Abstract
The combination of cyclophosphamide, doxorubicin, vincristine, and prednisone, given every 3 weeks (CHOP-21) is standard chemotherapy for aggressive lymphomas. To determine whether CHOP given every 2 weeks (CHOP-14) or the addition of etoposide (CHOEP-21, CHOEP-14) can improve results in patients ages 18 to 60 years with good prognosis (normal lactic dehydrogenase [LDH] level), 710 patients were randomized to 6 cycles of CHOP-21, CHOP-14, CHOEP-21 (CHOP plus etoposide 100 mg/m2 days 1-3), or CHOEP-14 in a 2 × 2 factorial study design. Patients in the biweekly regimens received granulocyte colony-stimulating factor (G-CSF) starting from day 4. Patients received radiotherapy (36 Gy) to sites of initial bulky disease and extranodal disease. CHOEP achieved better complete remission (87.6% versus 79.4%; P = .003) and 5-year event-free survival rates (69.2% versus 57.6%; P = .004, primary end point) than CHOP, whereas interval reduction improved overall survival (P = .05; P = .044 in the multivariate analysis). Although the CHOEP regimens induced more myelosuppression, all regimens were well tolerated. CHOEP should be the preferred chemotherapy regimen for young patients with good-prognosis (normal LDH level) aggressive lymphoma.
Introduction
Patients younger than 60 years of age with aggressive lymphoma of the low-intermediate and low risk groups according to the International Prognostic Index1 (IPI) have a 5-year event-free survival (EFS) rate of only about 50% and 80%, respectively, which definitely warrants improvement. After the Intergroup trial2 had confirmed the CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) regimen3 as standard care, the German High-Grade Non-Hodgkin's Lymphoma Study Group (DSHNHL) decided to investigate in the non-Hodgkin lymphoma–B1 (NHL-B1) trial whether the reduction of treatment intervals from 3 to 2 weeks (CHOP-14), or the addition of etoposide, a potent antilymphoma agent, to CHOP (CHOEP-214 ), or a combination of both (CHOEP-145 ) would improve outcome for young patients with good-prognosis aggressive lymphoma.
Patients and methods
Patients
The study was conducted in accordance with the Helsinki declaration. The protocol was approved by the ethics review committee of each participating center. All patients gave written informed consent. Patients were eligible if they had previously untreated, biopsy-confirmed aggressive non-Hodgkin lymphoma according to the Revised European-American Lymphoma Classification6 (translated into the World Health Organization [WHO] classification7 ) and were between 18 and 60 years old. Excluded were patients if the diagnosis of aggressive or very aggressive lymphoma was not confirmed (ie, no pathology review was available) or if the diagnosis had to be changed into indolent lymphoma or no lymphoma at all by one of 5 expert hematopathologists who conducted a blinded central pathology review. Patients with lymphoma associated with AIDS; a history of indolent lymphoma or other neoplasms; marked impairment of cardiac, pulmonary, hepatic, or renal function; WHO performance status 4; bone marrow involvement with more than 25% lymphoma cells; initial white blood cell (WBC) count less than 3 × 109/L; initial platelet count less than 100 × 109/L; or inability to comply with study requirements were excluded. The patients had mandatory baseline examinations that included clinical examination, laboratory tests, chest radiograph, abdomen sonography, computed tomography of chest and abdomen, and a bone marrow biopsy.
Between September 1993 and June 2000, 866 patients were randomized by 140 institutions after a telephone interview. Randomization was performed at a 1:1:1:1 ratio using the minimization algorithm by Pocock8 considering stratification for centers, advanced stage III/IV, and bulky disease. All patients for whom the eligibility criteria were not confirmed after randomization were withdrawn and the balances were appropriately adjusted in the randomization program.
Treatment protocol
The CHOP regimen3 consisted of cyclophosphamide (750 mg/m2 intravenously), doxorubicin (50 mg/m2 intravenously), vincristine (2 mg intravenously) on day 1, and prednisone (100 mg orally) given on days 1 to 5. CHOEP was identical to CHOP with etoposide (100 mg/m2 intravenously) added on days 1 to 3. CHOP-21 and CHOEP-21 were recycled every 3 weeks; CHOP-14 and CHOEP-14 were recycled every 2 weeks, with patients receiving recombinant human granulocyte colony-stimulating factor (G-CSF; filgrastim) from days 4 to 13 at a dosage of 300 μg/d or 480 μg/d for patients less than 75 kg or 75 kg or more body weight, respectively. G-CSF administration in the 3-week regimens was at the discretion of the treating physician. The next chemotherapy cycle was scheduled for day 15 or 22, respectively, after recovery of WBC count (> 2.5 × 109/L) and platelet count (> 80 × 109/L). If recovery was not achieved, blood counts were repeated 3 to 4 days later, and, if necessary, 7 days later. The dosages of myelosuppressive drugs were reduced by 25% if WBC and platelet recovery exceeded 1 week, or by 50% if the delay was more than 2 weeks. Planned treatment consisted of 6 cycles of the assigned regimen. Treatment was stopped if lymphoma progressed, if the patient declined to continue with the protocol, or at the discretion of the treating physician in cases of intercurrent illness or adverse events. Patients with initial bulky disease (defined as lymphoma masses or conglomerates with a diameter ≥ 7.5 cm) received radiotherapy (36 Gy) to these areas irrespective of the result of chemotherapy. Radiotherapy at the same dose was recommended to extranodal sites of disease whenever feasible.
All patients underwent restaging 4 weeks after the end of therapy. This included the examination of all involved sites by appropriate methods. Tumor responses were classified as complete remission (CR), unconfirmed complete remission (CRu), partial remission (PR), stable disease, or progressive disease according to the International Workshop criteria9 with the modification that CR and CRu had to be confirmed by the first follow-up examination 2 months after restaging. Death during therapy or within 4 weeks after the end of therapy from causes other than lymphoma was designated as therapy-related death.
Adverse events reported by the patient or observed by the treating physician were coded on the case-report forms according to WHO grades. An adverse event was defined as any adverse change from the patient's baseline condition after the initiation of therapy, whether or not it was considered related to treatment. The WHO grades for hematotoxicity were assessed from blood counts within treatment-specific nadir windows. WHO events and therapeutic interventions between treatment arms were compared by χ2 tests and Fisher exact tests if required. For estimating the treatment duration, dose intensity and dose erosion the technique of Kaplan-Meier estimators were used as described elsewhere.10
Statistical analysis
The trial was planned in a 2 × 2 factorial design. Hence, 2 independent contrasts were subjected to significance testing: interval reduction (comparing all patients randomized to 2-weekly regimens with those in 3-weekly regimens) and addition of etoposide (comparing all patients randomized to CHOP regimens with all patients randomized to CHOEP). The NHL-B1 trial was powered to reveal an improvement of 10% in the primary end point of 2-year EFS (baseline 67%) with a power of 80% and a significance level of 5% in a 2-sided log-rank test for each of the 2 contrasts. Taking a sequential stopping procedure into account we calculated a sample size of at least 700 informative patients (PEST 2, truncated probability ratio test11 ).
The 710 eligible patients were analyzed according to their allocation by the randomization procedure, irrespective of whether they received the intended therapy or not. The primary end point was EFS, which was defined as the time from the beginning of therapy to either disease progression, initiation of additional (off-protocol) or salvage therapy, relapse, or death. The final analysis presented here proceeded as planned in the protocol. First, we checked for violations of the assumptions made in the factorial study design (ie, independence, interaction). Because no indications were found, the primary end point was analyzed on the 2 contrasts independently.
Secondary end points investigated with regard to the 2 contrasts were overall survival, defined as time from the beginning of therapy to death for any cause, the rate of CR and the rate of progression. Rates of CR and progression were defined as percentage of patients with CR/CRu (and not receiving further treatment) or progression, respectively, among all eligible patients.
Event-free and overall survival were estimated according to Kaplan and Meier.12 The estimators at 5 years for EFS and overall survival are given with the 95% confidence limits. Regarding the survival end points, independent log-rank tests for each of the factor contrasts were calculated. To investigate whether adjustment for known prognostic factors would change the conclusions regarding overall treatment effects, a proportional hazard model with only 2 factors (treatment interval and use of etoposide) was fitted adjusted for the randomization strata (stage III/IV and bulky disease) into the models. A logistic regression model was used in the same way for the CR rates and rates of progressive disease.
Some exploratory secondary analyses were performed. To investigate whether CHOEP-14 has a better tumor response than CHOEP-21 univariate χ2 and log-rank tests were performed. To evaluate the effect of each single of the 3 intensified regimens CHOP-14, CHOEP-21, and CHOEP-14, the treatment effect was modeled using 3 indicator variables in all multivariate models. CHOP-21 was considered as the baseline cohort and binary indicator variables were coded for each of the 3 other treatment arms.
Results
Patients
Between September 1993 and June 2000, 866 patients were recruited by 140 institutions. Central pathology review was done in 92% of the cases. Fifty-two patients (6%) had to be excluded because no pathology review was available and 61 patients (7%) were excluded because on pathology review the original diagnosis of aggressive lymphoma had to be changed into indolent lymphoma or no lymphoma at all. Other reasons for exclusion were missing informed consent (n = 12), concomitant other neoplastic disease (n = 4), previous treatment of lymphoma (n = 8), serious other concomitant disease (n = 2), elevated lactic dehydrogenase (LDH) level (n = 10), no information about initiation of treatment (n = 1), and other (n = 6). There were no significant differences in exclusion rates between the treatment arms. Thus, of the 710 eligible patients, 176 were randomized to CHOP-21, 172 to CHOP-14, 185 to CHOEP-21, and 177 to CHOEP-14. Except for the presence of one risk factor according to the IPI, the 4 cohorts were well balanced in clinical and pathologic characteristics (Tables 1 and 2).
Characteristics of patients included in the NHL-B1 trial
Patient characteristics . | All, % . | CHOP-21, % . | CHOP-14, % . | CHOEP-21, % . | CHOEP-14, % . | P . |
|---|---|---|---|---|---|---|
| Age, y | .951 | |||||
| 18-40 | 32.1 | 33.0 | 32.0 | 33.5 | 29.9 | |
| 41-50 | 23.5 | 21.0 | 25.6 | 23.2 | 24.3 | |
| 51-60 | 44.4 | 46.0 | 42.4 | 43.2 | 45.8 | |
| Sex | .075 | |||||
| Male | 61.7 | 65.3 | 62.2 | 65.4 | 53.7 | |
| Female | 38.3 | 34.7 | 37.8 | 34.6 | 46.3 | |
| Stage | .069 | |||||
| I | 24.2 | 25.0 | 23.3 | 26.5 | 22.0 | |
| II | 45.2 | 43.8 | 45.3 | 44.9 | 46.9 | |
| III | 17.0 | 11.9 | 22.7 | 17.8 | 15.8 | |
| IV | 13.5 | 19.3 | 8.7 | 0.8 | 15.3 | |
| III/IV | 30.6 | 31.3 | 31.4 | 28.6 | 31.1 | .933 |
| Bulky disease, 7.5 cm or more | 27.7 | 27.8 | 27.3 | 27.6 | 28.2 | .998 |
| ECOG performance status | .471 | |||||
| 0 | 72.5 | 73.9 | 73.8 | 71.9 | 70.6 | |
| 1 | 22.1 | 22.2 | 22.1 | 21.1 | 23.2 | |
| 2 | 4.9 | 4.0 | 4.1 | 7.0 | 4.5 | |
| 3 | 0.4 | 0.0 | 0.0 | 0.0 | 1.7 | |
| Higher than 1 | 5.4 | 4.0 | 4.1 | 7.0 | 6.2 | .475 |
| Extranodal sites | .680 | |||||
| No | 56.6 | 54.0 | 55.2 | 60.0 | 57.1 | |
| Yes | 43.4 | 46.0 | 44.8 | 40.0 | 42.9 | |
| More than 1 | 14.6 | 18.2 | 14.5 | 10.8 | 15.3 | .262 |
| Bone marrow involvement | 5.4 | 9.1 | 2.9 | 3.8 | 5.6 | .050 |
| B symptoms | 21.0 | 17.6 | 20.3 | 23.8 | 22.0 | .524 |
| IPI, age adjusted | .008 | |||||
| 0 | 66.8 | 64.8 | 66.3 | 70.3 | 65.5 | |
| 1 | 30.6 | 35.2 | 32.0 | 23.8 | 31.6 | |
| 2 | 2.7 | 0.0 | 1.7 | 5.9 | 2.8 |
Patient characteristics . | All, % . | CHOP-21, % . | CHOP-14, % . | CHOEP-21, % . | CHOEP-14, % . | P . |
|---|---|---|---|---|---|---|
| Age, y | .951 | |||||
| 18-40 | 32.1 | 33.0 | 32.0 | 33.5 | 29.9 | |
| 41-50 | 23.5 | 21.0 | 25.6 | 23.2 | 24.3 | |
| 51-60 | 44.4 | 46.0 | 42.4 | 43.2 | 45.8 | |
| Sex | .075 | |||||
| Male | 61.7 | 65.3 | 62.2 | 65.4 | 53.7 | |
| Female | 38.3 | 34.7 | 37.8 | 34.6 | 46.3 | |
| Stage | .069 | |||||
| I | 24.2 | 25.0 | 23.3 | 26.5 | 22.0 | |
| II | 45.2 | 43.8 | 45.3 | 44.9 | 46.9 | |
| III | 17.0 | 11.9 | 22.7 | 17.8 | 15.8 | |
| IV | 13.5 | 19.3 | 8.7 | 0.8 | 15.3 | |
| III/IV | 30.6 | 31.3 | 31.4 | 28.6 | 31.1 | .933 |
| Bulky disease, 7.5 cm or more | 27.7 | 27.8 | 27.3 | 27.6 | 28.2 | .998 |
| ECOG performance status | .471 | |||||
| 0 | 72.5 | 73.9 | 73.8 | 71.9 | 70.6 | |
| 1 | 22.1 | 22.2 | 22.1 | 21.1 | 23.2 | |
| 2 | 4.9 | 4.0 | 4.1 | 7.0 | 4.5 | |
| 3 | 0.4 | 0.0 | 0.0 | 0.0 | 1.7 | |
| Higher than 1 | 5.4 | 4.0 | 4.1 | 7.0 | 6.2 | .475 |
| Extranodal sites | .680 | |||||
| No | 56.6 | 54.0 | 55.2 | 60.0 | 57.1 | |
| Yes | 43.4 | 46.0 | 44.8 | 40.0 | 42.9 | |
| More than 1 | 14.6 | 18.2 | 14.5 | 10.8 | 15.3 | .262 |
| Bone marrow involvement | 5.4 | 9.1 | 2.9 | 3.8 | 5.6 | .050 |
| B symptoms | 21.0 | 17.6 | 20.3 | 23.8 | 22.0 | .524 |
| IPI, age adjusted | .008 | |||||
| 0 | 66.8 | 64.8 | 66.3 | 70.3 | 65.5 | |
| 1 | 30.6 | 35.2 | 32.0 | 23.8 | 31.6 | |
| 2 | 2.7 | 0.0 | 1.7 | 5.9 | 2.8 |
ECOG indicates Eastern Cooperative Oncology Group. Patient populations are as follows: all, N = 710; CHOP-21, n = 176; CHOP-14, n = 172; CHOEP-21, n = 185; and CHOEP-14, n = 177.
*Calculated for stages I-IV.
Diagnosis of patients included in the NHL-B1 trial after histopathologic review
. | All, % . | CHOP-21, % . | CHOP-14, % . | CHOEP-21, % . | CHOEP-14, % . |
|---|---|---|---|---|---|
| B-cell | 85.8 | 89.2 | 83.6 | 83.3 | 87.0 |
| Diffuse large | 59.8 | 60.2 | 57.5 | 58.3 | 62.6 |
| Centroblastic | 46.0 | 50.5 | 44.1 | 42.7 | 46.3 |
| Immunoblastic | 4.9 | 3.4 | 4.7 | 5.9 | 5.6 |
| Anaplastic | 2.4 | 0.6 | 2.3 | 3.2 | 3.4 |
| T-cell rich | 2.3 | 1.7 | 2.9 | 2.7 | 1.7 |
| NOS | 4.2 | 4.0 | 3.5 | 3.8 | 5.6 |
| Mediastinal B cell | 3.0 | 4.0 | 3.5 | 1.1 | 3.4 |
| Follicular grade 3b | 8.8 | 7.9 | 9.8 | 10.3 | 7.3 |
| Burkitt lymphoma | 1.4 | 2.3 | 1.2 | 2.2 | 0.0 |
| Aggressive marginal zone | 1.4 | 1.7 | 0.6 | 1.1 | 2.3 |
| Unspecified for technical reasons* | 5.4 | 6.3 | 3.5 | 4.9 | 6.8 |
| NOS | 6.0 | 6.8 | 7.5 | 5.4 | 4.6 |
| T-cell | 13.7 | 10.8 | 15.8 | 16.6 | 12.0 |
| Anaplastic large cell | 9.4 | 7.9 | 9.9 | 10.8 | 9.1 |
| Lymphoblastic | 0.4 | 0.6 | 1.2 | 0.0 | 0.0 |
| Peripheral T, unspecified | 2.5 | 1.7 | 3.5 | 4.2 | 0.6 |
| Angioimmunoblastic | 0.1 | 0.0 | 0.0 | 0.0 | 0.6 |
| Extranodal NK/T, nasal type | 0.7 | 0.0 | 1.2 | 1.1 | 0.6 |
| NOS | 0.6 | 0.6 | 0.0 | 0.5 | 1.1 |
| Lymphoblastic, NOS | 0.4 | 0.0 | 0.6 | 0.0 | 1.1 |
. | All, % . | CHOP-21, % . | CHOP-14, % . | CHOEP-21, % . | CHOEP-14, % . |
|---|---|---|---|---|---|
| B-cell | 85.8 | 89.2 | 83.6 | 83.3 | 87.0 |
| Diffuse large | 59.8 | 60.2 | 57.5 | 58.3 | 62.6 |
| Centroblastic | 46.0 | 50.5 | 44.1 | 42.7 | 46.3 |
| Immunoblastic | 4.9 | 3.4 | 4.7 | 5.9 | 5.6 |
| Anaplastic | 2.4 | 0.6 | 2.3 | 3.2 | 3.4 |
| T-cell rich | 2.3 | 1.7 | 2.9 | 2.7 | 1.7 |
| NOS | 4.2 | 4.0 | 3.5 | 3.8 | 5.6 |
| Mediastinal B cell | 3.0 | 4.0 | 3.5 | 1.1 | 3.4 |
| Follicular grade 3b | 8.8 | 7.9 | 9.8 | 10.3 | 7.3 |
| Burkitt lymphoma | 1.4 | 2.3 | 1.2 | 2.2 | 0.0 |
| Aggressive marginal zone | 1.4 | 1.7 | 0.6 | 1.1 | 2.3 |
| Unspecified for technical reasons* | 5.4 | 6.3 | 3.5 | 4.9 | 6.8 |
| NOS | 6.0 | 6.8 | 7.5 | 5.4 | 4.6 |
| T-cell | 13.7 | 10.8 | 15.8 | 16.6 | 12.0 |
| Anaplastic large cell | 9.4 | 7.9 | 9.9 | 10.8 | 9.1 |
| Lymphoblastic | 0.4 | 0.6 | 1.2 | 0.0 | 0.0 |
| Peripheral T, unspecified | 2.5 | 1.7 | 3.5 | 4.2 | 0.6 |
| Angioimmunoblastic | 0.1 | 0.0 | 0.0 | 0.0 | 0.6 |
| Extranodal NK/T, nasal type | 0.7 | 0.0 | 1.2 | 1.1 | 0.6 |
| NOS | 0.6 | 0.6 | 0.0 | 0.5 | 1.1 |
| Lymphoblastic, NOS | 0.4 | 0.0 | 0.6 | 0.0 | 1.1 |
Patient populations are as follows: all, N = 710; CHOP-21, n = 176; CHOP-14, n = 172; CHOEP-21, n = 185; and CHOEP-14, n = 177. NOS indicates not otherwise specified; NK, natural killer (cell).
Diagnosis of aggressive B-cell lymphoma was confirmed on pathology review; however, due to quality or quantity of the biopsy material, a further subclassification was not possible.
Treatment
All 4 treatment regimens could be administered as planned. Dosage reductions were permitted only if a treatment cycle had to be delayed by more than 1 week. This strategy resulted in median relative dosage intensities13 for the myelosuppressive drugs cyclophosphamide, doxorubicin, and etoposide (in the case of the CHOEP regimens) of 98% for CHOP-21, 97% for CHOP-14 and CHOEP-21, and 95% for CHOEP-14. Of the 171 patients with bulky disease who completed therapy, all but 19 received radiotherapy (36 Gy) to the initial site of bulky involvement (in 9 cases bulk was removed surgically, in 3 patients radiotherapy was not possible, 7 had protocol deviations). In contrast, 24 patients received radiotherapy to their largest site of involvement even though the definition of initial bulky disease (≥ 7.5 cm) was not fulfilled. These cases were counted as events at the time of initiation of radiotherapy. All these patients had been evaluated clinically as CR or CRu after 6 cycles of chemotherapy and only 5 of these patients had later relapses.
Response to treatment
The primary end point of the trial was EFS. Because no evidence for an interaction between the 2 factors etoposide and interval reduction was found in a Cox model (relative risk [RR] for interaction, 1.02; P = .943), the trial was analyzed according to the protocol in a 2 × 2 factorial design, comparing the 2 CHOP cohorts with the 2 CHOEP cohorts, and the 2 biweekly regimens with the 3-week regimens independently.
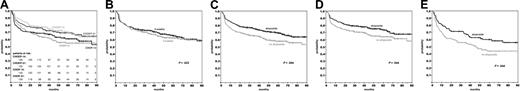
The Kaplan-Meier estimates for the primary end point EFS are shown in Figure 1. The median time of observation is 58 months. EFS curves of the 4 treatment groups are given in Figure 1A. Whereas the improvement by the reduction to 2-week intervals was not significant in (P = .622; Figure 1B), the addition of etoposide resulted in an improved EFS (P = .004; Figure 1C). This improvement was 11.6% after 5 years and was significant both for patients in limited stages I/II and for patients in advanced stages III/IV (Figure 1D-E).
EFS of 710 patients treated according to the NHL-B1 protocol. EFS according to the 4 treatment arms (A). A 2 × 2 factorial analysis comparing the 3-weekly regimens (CHOP-21/CHOEP-21) with the 2-weekly regimens (CHOP-14/CHOEP-14; B) and the CHOP regimens (CHOP-21/CHOP-14; C) with the etoposide-containing regimens (CHOEP-21/CHOEP-14). Effect of etoposide in stage I/II patients (D) and in stage III/IV patients (E). The median time of observation for all patients was 58 months.
EFS of 710 patients treated according to the NHL-B1 protocol. EFS according to the 4 treatment arms (A). A 2 × 2 factorial analysis comparing the 3-weekly regimens (CHOP-21/CHOEP-21) with the 2-weekly regimens (CHOP-14/CHOEP-14; B) and the CHOP regimens (CHOP-21/CHOP-14; C) with the etoposide-containing regimens (CHOEP-21/CHOEP-14). Effect of etoposide in stage I/II patients (D) and in stage III/IV patients (E). The median time of observation for all patients was 58 months.
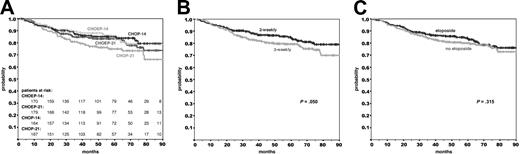
The Kaplan-Meier estimates of the secondary end point overall survival are shown in Figure 2A. The median time of observation is 58 months. Interval reduction from 3 to 2 weeks improved overall survival (P = .050; P = .044 on multivariate analysis), whereas the improvement achieved by the addition of etoposide did not provide a significant survival benefit(P = .315).
Overall survival of 710 patients treated according to the NHL-B1 protocol. Overall survival according to the 4 treatment arms (A). A 2 × 2 factorial analysis comparing the 3-weekly regimens (CHOP-21/CHOEP-21) with the 2-weekly regimens (CHOP-14/CHOEP-14; B) and the CHOP regimens (CHOP-21/CHOP-14; C) with the etoposide-containing regimens (CHOEP-21/CHOEP-14). The median time of observation for all patients was 58 months.
Overall survival of 710 patients treated according to the NHL-B1 protocol. Overall survival according to the 4 treatment arms (A). A 2 × 2 factorial analysis comparing the 3-weekly regimens (CHOP-21/CHOEP-21) with the 2-weekly regimens (CHOP-14/CHOEP-14; B) and the CHOP regimens (CHOP-21/CHOP-14; C) with the etoposide-containing regimens (CHOEP-21/CHOEP-14). The median time of observation for all patients was 58 months.
As an additional secondary end point we assessed primary outcome rates of all eligible patients based on their treatment allocation according to the randomization procedure irrespective of whether they received the intended treatment or not. The complete remission rates ranged between 80.1% in the CHOP-21 and 90.4% in the CHOEP-14 cohort (Table 3). According to this analysis (Table 4), the complete remission rates were significantly better for the etoposide-containing regimens (87.6%) than for the CHOP regimens (79.4%, P = .003), whereas the difference between the 2-weekly and 3-weekly regimens was not significant (84.6% versus 82.5%, P = .477).
Response to treatment of patients treated with CHOP-21, CHOP-14, CHOEP-21, and CHOEP-14 according to the NHL-B1 protocol
Responses . | CHOP-21, % . | CHOP-14, % . | CHOEP-21, % . | CHOEP-14, % . |
|---|---|---|---|---|
| Complete remission | 80.1 (73.4;85.7) | 78.5 (71.6;84.4) | 84.9 (78.9;89.7) | 90.4 (85.1;94.3) |
| Partial remission | 3.4 (1.3;7.3) | 6.4 (3.2;11.2) | 3.2 (1.2;6.9) | 2.8 (0.9;6.5) |
| Stable disease | 1.1 (0.1;4.0) | 2.9 (1.0;6.6) | 1.6 (0.3;4.7) | 0.0 (0.0;2.1) |
| Progressive disease | 10.2 (6.2;15.7) | 5.8 (2.8;10.4) | 7.0 (3.8;11.7) | 3.4 (1.2;7.2) |
| Therapy-associated deaths | 0.0 (0.0;2.1) | 0.0 (0.0;2.1) | 0.5 (0.0;3.0) | 1.1 (0.1;4.0) |
| Unknown response | 0.0 (0.0;2.1) | 0.6 (0.0;3.2) | 0.5 (0.0;3.0) | 0.6 (0.0;3.1) |
| Additional therapy* | 5.1 (2.4;9.5) | 5.8 (2.8;10.4) | 2.2 (0.6;5.4) | 1.7 (0.4;4.9) |
| 5-y EFS† | 54.7 (46.7;62.6) | 60.8 (52.9;68.6) | 69.2 (62.2;76.1) | 69.4 (62.0;76.8) |
| 5-y overall survival† | 74.9 (67.8;81.9) | 85.0 (79.3;90.6) | 83.3 (77.6;88.9) | 85.1 (79.3;90.9) |
Responses . | CHOP-21, % . | CHOP-14, % . | CHOEP-21, % . | CHOEP-14, % . |
|---|---|---|---|---|
| Complete remission | 80.1 (73.4;85.7) | 78.5 (71.6;84.4) | 84.9 (78.9;89.7) | 90.4 (85.1;94.3) |
| Partial remission | 3.4 (1.3;7.3) | 6.4 (3.2;11.2) | 3.2 (1.2;6.9) | 2.8 (0.9;6.5) |
| Stable disease | 1.1 (0.1;4.0) | 2.9 (1.0;6.6) | 1.6 (0.3;4.7) | 0.0 (0.0;2.1) |
| Progressive disease | 10.2 (6.2;15.7) | 5.8 (2.8;10.4) | 7.0 (3.8;11.7) | 3.4 (1.2;7.2) |
| Therapy-associated deaths | 0.0 (0.0;2.1) | 0.0 (0.0;2.1) | 0.5 (0.0;3.0) | 1.1 (0.1;4.0) |
| Unknown response | 0.0 (0.0;2.1) | 0.6 (0.0;3.2) | 0.5 (0.0;3.0) | 0.6 (0.0;3.1) |
| Additional therapy* | 5.1 (2.4;9.5) | 5.8 (2.8;10.4) | 2.2 (0.6;5.4) | 1.7 (0.4;4.9) |
| 5-y EFS† | 54.7 (46.7;62.6) | 60.8 (52.9;68.6) | 69.2 (62.2;76.1) | 69.4 (62.0;76.8) |
| 5-y overall survival† | 74.9 (67.8;81.9) | 85.0 (79.3;90.6) | 83.3 (77.6;88.9) | 85.1 (79.3;90.9) |
Patient populations are as follows: all, N = 710; CHOP-21, n = 176; CHOP-14, n = 172; CHOEP-21, n = 185; and CHOEP-14, n = 177.95% confidence intervals (Cls) are given in parentheses.
Radiotherapy in the absence of bulky disease, more than 6 cycles of chemotherapy, or alternative treatment.
Estimated after a median time of observation of 58 months.
2 × 2 factorial design analysis of treatment results of the NHL-B1 trial
Results . | CHOP-14/21, % . | CHOEP-14/21, % . | CHO(E)P-21, % . | CHO(E)P-14, % . |
|---|---|---|---|---|
| Complete remission | 79.4 (74.7;83.4) | 87.6 (83.7;90.8) | 82.5 (78.2;86.3) | 84.6 (80.3;88.2) |
| Partial remission | 4.9 (2.9;7.7) | 3.0 (1.5;5.4) | 3.3 (1.7;5.7) | 4.6 (2.6;7.3) |
| Stable disease | 2.0 (0.8;4.1) | 0.9 (0.2;2.4) | 1.4 (0.4;3.2) | 1.5 (0.5;3.3) |
| Progressive disease | 8.0 (5.4;11.4) | 5.2 (3.2;8.1) | 8.6 (5.9;12.0) | 4.6 (2.6;7.3) |
| Therapy-associated deaths | 0.0 (0.0;1.0) | 0.8 (0.2;2.4) | 0.3 (0.0;1.5) | 0.6 (0.1;2.0) |
| Unknown | 0.3 (0.0;1.6) | 0.6 (0.1;2.0) | 0.3 (0.0;1.5) | 0.6 (0.1;2.0) |
| Additional therapy* | 5.5 (3.3;8.4) | 1.9 (0.8;3.9) | 3.6 (1.9;6.1) | 3.7 (2.0;6.3) |
| 5-y EFS† | 57.6 (52.1;63.2) | 69.2 (64.1;74.3) | 62.1 (56.8;67.4) | 65.2 (59.8;70.6) |
| 5-y overall survival† | 79.9 (75.4;84.4) | 84.1 (80.0;88.2) | 79.2 (74.8;83.7) | 85.0 (81.0;89.0) |
Results . | CHOP-14/21, % . | CHOEP-14/21, % . | CHO(E)P-21, % . | CHO(E)P-14, % . |
|---|---|---|---|---|
| Complete remission | 79.4 (74.7;83.4) | 87.6 (83.7;90.8) | 82.5 (78.2;86.3) | 84.6 (80.3;88.2) |
| Partial remission | 4.9 (2.9;7.7) | 3.0 (1.5;5.4) | 3.3 (1.7;5.7) | 4.6 (2.6;7.3) |
| Stable disease | 2.0 (0.8;4.1) | 0.9 (0.2;2.4) | 1.4 (0.4;3.2) | 1.5 (0.5;3.3) |
| Progressive disease | 8.0 (5.4;11.4) | 5.2 (3.2;8.1) | 8.6 (5.9;12.0) | 4.6 (2.6;7.3) |
| Therapy-associated deaths | 0.0 (0.0;1.0) | 0.8 (0.2;2.4) | 0.3 (0.0;1.5) | 0.6 (0.1;2.0) |
| Unknown | 0.3 (0.0;1.6) | 0.6 (0.1;2.0) | 0.3 (0.0;1.5) | 0.6 (0.1;2.0) |
| Additional therapy* | 5.5 (3.3;8.4) | 1.9 (0.8;3.9) | 3.6 (1.9;6.1) | 3.7 (2.0;6.3) |
| 5-y EFS† | 57.6 (52.1;63.2) | 69.2 (64.1;74.3) | 62.1 (56.8;67.4) | 65.2 (59.8;70.6) |
| 5-y overall survival† | 79.9 (75.4;84.4) | 84.1 (80.0;88.2) | 79.2 (74.8;83.7) | 85.0 (81.0;89.0) |
Table shows CHOP-14/21 versus CHOEP-14/21 and 3-weekly CHO(E)P-21 versus 2-weekly CHO(E)P-14. 95% Cls are shown in parentheses. Patient populations are as follows: CHOP-14/21, n = 348; CHOEP-14/21, n = 362; CHO(E)P-21, n = 361; and CHO(E)P-14, n = 349.
Radiotherapy in the absence of bulky disease, more than 6 cycles of chemotherapy, or alternative treatment.
Estimated after a median time of observation of 58 months.
In a multivariate analysis of prognostic factors that included the randomization strata advanced stage and bulky disease as well as the effect of interval reduction and the addition of etoposide, advanced stage had a prognostic impact on EFS and overall survival (P < .001 and P = .004, respectively), whereas bulky disease was a prognostic factor with respect to the rate of progressive disease and overall survival (P = .014 and P = .006, respectively). The addition of etoposide had a positive effect on complete remission rate and EFS (P = .003 and P = .004, respectively), but not on overall survival (P = .276), whereas interval reduction from 3 to 2 weeks had a significant effect on the rate of progressive disease and overall survival (P = .032 and P = .044, respectively; Table 5).
Multivariate analysis of prognostic factors adjusted for randomization strata
. | No complete remission*† . | . | . | Progressive disease* . | . | . | EFS event‡§ . | . | . | Death‡ . | . | . | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Factors . | OR . | 95% CI . | P . | OR . | 95% CI . | P . | RR . | 95% CI . | P . | RR . | 95% CI . | P . | ||||||||
| Addition of etoposide | 0.54 | 0.36;0.82 | .003 | 0.63 | 0.34;1.16 | .135 | 0.70 | 0.54;0.89 | .004 | 0.83 | 0.59;1.16 | .276 | ||||||||
| Interval reduction | 0.86 | 0.57;1.28 | .453 | 0.50 | 0.27;0.94 | .032 | 0.93 | 0.73;1.20 | .588 | 0.70 | 0.50;0.99 | .044 | ||||||||
| Stage III/IV | 1.40 | 0.92;2.13 | .116 | 1.64 | 0.89;3.02 | .114 | 1.64 | 1.27;2.10 | < .001 | 1.66 | 1.18;2.35 | .004 | ||||||||
| Bulky disease | 0.95 | 0.60;1.48 | .810 | 2.15 | 1.17;3.96 | .014 | 1.13 | 0.86;1.47 | .373 | 1.63 | 1.15;2.31 | .006 | ||||||||
. | No complete remission*† . | . | . | Progressive disease* . | . | . | EFS event‡§ . | . | . | Death‡ . | . | . | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Factors . | OR . | 95% CI . | P . | OR . | 95% CI . | P . | RR . | 95% CI . | P . | RR . | 95% CI . | P . | ||||||||
| Addition of etoposide | 0.54 | 0.36;0.82 | .003 | 0.63 | 0.34;1.16 | .135 | 0.70 | 0.54;0.89 | .004 | 0.83 | 0.59;1.16 | .276 | ||||||||
| Interval reduction | 0.86 | 0.57;1.28 | .453 | 0.50 | 0.27;0.94 | .032 | 0.93 | 0.73;1.20 | .588 | 0.70 | 0.50;0.99 | .044 | ||||||||
| Stage III/IV | 1.40 | 0.92;2.13 | .116 | 1.64 | 0.89;3.02 | .114 | 1.64 | 1.27;2.10 | < .001 | 1.66 | 1.18;2.35 | .004 | ||||||||
| Bulky disease | 0.95 | 0.60;1.48 | .810 | 2.15 | 1.17;3.96 | .014 | 1.13 | 0.86;1.47 | .373 | 1.63 | 1.15;2.31 | .006 | ||||||||
OR indicates odds ratio; and RR, relative risk.
Logistic regression (OR).
No complete remission: partial response, stable disease, progressive disease, therapy-associated deaths, unknown response, additional therapy.
Cox proportional models (RR).
EFS events: progression, no complete remission at the end of treatment, relapse after complete remission, death, unplanned additional treatment or change of treatment, whatever comes first.
Sensitivity analysis
In an additional sensitivity analysis we investigated whether the slight imbalance in the cohorts with regard to the IPI factor might have an impact on treatment outcome. Multivariate modeling adjusting for IPI showed no relevant contribution. In a further analysis we investigated whether inclusion of the 52 patients excluded because of missing histopathology review would have changed the results. All these patients were treated according to the protocol and equally allocated to the treatment arms. Because about 7% of all reviews did not confirm the inclusion criteria, we estimate that about 4 of 52 patients were not eligible for the trial. The sensitivity analysis of all primary and secondary end points provided almost identical results to the analysis reported.
As can be seen from Table 3, there was a tendency of more events in the CHOP treatment arms compared to the CHOEP regimens that were due to off-protocol additional therapy (radiotherapy in the absence of bulky disease, more than 6 cycles of chemotherapy, or alternative treatment). Except for one patient in the CHOP-21 arm who received high-dose cyclophosphamide for stem cell harvesting, additional off-protocol consisted of radiotherapy in the absence of bulky disease in all other cases. Although the increased use of off-protocol additional treatment in the CHOP treatment arms was not significant, we performed a sensitivity analysis to investigate whether this imbalance had an impact on the results. Censoring these events confirmed both a significant improvement of the primary end point EFS achieved by the addition of etoposide (P = .033 in the sensitivity analysis versus .004 in the primary analysis), and the absence of a beneficial effect of interval reduction on EFS (2 versus 3 weeks P = .558 in the sensitivity analysis and P = .622 in the primary analysis).
Safety
G-CSF was mandatory in the 2-weekly regimens from days 4 to 13. Except after the last cycle, when only 90.6% of the patients in the CHOP-14 and 93.5% in the CHOEP-14 regimen received G-CSF, between 100% and 96% of the patients received the growth factor after cycles 1 to 5. In the 3-weekly regimens, G-CSF use was left to the physician's discretion and was actually given with increasing frequency over the cycles. After the fifth cycle, 6.0% in the CHOP-21 and 16.9% in the CHOEP-21 cohort received G-CSF. Leukocytopenia of grades 3 and 4 occurred less often in the 2-weekly than in the respective 3-weekly regimens (Table 6). The neutrophil nadirs occurred on days 10 to 12 of the cycle in 3-week regimens and on days 8 to 10 in the 2-week regimens.
Side effects according to treatment arms
Effects . | CHOP-21, % . | CHOP-14, % . | CHOEP-21, % . | CHOEP-14, % . | P . |
|---|---|---|---|---|---|
| Leukocytopenia | 34.1 | 33.6 | 73.6 | 72.5 | < .001 |
| Thrombocytopenia | 2.4 | 1.2 | 7.0 | 22.2 | < .001 |
| Anemia | 3.6 | 5.6 | 8.5 | 35.4 | < .001 |
| Infection | 1.8 | 4.2 | 4.4 | 5.2 | .390 |
| Mucositis | 2.9 | 3.0 | 1.6 | 6.9 | .048 |
| Cardiac toxicity | 0.6 | 0.6 | 2.8 | 0.6 | .232 |
| Neurologic toxicity | 3.5 | 0.6 | 1.6 | 3.5 | .171 |
| Renal toxicity | 0.0 | 0.0 | 0.0 | 1.2 | .182 |
| Lung toxicity | 0.0 | 0.6 | 1.7 | 1.7 | .320 |
| Nausea or vomiting | 11.7 | 6.5 | 9.4 | 8.6 | .415 |
| Alopecia | 63.6 | 64.8 | 70.9 | 67.6 | .469 |
Effects . | CHOP-21, % . | CHOP-14, % . | CHOEP-21, % . | CHOEP-14, % . | P . |
|---|---|---|---|---|---|
| Leukocytopenia | 34.1 | 33.6 | 73.6 | 72.5 | < .001 |
| Thrombocytopenia | 2.4 | 1.2 | 7.0 | 22.2 | < .001 |
| Anemia | 3.6 | 5.6 | 8.5 | 35.4 | < .001 |
| Infection | 1.8 | 4.2 | 4.4 | 5.2 | .390 |
| Mucositis | 2.9 | 3.0 | 1.6 | 6.9 | .048 |
| Cardiac toxicity | 0.6 | 0.6 | 2.8 | 0.6 | .232 |
| Neurologic toxicity | 3.5 | 0.6 | 1.6 | 3.5 | .171 |
| Renal toxicity | 0.0 | 0.0 | 0.0 | 1.2 | .182 |
| Lung toxicity | 0.0 | 0.6 | 1.7 | 1.7 | .320 |
| Nausea or vomiting | 11.7 | 6.5 | 9.4 | 8.6 | .415 |
| Alopecia | 63.6 | 64.8 | 70.9 | 67.6 | .469 |
Values in the table represent the percentage of all patients experiencing the respective side effect at least once.
Besides leukocytopenia, anemia and thrombocytopenia were the most frequent adverse events. There was a tendency for cumulative thrombocytopenia in the regimens containing etoposide. Grade 3 and 4 thrombocytopenias occurred in 7.0% of the patients treated with CHOEP-21 and 22.2% of the patients treated with CHOEP-14. Anemia increased with treatment duration and was most frequent in the CHOEP-14 regimen. The rates of red blood cell transfusions, platelet transfusions, and intravenous administration of antibiotics are shown in Table 7. There were 3 therapy-associated deaths, one (0.5%) in the CHOEP-21 and 2 (1.1%) in the CHOEP-14 cohort.
Therapeutic interventions
Interventions . | CHOP-21, % . | CHOP-14, % . | CHOEP-21, % . | CHOEP-14, % . | P . |
|---|---|---|---|---|---|
| RBC transfusions | |||||
| Per patient | 4.1 | 7.1 | 10.5 | 38.6 | < .001 |
| Per cycle | 0.9 | 1.6 | 3.4 | 11.8 | < .001 |
| Platelet transfusion | |||||
| Per patient | 0.6 | 0.0 | 1.6 | 5.1 | .002 |
| Per cycle | 0.1 | 0.0 | 0.4 | 1.1 | .001 |
| IV antibiotics | |||||
| Per patient | 25.1 | 27.4 | 40.6 | 38.1 | .003 |
| Per cycle | 8.6 | 8.5 | 15.3 | 15.0 | .001 |
Interventions . | CHOP-21, % . | CHOP-14, % . | CHOEP-21, % . | CHOEP-14, % . | P . |
|---|---|---|---|---|---|
| RBC transfusions | |||||
| Per patient | 4.1 | 7.1 | 10.5 | 38.6 | < .001 |
| Per cycle | 0.9 | 1.6 | 3.4 | 11.8 | < .001 |
| Platelet transfusion | |||||
| Per patient | 0.6 | 0.0 | 1.6 | 5.1 | .002 |
| Per cycle | 0.1 | 0.0 | 0.4 | 1.1 | .001 |
| IV antibiotics | |||||
| Per patient | 25.1 | 27.4 | 40.6 | 38.1 | .003 |
| Per cycle | 8.6 | 8.5 | 15.3 | 15.0 | .001 |
RBC indicates red blood cell; IV, intravenous.
Of the nonhematologic toxicities, neurologic side effects were not significantly different among the 4 cohorts, indicating that neither the interval reduction nor the addition of etoposide increased the neurotoxic potential of the chemotherapy (Table 6).
After a median observation time of 58 months, 20 secondary neoplasms have occurred: 4 myelodysplastic syndromes (MDSs) and acute myeloid leukemias (AMLs), 13 solid tumors, 2 acute lymphocytic leukemias, and one non-Hodgkin lymphoma of the T-cell type after a primary diffuse large B-cell lymphoma. The incidence of secondary tumors was not correlated with any particular regimen, and of the 4 cases with MDS/AML one each was observed after CHOP-14 and CHOEP-21 and 2 after CHOEP-14.
Discussion
When interpreting the data of the NHL-B1 trial it should be kept in mind that only a pair-wise comparison of the 2 CHOP with the 2 CHOEP arms and of the two 2-weekly with the two 3-weekly regimens were planned analyses according a 2 × 2 factorial design. Because no interaction term was relevant, this 2 × 2 analysis could be performed as planned according to the protocol. Results by the 4 treatment arms are only shown for reasons of exploratory or clinical information. Similarly, because the NHL-B1 trial had been designed before the publication of the IPI,1 the patients were stratified according to the presence of bulky disease and advanced stage, but not according to the IPI. Hence, subgroup and multivariate analyses were restricted to these strata.
Although other attempts to improve treatment results in young good-risk patients have failed to date,14 we can show that the addition of etoposide to the CHOP regimen resulted in a higher rate of complete remissions and a significant 12% improvement of EFS after 5 years in young patients with good prognosis aggressive lymphoma. CHOEP is therefore the first improvement for this group of patients since the introduction of the CHOP regimen 27 years ago.3 In contrast to other dosage intensifications of CHOP15 no increase in secondary MDSs and AMLs was observed after CHOEP.
The improvement with etoposide applies to the entire NHL-B1 population and was similar in patients with limited (I/II) and advanced stages (III/IV). In contrast to etoposide, interval reduction or “dose densification” improved the primary end point EFS only marginally (3.1% after 5 years), but provided a small, yet significant benefit (5.8% after 5 years) with respect to overall survival for younger patients with normal LDH levels. There is no obvious explanation why dose densification had a stronger effect on overall survival than on EFS in the NHL-B1 trial, but a similar observation was made in the NHL-B2 trial,16 where the same 4 regimens were tested in elderly patients. In the NHL-B2 trial interval reduction resulted in significantly improved CR rates, reduced progression rates, and improved EFS and overall survival. The stronger effect of dose densification on all end points in the NHL-B2 trial is not likely to be due to differences in the biology of aggressive lymphomas in young and elderly patients; rather, it might be attributable to the fact that in the NHL-B1 trial patients with elevated LDH levels were excluded. If the pretreatment LDH level can be taken as a surrogate marker for rapid tumor growth, it is conceivable that interval reduction had only a smaller effect on the comparatively slow-growing tumors with normal LDH levels included in the NHL-B1 trial.
It is a legitimate clinical question, which of the 4 treatment regimens tested in this study should be given preference. However, because the 2 × 2 factorial design of this study allows only for a pair-wise comparison of the 2-week with the 3-week regimens, our trial was not designed to answer this question. Hence, the choice between CHOP-21, CHOP-14, CHOEP-21, and CHOEP-14 cannot be made without considering clinical aspects other than efficacy, such as side effects and costs. The 11.6% gain in 5-year EFS achieved by the well-tolerated addition of etoposide to CHOP clearly favors CHOEP over CHOP in young patients. In addition, some exploratory (ie, unplanned) analyses might be helpful when discussing the preferred treatment regimen. When the 3 intensified regimens are compared in such an analysis with the standard regimen CHOP-21 (Tables 3 and 8), it becomes clear that CHOP-14 is better than CHOP-21 only with respect to survival and CHOEP-21 improves only EFS, whereas CHOEP-14 significantly improves CR rates (by 10.3%), reduces progressions under therapy (by 6.8%), and improves both EFS and overall survival (by 14.7% and 10.2%, respectively) over CHOP-21. Although such a perspective would favor CHOEP-14 as the preferred regimen, an exploratory direct comparison of CHOEP-14 with CHOEP-21 does not reveal any significant advantage for CHOEP-14 (CR rate, P = .111; progression rate, P = .121; EFS, P = .842, overall survival, P = .472) and it remains a matter of debate, whether the increased side effects of CHOEP-14 and its additional costs due to the obligatory use of G-CSF justify a preference for CHOEP-14 in all young patients with good-prognosis aggressive lymphomas. CHOEP-14 might be particularly appropriate for young low-intermediate risk patient with LDH level as the only risk factor and as a conventional chemotherapy regimen for young poor-prognosis patients who usually present with elevated LDH levels. In contrast to the elderly patients in the NHL-B2 trial, where CHOEP-14 was too toxic, caused frequent treatment delays, and resulted in an outcome inferior to CHOP-14, CHOEP-14 can be given to young patients with high-dose density and hence with noncompromised efficacy.
Comparison of treatment results of 3 intensified regimens with CHOP-21
Regimen compared with CHOP-21 . | No complete remission . | . | . | Progressive disease . | . | . | EFS event . | . | . | Death . | . | . | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | OR . | 95% Cl . | P . | OR . | 95% Cl . | P . | RR . | 95% Cl . | P . | RR . | 95% Cl . | P . | ||||||||
| CHOP-14 | 1.10 | 0.66-1.86 | .710 | 0.54 | 0.24-1.21 | .136 | 0.93 | 0.66-1.29 | .652 | 0.61 | 0.38-0.99 | .048 | ||||||||
| CHOEP-21 | 0.72 | 0.42-1.25 | .248 | 0.67 | 0.32-1.42 | .294 | 0.69 | 0.49-0.97 | .035 | 0.74 | 0.47-1.15 | .183 | ||||||||
| CHOEP-14 | 0.43 | 0.23-0.80 | .007 | 0.30 | 0.12-0.79 | .014 | 0.65 | 0.46-0.92 | .017 | 0.60 | 0.37-0.96 | .034 | ||||||||
Regimen compared with CHOP-21 . | No complete remission . | . | . | Progressive disease . | . | . | EFS event . | . | . | Death . | . | . | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | OR . | 95% Cl . | P . | OR . | 95% Cl . | P . | RR . | 95% Cl . | P . | RR . | 95% Cl . | P . | ||||||||
| CHOP-14 | 1.10 | 0.66-1.86 | .710 | 0.54 | 0.24-1.21 | .136 | 0.93 | 0.66-1.29 | .652 | 0.61 | 0.38-0.99 | .048 | ||||||||
| CHOEP-21 | 0.72 | 0.42-1.25 | .248 | 0.67 | 0.32-1.42 | .294 | 0.69 | 0.49-0.97 | .035 | 0.74 | 0.47-1.15 | .183 | ||||||||
| CHOEP-14 | 0.43 | 0.23-0.80 | .007 | 0.30 | 0.12-0.79 | .014 | 0.65 | 0.46-0.92 | .017 | 0.60 | 0.37-0.96 | .034 | ||||||||
*Logistic regression adjusted for the strata stages III/IV and bulky disease (OR).
†No complete remission: partial response, stable disease, progressive disease, therapy-associated deaths, unknown response, additional therapy.
‡Cox proportional models adjusted for the strata stages III/IV and bulky disease (RR).
§EFS events: progression, no complete remission at the end of treatment, relapse after complete remission, death, unplanned additional treatment or change of treatment, whatever comes first.
The EFS of patients treated with CHOP-21 in this trial might appear lower than expected for the study population, whereas overall survival does not. This is probably due to the rigorous definition of an event that included all patients who received more than 6 cycles of chemotherapy or received radiotherapy despite the absence of bulky disease. Most of these patients were in CR/CRu after 6 cycles of therapy and these “events” occurred in only a few of the participating institutions, suggesting that the additional therapy was not given because it was considered medically indicated, but rather because it conformed with the respective institution's usual policy.
Six cycles of CHOP and CHOEP, respectively, were given in NHL-B1, and radiotherapy was restricted to those patients who presented with bulky disease. Whether giving additional radiotherapy to all patients and not restricting it to those with bulky disease would have improved results can only be speculated on, and the same applies to the number of chemotherapy cycles. In the original CHOP protocol,3 CHOP was given 3 cycles beyond achieving complete remission, resulting in 5 to 8 cycles for most patients. Although we cannot exclude the possibility that 8 cycles of CHOP might be better than 6, no evidence from randomized trials supports this assumption; indeed, this question is currently being addressed in the ongoing RICOVER-60 trial of the DSHNHL, where elderly patients are randomized to 6 or 8 cycles of CHOP-14 with or without rituximab.
In the present study, patients with elevated LDH levels were excluded because the complementary NHL-A trial of the DSHNHL,17 which included young “high-risk” with elevated LDH levels, had also been designed and had already started before the IPI1 was published. Patients with stage I disease were included in NHL-B1. This strategy has recently been supported by the results of a Group d'Etudes des Lymphomes de l'Adult (GELA) trial in early stage aggressive lymphomas, which showed an improved outcome of young low-risk patients with full-cycle chemotherapy compared to a combined-modality approach18 ; moreover, a longer follow-up19 of a randomized trial of the Southwest Oncology Group could not confirm the previously reported advantage of a combined modality approach consisting of 3 cycles of CHOP and involved field radiotherapy over a full-cycle chemotherapy alone20 for this population. A few patients in the NHL-B1 trial (19 patients or 3%) fall into the high-intermediate risk group according to the IPI and would thus be considered to have a poor prognosis. Nevertheless, the patients in the NHL-B1 study are quite representative for the low-risk aggressive lymphoma population because 97% belong to the low and low-intermediate risk groups of the IPI.
NHL-B1 and NHL-B2 represent the first long-term improvements for young low-risk and elderly patients with aggressive lymphomas, respectively. Whether the outcome of young good-prognosis patients can be further improved by the addition of the monoclonal anti-CD20 antibody rituximab, another strategy that has recently been shown to improve results in elderly patients with aggressive lymphomas,21 can only be answered by an appropriate study. This study is currently being conducted by the Mabthera International Trial (MINT) group and recruitment was closed in October 2003 after randomization of 820 young good-prognosis patients with aggressive lymphoma.
Appendix
The membership of the DSHNHL is composed of all of the individuals who participated in the study. The following is a list of study participants. Pathologic review committee: A. C. Feller, M. L. Hansmann, H.-K. Müller-Hermelink, P. Moeller, R. Parwaresch, and H. Stein; coordinating physicians: R. Schmits and F. Hartmann, L. Trümper; reference radiotherapists: K. Schnabel and C. Rübe; biometry: M. Loeffler, D. Hasenclever, and M. Kloess; data management team: B. Mann. U. Schönwiese, A. Schöler, L. Martin Montanez, W. Beck, V. Barnstorf, G. Held, and H. Maintz. Database: M. Kunert and B. Wicklein. Institutions recruiting patients: Universitätsklinik, Köln, V. Diehl, A. Engert, and M. Reiser; Carl-Thiem-Klinikum, Cottbus, Ch. Rudolf, H. Steinhauer; Städt. Klinikum, Oldenburg, H. J. Illiger and B. Metzner; Med Universitätsklinik, Homburg, F. Hartmann, M. Pfreundschuh, and R. Schmits; Universitätskrankenhaus Eppendorf, Hamburg, D. K. Hossfeld; Klinikum der Friedrich-Schiller-Universität, Jena, K. Höffken; Ruprecht-Karls-Universität, Heidelberg, M. Baudis, A. D. Ho, and A. Krämer; Krankenhaus Maria-Hilf/Franziskushaus, Mönchengladbach, D. Kohl and H. E. Reis; Klinikum, Minden, H. Bodenstein, J. Fleeth, and D. Nischik; Universität, Würzburg, T. Wässa and K. Wilms; Krankenhaus Mutterhaus der Borromäerinnen, Trier, M. Clemens; St-Josef-/St-Marien-Hospital, Hagen, H. Eimermacher; Klinikum der Stadt, Ludwigshafen, H. Brass, M. Hoffmann, and M. Uppenkamp; Med Universitätsklinik, Münster, W. E. Berdel, R. Mesters, and P. Koch; Städt Klinikum, Darmstadt, D. Fritze and H. Schuppert; Universitätsklinikum Charité, Berlin, B. Dörken; Klinikum der Stadt, Mannheim, R. Hehlmann and F. Schlegel; Städt Krankenhaus Schwabing, München, Ch. Nerl and R. Schulz; Diakonissenkrankenhaus, Stuttgart, E. Heidemann; Klinikum der Universität, Regensburg, R. Andresen; Med Universitäts und Poliklinik, Bonn, E. Ortiz and H. Vetter; Universität, Leipzig, D. Niederwieser; Medizinische Akademie, Magdeburg, A. Franke; Katharinenhospital, Stuttgart, H. G. Mergenthaler and D. Assmann; Med Universitätsklinik, Ulm, H. Döhner, S. Wessendorf; Zentralklinikum, Augsburg, G. Schlimok; Robert-Bosch-Krankenhaus, Stuttgart, W. E. Aulitzky; Klinikum Ernst von Bergmann, Potsdam, R. Pasold; Universitätsklinik, Rostock, M. Freund; Med Hochschule, Hannover, J. Atzpodien, A. Ganser, and G. Röhrig; Bürgerhospital, Stuttgart, H. Ch. Benöhr and W. Grimminger; Städt Krankenhaus, Kiel, M. Kneba; Krankenhaus Küchwald, Chemnitz, F. Fiedler and A. Thiel; Ernst-Moritz-Arndt-Universität, Greifswald, D. Dölken, U. Hutzschenreuter, Ch. Sucker, and M. Schwenke; Evangl Krankenhaus, Hamm, L. Balleisen; Städt Krankenhaus Martha-Maria, Halle, U. Neef and W. Schütt; Universitätsklinikum, Essen, U. Dührsen; Städt Krankenanstalten, Krefeld, K. Becker, T. Frieling, and M. Planker; Klinikum Siloah, Hannover, H. Kirchner; Klinikum Großhadern, München, W. Hiddemann, Ch. Nickenig, and C. Warmuth-Lembcke; Universitätsklinikum, Marburg, A. Lorsch, U. Kaiser, and A. Neubauer; Medizinische Universität, Lübeck, T. Wagner; Städt Klinikum, Karlsruhe, Th. Fischer; Kreiskrankenhaus, Aurich, T. Langenbuch and F. Püschel; Leopoldina-Krankenhaus, Schweinfurt, W. Koch and M. Lutz; St-Antonius-Hospital, Eschweiler, R. Fuchs and S. Schäfer; Dr-Horst-Schmidt-Kliniken, Wiesbaden, N. Frickhofen; St Johannes-Hospital, Dortmund, V. Hagen and H. Pielken; Med Universitätsklinik, Bochum, U. Greven and W. Schmiegel; Krankenhaus der Barmherzigen Brüder, Trier, H. Kirchen, C. B. Kölbel, and S. Nispel; Thoraxklinik, Heidelberg, H. Bischoff and P. Drings; Westpfalz-Klinikum, Kaiserslautern, F. G. Hagmann, H. Link, and Ch. Wollermann; Marienhospital, Herne, R. Voigtmann and E. Schilling; Gemeinschaftspraxis, Jena, S. Hahnfeld and K. Ruffert; Kreiskrankenhaus Am Plattenwald, Bad Friedrichshall, P. Keller and C. Wojatschek; Klinikum Kreis Herford, U. Schmitz-Hübner; Georg-August-Universität, Göttingen, G. Brittinger, R. B. Kühn, and L. Trümper; Caritasklinik St Theresia, Saarbrücken, J. Preiß and P. Schmidt; Heinrich-Braun-KH/Städt Klinikum, Zwickau, G. Schott; Klinikum, Fankfurt/Oder, H. Burchardt; Allgemeines Krankenhaus Altona, Hamburg, D. Braumann; Kreiskrankenhaus, Neumarkt, F. Tympner; Klinikum, Aschaffenburg, W. Fischbach; Universitätsspital, Zürich, R. Stahel; Krankenhaus, Bietigheim, S. Walker; Franz-Hospital, Dülmen, G. Dresemann; Krankenhaus Altstadt, Magdeburg, E. Kettner; Zentrum für Innere Medizin, Gießen, H. Pralle; Kreiskrankenhaus, Waldbröl, H. J. Bias, L. Labedzki; St Elisabethen-Krankenhaus, Ravensburg, G. Meuret; Klinikum, Ludwigsburg, G. Liebau and D. Notnagel; St Marien-Hospital, Mühlheim/Ruhr, T. Grävinghoff, H. König and H. Lukas; St Vincenz-Krankenhaus, Limburg, K. Schalk; Gemeinschaftspraxis für Hämatologie and Intern Onkologie, Köln, St. Schmitz and T. Steinmetz; Onkologische Gemeinschaftspraxis, München, W. Abenhardt, L. Böning, D. Bosse, and F. J. Tigges; Städt Klinikum, Pforzheim, L. Theilmann; Gemeinschaftspraxis, Leipzig, A. Aldaoud, A. Schwarzer; St Johannes-Hospital, Duisburg, C. Aul; Lukaskrankenhaus, Neuss, P. Czygan; Hämatologische Praxis, Aachen, U. Essers, Guggenberger, D. Tummes, and R. Weinberg; St Marienkrankenhaus, Ludwigshafen, H. Weiss; Klinikum Lippe, Lemgo, H. Lohrmann; Caritas-Krankenhaus, Lebach, D. Hufnagel; Kreiskrankenhaus, Heidenheim, F. Klumpp; Klinikum Südstadt, Rostock, M. Kaysser; Städt Krankenhaus, Gütersloh, C. Gropp; Kreiskrankenhaus, Offenburg, F. Hirsch; Krankenhaus, Neunkirchen, W. Maurer; Kreiskrankenhaus, Bad Hersfeld, R. Paliege; Universitätsklinikum, Dresden, G. Ehninger and C. Schimming; Paracelsus-Klinik, Osnabrück, O. M. Koch; Allgemeines Krankenhaus, Celle, J. Hotz; Lungenklinik, Köln-Mehrheim, Engel-Riedel, Klüppelberg, and Stei; Klinikum, Hoyerswerda, Klabes; Gemeinschaftspraxis, Augsburg, O. Brudler and B. Heinrich; St Marienhospital, Vechta, J. Diers; Lukaskrankenhaus, Bünde, F. Müller-Faßbender; Klinikum der Innenstadt, München, B. Emmerich; Städt Klinikum, Fulda, M. Arland and C. Hofmann; Ev Krankenhaus, Oldenburg, Schwarz-Eywill; Praxis, Hamburg, U. Kleeberg; Gemeinschaftspraxis, Hannover, Gaede and H. Wysk; Evang Krankenhaus, Essen-Werden, Heit; Evang Stift St Martin gGmbH, Koblenz, Niemann and von Roye; Evang Krankenhaus Bethesda, Mönchengladbach, H. Dorst; Krankenhaus Nordwest, Frankfurt am Main, Bronzieri and A. Knuth; Praxis, Trier, M. Grundheber; Evang Diakoniekrankenhaus, Freiburg, H. Arnold; Krankenhaus Hohe Warte, Bayreuth, Seybold; Allgemeines Krankenhaus, Hagen, T. Scholten; Klinikum, Traunstein, H. G. Biedermann; Jakobi-Krankenhaus, Rheine, Bauer and G. Raschke-Günaydin; St Bonifatius Hospital, Lingen, R. Zick; Hans-Susemihl-Krankenhaus, Emden, H. Becker; Gemeinschaftspraxis, Koblenz, J. Heymanns, H. Köppler, and R. Weide; Städt Krankenhaus, München, D. Fleckenstein; Universitätsklinikum Kröllwitz, Halle, H. J. Schmoll and H. H. Wolf; Evang Krankenhaus, Unna, D. B. Einig; Rotes Kreuz Krankenhaus, Kassel, Ch. Käser and H. Urbanke-Seibert; Kreiskrankenhaus, Radebeul. Borgmann; Onkologische Fachpraxis, Köln-Kalk, D. Mainka; Triemli-Stadthospital, Zürich, L. Widmer; Evang Jung-Stiftung-Krankenhaus, Siegen, E. Jaehde; Humaine-Klinik, Bad Saarow, W. Schultze; Gemeinschaftspraxis, Minden, M. Becker and Ch. Kreisel-Büstgens; Schwerpunktpraxis für Onkologie, Aschaffenburg, M. Klausmann and G. Welslau; Deutsche Klinik für Diagnostik/Onkologie, Wiesbaden, Josten; Hämatologische-Onkologische Praxis, Mönchengladbach/Rheydt, U. Grabenhorst; Praxis für Hämatologie/Onkologie, Regensburg, R. Dengler; Evang Krankenhaus, Holzminden, Burghardt; Privatklinik, Herrsching, H. Dietzfelbinger; Gemeinschaftspraxis, Berlin, I. Blau and H. Ihle; Praxis für Hämatologie-Onkologie, Augsburg, H. R. Slawik; Praxis für Hämatologie-Onkologie, Rostock, V. Lakner; Gemeinschaftspraxis Hämatologie und Internistische Onkologie, Saarbrücken, G. Jacobs and J. Schimke; Gemeinschaftspraxis, Ansbach, M. Hahn; St Elisabeth/St Barbara-Krankenhaus, Halle/Saale, Fasshauer, Moeller, and R. Zachaeus; St Elisabeth-Krankenhaus, Saarlouis, Bilsdorfer, Brase; Städt Klinikum St Georg, Leipzig, L. Mantovani and B. Matthè; Praxis für Hämatologie und Internistische Onkologie, Norderstedt, R. Hoffmann.
Prepublished online as Blood First Edition Paper, February 24, 2004; DOI 10.1182/blood-2003-06-2094.
Supported by a grant from Deutsche Krebshilfe e.V. and unrestricted grants from Amgen and Bristol-Myers.
A complete list of the DSHNHL participants appears in the “Appendix.”
An Inside Blood analysis of this article appears in the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal