Abstract
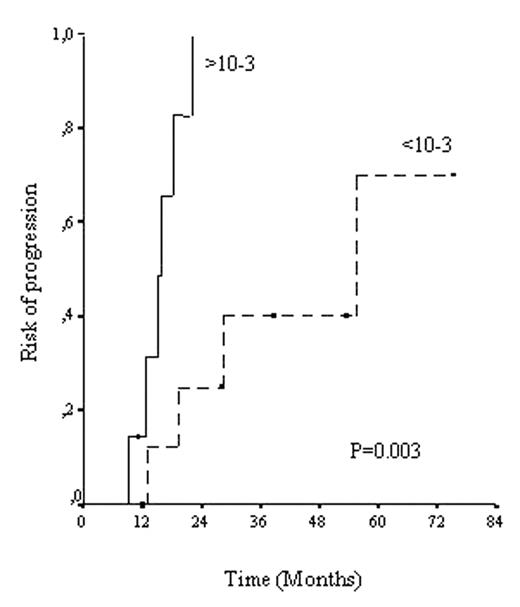
Autologous stem cell transplants (auto-SCT) are increasingly performed in patients with CLL. Although this procedure results in a high complete response (CR) rate, most patients eventually relapse. The median time to relapse is around 5 years. Increasing levels of minimal residual disease (MRD), detected by PCR or flow cytometry (FC) are associated with clinical relapse. The early detection of patients likely to relapse shortly after SCT may be useful in the management of these patients. With this background, we analyzed the levels of MRD and its correlation with the risk of relapse and clinical outcome in 19 patients with CLL submitted to auto-SCT. MRD was assessed by FC and quantitative real time PCR of the IgH region using allele-specific oligonucleotides (ASO-PCR) in peripheral blood and/or bone marrow DNA samples obtained before SCT and at different time points thereafter. After SCT, 17 patients achieved CR and 2 partial response. A continuous pattern of relapses was observed and, after a median follow-up of 48 months (range, 11–101), 11/19 patients have progressed. The median number of CLL cells detected prior to SCT was 2.4x10−2 decreasing to 5.31x10−4 at 3–6 months after auto-SCT. No further decrease was observed beyond that point. At 3–6 months after auto-SCT, only 3/17 patients in CR had undetectable levels of disease. Patients with a MRD level >10−3 at this time point (3–6 months after transplant) had a significantly higher risk of progression than those who had less than 10−3 CLL cells. All but one patients with MRD>10−3 have relapsed (7/8) whereas only 4/9 with MRD<10−3 did so. As shown in the figure, median time to progression was significantly shorter in those patients with a higher MRD level (16 vs. 55 months; p=0.003)
In conclusion, quantification of MRD within the first 6 months after auto-SCT allows the identification of CLL patients with a high risk of early clinical relapse. These data provide background to investigate whether early treatment, before clinically overt relapse occurs, might be useful in patients with high risk of relapse after SCT.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal