Abstract
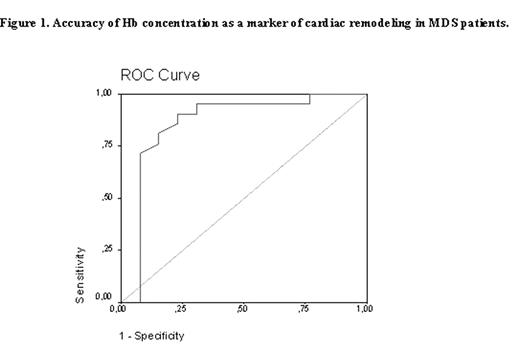
Anemia is a frequent complication in myelodysplastic syndrome (MDS). Treatment with recombinant human epoetin, though effective in up to 40% of patients, is generally limited by financial constraints. On the other hand, anemia has been associated with increased cardiac morbidity and mortality. The main hemodynamic factor is the increased cardiac output mediated by lower afterload, higher preload and positive inotropic and chronotropic effects, leading to gradual cardiac enlargement and left ventricular hypertrophy (LVH). The important relationship between anemia and cardiac morbidity has never been investigated in MDS. We evaluated this association, together with quality of life (QOL) dimensions, in a cross-sectional study in 34 MDS patients. Mean age was 70 (range 41–88) years. QOL measures were obtained by applying the MDS-specific questionnaire QOL-E©. Echocardiographic measurements were carried out according to the recommendations of the American Society of Echocardiography by an external investigator who was blind to the biochemical results. Since 11 patients were transfusion-dependent and 23 were transfusion-free with mean Hb concentration of 10.9 (SD ± 2) g/dL, two groups of patients were formed initially. The groups were comparable for body mass index (BMI), weight, age, blood pressure and heart rate. Echocardiography detected significant cardiac remodeling in 10 out of 11 transfusion-dependent vs 11 out of 23 transfusion-free patients (p=0.01), associated with lower mean Hb levels (8.7±1.5 g/dL versus 11.5±2.4 g/dL, p<0.0001) and duration of severe anemia (p=0.036). In the transfusion-dependent group, LVH was associated with higher BMI (p=0.003). In the transfusion-free group, male gender (p=0.02), age (p=0.002) and Hb levels (p=0.003) were associated with LVH. When adjusted for age and gender in a multiple stepwise backward regression, the Hb level retained its effect (p=0.019) on the occurrence of cardiac remodeling, independently of gender (p=0.042). The logistic model had an accuracy of 87% and predicted that each unit increase of Hb may lead to an average decrease of 36% in the risk of occurrence of LVH (84.5% to 14.9%) which was confirmed by the area under the ROC curve of 0.86 (p<0.0001). At Hb 10.7 g/dL, sensitivity was 95% and specificity 69%. When QOL was compared between patients as stratified by Hb cut-off level of 10.7 g/dL, functional QOL-E© scores were lower in patients with Hb values below this therapeutic threshold (54±7% versus 74±6%, p=0.03). Our current and novel results, although obtained in a small group of MDS patients, clearly illustrate the relationship between Hb levels, cardiac remodeling and QOL. It is suggested that patients should maintain nearly normal Hb levels to prevent LVH. Our pilot results warrant early epoetin treatment, though a larger follow-up trial is necessary to confirm our findings and establish whether early treatment be causally related to the reduction of risk of cardiac morbidity and mortality in responsive MDS patients.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal