Abstract
CD4+CD25+ regulatory T (Treg) cells are pivotal for the maintenance of self-tolerance, and their adoptive transfer gives protection from autoimmune diseases and pathogenic alloresponses after solid organ or bone marrow transplantation in murine model systems. In vitro, human CD4+CD25+ Treg cells display phenotypic and functional characteristics similar to those of murine CD4+CD25+ Treg cells: namely, hyporesponsiveness to T-cell receptor (TCR) stimulation and suppression of CD25- T cells. Thus far, the detailed characterization and potential clinical application of human CD4+CD25+ Treg cells have been hampered by their paucity in peripheral blood and the lack of appropriate expansion protocols. Here we describe the up to 40 000-fold expansion of highly purified human CD4+CD25high T cells in vitro through the use of artificial antigen-presenting cells for repeated stimulation via CD3 and CD28 in the presence of high-dose interleukin 2 (IL-2). Expanded CD4+CD25high T cells were polyclonal, maintained their phenotype, exceeded the suppressive activity of freshly isolated CD4+CD25high T cells, and maintained expression of the lymph node homing receptors L-selectin (CD62L) and CCR7. The ability to rapidly expand human CD4+CD25high Treg cells on a large scale will not only facilitate their further exploration but also accelerate their potential clinical application in T cell–mediated diseases and transplantation medicine.
Introduction
Immunosuppression is an intrinsic capacity of the immune system and is partially mediated by T cells. The best-defined T-cell population with immunosuppressive activity is CD4+ and constitutively expresses the interleukin 2 receptor (IL-2R) α-chain (CD25).1 These thymus-derived suppressor cells2,3 contribute to the maintenance of self-tolerance and thereby give protection from a variety of autoimmune diseases.1,4 They control the size of the peripheral T-cell pool,5 modulate immune responses after infection6 and against tumors,7,8 and contribute to tolerance induction after solid organ transplantation.9,10 These findings confirm the central role of Treg cells in the modulation of immune responses under physiologic as well as pathologic conditions.
We and others recently showed that donor-type CD4+CD25+ Treg cells themselves do not induce graft-versus-host disease (GVHD) after major histocompatibility complex (MHC)–mismatched bone marrow transplantation but suppress GVHD induced by nonregulatory donor T cells.11-14 Importantly, cotransfer of CD4+CD25+ Treg cells neither interferes with stem cell engraftment15-17 nor abrogates the beneficial antitumor activity of donor T-cell infusions.15,18,19 These murine studies encouraged clinical transplanters to further investigate the role of donor CD4+CD25+ Treg cells for the improvement of stem cell transplantation (SCT).
CD4+ T cells with high expression levels of CD25 have been isolated from human blood, peripheral lymphoid organs, umbilical cord blood, and thymus.20-25 Phenotypically, they are comparable to their murine counterparts; that is, they constitutively express CD25, glucocorticoid-induced tumor necrosis factor receptor family–related gene (GITR) and intracellular cytotoxic T lymphocyte–associated antigen-4 (CTLA-4). In addition, expression of the transcription factor forkhead box P3 (FoxP3), described recently as a key regulatory gene for the development of CD4+CD25+ T cells in mice,26 could now be demonstrated in human CD4+CD25+ Treg cells.27 Most importantly, however, functional characteristics of murine CD4+CD25+ Treg cells could be confirmed for human CD4+CD25+/high Treg cells, such as hyporesponsiveness to T-cell receptor (TCR)–mediated stimulation and cytokine-independent, cell contact–dependent suppression of cocultured CD25- T cells.20,21,23,25 Thus, immunoregulation by CD4+CD25+ Treg cells seems to be a conserved mechanism, and their adoptive transfer or therapeutic manipulation in vivo might therefore be an attractive strategy for the prevention or treatment of T cell–mediated diseases and, in particular, for the protection from GVHD after allogeneic SCT.
The main obstacle for the clinical application of human CD4+CD25+ Treg cells so far is their paucity in peripheral blood and, in consequence, the necessity to develop reliable expansion protocols. Although several studies demonstrated that exogenous IL-2 can abrogate the anergic state of human and murine CD4+CD25+ Treg cells,4,20,21,23 efficient long-term culture and polyclonal expansion of human CD4+CD25+ Treg cells has not yet been reported. The few protocols published thus far for human CD4+CD25+ Treg cells required stimulation either by allogeneic mononuclear cells (MNCs) combined with anti-CD3 antibodies, IL-2, and allogeneic lymphoblastic feeder cells23 or by autologous in vitro differentiated dendritic cells (DCs), together with exogenous IL-2 and IL-7,28 and resulted in only a limited expansion of regulatory T cells (approximately 20-fold within 14 days and 3-fold within 7 days, respectively). Similarly, standard T-cell culture conditions or stimulation with autologous DCs resulted in only limited expansion rates in the murine system,14,29,30 and only allogeneic stimulation combined with high-dose IL-2 or the use of a superagonistic anti-CD28 antibody allowed efficient expansion of murine and rat CD4+CD25+ Treg cells, respectively.19,31 We now demonstrate that repeated stimulation with cross-linked anti-CD3 and anti-CD28 antibodies together with high-dose IL-2 results in the profound polyclonal proliferation of highly purified human CD4+CD25high T cells and their up to 40 000-fold expansion within 3 to 4 weeks. Expanded CD4+CD25high T cells retained their phenotype and showed even increased suppressive activity. In contrast to CD4+CD25- T cells, they maintained expression of the lymph node homing receptors L-selectin (CD62L) and CC chemokine receptor 7 (CCR7) during expansion. This expression profile might support the ability of expanded CD4+CD25high T cells to enter lymphatic organs after reinfusion to mediate their suppressive activity in a site-specific manner in vivo.
Materials and methods
Cell lines and culture medium
The L929-derived murine Ltk- cell line stably transfected with human FcγRII (CD32) has been described previously32 and was a kind gift from R. Levy, Stanford University (Stanford, CA). Cells were grown in RPMI 1640 (Bio Whittaker, Verviers, Belgium) with 10% fetal calf serum (FCS) (Gibco BRL, Karlsruhe, Germany), 2 mM glutamine, 10 mM HEPES (N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid), 1% nonessential amino acids (all PAN Biotech, Aidenbach, Germany), 50 U/mL penicillin, 50 μg/mL streptomycin, and 5 × 10-5 M 2-mercaptoethanol (2-ME) (all Gibco BRL) (cRPMI). Hypoxanthine, aminopterin, thymidine (HAT) selection was performed in intervals to ensure CD32 expression.
Cytokines and T-cell stimulatory antibodies
Recombinant human IL-2 (rh IL-2) (aldesleukin) was from Chiron (Amsterdam, the Netherlands); anti-CD3 (OKT3) (muromonab-CD3) was a kind gift from Ortho Biotech (Neuss, Germany); and purified anti-CD28 (CD28.2) was purchased from BD Biosciences (Heidelberg, Germany). Clinical grade beads coated with anti-CD3 and anti-CD28 antibodies (T-cell expander) were purchased from Dynal Biotech (Hamburg, Germany).
Antibodies and flow cytometry (FACS)
For fluorescence-activated cell sorter (FACS) analysis, allophycocyanin (APC)–anti-CD3 (UCHT1); APC–, peridinin chlorophyll-alpha protein (PerCP)–, and fluorescein isothiocyanate (FITC)–anti-CD4 (SK3); FITC–anti-CD19 (4G7); APC– and phycoerythrin (PE)–anti-CD25 (2A3); PE–anti-CD45RA (HI100); PE–anti-CD45RO (UCHL1); APC–anti-CD62L (DREG-56); FITC–anti-CD27 (L128); PE–anti-CD152 (BNI3); and matched mouse isotype control antibodies were from BD Biosciences. FITC–anti-CCR7 (150503) and PE–anti-GITR (110416) antibodies were from R&D Systems (Abingdon, United Kingdom). For TCR Vβ-repertoire analysis the IOTest Beta Mark kit (Beckman Coulter, Krefeld, Germany) was used. For intracellular staining, the Cytofix/Cytoperm kit (BD Biosciences) was used. All stainings were performed in phosphate-buffered saline (PBS)/2% FCS and 1% human immunoglobulin (Flebogamma) (Grifols, Langen, Germany) to block unspecific staining. Propidium iodide was added to exclude dead cells. Flow cytometry was performed on a FACSCalibur (BD Biosciences), and data were analyzed with CellQuest (BD Biosciences) or FlowJo (Treestar, Ashland, OR) software.
Cell isolation and sorting
Peripheral blood mononuclear cells (PBMCs) were isolated from leukapheresis products of healthy volunteers (after their informed consent and in accordance with protocols approved by the local authorities) by density gradient centrifugation over Ficoll/Hypaque (Pharmacia, Freiburg, Germany). Cells were stained with PE–anti-CD25 and anti-PE magnetic beads (Miltenyi Biotec, Bergisch Gladbach, Germany), and CD25+ cells were enriched with the use of the Midi-MACS system (Miltenyi Biotec). CD25-enriched and CD25-depleted cell populations were stained with FITC–anti-CD4 and sorted into CD4+CD25- and CD4+CD25high T cells on a FACStar Plus (BD Biosciences). Gates for the purification of CD4+CD25high cells were set to exclude propidium iodide (PI)–positive dead cells, to include CD4+ T cells that exceed the CD25 expression level of CD4-CD25+ cells contained in PBMCs (mostly CD19+ B cells), and to include only cells with a slightly lower CD4 expression level within the CD4+CD25high population (Figure 1). Cells were reanalyzed after sorting and routinely showed greater than 98% purity.
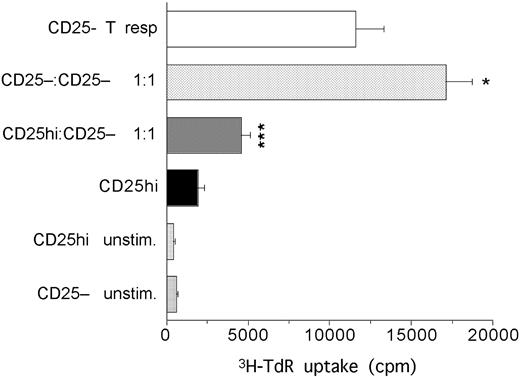
Phenotype and function of CD4+CD25high Treg cells from human peripheral blood. (A) Expression of CD4 and CD25 on human PBMCs and sort gates (i) used to isolate CD4+CD25- (ii) and CD4+CD25high T cells (iii). Numbers indicate the precentage of cells in each quadrant. (B) Intracellular expression of CTLA-4 and surface expression of CD62L and CCR7 on sorted CD4+CD25- T cells (solid line histogram in i; also ii) and CD4+CD25high Treg cells (gray histogram in i; also iii). Dotted line indicates isotype control. (C) CD4+ T cells (Tresp) were cultured either for 5 days with irradiated allogeneic stimulator cells (i) or for 4 days with irradiated autologous PBMCs and soluble anti-CD3 (ii) and variable numbers of CD4+CD25high or CD4+CD25- T cells to obtain the indicated ratios. ***P < .001 (Student t test). *P < .05. Panels show 1 of at least 3 independent experiments using cells from different donors. Error bars represent standard deviation from the triplicate wells.
Phenotype and function of CD4+CD25high Treg cells from human peripheral blood. (A) Expression of CD4 and CD25 on human PBMCs and sort gates (i) used to isolate CD4+CD25- (ii) and CD4+CD25high T cells (iii). Numbers indicate the precentage of cells in each quadrant. (B) Intracellular expression of CTLA-4 and surface expression of CD62L and CCR7 on sorted CD4+CD25- T cells (solid line histogram in i; also ii) and CD4+CD25high Treg cells (gray histogram in i; also iii). Dotted line indicates isotype control. (C) CD4+ T cells (Tresp) were cultured either for 5 days with irradiated allogeneic stimulator cells (i) or for 4 days with irradiated autologous PBMCs and soluble anti-CD3 (ii) and variable numbers of CD4+CD25high or CD4+CD25- T cells to obtain the indicated ratios. ***P < .001 (Student t test). *P < .05. Panels show 1 of at least 3 independent experiments using cells from different donors. Error bars represent standard deviation from the triplicate wells.
T-cell expansion cultures
FACS-purified CD4+CD25high or CD4+CD25- T cells (2 × 104 per well) were placed into 96-well flat-bottom plates with 1.5 × 104 irradiated (70 Gy) CD32+ L cells.32 Cultures were in 200 μL cRPMI with 100 ng/mL OKT3, 100 ng/mL anti-CD28 antibody (Ab), and 300 U/mL IL-2. After 5 to 6 days, cells were harvested, and 1 × 105 T cells were cocultured with 8 × 104 CD32+ L cells in 500 μL cRPMI supplemented with Abs and IL-2 in 24-well plates. Cultures were supplemented with 200 μL cRPMI/IL-2 after 4 days and split onto fresh CD32+ L cells once per week.
Helper cell–free expansion cultures were performed in 96-well U-bottom plates by adding T-cell expander beads at a ratio of 4 beads per cell to 2 × 104 CD4+CD25high T cells for the first week, and at a 1:1 ratio with 5 × 105 cells per well in 24-well plates thereafter. Cells were cultured in cRPMI with 300 U/mL IL-2, fed with cRPMI/IL-2 after 4 days, and restimulated with fresh beads weekly. CD4+CD25- T cells were stimulated as CD4+CD25high T cells for the first 2 weeks and later on with a reduced ratio of 1 bead per 10 cells. T-cell expansion was determined by counting trypan blue–negative aliquots in approximately weekly intervals.
Stimulation assay and MLR
For polyclonal stimulation, 5 × 104 purified CD4+ responder T cells (Tresp) (selected from PBMCs with anti-CD4 MACS beads; Miltenyi Biotec) were cocultured in 96-well U-bottom plates with 5 × 104 irradiated (30 Gy) autologous PBMCs in the presence of 100 ng/mL OKT3 in 200 μL cRPMI. Where indicated, titrated numbers of freshly purified or in vitro expanded autologous CD4+CD25high T cells were added to obtain the ratios described. Expanded T cells were harvested and rested in IL-2 containing cRPMI 48 hours prior to use. Cultures were incubated for 4 days and labeled with 0.5 μCi (0.0185 MBq) [3H]thymidine ([3H]TdR) (Hartmann Analytics, Braunschweig, Germany) per well for the last 18 hours. [3H]thymidine incorporation was measured by liquid scintillation counting (Top Count; Perkin Elmer, Rodgau-Jügesheim, Germany). Mixed lymphocyte reactions (MLRs) were performed similarly, with 1 × 105 CD4+ Tresp cells, graded numbers of autologous CD4+CD25high T cells, and 1 × 105 irradiated allogeneic PBMCs as stimulators, and were harvested after 5 days. All assays were performed in triplicate.
For neutralization experiments, antibodies to human IL-4 (5 μg/mL MP4-25D2; BD Biosciences), IL-10 (1 μg/mL JES3-19F1; BD Biosciences), and transforming growth factor–β (TGF-β) (5 μg/mL 1D11; R&D Systems) were added at the start of the cocultures. Antibody concentrations neutralize up to 200 ng/mL IL-4, 50 ng/mL IL-10, and 12.5 ng/mL TGF-β.
For select experiments, 2 × 104 FACS-sorted CD4+CD25high or CD4+CD25- T cells were seeded in 96-well U-bottom plates precoated with anti-CD3 (10 μg/mL) and costimulated with soluble anti-CD28 (100 ng/mL), with or without IL-2 (300 U/mL), for 3 days. In parallel, 2 × 104 FACS-sorted CD4+CD25high or CD4+CD25- T cells were seeded in 96-well flat bottom plates with 1.5 × 104 irradiated CD32+ L cells, and stimulated with anti-CD3 and anti-CD28 (100 ng/mL each) and/or IL-2 (300 U/mL) for 3 days. Cultures were labeled with 0.5 μCi (0.0185 MBq) [3H]thymidine for the last 18 hours.
Cytokine detection
First, 5 × 104 FACS-sorted or in vitro–expanded (on either L cells or on beads) CD4+CD25high or CD4+CD25- T cells were seeded in new wells and (further) incubated under the respective culture conditions (L cell based or bead based) for 3 days. For detection of endogenous IL-2, parallel cultures were set up without rh IL-2. Supernatants were collected and analyzed for IL-2, IL-4, IL-10, tumor necrosis factor-α (TNF-α), and interferon-γ (IFN-γ) using the human T-helper 1 (Th1)/Th2 competitive binding assay (CBA) kit from BD Biosciences. TGF-β was determined by enzyme-linked immunosorbent assay (ELISA) (R&D Systems) following the manufacturer's recommendations.
Statistical analysis
Differences in proliferation of Tresp cells were analyzed by means of the 2-tailed Student t test. P less than .05 was considered significant.
Results
Highly purified human CD4+CD25high T cells are anergic and suppressive
Coexpression of CD4 and CD25 has been used to identify Treg cells in mice and humans. However, human PBMCs contain not only CD4+CD25+ T cells with regulatory function, but also substantial numbers of CD4+CD25int T cells, which predominantly represent recently activated cells25 (Figure 1Ai). Since the goal of this study was the expansion of the Treg-cell population, we aimed at isolating them at highest purity. In consequence, only CD4+ T cells with a CD25 expression level exceeding that of CD4-CD25+ cells within PBMCs (predominantly activated B cells) were FACS sorted to greater than 98% purity (Figure 1Aiii). These CD4+CD25high T cells represented, on average, 1.8% of PBMCs (range, 1.1% to 3.4%; n = 20 analyses with cells from 13 different donors) and showed a slightly, but reproducibly, lower CD4 expression than the CD4+CD25int cells (Figure 1Ai), probably owing to their smaller size, as revealed in the forward scatter channel (FSC) (data not shown). When compared, CD25high and CD25-CD4+ T cells differed not only in their CD25, but also in their intracellular CTLA-4 expression levels (Figure 1Bi), while both T-cell populations were predominantly double-positive for the lymph node (LN) homing receptors CCR7 and CD62L (Figure 1Bii-iii).
We tested the suppressive activity of sorted CD4+CD25high T cells through their ability to inhibit the proliferation of autologous CD4+ T cells after allogeneic stimulation in MLRs. CD4+ responder T cells, in contrast to FACS-purified CD4+CD25high T cells, showed a vigorous proliferative response to irradiated PBMCs from an unrelated donor that was dose-dependently inhibited up to 60% at a 1:1 ratio upon coculture of the 2 cell populations (Figure 1Ci). In contrast, FACS-sorted CD4+CD25- T cells did not inhibit the proliferation of CD4+ responder T cells in cocultures (Figure 1Ci). Similarly, freshly purified CD4+CD25high T cells were hyporesponsive to polyclonal stimulation provided by anti-CD3 antibodies in the presence of autologous PBMCs, but suppressed the proliferation of CD4+ responder T cells with even higher efficiency (89% at a 1:1 ratio) in this assay system (Figure 1Cii).
Polyclonal expansion of highly suppressive CD4+CD25high Treg cells after strong costimulation provided by artificial antigen-presenting cells
As previously described for human CD4+CD25+ Treg cells, the anergic state of pure CD4+CD25high T cells was abrogated after simultaneous stimulation via TCRs and CD28 in the presence of IL-2, while neither IL-2 nor platebound anti-CD3 combined with soluble anti-CD28 could break their unresponsiveness (Figure 2A). Since these results suggested that CD4+CD25high T cells were not per se incapable of proliferating, we next examined whether their long-term and large-scale expansion could be achieved under adequate costimulatory conditions. We applied a previously described culture system in which stimulatory antibodies are presented by FcγRII (CD32)–bearing L cells.32 Neither CD4+CD25high nor CD4+CD25- T cells proliferated upon coculture with L cells alone or additional IL-2. However, the combined stimulation via CD3 and CD28 in the presence of CD32+ L cells was sufficient to induce proliferation in both populations, which was further enhanced by IL-2 and reached maximum levels at 100 to 1000 U/mL (Figure 2A and data not shown). In consequence, saturating doses of 300 U/mL IL-2 were used in all subsequent experiments. CD4+CD25high T cells cultured under these conditions expanded dramatically with an average 13 000-fold (range, 1250- to 39 600-fold) increase in cell numbers within 3 to 4 weeks (n = 9 cultures from separate leukaphereses of 5 donors) (Figure 2B). Although CD4+CD25high T-cell expansion usually slowed down after 4 weeks, individual cultures were propagated for more than 3 months with a maximum expansion rate of 1.2 × 109. Expansion of CD4+CD25- T cells from the same donors cultured in parallel usually exceeded that of CD4+CD25high T cells and resulted in an average 28 900-fold expansion (range, 2200- to 56 900-fold) within 3 to 4 weeks (n = 9 cultures from separate leukaphereses of 5 donors; data not shown).
Large-scale expansion of polyclonal CD4+CD25high T cells on CD32+ L cells. (A) Proliferation of sorted CD4+CD25high T cells and CD4+CD25- T cells in response to IL-2, anti-CD3/anti-CD28 (precoated and soluble, respectively), or both in the presence or absence of irradiated CD32+ L cells. One of 3 independent experiments using cells from 3 different donors. (B) Expansion of sorted CD4+CD25high T cells (n = 9 individual cultures) cultured on irradiated CD32+ L cells with anti-CD3 and anti-CD28 Abs plus IL-2. Symbols indicate different donors (n = 5). (C) TCR Vβ-repertoire of primary and 25-day–expanded CD4+CD25high and CD4+CD25- T cells. One of 5 individual cultures with cells from 5 different donors.
Large-scale expansion of polyclonal CD4+CD25high T cells on CD32+ L cells. (A) Proliferation of sorted CD4+CD25high T cells and CD4+CD25- T cells in response to IL-2, anti-CD3/anti-CD28 (precoated and soluble, respectively), or both in the presence or absence of irradiated CD32+ L cells. One of 3 independent experiments using cells from 3 different donors. (B) Expansion of sorted CD4+CD25high T cells (n = 9 individual cultures) cultured on irradiated CD32+ L cells with anti-CD3 and anti-CD28 Abs plus IL-2. Symbols indicate different donors (n = 5). (C) TCR Vβ-repertoire of primary and 25-day–expanded CD4+CD25high and CD4+CD25- T cells. One of 5 individual cultures with cells from 5 different donors.
To differentiate CD4+CD25high T-cell expansion that was was polyclonal from that driven by individual T-cell clones, TCR Vβ-analysis was performed. CD4+CD25high T cells within unmanipulated PBMCs showed a polyclonal Vβ-usage similar to that of CD4+CD25- T cells (Figure 2C). After isolation and in vitro expansion for 25 days, their TCR Vβ-repertoire did not differ significantly either from that of freshly isolated CD4+CD25high T cells or from that of freshly isolated or expanded CD4+CD25- T cells (Figure 2C). Thus, CD4+CD25high T cells expanded polyclonally and without loss of clonotypes under these culture conditions.
FACS analysis of CD4+CD25high T-cell populations expanded beyond 2 and 3 weeks revealed a CD45ROhigh and CD45RAlow phenotype, reflecting their activated state (data not shown). In addition, expression of CD25 and intracellular CTLA-4 was further up-regulated as compared with freshly isolated CD4+CD25high T cells from the same donor (Figures 3A, i and iii, and 1A-B). In comparison, up-regulation of CD25 and CTLA-4 by expanded CD4+CD25- T cells was more heterogeneous and did not show the uniformly high levels of CD4+CD25high T cells, whereas both populations comparably up-regulated GITR expression after expansion (Figure 3A, i and iii, and data not shown). CD4+CD25high T cells expanded for 2 weeks maintained high expression levels for both CD62L and CCR7, whereas CD4+CD25- T cells rapidly lost CCR7 expression upon in vitro culture and significantly down-regulated CD62L within the first 2 weeks (Figure 3A, ii). Even after more than 3 weeks in culture, CD4+CD25high T cells still remained CD25high and CD62L+, with close to 30% of them still expressing CCR7 (Figure 3A, iii and iv). Thus, in vitro expanded CD4+CD25high T cells maintained phenotypic characteristics of Treg cells and clearly differed from expanded CD4+CD25- T cells.
Treg-cell characteristics in expanded CD4+CD25high T cells. Expanded CD4+CD25high T cells retain phenotypical and functional characteristics of Treg cells. (A) Surface expression of CD25, CD62L, and CCR7, and intracellular expression of CTLA-4 of CD4+CD25high T cells (gray histograms and right dot plots) and CD4+CD25- T cells (solid line histograms and left dot plots) expanded for 2 weeks (i-ii) or 3.5 weeks (iii-iv) on CD32+ L cells. Dotted line in i and iii indicates isotype control. Numbers indicate the percentage of cells within each quadrant. (B) CD4+ Tresp cells were stimulated with allogeneic PBMCs (i), or with anti-CD3 Ab and autologous PBMCs (ii) for 5 or 4 days, respectively. CD4+CD25high or CD25- T cells, expanded on CD32+ L cells for 23 days and then rested for 2 days, were added at variable numbers to obtain the indicated ratios. ***P < .001 (Student t test). *P < .05. One of at least 4 independent experiments using cells from different donors. Error bars represent standard deviations for triplicate wells.
Treg-cell characteristics in expanded CD4+CD25high T cells. Expanded CD4+CD25high T cells retain phenotypical and functional characteristics of Treg cells. (A) Surface expression of CD25, CD62L, and CCR7, and intracellular expression of CTLA-4 of CD4+CD25high T cells (gray histograms and right dot plots) and CD4+CD25- T cells (solid line histograms and left dot plots) expanded for 2 weeks (i-ii) or 3.5 weeks (iii-iv) on CD32+ L cells. Dotted line in i and iii indicates isotype control. Numbers indicate the percentage of cells within each quadrant. (B) CD4+ Tresp cells were stimulated with allogeneic PBMCs (i), or with anti-CD3 Ab and autologous PBMCs (ii) for 5 or 4 days, respectively. CD4+CD25high or CD25- T cells, expanded on CD32+ L cells for 23 days and then rested for 2 days, were added at variable numbers to obtain the indicated ratios. ***P < .001 (Student t test). *P < .05. One of at least 4 independent experiments using cells from different donors. Error bars represent standard deviations for triplicate wells.
Next we examined whether expanded CD4+CD25high T cells maintained their suppressive activity. To this end, expanded CD4+CD25high T cells were rested in IL-2–containing medium without L cells and antibody stimulation for 48 hours. Rested CD4+CD25high T cells reverted to their anergic state and did not proliferate in response to allogeneic stimulation (Figure 3Bi). In contrast, freshly isolated CD4+ T cells proliferated well under these conditions, and their proliferation was dose-dependently suppressed in cocultures with in vitro expanded CD4+CD25high T cells (Figure 3Bi). Interestingly, suppression by expanded CD4+CD25high T cells on a per cell basis was stronger than that of freshly isolated CD4+CD25high T cells from the same donor, still resulting in a highly significant reduction of [3H]thymidine incorporation at a 1:8 ratio of CD4+CD25high T cells to responder T cells (compare Figures 3Bi and 1Ci). In contrast to CD4+CD25high T cells, in vitro expanded CD4+CD25- T cells did not suppress the proliferation of responder T cells.
Similarly, expanded CD4+CD25high T cells were also hyporesponsive to polyclonal stimulation but showed a significantly enhanced activity for the suppression of freshly isolated CD4+ responder T cells. [3H]thymidine incorporation was reduced by greater than 65%, even at a 1:16 ratio of CD4+CD25high T cells to responder T cells (Figure 3Bii). Although never to the same extent as CD4+CD25high T cells, CD4+CD25- T cells expanded beyond 3 weeks also diminished [3H]thymidine incorporation in this assay system. This effect probably reflects different proliferation kinetics of long-term–cultured T cells, resulting in earlier exhaustion of the cultures and/or higher cytokine consumption after their polyclonal restimulation, since it was only sporadically observed with CD4+CD25- T cells expanded up to 2 weeks (data not shown) and never occurred in MLR assays (Figures 3Bi and 4D).
Polyclonal expansion of sorted CD4+CD25high T cells with bead-coupled anti-CD3/anti-CD28 Abs and high-dose IL-2. Sorted CD4+CD25high T cells can be expanded polyclonally with bead-coupled anti-CD3/anti-CD28 Abs and high-dose IL-2 without down-regulation of LN homing receptors or loss of suppressive function. (A) Sorted CD4+CD25high T cells (n = 7 individual cultures) were stimulated with anti-CD3/anti-CD28–coated beads plus IL-2. Symbols indicate different donors (n = 5; same as in Figure 2). (B) TCR Vβ-repertoire of CD4+CD25high and CD4+CD25- T cells before and after expansion for 24 days with Ab-coated beads and IL-2. One of 5 different cultures with cells from 5 different donors. (C) Surface expression of CD25, CD62L, CCR7, and CD27, and intracellular expression of CTLA-4 of CD4+CD25high T cells (gray histograms in i and ii; and iv and vi) and CD4+CD25- T cells (solid-line histograms in i and ii; and iii and v) after expansion with Ab-coated beads and IL-2 for 3 weeks. Dotted line indicates isotype control. Numbers indicate the percentage of cells within each quadrant. (D) CD4+ Tresp cells were stimulated with allogeneic PBMCs for 5 days. CD4+CD25high T cells, freshly isolated or expanded with Ab-coated beads for 13 or 22 days and then rested for 2 days, were added at variable numbers to obtain the indicated ratios. One of 3 independent experiments using cells from different donors. Error bars represent standard deviations from triplicate wells.
Polyclonal expansion of sorted CD4+CD25high T cells with bead-coupled anti-CD3/anti-CD28 Abs and high-dose IL-2. Sorted CD4+CD25high T cells can be expanded polyclonally with bead-coupled anti-CD3/anti-CD28 Abs and high-dose IL-2 without down-regulation of LN homing receptors or loss of suppressive function. (A) Sorted CD4+CD25high T cells (n = 7 individual cultures) were stimulated with anti-CD3/anti-CD28–coated beads plus IL-2. Symbols indicate different donors (n = 5; same as in Figure 2). (B) TCR Vβ-repertoire of CD4+CD25high and CD4+CD25- T cells before and after expansion for 24 days with Ab-coated beads and IL-2. One of 5 different cultures with cells from 5 different donors. (C) Surface expression of CD25, CD62L, CCR7, and CD27, and intracellular expression of CTLA-4 of CD4+CD25high T cells (gray histograms in i and ii; and iv and vi) and CD4+CD25- T cells (solid-line histograms in i and ii; and iii and v) after expansion with Ab-coated beads and IL-2 for 3 weeks. Dotted line indicates isotype control. Numbers indicate the percentage of cells within each quadrant. (D) CD4+ Tresp cells were stimulated with allogeneic PBMCs for 5 days. CD4+CD25high T cells, freshly isolated or expanded with Ab-coated beads for 13 or 22 days and then rested for 2 days, were added at variable numbers to obtain the indicated ratios. One of 3 independent experiments using cells from different donors. Error bars represent standard deviations from triplicate wells.
Helper cell–free expansion of human CD4+CD25high Treg cells
For clinical applications, a helper cell–free expansion protocol for CD4+CD25high T cells would be preferable. We therefore applied clinical grade beads coated with anti-CD3 and anti-CD28 antibodies plus IL-2 to induce proliferation in CD4+CD25high T cells. While the dose of beads recommended for non-Treg cells was insufficient for sustained CD4+CD25high T-cell proliferation (data not shown), significant expansion was observed when a high bead-cell ratio was used for the initiation of cultures (4 beads per cell) as well as their long-term propagation (1 bead per cell). Although less efficiently than in L cell cultures, CD4+CD25high T cells still expanded on average 2775-fold (range, 620- to 6870-fold) within 3 to 4 weeks (Figure 4A; n = 7 cultures from individual leukapheresis products derived from 5 different donors).
TCR Vβ-screening performed on day 24 confirmed that bead-cultured CD4+CD25high T cells also expanded polyclonally, since the Vβ-usage of expanded cells did not differ significantly either from that of freshly isolated CD4+CD25high T cells or from that of freshly isolated or bead-expanded CD4+CD25- T cells (Figure 4B). Similarly to L cell–expanded cells, both populations completely converted to a CD45RO+ state, and both showed upregulation of GITR expression after 2 and 3 weeks of expansion (data not shown). In addition, bead-expanded CD4+CD25high T cells showed a homogeneous up-regulation of CD25 and CTLA-4 and a sustained expression of CD62L, CCR7, and CD27 (Figure 4C), whereas bead-expanded CD4+CD25- T cells again differed in their CD25 and CTLA-4 expression levels, completely down-regulated CCR7, and substantially decreased their CD62L and CD27 expression (Figure 4C). The suppressive activity of bead-expanded CD4+CD25high T cells after allogeneic stimulation, as determined after 2 or 3.5 weeks of expansion, was comparable to that of L cell–expanded CD4+CD25high T cells and again significantly stronger than that of freshly isolated CD4+CD25high T cells from the same donor (Figure 4D). Similar results were obtained after polyclonal stimulation (data not shown). Hence, CD4+CD25high T cells expanded under helper cell–free conditions retained their characteristic phenotype as well as their suppressive function.
Next we examined, whether expanded CD4+CD25high T cells suppress not only naive, but also preactivated, responder T cells. When polyclonally expanded CD4+CD25- T cells were rested for 2 days in IL-2–containing medium and then tested in the MLR, they responded well to allogeneic restimulation. Addition of in vitro expanded CD4+CD25high T cells suppressed their alloresponse, while addition of in vitro expanded CD4+CD25- T cells further increased [3H]thymidine uptake (Figure 5). Thus, in vitro expanded CD4+CD25- T cells are susceptible to restimulation and to suppression by CD4+CD25high T cells, while expanded CD4+CD25high T cells suppress both naive (Figures 3, 4) and antigen-experienced T cells.
Effect of expanded CD4+CD25high T cells on the alloresponse of antigen-experienced responder T cells. Expanded CD4+CD25high T cells suppress the alloresponse of antigen-experienced responder T cells. Sorted CD4+CD25- T cells were expanded with anti-CD3/anti-CD28–coated beads, rested for 2 days, and then stimulated with irradiated allogeneic PBMCs in the absence or presence of autologous expanded CD4+CD25high or CD25- T cells at a 1:1 ratio for 5 days. ***P < .001(Student t test). *P < .05. One of 3 independent experiments using cells from different donors.
Effect of expanded CD4+CD25high T cells on the alloresponse of antigen-experienced responder T cells. Expanded CD4+CD25high T cells suppress the alloresponse of antigen-experienced responder T cells. Sorted CD4+CD25- T cells were expanded with anti-CD3/anti-CD28–coated beads, rested for 2 days, and then stimulated with irradiated allogeneic PBMCs in the absence or presence of autologous expanded CD4+CD25high or CD25- T cells at a 1:1 ratio for 5 days. ***P < .001(Student t test). *P < .05. One of 3 independent experiments using cells from different donors.
Suppression by expanded CD4+CD25high T cells is cytokine independent
Cytokine secretion of CD4+CD25high T cells expanded under both culture conditions was compared with that of freshly sorted CD4+CD25high T cells stimulated for 72 hours in L cell cultures or with CD3/CD28 beads (Figure 6A). Neither fresh nor expanded CD4+CD25high T cells produced significant amounts of IL-2 or TNF-α, and both produced only marginal amounts of IFN-γ. TGF-β production by fresh and expanded CD4+CD25high T cells was slightly increased upon L cell–based stimulation, while IL-4 production was increased in CD4+CD25high T cells expanded under both conditions as compared with freshly sorted CD4+CD25high T cells. Most strikingly, IL-10 secretion by expanded cells significantly exceeded that of freshly isolated CD4+CD25high T cells. In comparison, freshly isolated CD4+CD25- T cells secreted at least 2 log higher amounts of IL-2, IFN-γ, and TNF-α, but no detectable IL-4 or IL-10 and only marginal amounts of TGF-β. After expansion, IL-2, IFN-γ, and TNF-α stayed high while IL-4 and IL-10 were up-regulated to levels comparable to those of expanded CD4+CD25high T cells (data not shown).
Immunosuppressive cytokines of CD4+CD25high T cells. CD4+CD25high T cells produce immunosuppressive cytokines, but their mode of suppression is cytokine independent. (A) First, 5 × 104 CD4+CD25high T cells, freshly sorted or expanded either on CD32+ L cells or with anti-CD3/anti-CD28–coated beads (TCE) were stimulated (or restimulated) under the indicated culture conditions for 3 days. Supernatants were harvested and analyzed by ELISA (TGF-β) or with a CBA kit (all others). One of 2 independent experiments with cells from 2 different donors is shown. (B) CD4+ Tresp cells were stimulated with allogeneic PBMCs for 5 days in the absence or presence of bead-expanded (left) or L cell–expanded CD4+CD25high T cells (right) at a 1:1 ratio and neutralizing antibodies, as indicated. P < .001 for all cocultures versus Tresp cells alone.
Immunosuppressive cytokines of CD4+CD25high T cells. CD4+CD25high T cells produce immunosuppressive cytokines, but their mode of suppression is cytokine independent. (A) First, 5 × 104 CD4+CD25high T cells, freshly sorted or expanded either on CD32+ L cells or with anti-CD3/anti-CD28–coated beads (TCE) were stimulated (or restimulated) under the indicated culture conditions for 3 days. Supernatants were harvested and analyzed by ELISA (TGF-β) or with a CBA kit (all others). One of 2 independent experiments with cells from 2 different donors is shown. (B) CD4+ Tresp cells were stimulated with allogeneic PBMCs for 5 days in the absence or presence of bead-expanded (left) or L cell–expanded CD4+CD25high T cells (right) at a 1:1 ratio and neutralizing antibodies, as indicated. P < .001 for all cocultures versus Tresp cells alone.
Since it is well established that in vitro suppression of responder T cells by freshly isolated CD4+CD25+/high T cells is independent from secreted cytokines, we next examined whether the same was true for CD4+CD25high T cells expanded either on L cells or with antibodycoated beads. To this end, neutralizing antibodies to IL-4, IL-10, and TGF-β were added to MLR assays. None of the antibodies abrogated the suppressive activity of expanded CD4+CD25high T cells, nor did the combined blockade of all 3 cytokines (Figure 6B). Thus, in vitro–expanded CD4+CD25high T cells seem to mediate suppression by the same, yet unidentified, cytokine-independent mechanism as freshly isolated CD4+CD25high T cells.
Discussion
Thus far, the anergic state of human as well as murine CD4+CD25+ Treg cells hindered their efficient long-term propagation and large-scale expansion in vitro. Yet, several animal studies have demonstrated that CD4+CD25+ Treg cells can proliferate and expand in vivo: for example, in lymphopenic hosts,33 after antigen (Ag)–specific stimulation,34,35 and even under steady-state conditions in unmanipulated animals.36 Decreased numbers or complete absence of CD4+CD25+ Treg cells in various knockout (KO) mice revealed the relevance of IL-2 and CD28/B7 costimulation for their thymic generation4,37-39 as well as for their peripheral function and expansion.30,40-42 While stimulation with a superagonistic CD28-specific monoclonal antibody was shown to be sufficient for rat CD4+CD25+ T-cell expansion in vitro and in vivo,31 combined stimulation via TCR, CD28, and IL-2R was required to transiently brake the anergic state of human and murine CD4+CD25+/high Treg cells.1,21,29,43 However, these strategies applying soluble or plate-bound antibody stimulation did not result in sustained Treg-cell proliferation, and even the most successful protocols reported so far involving allogeneic stimulation resulted only in short-term proliferation and/or marginal expansion of human CD4+CD25+/high Treg cells.23,28 In light of these results, we examined whether highly purified human CD4+CD25high Treg cells could be propagated long-term and on a large scale in vitro through potent costimulation provided by 2 types of artificial antigen-presenting cells. To avoid contamination with recently activated CD4+CD25int T cells, isolation of CD4+CD25high Treg cells was carried out under stringent sorting conditions, with selection of only those CD4+ cells that exceeded the CD25 expression level of CD4-CD25+ cells (Figure 1) and that were slightly, but detectably, smaller than recently activated CD4+CD25int T cells and discretely lower in CD4 expression. As described previously for murine as well as human CD4+CD25+ Treg cells,11,21,23,44 these CD4+CD25high T cells constitutively expressed intracellular CTLA-4, were hyporesponsive to CD3-mediated or allogeneic stimulation, and dose-dependently suppressed cocultured CD4+ responder T cells, thereby confirming earlier reports by Baecher-Allen et al.25 Yet CD4+CD25high Treg cells proliferated and expanded when cultured on L cells presenting anti-CD3 and anti-CD28 antibodies via human FcγRII for efficient TCR-synapse formation.32,45 Addition of high-dose IL-2 further increased their proliferation and led to an average 13 000-fold expansion within 3 to 4 weeks, which is several logs higher than any other Treg-cell expansion rate reported thus far. The use of anti-CD3/anti-CD28 coated beads and high-dose IL-2 also promoted profound and reproducible expansion, demonstrating that repeated stimulation via TCR and CD28 together with IL-2 is necessary and sufficient for the long-term propagation of human CD4+CD25high Treg cells in vitro. Since these beads are approved for clinical use, the ex vivo–expansion of human CD4+CD25high Treg cells for clinical application now seems feasible.
As reported earlier,46 unmanipulated CD4+CD25high T cells displayed a broad TCR Vβ-usage similar to that of CD4+CD25-T cells. This TCR Vβ-repertoire remained virtually unchanged after in vitro culture, thereby documenting the polyclonal expansion of CD4+CD25high Treg cells. In vitro expanded CD4+CD25high T cells maintained phenotypic markers characteristic for primary CD4+CD25high Treg cells, including uniformly high levels of CD25 and CTLA-4 as well as GITR expression. Most importantly, however, expanded CD4+CD25high T cells could regain their anergic state, and their suppressive activity exceeded even that of primary CD4+CD25high Treg cells from the same donor. These findings are consistent with previous reports demonstrating augmented suppressive capacity of short-term–stimulated CD4+CD25+ Treg cells29,30 and support the observation that the proliferation and suppressive function of CD4+CD25+/high T cells are not mutually exclusive.35
In model systems of autoimmunity, antigen-specific CD4+CD25+ Treg cells are found predominantly in draining LNs of affected organs,34 where their local proliferation is driven by Ag-presenting DCs expressing the costimulatory molecules CD80 and CD86.30 Suppression of effector T cells by CD4+CD25+ Treg cells therefore seems to require their migration to secondary lymphoid organs where all 3 cell populations interact in close proximity. Expression of CD62L and CCR7 crucially determines the LN homing capacity of cells, including CD4+CD25+ Treg cells.47 Szanya et al48 showed, that only CD62L+CD4+CD25+ Treg cells, which also expressed higher levels of CCR7 than the CD62L- subpopulation, migrated to pancreatic LNs and delayed diabetes onset in an adoptive transfer setting. Similarly, we could show that only CD62L+CD4+CD25+ donor Treg cells provided protection from lethal GVHD after allogeneic bone marrow transplantation (BMT) although both CD62L+ and CD62L- Treg cells were equally suppressive in vitro.49 Reisolation of donor T cells from transplant recipients confirmed the impaired ability of CD62L-CD4+CD25+ Treg cells to enter mesenteric lymph nodes. These findings suggest that lymphatic organs are the crucial sites for protection from GVHD by donor CD4+CD25+ Treg cells and that host antigen-presenting cells not only are responsible for the priming of alloaggressive T cells,50,51 but also provide the strong costimulation required for the activation and in vivo expansion of alloantigen-specific donor Treg cells.30,34 Since the suppressive activity of CD4+CD25high Treg cells depends crucially on their own activation, we examined whether in vitro expanded CD4+CD25high T cells maintained lymph node homing receptors. Our data clearly demonstrate sustained expression of CD62L and CCR7 on in vitro expanded human CD4+CD25high Treg cells, suggesting that they maintain the ability to enter lymphatic tissues to exert their suppressive function in a site-specific manner. The combined expression of CD62L, CCR7, and CD27 on Ag-experienced CD45RO+ T cells has recently been described as being characteristic for central memory T cells that continuously screen lymphoid organs for recall antigens.52,53 Their comparable phenotype suggests a similar capacity of activated CD4+CD25high Treg cells.
Trenado et al19 recently demonstrated improved protection from lethal GVHD by in vitro expanded CD62L+CD4+CD25+ Treg cells primed to host alloantigens as compared with Treg cells primed by third-party stimulators in murine models. Those experiments confirmed that in vitro expanded Treg cells survive after reinfusion and that they still depend on TCR stimulation to mediate suppression. Taking these observations into account, we purposely aimed at expanding human CD4+CD25high T cells polyclonally rather than using allogeneic stimulator cells for future clinical trials in BMT patients. This decision was based on our previous finding that in vitro priming is not required for GVHD inhibition, since activation of alloantigen-specific Treg cells occurs efficiently in vivo.11,15 The potential advantage of this in vivo selection is the maintenance of TCR specificities reactive to nonhematopoietic minor alloantigens that are not necessarily presented by recipient stimulator cells isolated from peripheral blood. In contrast to polyclonally expanded Treg cells, in vitro expanded Treg cells primed by host PBMCs are expected to recognize predominantly hematopoietic alloantigens. However, suppression of the graft-versus-hematopoiesis effect of donor T cells is not intended in allogeneic BMT and might even result in graft rejection or higher relapse rates in patients receiving transplants for hematologic malignancies. Owing to the lack of protocols for the efficient polyclonal expansion of CD4+CD25+ Treg cells, a systematic comparison of differentially expanded CD4+CD25+ Treg cells in GVHD models could not be performed thus far, but is now under investigation.
In summary, we have shown that highly purified CD4+CD25high T cells are a polyclonal Treg-cell population that rapidly expands in vitro upon strong costimulation. Expanded CD4+CD25high Treg cells retain their phenotypic characteristics, maintain expression of LN homing receptors, and show even increased suppressive activity when compared with freshly isolated cells. These findings will facilitate the elucidation of their mode of action and allow the detailed examination of their Ag specificity. Importantly, the prospect of expanding CD4+CD25high Treg cells with clinical grade reagents will accelerate their exploitation for the treatment of autoimmune diseases as well as pathogenic alloresponses after solid organ or stem cell transplantation.
Prepublished online as Blood First Edition Paper, April 15, 2004; DOI 10.1182/blood-2004-01-0086.
Supported by grants from the Dr Mildred Scheel Stiftung, the Wilhelm Sander Stiftung, and the Regensburg medical research program (ReForM).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank M. Hoffmann for excellent technical assistance with FACS sorting.






This feature is available to Subscribers Only
Sign In or Create an Account Close Modal