Abstract
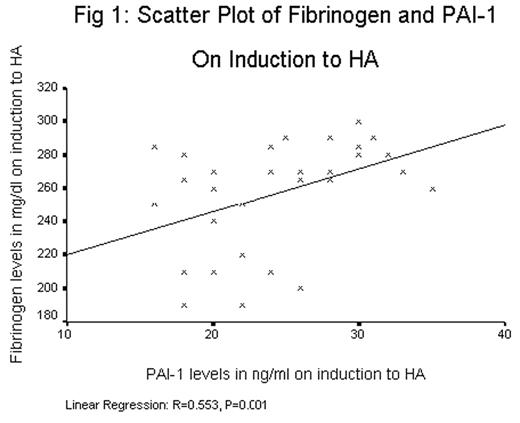
Thrombosis has been recognized as a complication of rapid ascent as well as long-term stay at high altitude (HA). Researchers have presented conflicting results and majority of them studied only short-term stay. A prospective cohort study was carried out at a height of 3500 m to study the hematological factors, which may lead to increased propensity to thrombosis on prolonged stay at HA. The subjects were healthy low landers (initial N=38, complete follow up N=32) in age group of 20–40 years, inducted to HA and investigated at induction and subsequently at 3 and 8 months. The comparison cohort was age and sex matched low landers not inducted to HA. Bleeding time, clotting time, hemoglobin (Hb), HCT, platelet count, prothrombin time, APTT, fibrinogen, d-dimers. Protein C, protein S, anti-thrombin III levels, APC resistance, PAI-1, Beta thromboglobulin (BTG) and PF4 were estimated. On induction to HA the mean Hb, platelet count, fibrinogen levels, PAI-1 levels and levels of platelet activation factors were in normal range and not statistically different from those at low altitude (P>0.05). None of the subjects had thrombophilia. There was no statistically significant change in Protein C, Protein S, AT III levels, APC resistance, BT, CT, PT and APTT. The mean values were: Hb (13.9, 15.6, 16.6 gm/dl); platelet count (255, 309, 343 x 103/mm3); fibrinogen (253, 304, 346 mg/dl); BTG (30.3, 38.5, 47.3 IU/ml); PF 4 (3.9, 7.6, 13.7 IU/ml) and; PAI-1 (23.7, 40.1, 49.3 ng/ml), at (induction, 3 months, 8 months) respectively. The P value for all was 0.000 by repeated measure analysis. The high Hb itself is unlikely to be the single cause of the thrombotic tendency at HA as its maximum value was 18.0 gm/dl. Erythrocytosis and hyper viscosity are known to activate platelets, however, platelet activation may be the result of hypoxic stress and injury to platelets or endothelium. An important finding of the study was the rise in PAI-1 levels that correlated with rise in fibrinogen levels and duration of stay at HA (Figure 1 and 2). The endothelial injury and clotting activation followed by increased fibrinolysis maintains homeostasis. We hypothesize that increased PAI-1 level tilts the balance by decreasing fibrinolytic activity and increasing propensity to thrombosis. Hypoxia during surgery is known to cause raised postoperative PAI-1 levels leading to a tendency of postoperative thrombosis. The prolonged hypoxia in a lowlander staying in HA may have a similar effect. By virtue of increased platelet count, hematocrit, platelet activation factors, PAI-1 and fibrinogen, prolonged stay at HA is a pro thrombotic state. Thus, there may be a role for antiplatelet drugs in prevention in view of the platelet hyperactivity and interventional trials with homocysteine lowering vitamins or aspirin also need to be considered.
Author notes
Corresponding author


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal