Abstract
Follicular lymphoma is generally an indolent disease with a relatively long natural history requiring multiple therapies over many years. The optimal combination and sequence of these therapies continue to evolve. Despite substantial supporting evidence (including a recently published, randomized study), the role of high dose therapy with ASCT in follicular lymphoma has been questioned. Therefore, we reviewed the Cleveland Clinic experience to determine the long-term outcome of follicular lymphoma patients according to histologic grade. Between June 1991 and June 2004, 105 patients with relapsed, grade 1–3, follicular lymphoma (without histologic transformation) received high dose CBV (n=9) or BuCyVP (n=96) and ASCT at the Cleveland Clinic. The median follow-up among survivors is 4.4 (0.1–11.4) years.
Table of patient, disease, ASCT characteristics, and outcome
| Variable . | Grade 1 (n=45) . | Grade 2 (n=36) . | Grade 3 (n=24) . | p-value . |
|---|---|---|---|---|
| Age: median (range) | 49(35–62) | 51(33–58) | 53(42–64) | 0.042 |
| Male sex: N (%) | 23(51) | 20(56) | 12(50) | 0.89 |
| Years from diagnosis to ASCT: median (range) | 3.0(0.4–15.7) | 3.0(0.9–17.6) | 2.3(0.6–15.2) | 0.34 |
| Prior # chemotherapy regimens: 2–3/>4, N (%) | 36(80)/9(20) | 32(89)/4(11) | 19(79)/5(21) | 0.49 |
| Disease status at ASCT: CR/PR, N (%) | 6(13)/33(73) | 10(28)/22(61) | 6(25)/15(63) | 0.58 |
| Bone marrow status at ASCT: +/−, N (%) | 8(23)/27(77) | 4(13)/28(88) | 4(18)/18(82) | 0.54 |
| Prior radiation therapy: N (%) | 14(31) | 11(31) | 5(21) | 0.63 |
| LDH > normal at ASCT: N (%) | 28(62) | 27(77) | 13(54) | 0.16 |
| Tumor bulk >10 cm at ASCT: N (%) | 8(18) | 6(17) | 5(21) | 0.92 |
| Disease progression: N (%) | 20(44) | 13(36) | 11(46) | – |
| Death: N (%) | 17(38) | 11(31) | 10(42) | – |
| Variable . | Grade 1 (n=45) . | Grade 2 (n=36) . | Grade 3 (n=24) . | p-value . |
|---|---|---|---|---|
| Age: median (range) | 49(35–62) | 51(33–58) | 53(42–64) | 0.042 |
| Male sex: N (%) | 23(51) | 20(56) | 12(50) | 0.89 |
| Years from diagnosis to ASCT: median (range) | 3.0(0.4–15.7) | 3.0(0.9–17.6) | 2.3(0.6–15.2) | 0.34 |
| Prior # chemotherapy regimens: 2–3/>4, N (%) | 36(80)/9(20) | 32(89)/4(11) | 19(79)/5(21) | 0.49 |
| Disease status at ASCT: CR/PR, N (%) | 6(13)/33(73) | 10(28)/22(61) | 6(25)/15(63) | 0.58 |
| Bone marrow status at ASCT: +/−, N (%) | 8(23)/27(77) | 4(13)/28(88) | 4(18)/18(82) | 0.54 |
| Prior radiation therapy: N (%) | 14(31) | 11(31) | 5(21) | 0.63 |
| LDH > normal at ASCT: N (%) | 28(62) | 27(77) | 13(54) | 0.16 |
| Tumor bulk >10 cm at ASCT: N (%) | 8(18) | 6(17) | 5(21) | 0.92 |
| Disease progression: N (%) | 20(44) | 13(36) | 11(46) | – |
| Death: N (%) | 17(38) | 11(31) | 10(42) | – |
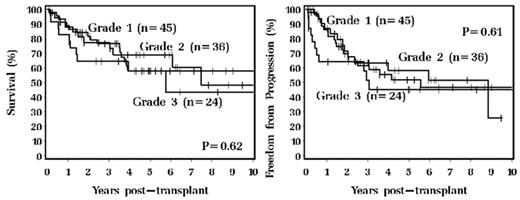
Kaplan-Meier freedom from progression and overall survival according to histologic grade are shown:
By Cox proportional univariate analysis, male sex, ≥4 prior chemotherapy regimens, and elevated LDH predicted a higher risk of progression while prior radiation therapy and bone marrow involvement predicted a higher risk of death. By Cox proportional multivariate analysis, male sex and elevated LDH predicted a higher risk of progression while prior radiation therapy and tumor bulk predicted a higher risk of death. In conclusion, approximately half of all patients that receive high dose therapy and ASCT for relapsed follicular lymphoma of any histologic grade enjoy long-term remissions and survival. ASCT remains one of the most beneficial treatment options for many patients with relapsed follicular lymphoma.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal