Abstract
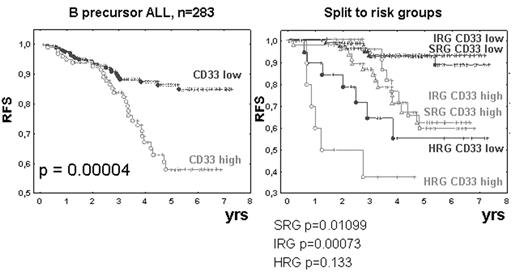
INTRODUCTION. There has been a controversy about the prognostic impact of myeloid antigens (MyAgs) in ALL. The issue has now regained significance since a monoclonal antibody (mAb) is available for clinical treatment, which is considered for AML as well as for ALL with CD33 expression. Previous studies on prognostic impact of MyAgs often combined the information on several MyAgs using logical OR or AND. Since regulation and mutual relationships of MyAg expression are unknown, a study on prognostic impact of each MyAg alone is needed. In addition, recent in vitro data showed a higher resistance for ALL blasts with MyAgs, contrasting with clinical studies showing no prognostic value of MyAgs. DESIGN. We evaluated the prognostic impact of CD33, CD13, CD15 and CD65 in uniformly treated Czech patients. PATIENTS AND METHODS. From 9/1996 to 10/2002, 343 children with ALL were enrolled in a nationwide study ALL BFM 95. In 327 patients (96%) immunophenotyping and molecular genetics was performed centrally in our reference labs. DNA index 1.16–1.6 determined hyperdiploidy. Prednisone good responders (PGR) with WBC at diagnosis <20000/uL and age 1–6yrs were assigned into standard risk group (SRG). High RG (HRG) corresponded to prednisone poor response (PPR) or no remission at day 33 or BCR/ABL or MLL/AF4 fusions. Remaining patients were in the intermediate RG (IRG). For identification of independent RFs (RFs) multivariate analysis using Cox’s proportional hazard regression was performed. The primary end point of follow up was relapse of the disease (52/327), death or treatment failure whichever occurred first. Comparisons of relapse free survival (RFS) for patients’ subgroups used log-rank statistics and Kaplan-Meier life-table estimation. Spearman R coefficient assessed relations among individual parameters and prognosis. RESULTS. Among MyAgs, only CD33 was found to be an independent RF only in B-cell precursor (BCP) ALL (n=283) but not in T ALL (n=44), therefore we excluded T ALL from further analyses. CD33 was shown to be the only independent RF among MyAgs. RFS was extremely significantly worse in BCP ALL patients with CD33 expression at or above 10% out of blasts (p=0.00004)
or 20% (p=0.00327). Patients with BCP ALL with CD33 at or above 10% had poorer RFS in separate analyses for: IRG, SRG, PGR, TEL/AML1+ and hyperdiploid (always p<0.05). In HRG, as well as in PPR we failed to prove prognostic significance of CD33 expression. Furthermore, combining the information on CD33 expression with other MyAgs reduced the level of significance. DISCUSSION. In contrast to several previous reports, we prove that CD33 is a highly significant prognostic factor in childhood BCP ALL. This was enabled by using the same clone of mAb in one laboratory throughout the study and by not combining results of several MyAgs into composite criteria. Subsets of ALL patients with CD33 expression may benefit from anti-CD33 immunotherapy. Supported by a grant IGA MZCR7430–3.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal