigators (including 23.1% focused in laboratory research and 38.7% focused on clinical research). The other one third of training faculty have a dominant focus on clinical care and education. Among the mentor pool in adult programs (an average number of 21 faculty), a greater proportion have a dominant focus on clinical trials research as compared with their pediatric counterparts (with an average faculty pool of 15).
Whereas most training programs encourage their trainees to apply for independent fellowship or career development funding, this is required in only 6% of programs. Despite the encouragement to apply for independent fellowship or career development funding, nearly one half (46%) of adult training program directors report that none of their trainees have successfully competed for this support over the preceding 3 years; an additional 30% report that the percentage of trainees who successfully competed for this kind of funding was no more than 25%. Success in competing for extramural funding was higher for pediatric trainees with 35% of pediatric training program directors reporting a funding rate of between 25% and 50%, and another 27% reporting a funding rate exceeding 50%. Trainees of academically based programs are no more successful in competing for career development funding than trainees of academically affiliated or nonacademic programs.
Clinical training
With respect to clinical training, adult training program directors report that a majority (74%) of their trainees seek double-board eligibility in both hematology and oncology with only 10% and 13% seeking single-board eligibility in hematology alone or medical oncology alone, respectively. Only 1% of trainees seek specialized training in medical oncology and geriatrics. The majority of training programs report on-site training experience in hematopoietic stem cell transplantation (91% of adult programs and 78% of pediatric programs). For 3-year training programs, trainees are required to spend the equivalent of 3 months each in an inpatient and outpatient transplantation training experience (with the outpatient experience being somewhat higher in pediatric programs [4.6 months]); for 2-year programs the transplantation requirement is approximately half. Seventy-six percent of the responding training programs (67% of adult programs and 94% of pediatric programs) provide their fellowship trainees with an option to supplement their experience in hematopoietic stem cell transplantation beyond the requirements for board eligibility (currently 1 month). Among the 81 programs offering this supplemental experience, 49% of programs offer a program that exceeds 6 months with another 28% offering programs of 3 to 6 months in duration.
In addition to an experience in hematopoietic stem cell transplantation, the vast majority of training programs (95%-97%) offer elective or required rotations in other clinical experiences, including transfusion medicine/blood banking, hematopathology, and thrombosis/hemostasis, with no significant difference in these requirements/electives between adult and pediatric programs. Eighty-nine percent of programs offer a rotation in radiation oncology. Other foci of clinical training offered by both adult and pediatric programs include neuro-oncology (67% of programs overall), hospice/palliative care (78%), and disease-specific multi-disciplinary clinics (74%). Among adult training programs, 70% offer rotations in pediatric hematology/oncology, 87% offer rotations in gynecologic oncology, 48% offer rotations in geriatric oncology, and 53% require ambulatory clinic or inpatient experiences at a VA hospital.
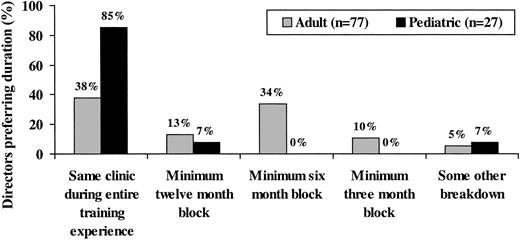
In nearly half (45%) of adult programs, at least 41% of the clinical training experience takes place in the ambulatory clinic (more than 50% of experience in 19% of the adult programs). Pediatric trainees spend less time in the ambulatory clinic with 60% of the programs requiring an ambulatory experience of between 21% and 40%. It is an RRC requirement that the ambulatory clinic experience include a continuity clinic throughout the training experience.1 Among directors of adult training programs, roughly one third favor continuity clinics consisting of 6-month blocks with another one third favoring the same clinic during the entire training experience. Most pediatric directors favor one continuity clinic throughout training (Figure 1).
Training program director preferences about the optimal duration of the required continuity clinic experiences. The vertical bars indicate the percentage of training program directors with the indicated preferences regarding the duration of the continuity clinic.
Training program director preferences about the optimal duration of the required continuity clinic experiences. The vertical bars indicate the percentage of training program directors with the indicated preferences regarding the duration of the continuity clinic.
Meeting attendance
All fellowship trainees in both adult and pediatric training programs are encouraged to attend the ASH annual meeting, and 90% of trainees within adult training programs are encouraged to attend the annual meeting of the American Society for Clinical Oncology (ASCO); approximately 30% of training program directors encourage attendance at the annual meeting of the American Association for Cancer Research (AACR). Roughly half of the trainees in adult hematology/oncology training programs are encouraged to attend clinical research workshops sponsored by either ASH or ASCO/AACR (less than 1 of 4 pediatric program training program directors encourage participation in either of these clinical research experiences).
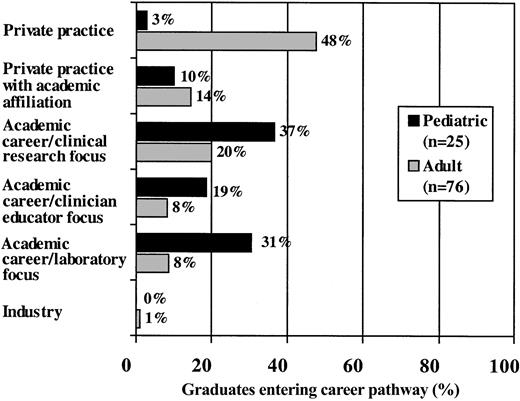
Career pathways after fellowship
With respect to the career pathways of recent fellowship trainee graduates (Figure 2), 62% of graduates of adult hematology/oncology training programs enter private practice, of whom 14% have an academic affiliation. Conversely, only 36% of graduates of adult hematology/oncology training programs pursue academic careers (20% with a clinical research focus, 8% with a laboratory focus, and 8% fulfilling a role as clinician educator). However, the majority of graduates of pediatric hematology/oncology training programs enter careers in academic medicine (37% with a clinical focus, 31% with a laboratory focus, and 19% with a clinician-educator focus). Overall, no major differences in career pathway were observed comparing academically based programs with programs operating outside academic centers. Among those individuals pursuing academic careers, 28% overall accepted positions at the home institution (26% for graduates of adult programs and 35% of graduates of pediatric programs).
Career pathways selected by graduates of adult and pediatric training programs over the past 3 years. The horizontal bars indicate the mean percentage of training graduates (as reported by training program directors) who have left the program to start careers in the indicated pathways.
Career pathways selected by graduates of adult and pediatric training programs over the past 3 years. The horizontal bars indicate the mean percentage of training graduates (as reported by training program directors) who have left the program to start careers in the indicated pathways.
With respect to dominant areas of clinical focus (Table 3), most graduates of adult training programs who enter private practice target malignant hematology and solid-tumor oncology as clinical foci. Only one fifth of these private practitioners restricted their practices to solid-tumor oncology, and only a small minority of these individuals focused primarily on malignant hematology alone or nonmalignant hematology. Graduates of adult programs who pursued academic careers tended to be more specialized, including 30% who focus on solid-tumor oncology, 18.5% who focus on malignant hematology, and 7.7% who focus on hematopoietic stem cell transplantation. Thirty-four percent of these academic practitioners treat patients with malignant hematologic diseases and with solid tumors, whereas less than 5% focus on nonmalignant hematology disorders. Among graduates of pediatric training programs, most practitioners in both the private and academic groups treat patients with both malignant hematology and solid-tumor oncology conditions. Academic pediatric hematology/oncology graduates may specialize in nonmalignant hematology and hematopoietic stem cell transplantation.
Clinical focus of trainee graduates who pursue private practice or academic careers
. | Adult training program, % . | . | Pediatric training program, % . | . | ||
|---|---|---|---|---|---|---|
. | Private . | Academic . | Private . | Academic . | ||
| Nonmalignant hematology | 5.8 | 4.6 | 0.9 | 13.1 | ||
| Malignant hematology | 5.1 | 18.5 | 0.0 | 11.7 | ||
| Solid-tumor oncology | 20.5 | 30.0 | 0.0 | 5.4 | ||
| Malignant hematology and solid-tumor oncology | 73.4 | 34.0 | 41.4 | 54.3 | ||
| Hematopoietic stem cell transplantation | 1.6 | 7.7 | 0.9 | 22.2 | ||
. | Adult training program, % . | . | Pediatric training program, % . | . | ||
|---|---|---|---|---|---|---|
. | Private . | Academic . | Private . | Academic . | ||
| Nonmalignant hematology | 5.8 | 4.6 | 0.9 | 13.1 | ||
| Malignant hematology | 5.1 | 18.5 | 0.0 | 11.7 | ||
| Solid-tumor oncology | 20.5 | 30.0 | 0.0 | 5.4 | ||
| Malignant hematology and solid-tumor oncology | 73.4 | 34.0 | 41.4 | 54.3 | ||
| Hematopoietic stem cell transplantation | 1.6 | 7.7 | 0.9 | 22.2 | ||
Percentages indicate the mean percentage of trainees (as reported by training program directors) who pursued the indicated categories of clinical focus.
Conclusions and recommendations
The results of this survey provide unique insights into the current recruitment and training environment for adult and pediatric hematology and hematology/oncology fellowship programs in the U.S. and Canada. This information should prove useful to training program directors by providing alternative options for programatic redesign, and as a means of assessing training program policy changes initiated by the ACGME. Based on these results, we make the following conclusions and recommendations:
Interest in the subspecialties of hematology/oncology is growing, particularly among adult programs. Whereas gender diversity has improved, the proportion of URM physicians entering subspecialty training lags behind the proportion of URM matriculants to U.S. medical schools.4 The 90% of training programs that make no special effort to recruit URM trainees should consider the benefits of enhanced ethnic diversity for the profession and for society as a whole.5
Whereas 95% of existing adult trainees were recruited from U.S. or Canadian internal medicine training programs, the RRC proposes that all subspecialty trainees at U.S. training programs be graduates of ACGME institutions (disallowing candidates from residency training programs in Canada and elsewhere). We strongly urge the RRC to maintain the current level of flexibility in allowing U.S. subspecialty training programs to recruit outstanding graduates of non-U.S. residency programs (up to the current allowable proportion of 25%).
Support for a uniform acceptance date is high among adult training program directors. We encourage the general acceptance of a uniform acceptance date as well as the proposal by the Association of Subspecialty Professors (ASP) to move the “recruiting calendar” to later in the internal medicine residency training schedule. Both of these initiatives are “resident friendly” and will allow prospective trainees to make critical career decisions in a less high-pressure environment.
Hospital funds (largely attributable to Medicare payments for graduate medical education [GME]) are a major source of support for the clinical training component of 72% of the programs responding to this survey. This observation underscores the critical importance of Medicare funding and the need to preserve this source of support for subspecialty training. As the interest and options for careers in these subspecialties increase, and as educational and clinical service opportunities expand (due to increasing numbers of patients and the effect of duty hour regulations), current Medicare GME caps should be reevaluated and increased as appropriate.
Research training accounts for less than 50% of the total training experience in the majority (65%) of the training programs responding to this survey. Despite tremendous recent advances in the fields of genomics and proteomics, few graduates of adult training programs are pursuing careers in laboratory medicine. Newly proposed internal medicine RRC recommendations that seek to increase the magnitude of ambulatory training threaten to constrain research training further.1 For some time it has been recognized that the physician scientist is “an endangered species,”6 and, accordingly, we strongly encourage training programs in our discipline to preserve and, where possible, expand their programmatic research initiatives.
Whereas most pediatric training program directors favor a uniform (same clinic throughout the training experience) continuity clinic experience, roughly two thirds of adult training program directors favor continuity clinic experiences of shorter durations, possibly reflecting the need to ensure a diverse clinical training experience in units dominated by single disease subspecialty clinics. Accordingly, we strongly encourage the RRC to continue to provide adult training programs with the level of flexibility needed to organize the continuity clinic experience in such a way that maximizes trainee exposure to all relevant disease categories without disrupting disease-oriented clinical care.
Concern is raised over the small numbers of trainees who opt for single-board eligibility in hematology (10%) and pursue careers in nonmalignant hematology (< 6% of graduates of adult training programs). The discipline of hematology must strive to maintain and enhance its visibility and leadership in the fields of thrombosis, hemostasis, and vascular medicine by encouraging trainees to consider these areas of clinical and research foci.7
Despite the significant administrative efforts required, most training program directors do not receive institutional funding commensurate with the level of effort expended. We support current RRC expectations1 that directors receive adequate funding for their service.
Appendix
The other members of the ASH Committee on Training Programs during the design and conduct of the survey are as follows: Drs Dean Bajorin (Memorial Sloan-Kettering Cancer Center), Edward Ball (University of California, San Diego [UCSD]), Mark Crowther (St. Joseph's Hospital [Ontario, Canada]), Mary Cushman (University of Vermont), James George (University of Oklahoma), Kenneth Hande (Vanderbilt University), Robert Handin (Brigham and Women's Hospital), Ronald Hoffman (University of Illinois, Chicago), Alan List (Arizona Cancer Center), Ari Melnick (Mount Sinai Medical Center [New York, NY]), Donald Miller (University of Louisville), Jeanette Mladenovic (State University of New York Health Science Center [Brooklyn, NY]), Elaine Muchmore (UCSD), Stephen Nimer (Memorial Sloan-Kettering Cancer Center), David Peace (University of Illinois, Chicago), Stanley Schrier (Stanford University), and Kenneth Zuckermn (H. Lee Moffitt Cancer Center).
Prepublished online as Blood First Edition Paper, February 5, 2004; DOI 10.1182/blood-2003-11-3986.
A list of the other members of the ASH Committee on Training Programs during the design and conduct of the survey appears in the “Appendix.”
Supported by the American Society of Hematology (ASH).
An Inside Blood analysis of this article appears in the front of this issue.
We thank Alan Newman of Alan Newman Research, Inc, (Richmond, VA) for conducting the survey and data analysis; Mr Augustine Cruz and Mr Greg Volkar of ASH for assistance in preparing the survey and editorial assistance, and Ms Evelyn Mitchell for preparing the manuscript. We also wish to thank all of the program directors who responded to this survey.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal