Abstract
Introduction: Pulmonary hypertension (PHT) is a common complication of sickle cell disease (SCD). Most SCD patients who have PHT appear to have only mild elevations in their pulmonary artery systolic pressure (PASP). Although SCD patients with PHT have been reported to have an increased mortality, the effect of mild PHT on survival in patients with SCD remains uncertain.
Methods: The study subjects represent a cohort of patients followed at the Sickle Cell Clinic at UNC, Chapel Hill. Doppler echocardiography was used to estimate the PASP. The PASP was determined by applying the modified Bernoulli equation (PASP = 4V2 + right atrial pressure), if an adequate tricuspid regurgitant velocity was observed. A subject was considered to have PHT if his/her PASP exceeded the upper limits of normal in the age- and body mass index-adjusted reference ranges. Subjects with PHT were sub-classified into mild (above normal values up to 44 mm Hg), moderate (45 – 74 mm Hg) or severe pulmonary hypertension (≥ 75 mm Hg). Patients’ data were censored at the time of their death or loss to follow-up.
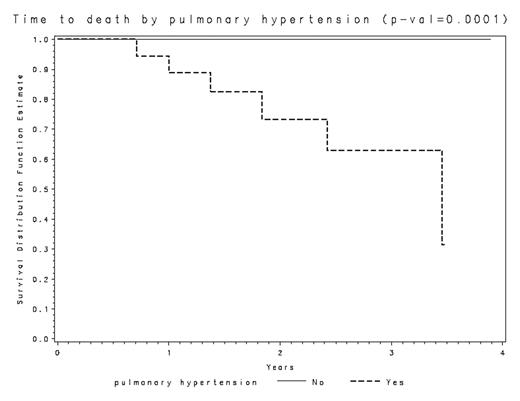
Results: The 60 subjects enrolled in this study have been followed for a period of 9 to 47 months (mean [± SD] of 29.8 ± 10.7 months). Pulmonary hypertension was observed in 18 subjects on initial evaluation, while the remaining 34 subjects had no evidence of PHT. The 18 subjects with PHT have been followed for 24.9 ± 10.6 months, while the 34 subjects without PHT have been followed for 31.8 ± 10.1 months. Six patients have died to date. All of these 6 patients had evidence of PHT, with estimated PASP values of 44, 44, 48, 54, 74 and 84 mm Hg (mean = 58 mm Hg) respectively. The presence of PHT was strongly associated with an increased risk of death (p = 0.0001). No other variables were associated with the risk of death in these patients. Although more patients with moderate and severe PHT died when compared to patients with mild PHT, the difference was not statistically significant.
Conclusion: Pulmonary hypertension is strongly associated with an increased risk of death in patients with SCD. While our study did not find a significant difference in the risk of death when patients with mild PHT were compared to patients with more severe disease, the number of patients followed was relatively small and the duration of follow-up was short. More patients and a longer period of follow-up would be required to ascertain whether the effect of mild pulmonary hypertension on mortality is different from that of more severe PHT in patients with SCD.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal