Abstract
Chronic graft-versus-host disease (cGVHD) is an increasingly common cause of morbidity and mortality in allogeneic stem cell transplantation (alloSCT). Relative to acute GVHD (aGVHD), much less is understood about cGVHD. Using the B10.D2 → BALB/c murine cGVHD model, which shares critical pathologic features with human cGVHD, we find that radiation-resistant host T cells regulate cGVHD. We initially observed that recipients lacking all lymphocytes developed accelerated and more severe cGVHD. Using genetically deficient recipients, we determined that αβ+CD4+ T cells were required to regulate cGVHD. Increased cGVHD severity was not due to the absence of T cells per se. Rather, the potency of regulation was proportional to host T-cell receptor (TCR) diversity. Only CD4+CD25+, and not CD4+CD25-, host T cells ameliorated cGVHD when added back, indicating that host T cells acted not via host-versus-graft activity or by reducing homeostatic proliferation but by an undefined regulatory mechanism. Thus, preparative regimens that spare host CD4+CD25+ T cells may reduce cGVHD. Donor CD4+CD25+ T cells also reduced cGVHD. Depletion of CD4+CD25+ cells from the inoculum exacerbated disease, whereas transplantation of additional CD4+CD25+ cells protected against severe cGVHD. Additional CD4+CD25+ cells also promoted healing of established lesions, suggesting that their effects persist during the evolution of cGVHD.
Introduction
Chronic graft-versus-host disease (cGVHD) is an increasingly common complication of allogeneic stem cell transplantation (alloSCT). Its incidence, as high as 80% in some series, is thought to be on the rise at least in part due to the use of peripheral blood as a stem cell source, nonmyeloablative conditioning, withdrawal of immunosuppression to induce antitumor activity, better supportive care allowing longer survival, and the number of patients receiving donor leukocyte infusions.1-7 Even with a wide range of therapeutic options including agents that target tumor necrosis factor-α (TNF-α) and the interleukin-2 (IL-2) receptor, cGVHD and the infectious complications of its management are major causes of late mortality for alloSCT recipients.8 Acute GVHD (aGVHD) and cGVHD are traditionally diagnosed primarily by time of onset, with cGVHD occurring after day 100 after transplantation.9 However, cGVHD has distinct clinicopathologic features and is often diagnosed based on these features regardless of time of onset.10 aGVHD typically presents with inflammatory skin, gastrointestinal, and/or hepatic disease, while cGVHD is characterized by cutaneous fibrosis, involvement of exocrine glands, myositis, and hepatic disease.9,10 Often cGVHD occurs in patients who have had prior aGVHD, although de novo cGVHD without aGVHD is not uncommon and the relationship between the two is unclear. In particular, de novo cGVHD occurs with some frequency after delayed leukocyte infusion given for the treatment of relapsed leukemia. Importantly, both de novo cGVHD and that which emerges from prior aGVHD share clinicopathologic features.
Donor T cells cause cGVHD, but much about the pathobiology of cGVHD is unknown. Most animal research on GVHD has been performed in murine models of aGVHD, with donor and recipient strains partially or fully mismatched at the major histocompatibility complex (MHC) locus. Broadly speaking, disease in these models is characterized by hunched posture, wasting, and death with inflammatory skin, gastrointestinal, and hepatic pathology. Experiments in such aGVHD models have yielded important insights into the mechanisms of initial activation of T cells, including required antigen-presenting cells (APCs)11 and costimulatory molecules,12-14 the mechanism of damage to host tissues by donor T cells,15-17 the roles of cytokines,18-24 and the influence of donor regulatory T cells.25-31 While aGVHD and cGVHD are similar in some respects, it seems likely that the two diseases have different initiation requirements and pathogenic mechanisms, and it is not obvious whether findings in aGVHD models also apply to the cGVHD syndrome and vice versa.32
Compared with aGVHD, cGVHD has been less well studied. This may be a consequence of the limited number of murine models that resemble human cGVHD. Several parent → F1 transplantation models, while described as cGVHD models, result in a disease more similar to systemic lupus erythematosus than cGVHD.33-36 However, the B10.D2 (H-2d) → BALB/c (H-2d) MHC-compatible, multiple minor histocompatibility antigen (miHA)–incompatible model of cGVHD37-41 does share critical characteristics with human cGVHD. Its dominant features include skin fibrosis (due to increased collagen deposition) as well as lichenoid subepithelial infiltrates, follicular drop-out, loss of subdermal fat, and dermal mononuclear infiltrates.37 Hepatic disease is characterized by intrahepatic and extrahepatic bile duct mononuclear infiltration followed by fibrous thickening and sclerosis of the bile duct wall.42-44 Pulmonary fibrosis has been observed as well.45 Moreover, we have commonly noted inflammation and destruction of salivary and lacrimal glands (B.E.A. and M.J.S., unpublished observations, March 2001) although we do not routinely measure this outcome. Furthermore, the onset of clinical signs of cGVHD in this model, at around day 21, is later than in many models of murine aGVHD. Several groups have investigated the mechanisms of pathogenesis in this model, including the initiating T-cell subsets,41,46 the role of mast cells,38,47 involved adhesion molecules,46,48 fibrogenic cytokines,45 and chemokines.49 Although this model is best viewed as a de novo model of cGVHD, its value lies in the strong resemblance to the clinicopathologic features found in both primary and secondary cGVHD in humans.
In general, most GVHD research—whether using acute or chronic models—has focused on the properties of donor T cells, and less attention has been given to host factors that might influence the incidence and character of GVHD. However, several studies have shown that recipient cells can indeed affect GVHD. Our previous studies have shown a requirement for host APCs to initiate disease in an aGVHD model.50 Schultz and coworkers suggested a role for host B cells using an aGVHD model.51 Studies by Blazar and colleagues provided evidence that host T cells could affect aGVHD caused by donor leukocyte infusions.52 With further understanding of their roles, host factors could potentially be modified for therapeutic benefit.
Here we have used the B10.D2 → BALB/c model of cGVHD to address the role of host lymphocytes in cGVHD. We first observed that lymphocyte-deficient (RAG2-/-)53 recipients developed cGVHD that was more rapid in onset and more severe than in wild-type (WT) recipients. These data indicated that, even after radiation, residual host lymphocytes could modulate the severity of cGVHD. Because this observation could have clinical implications, we went on to further investigate the identity of the involved recipient lymphocytes.
To do this, we compared cGVHD in recipient BALB/c strains genetically lacking specific lymphocyte subsets. Taken together, these data indicated a role for host CD4+ T cells and ruled out a number of other explanations. To define a CD4+ T-cell type that could mediate protection, we added back specific T-cell subsets to RAG2-/- recipients in an attempt to reconstitute the missing lymphocyte component. These studies demonstrated that recipient-type CD4+CD25+ but not CD4+CD25- T cells can regulate cGVHD. Finally, we showed that donor CD4+CD25+ T cells also have the capacity to affect cGVHD. These data suggest an unexpected role for recipient T cells that survive irradiation and, in addition, extend our knowledge of donor CD4+CD25+ T cells to a model of cGVHD. Our results suggest how the design of preparative regimens might influence the likelihood of cGVHD as well as provide therapeutic strategies to control cGVHD.
Materials and methods
Mice
Five- to 8-week-old male B10.D2.oSN or B10.D2.nSN (H-2d) donor mice were purchased from the Jackson Laboratory (Bar Harbor, ME). BALB/c (H-2d) recipient mice were purchased from Taconic Farms (Germantown, NY) or the National Cancer Institute (Frederick, MD). Genetically modified recipients, all on a BALB/c background, were obtained as follows: RAG2-/- mice were purchased from Taconic or the National Cancer Institute (Bethesda, MD). Jh-/- B cell–deficient mice on the BALB/c background were bred in our laboratory54 from the original gene-targeted strain.55 T-cell receptor–α-/- (TCRα-/-) and DO11.10 (RAG2+/+) mice were a kind gift from Dr Kim Bottomly and bred at Yale University. DO11.10 (RAG2-/-) mice were made by crossing DO11.10 to RAG2-/- mice. TCRδ-/- mice56 were a kind gift from Dr Pereira and bred at Yale University. All recipients were 8 to 12 weeks old at the time of transplantation.
Bone marrow transplantation (BMT)
Recipient mice received 850 cGy (137Cs source) total body irradiation (single dose) or two 380- or 450-cGy fractions separated by 3 hours. Three to 5 hours following the last irradiation dose, all recipients received 8 × 106 T-cell–depleted bone marrow (BM) suspended in injection buffer (1 × phosphate-buffered saline, 10 mM HEPES [N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid], 2.5% acid-citrate-dextrose anticoagulant, 0.5% penicillin-streptomycin) with or without donor T cells via tail vein injection on day 0. Total spleen cell dose was 6 × 106 or 107 cells per recipient, as indicated in the figure legends. The purified CD4+ T-cell dose was 1.5 × 106 or 2 × 106 cells per recipient. Animals were given water supplemented with trimethoprim/sulfamethoxazole for 2 weeks following bone marrow transplantation (BMT).
Cell separations
BM cells were collected by flushing femurs and tibias from donor mice into magnetic-activated cell separation (MACS) buffer (1 × phosphate-buffered saline, 5 mM EDTA [ethylenediaminetetraacetic acid], 3% calf serum). After red blood cell lysis, cells were incubated with biotinylated anti-Thy1.2 (30H12) monoclonal antibody (moAb) for 20 minutes on ice, washed once, and then incubated with streptavidin-conjugated microbeads (SA-beads) (Miltenyi Biotec, Auburn, CA) for 20 minutes at 4°C. Cells were depleted of Thy1.2-positive cells using an AutoMACS (Miltenyi Biotec). Remaining Thy1.2-positive cells were less than 0.5% of BM cells. Cells were resuspended in injection buffer prior to transplantation.
Spleen cells were collected from donor mice by crushing through 70-μm screens in MACS buffer. After red blood cell lysis, spleen cells were resuspended in injection buffer prior to transplantation or underwent further cell purifications. CD4+ T cells were enriched from total spleen cells using BioMag (Qiagen, Hilden, Germany) cell separation. After red blood cell lysis, total spleen cells were incubated with the following moAb supernatants (all laboratory prepared): anti-CD8α (TIB105), anti-B220 (RA3-6B2), anti–Mac-1 (M1/70), and anti-FcR (24G.2) for 30 minutes on ice followed by 2 washes in MACS buffer. Cells were incubated with prepared BioMag goat antirat magnetic beads for 30 minutes on ice in a T75 or T125 flask, which was then placed next to a strong magnet. Unbound cells were collected and were typically 70% to 80% CD4+ with less than 3% contaminating CD8+, B220+, CD11b+, or FcR+ cells as determined by flow cytometry.
Separation of CD25+ and CD25- CD4+ T cells was achieved by first incubating enriched CD4+ cells with biotinylated anti-CD25 (7D4; BD Pharmingen, San Diego, CA) for 30 minutes on ice. Cells were washed once in MACS buffer and then incubated with SA-beads for 25 minutes at 4°C. Cells were separated into CD25+ and CD25- fractions using an AutoMACS. Cell purity was checked by flow cytometry, with less than 3% contaminating CD25- or CD25+ cells, respectively. Cells were resuspended in injection buffer prior to injection.
The percentage of CD4+CD25+ cells in BALB/c spleens was determined by staining total spleen cell suspensions with CD4–fluorescein isothiocyanate (CD4-FITC) (GK1.5, laboratory prepared) and biotinylated anti-CD25 (7D4; BD Pharmingen) followed by secondary staining with streptavidin-conjugated Alexa647 (Molecular Probes, Eugene, OR). Cells were analyzed using a FACSCalibur (BD Immunocytometry Systems, San Jose, CA).
Evaluation of cGVHD
Following BMT, animals were weighed every 3 days and scored for skin manifestations of GVHD beginning on day 18. The following scoring system was used: healthy appearance equals 0; skin lesions with alopecia less than 1 cm2 in area, 1; skin lesions with alopecia 1 to 2 cm2 in area, 2; skin lesions with alopecia more than 2 cm2 in area, 3. Additionally, animals were assigned 0.3 point each for skin disease (lesions or scaling) on the ears, tail, and paws. Minimum score was 0, maximum score 3.9. Incidence and clinical score curves represent all mice that achieved a score of 0.6 or higher. Final scores for humanely killed animals were kept in the data set for the remaining time points of the experiment.
Tissue histopathology
Shaved skin from the interscapular region (approximately 2 cm2) was fixed in 10% formalin, embedded in paraffin, sectioned, slide mounted, and stained with hematoxylin and eosin. Slides were scored by a dermatopathologist (J.M.; blinded to experimental groups) on the basis of dermal fibrosis, fat loss, inflammation, epidermal interface changes, and follicular drop-out (0 to 2 for each category). Minimum score was 0, maximum score 10.
Statistics
The following nonparametric analyses were used: log-rank Mantel-Cox for incidence curves; Mann-Whitney for clinical score data and skin pathology data. χ2 analysis was used to determine the significance of differences in disease progression in Figure 5.
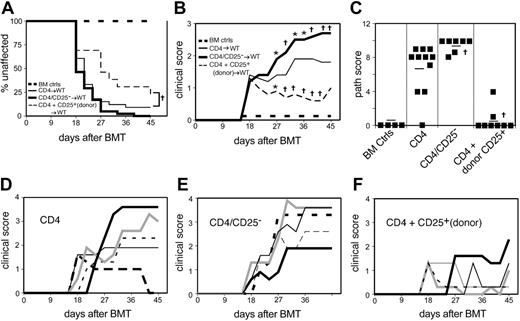
Donor CD4+CD25+ cells affect cGVHD. Combined data from 3 experiments. On day 0, WT recipient mice were lethally irradiated and reconstituted with 8 × 106 BM cells alone (n = 15), BM plus 1.5 × 106 to 2 × 106 (unfractionated) CD4+ T cells (CD4) (n = 33), BM plus 1.5 × 106 to 2 × 106 CD25-depleted CD4+ T cells (CD4/CD25-) (n = 41), or BM plus 1.5 × 106 to 2 × 106 (unfractionated) CD4+ cells plus 3 × 105 CD4+CD25+ T cells (CD4 + CD25+) (n = 13). (A) Incidence of cGVHD. †P < .01 for CD4 + CD25+ versus CD4. (B) *P < .05, †P < .01 for CD4/CD25- or CD4 + CD25+ recipients compared with CD4. BM control mice did not get cGVHD and are represented on the graph as scoring “0.” (C) Pathology score for representative mice. Mean score is indicated by a horizontal bar. †P < .01, CD4/CD25- or CD4 + CD25+ as compared with CD4. Pathology samples were taken on day 33 or 45. (D-F) Clinical scores for individual mice; 5 representative mice per group (D) CD4, (E) CD4/CD25-, and (F) CD4 + CD25+. Each line represents an individual mouse, and lines are given at varying patterns for clarity.
Donor CD4+CD25+ cells affect cGVHD. Combined data from 3 experiments. On day 0, WT recipient mice were lethally irradiated and reconstituted with 8 × 106 BM cells alone (n = 15), BM plus 1.5 × 106 to 2 × 106 (unfractionated) CD4+ T cells (CD4) (n = 33), BM plus 1.5 × 106 to 2 × 106 CD25-depleted CD4+ T cells (CD4/CD25-) (n = 41), or BM plus 1.5 × 106 to 2 × 106 (unfractionated) CD4+ cells plus 3 × 105 CD4+CD25+ T cells (CD4 + CD25+) (n = 13). (A) Incidence of cGVHD. †P < .01 for CD4 + CD25+ versus CD4. (B) *P < .05, †P < .01 for CD4/CD25- or CD4 + CD25+ recipients compared with CD4. BM control mice did not get cGVHD and are represented on the graph as scoring “0.” (C) Pathology score for representative mice. Mean score is indicated by a horizontal bar. †P < .01, CD4/CD25- or CD4 + CD25+ as compared with CD4. Pathology samples were taken on day 33 or 45. (D-F) Clinical scores for individual mice; 5 representative mice per group (D) CD4, (E) CD4/CD25-, and (F) CD4 + CD25+. Each line represents an individual mouse, and lines are given at varying patterns for clarity.
Results
Lymphocyte-deficient RAG2-/- mice develop more severe cGVHD than WT recipients
To determine whether recipient lymphocytes play a role in modulating cGVHD, RAG2-/- and WT mice were irradiated and reconstituted with T-cell–depleted B10.D2 BM with or without 107 B10.D2 spleen cells. RAG2-/- recipients of spleen cells developed cGVHD that was more rapid in onset and of higher penetrance than cGVHD in WT recipients (Figure 1A; P < .01 RAG2-/- versus WT). Disease in affected RAG2-/- recipients was also more extensive than that in affected WT mice (Figure 1B; P < .05 for day 27; P < .01 for all time points thereafter). Blinded pathologic scoring of skin disease confirmed the clinical result. Skin from RAG2-/- spleen cell recipients had an average pathology score of 7.7 compared with 3.7 for WT spleen cell recipients (Figure 1C; P < .05). However, the basic features of the pathologic disease— fibrosis, interface dermatitis, and fat atrophy—were similar. Thus, the absence of recipient lymphocytes exacerbates cGVHD in this model. We also performed experiments using B cell–deficient recipients using 107 unseparated donor spleen cells in the standard transplantation regimen. cGVHD in B cell–deficient recipients was comparable in penetrance and clinical and pathologic scores to WT recipients, indicating that B cells do not significantly influence cGVHD in this model (data not shown). Therefore, it was the absence of T cells in RAG2-/- recipients, not B cells, that led to more severe cGVHD.
Lymphocyte-deficient (RAG2-/-) recipients have accelerated cGVHD with greater penetrance and severity. Combined data from 3 experiments. On day 0, recipient mice were lethally irradiated and reconstituted with 8 × 106 B10.D2 BM cells alone (n = 19, all recipient types) or BM plus B10.D2 107 spleen cells: WT (n = 32), RAG2-/- (n = 28). In a separate experiment, RAG2-/- recipient mice were lethally irradiated and reconstituted with 8 × 106 syngeneic (BALB/c) BM plus 107 syngeneic (BALB/c) spleen cells (n = 9). (A) Incidence of cGVHD. †P < .01 for RAG2-/- recipients compared with WT recipients. (B) Average clinical disease score for mice affected with cGVHD (unaffected mice are excluded). *P < .05, †P < .01 for RAG2-/- recipients compared with WT recipients. BM control mice and RAG2-/- recipients of syngeneic cells did not get cGVHD and are represented on the graph as scoring “0.” (C) Pathology score for representative mice. Mean score is indicated by a horizontal bar. *P < .05 for RAG2-/- recipients compared with WT recipients. Pathology samples were taken on day 24, 33, or 50.
Lymphocyte-deficient (RAG2-/-) recipients have accelerated cGVHD with greater penetrance and severity. Combined data from 3 experiments. On day 0, recipient mice were lethally irradiated and reconstituted with 8 × 106 B10.D2 BM cells alone (n = 19, all recipient types) or BM plus B10.D2 107 spleen cells: WT (n = 32), RAG2-/- (n = 28). In a separate experiment, RAG2-/- recipient mice were lethally irradiated and reconstituted with 8 × 106 syngeneic (BALB/c) BM plus 107 syngeneic (BALB/c) spleen cells (n = 9). (A) Incidence of cGVHD. †P < .01 for RAG2-/- recipients compared with WT recipients. (B) Average clinical disease score for mice affected with cGVHD (unaffected mice are excluded). *P < .05, †P < .01 for RAG2-/- recipients compared with WT recipients. BM control mice and RAG2-/- recipients of syngeneic cells did not get cGVHD and are represented on the graph as scoring “0.” (C) Pathology score for representative mice. Mean score is indicated by a horizontal bar. *P < .05 for RAG2-/- recipients compared with WT recipients. Pathology samples were taken on day 24, 33, or 50.
Reconstitution of lymphocyte-deficient mice with syngeneic CD4+ cells was reported to cause an autoimmune syndrome, although such recipients developed colitis without skin disease.57 Nonetheless, we wanted to be sure that disease in RAG2-/- recipients was due to recognition of alloantigens. We therefore performed a syngeneic BALB/c→RAG2-/- experiment using the identical transplantation protocol. RAG2-/- recipients of syngeneic BM and splenocytes showed no evidence of cGVHD by both clinical observation and pathologic scoring (Figure 1). Thus, the more severe cGVHD we observed in RAG2-/- recipients of allogeneic spleen cells was due to donor T cells recognizing host miHAs.
Recipient αβ T cells control onset and penetrance of cGVHD
To distinguish which recipient T-cell lineage controlled cGVHD, we used recipients deficient in either αβ (TCRα-/-)58 or γδ (TCRδ-/-)59 T cells. In 2 separate experiments, the lack of αβ T cells led to a more rapid onset of cGVHD as compared with WT recipients (Figure 2A; P < .01), although the clinical appearance of affected animals was similar to WT recipients (Figure 2B). In contrast, γδ T-cell–deficient recipients had very similar penetrance and clinical disease compared with that of WT recipients in 3 separate experiments (Figure 2C-D). These experiments showed that the “missing lymphocyte” in RAG2-/- recipients was an αβ and not a γδ T cell. The difference in clinical severity between RAG2-/- and TCRα-/- could indicate that in the absence of αβ T cells, γδ T cells can regulate disease. Indeed, γδ T cells are known to regulate skin disease in a number of models.60-64
αβ T-cell–deficient recipients but not γδ T-cell–deficient recipients have an increased incidence of cGVHD. (A) Incidence of cGVHD in αβ T-cell–deficient recipients. Combined data from 2 experiments. On day 0, recipient mice were lethally irradiated and reconstituted with 8 × 106 BM cells alone (n = 10, both recipient types) or BM plus 107 spleen cells: WT (n = 29), TCRα-/- (n = 12). †P < .01 for TCRα-/- recipients as compared with WT recipients. (B) Clinical disease in αβ T-cell–deficient recipients. Average clinical score for mice affected with cGVHD (unaffected mice are excluded). BM control mice did not get cGVHD and are represented on the graph as scoring “0.” (C) Incidence of cGVHD in γδ T-cell–deficient recipients. Combined data from 3 experiments. On day 0, recipient mice were lethally irradiated and reconstituted with 8 × 106 BM cells alone (n = 28, both recipient types) or BM plus 107 spleen cells: WT (n = 41), TCRδ-/- (n = 38). (D) Clinical disease in γδ T-cell–deficient recipients. Average clinical score for mice affected with cGVHD (unaffected mice are excluded). BM control mice did not get cGVHD and are represented on the graph as scoring “0.”
αβ T-cell–deficient recipients but not γδ T-cell–deficient recipients have an increased incidence of cGVHD. (A) Incidence of cGVHD in αβ T-cell–deficient recipients. Combined data from 2 experiments. On day 0, recipient mice were lethally irradiated and reconstituted with 8 × 106 BM cells alone (n = 10, both recipient types) or BM plus 107 spleen cells: WT (n = 29), TCRα-/- (n = 12). †P < .01 for TCRα-/- recipients as compared with WT recipients. (B) Clinical disease in αβ T-cell–deficient recipients. Average clinical score for mice affected with cGVHD (unaffected mice are excluded). BM control mice did not get cGVHD and are represented on the graph as scoring “0.” (C) Incidence of cGVHD in γδ T-cell–deficient recipients. Combined data from 3 experiments. On day 0, recipient mice were lethally irradiated and reconstituted with 8 × 106 BM cells alone (n = 28, both recipient types) or BM plus 107 spleen cells: WT (n = 41), TCRδ-/- (n = 38). (D) Clinical disease in γδ T-cell–deficient recipients. Average clinical score for mice affected with cGVHD (unaffected mice are excluded). BM control mice did not get cGVHD and are represented on the graph as scoring “0.”
We compared WT recipients with recipients deficient in CD8+ T cells (CD8α-/-65 ; at least 11 mice per group) to assess whether the regulating recipient αβ T cell was CD4+ or CD8+. CD8α-/- recipients did not have accelerated or more severe cGVHD (data not shown), indicating that deficiency of CD8+ T cells could not account for the RAG2-/- phenotype and that CD4+ T cells were primarily responsible for the effect on cGVHD. We therefore focused our further research on recipient CD4+ T cells.
Increasing recipient T-cell repertoire ameliorates cGVHD
To begin to investigate the mechanism by which host αβ CD4+ T cells inhibit cGVHD, we asked if the presence of recipient CD4+ T cells per se could ameliorate cGVHD and if the specificity of those T cells was important. To accomplish this we studied cGVHD in recipients with progressively increasing CD4+ TCR repertoire diversity. The DO11.10 TCR transgene locus, when crossed to RAG2-/-, expresses a single αβ TCR that recognizes the ovalbumin 323-339 peptide presented by IAd and selects exclusively CD4+ T cells.66 DO11.10 mice on a RAG2+/+ background have a somewhat more complex repertoire due to limited rearrangement of the endogenous α chain, which pairs with the transgenic TCR β chain. If penetrance and severity of cGVHD were to correlate with the diversity of the CD4+ T-cell repertoire, we would predict that DO11.10 (RAG2-/-) mice would have cGVHD similar to RAG2-/- mice and that DO11.10 (RAG2+/+) recipients would have penetrance and severity of cGVHD between that seen in WT and RAG2-/- or TCRα-/- mice. Indeed, this was the case. Recipient mice that had only CD4+ T cells bearing a single TCR (DO11.10 RAG2-/-) had incidence and severity of cGVHD similar to RAG2-/- recipients (Figure 3), ruling out nonspecific effects of T-cell absence as explaining the RAG2-/- recipient cGVHD phenotype. DO11.10 (RAG2+/+) recipients had an intermediate rate of onset and penetrance of cGVHD as compared with RAG2-/- (Figure 3A; P < .05) or WT mice (Figure 3A; P < .05), suggesting that increasing the TCR repertoire via endogenous α chain rearrangement was sufficient to decrease the severity of cGVHD.
Increasing recipient TCR clonotypic variety reduces penetrance and severity of cGVHD. Combined data from 2 experiments. On day 0, recipient mice were lethally irradiated and reconstituted with 8 × 106 BM cells alone (n = 29, all recipient types) or BM plus 107 spleen cells: WT (n = 29), DO11.10 (RAG2+/+) (n = 12), DO11.10 (RAG2-/-) (n = 18), RAG2-/- (n = 16). (A) Incidence of cGVHD. *P < .05 for DO11.10 (RAG2+/+) versus WT and versus RAG2-/-; P = .094 for DO11.10 (RAG2+/+) versus DO11.10 (RAG2-/-). (B) Pathology score for representative mice. Mean score is indicated by a horizontal bar. *P < .05 for DO11.10 (RAG2+/+) versus DO11.10 (RAG2-/-) and versus RAG2-/-. Pathology samples were taken on day 24, 28, or 50.
Increasing recipient TCR clonotypic variety reduces penetrance and severity of cGVHD. Combined data from 2 experiments. On day 0, recipient mice were lethally irradiated and reconstituted with 8 × 106 BM cells alone (n = 29, all recipient types) or BM plus 107 spleen cells: WT (n = 29), DO11.10 (RAG2+/+) (n = 12), DO11.10 (RAG2-/-) (n = 18), RAG2-/- (n = 16). (A) Incidence of cGVHD. *P < .05 for DO11.10 (RAG2+/+) versus WT and versus RAG2-/-; P = .094 for DO11.10 (RAG2+/+) versus DO11.10 (RAG2-/-). (B) Pathology score for representative mice. Mean score is indicated by a horizontal bar. *P < .05 for DO11.10 (RAG2+/+) versus DO11.10 (RAG2-/-) and versus RAG2-/-. Pathology samples were taken on day 24, 28, or 50.
Reconstitution of CD4+CD25+ cells in RAG2-/- recipients reduces cGVHD
At least 3 possible mechanisms can explain how the increased TCR repertoire in WT and DO11.10 (RAG2+/+) recipients reduces cGVHD: increased host-versus-graft effects, decreased homeostatic proliferation of donor T cells, or an increase in the number of regulatory T cells. It seemed unlikely that the small number of T cells with endogenous α chains (approximately 6%-11% of CD4+ cells [B.E.A., unpublished data, May 2002]) in DO11.10 (RAG+/+) recipients would mount an effective host-versus-graft effect, although this could not be formally excluded. On the other hand, even low levels of endogenous TCR α chain rearrangement in αβ TCR transgenics can lead to decreased homeostatic proliferation of transferred cells67,68 and an increase in CD4+CD25+ T cells with regulatory capacities.69-71 Indeed, whereas CD4+CD25+ T cells are essentially absent in DO11.10 (RAG2-/-) mice, they constitute 3% to 5% of CD4+ cells in DO11.10 (RAG2+/+) as compared with 8% to 11% of CD4+ cells in WT animals (not shown). Therefore, to test a potential role of putative recipient-type regulatory cells, we reconstituted RAG2-/- recipients with syngeneic CD4+CD25+ T cells. To distinguish inhibition of homeostatic proliferation from other regulatory mechanisms, we also transferred syngeneic CD4+CD25- T cells, which are known to potently inhibit homeostatic proliferation72 but which were less likely to have had other types of regulatory T-cell activity.
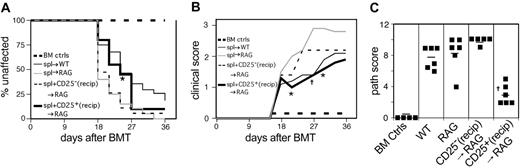
In 2 separate experiments, the transplantation of CD4+CD25+ T cells delayed the incidence and reduced the penetrance of cGVHD as compared with RAG2-/- recipients that received no syngeneic T cells (Figure 4A). In contrast, transplantation of CD4+CD25- T cells had no effect. The extent of clinical skin disease in affected RAG2-/- mice reconstituted with CD4+CD25+ T cells was also reduced as compared with that observed in RAG2-/- recipients that did not receive host T cells (Figure 4B; P < .05 days 21, 30; P < .01 day 27 after BMT). Additionally, histologic analysis revealed that RAG2-/- recipients reconstituted with host-type CD4+CD25+ T cells had much milder skin pathology (Figure 4C; P < .01 for RAG2-/- plus CD4+CD25+ versus all other experimental groups receiving T cells).
Reconstitution of RAG2-/- recipients with host-type CD4+CD25+ T cells reduces penetrance and severity of clinical cGVHD. (A) Incidence of cGVHD. Combined data from 2 experiments. On day 0, recipient mice were lethally irradiated and reconstituted with 8 × 106 BM cells alone (n = 18, both recipient types) or BM plus 6 × 106 WT spleen cells (n = 27). RAG2-/- recipients received BM + spl with either 106 freshly purified BALB/c CD4+CD25- T cells (spl + CD25-, n = 19) or 106 freshly purified BALB/c CD25+ T cells (spl + CD25+, n = 20). *P < .05 for RAG2-/- spl + CD25+ versus RAG2-/- BM + spl. (B) Average clinical disease score for mice affected with cGVHD (unaffected mice are excluded). *P < .05, †P < .01 for RAG2-/- spl + CD25+ compared with RAG2-/- BM + spl. BM control mice did not get cGVHD and are represented on the graph as scoring “0.” (C) Pathology scores for representative mice. Mean score is indicated by a horizontal bar. †P < .01 for RAG2-/- spl + CD25+ compared with RAG2-/- BM + spl, RAG2-/- spl + CD25-/-, or WT. Pathology samples were taken on day 26, 34, or 50.
Reconstitution of RAG2-/- recipients with host-type CD4+CD25+ T cells reduces penetrance and severity of clinical cGVHD. (A) Incidence of cGVHD. Combined data from 2 experiments. On day 0, recipient mice were lethally irradiated and reconstituted with 8 × 106 BM cells alone (n = 18, both recipient types) or BM plus 6 × 106 WT spleen cells (n = 27). RAG2-/- recipients received BM + spl with either 106 freshly purified BALB/c CD4+CD25- T cells (spl + CD25-, n = 19) or 106 freshly purified BALB/c CD25+ T cells (spl + CD25+, n = 20). *P < .05 for RAG2-/- spl + CD25+ versus RAG2-/- BM + spl. (B) Average clinical disease score for mice affected with cGVHD (unaffected mice are excluded). *P < .05, †P < .01 for RAG2-/- spl + CD25+ compared with RAG2-/- BM + spl. BM control mice did not get cGVHD and are represented on the graph as scoring “0.” (C) Pathology scores for representative mice. Mean score is indicated by a horizontal bar. †P < .01 for RAG2-/- spl + CD25+ compared with RAG2-/- BM + spl, RAG2-/- spl + CD25-/-, or WT. Pathology samples were taken on day 26, 34, or 50.
These experiments show that host CD4+CD25+, but not host CD4+CD25-, T cells can modulate cGVHD in RAG2-/- mice, rendering it comparable to that seen in intact WT recipients. Together with the data from knock-out recipients lacking various T-cell subsets presented above, these findings strongly suggest that the increased severity of cGVHD seen in RAG2-/- mice is due to the absence of CD4+CD25+ T cells. Furthermore, these data argue against host versus graft effects or increased homeostatic proliferation as the mechanism of cGVHD resistance. Host CD4+ T cells with antidonor specificity are unlikely to be confined to the CD4+CD25+ subset only and, in fact, better host-versus-graft effect might have been expected from CD4+CD25- T cells, yet they had no effect on modulating disease. Similarly, the reconstitution of host CD4+CD25+ or CD4+CD25- T cells should result in a comparable reduction in homeostatic proliferation of donor T cells.72 Because only the CD25+ subset blocked cGVHD, this indicates that the mechanism is unlikely to be nonspecific suppression of homeostatic proliferation.
Preferential survival of CD4+CD25+ cells after irradiation
The finding that reconstituting RAG2-/- mice with CD4+CD25+ T cells ameliorated subsequent cGVHD raised the question of whether such cells naturally survive irradiation in the host. We subjected BALB/c mice to our standard irradiation protocol and then used fluorescence-activated cell sorter (FACS) analysis to determine the percentages of CD4+CD25+ T cells in spleens at 1, 2, and 3 days after irradiation (Table 1). Initially, these cells constituted 1.7% of splenocytes. Although, as expected, numbers of splenocytes declined rapidly following irradiation, the fraction of CD4+CD25+ T cells increased to around 3% on days 1 and 2 and 6% on day 3 after treatment. In spleen alone, there were 170 000 remaining CD4+CD25+ T cells on day 1 and 50 000 on day 3. Considering that 106 such cells, when infused by tail vein, had demonstrable effects (Figure 4), and accounting for nonspecific cell losses in lung and liver and distribution of cells throughout the body following intravenous injection, the numbers of remaining cells are in the same range one might expect to achieve by cell infusion. In any case, CD4+CD25+ T cells do preferentially survive for a number of days after irradiation and would be expected to be present during at least the initial alloreactive activation phase of GVHD induction.
The survival of splenic CD4+CD25+ cells following lethal irradiation
Day after irradiation . | Average total spleen cell no., × 106 . | Average % CD4+CD25+ . |
|---|---|---|
| Nonirradiated | 46 | 1.7 |
| Day 1 | 5.2 | 3.3 |
| Day 2 | 2.8 | 2.6 |
| Day 3 | 0.8 | 6.1 |
Day after irradiation . | Average total spleen cell no., × 106 . | Average % CD4+CD25+ . |
|---|---|---|
| Nonirradiated | 46 | 1.7 |
| Day 1 | 5.2 | 3.3 |
| Day 2 | 2.8 | 2.6 |
| Day 3 | 0.8 | 6.1 |
The average total spleen cell number and percentage of splenic CD4+CD25+ cells were calculated for nonirradiated BALB/c mice or those that had received 850 cGy total body irradiation at day —1, —2, or —3. Data are from 5 mice in each irradiated group and 3 nonirradiated mice.
Donor CD4+CD25+ T cells also inhibit cGVHD
Although a definitive role for recipient-type CD4+CD25+ T cells in modulating GVHD has not been documented previously, several groups have demonstrated a role for CD4+CD25+ donor-type T cells in murine models of acute GVHD.25-31 We were therefore interested in whether donor CD4+CD25+ T cells could also regulate chronic GVHD in our model or whether this is a unique property of host T cells. To examine this, WT recipients underwent transplantation with purified donor total CD4+ T cells, CD4+ T cells depleted of CD4+CD25+ cells, or total CD4+ T cells plus 3 × 105 additional donor-type CD4+CD25+ T cells. In 3 separate experiments, depletion of CD4+CD25+ cells from the transplanted donor cells caused more extensive cGVHD as compared with recipients of unfractionated CD4+ T cells (Figure 5B; P < .05 for day 26 after BMT and thereafter), although the incidence of disease was similar. In contrast, transplantation of additional CD4+CD25+ T cells resulted in decreased penetrance (Figure 5A; P < .01) as well as extent of cGVHD (Figure 5B; P < .05 day 27; P < .01 days 30 to 45 after BMT) as compared with recipients of unfractionated CD4 cells.
Strikingly, recipients of additional CD4+CD25+ T cells had virtually no histopathologic skin disease at day 45, being indistinguishable from BM-alone controls (P = .3) and clearly different from recipients of CD4+ or CD4+/CD25- T cells (Figure 5C; P < .01 versus CD4+ and CD4+CD25+ recipients). In contrast, histology scores for CD4+/CD25- recipients showed even more severe disease (P < .01 versus CD4 recipients). The progression of clinical cGVHD was also different among the experimental cohorts. This was determined by comparing the percentage of mice that had equivalent or more extensive clinical disease at day 45 with day 21 (mice appearing healthy at day 21 were not included in the comparisons). Similar or more extensive clinical disease was seen in 78.9% and 96.6% of total CD4+ and CD4+CD25- recipients, respectively, showing a clear tendency to progress. On the other hand, disease progressed in only 25% of CD4+CD25+ recipients (P < .05 for total CD4+ and CD4+CD25- recipients versus the group that received CD4+CD25+ cells).
This point is further illustrated by the clinical course of individual representative mice in T-cell recipients (Figures 5D-F). As noted, clinical disease tended to be progressive or unremitting in mice that did not receive CD4+CD25+ cells (Figure 5D-E). A very different clinical course was seen in recipients of additional CD4+CD25+ T cells (Figure 5F). Early disease was similar to other T-cell recipient groups, with small lesions developing around day 18 after BMT; however, 5 of 10 mice developed ulcers that healed after approximately 1 week. Two of these animals showed no evidence of cGVHD at later time points, while 3 animals developed new lesions 1 to 3 weeks later (representative data shown in Figure 5F). One animal developed small lesions on the final time point (day 45). The sporadic occurrence and disappearance of skin lesions suggests ongoing regulation of the alloresponse. Thus, in agreement with other studies using murine models of acute GVHD across major MHC barriers, we conclude that donor CD4+CD25+ T cells can control severity of cGVHD. However, in addition, these data show that donor CD4+CD25+ T cells given at the time of transplantation can have late effects on established disease.
Discussion
Here we have shown that recipient CD4+CD25+ T cells normally regulate cGVHD in a murine model. This was initially inferred from the increased cGVHD seen in RAG2-/- and TCRα-/- mice versus the intact recipients. The role of host CD4+CD25+ T cells was further indicated by the finding that they can ameliorate cGVHD in RAG2-/- hosts whereas other T cells cannot. These 2 observations together strongly suggest that surviving CD4+CD25+ host T cells (Table 1) modulated cGVHD.
Our results raise the question of how these host T cells mediate this regulation. The explanation that a developmental defect due to lack of T cells per se was ruled out because repletion of monoclonal T cells without a CD4+CD25+compartment (ie, DO11.10 RAG2-/- mice) did not ameliorate cGVHD. Similarly, a host-versus-graft effect was rendered very unlikely by the finding that only CD4+CD25+—and not CD4+CD25-—T cells ameliorated cGVHD. There is no reason to think that miHA-reactive T cells would segregate to this compartment; if anything, one might have expected CD25+ cells to be more limited in host-versus-graft potential because they are anergic under many circumstances.73 Blocking homeostatic proliferation was another possible mechanism for modulating cGVHD. All GVHD settings are likely to stimulate homeostatic proliferation by donor T cells, which is defined as proliferation caused in response to lymphopenia rather than specific antigen, because all create lymphopenic host environments.74,75 In fact, whether this plays any mechanistic role in GVHD induction has not been determined. Results from Barthlott and colleagues in a variety of different homeostatic proliferation scenarios clearly show that CD25- T cells are at least as potent as CD25+ T cells at blocking homeostatic proliferation by CD4+ T cells.72 Moreover, in adoptive transfer experiments, Prlic et al saw no effect on homeostatic proliferation of transferred cells by endogenous CD4+CD25+ T cells.76 Because in our system CD25- T cells showed no protection from cGVHD, it is quite unlikely that CD4+CD25+ cells work by blocking homeostatic proliferation.
These considerations leave us with the possibility that host CD4+CD25+ T cells ameliorate cGVHD by “classical” regulatory T-cell mechanisms. Such mechanisms have been defined in numerous systems and can include IL-10 secretion, TGF-β, and contact-dependent effects.73,77-88 To clearly define such mechanisms in our system will require obtaining the proper knock-outs on BALB/c and repeating the infusion experiments. Because regulatory T cells can use different mechanisms in particular pathologic situations, these studies will be worth carrying out in the future.
Our data indicate that host cells that survive irradiation have demonstrable effects. It is interesting to consider that regulatory T cells could function after irradiation, presumably with reduced or absent proliferative capacity. In the inflammatory bowel disease model, CD4+CD25+ T cells have been shown to proliferate, but whether this is essential for function is unknown.57 In vitro, such cells can show suppressive activity without significant proliferation.89 There are other precedents for modulation of GVHD by surviving host cells. A polymorphism in the IL-10 promoter that affects expression influences risk of GVHD and must be present in the recipient, indicating that a recipient IL-10–producing cell plays a role in GVHD.90 In one model of transplantation, Lan and colleagues reported that host DX5+/asialo-GM1+ natural killer (NK) T cells that survived lymphoid irradiation inhibited GVHD in an IL-4–dependent manner in recipient BALB/c mice receiving an MHC-mismatched transplant.91 In our cGVHD model, NK cells are unlikely to play a role because anti–asialo-GM1 treatment of hosts prior to transplantation did not modify GVHD (data not shown).
We also showed that donor CD4+CD25+ T cells inhibited cGVHD. Similar findings have already been reported in several MHC- and miHA-mismatched GVHD models,25-31 though none in a model with the features of cGVHD seen in the B10.D2 → BALB/c strain pair. Thus, our results do extend these earlier findings to some unique pathologic manifestations. Even more intriguing is the finding that donor T cells modulate skin GVHD at later stages of disease, something that might only be observable in this chronic, nonlethal model. We would have thought that the major effect of CD4+CD25+ T cells given at the time of transplantation would be to prevent initial priming of alloreactive donor T cells. While this may occur, the very clear effects in promoting healing of established lesions (Figure 5) suggest that CD4+CD25+ T cells may (also) be working in target tissues or their draining lymph nodes at later times. It will be interesting to follow up this issue. One possibility is that donor CD4+CD25+ T cells in some fashion induce or promote the development of a new population of regulatory T cells—either from the donor CD4+ T-cell inoculum or from reconstituting BM-derived cells—and that these in turn mediate the late effects. Such a mechanism would be a form of infectious tolerance, which has been well documented in other systems such as solid organ and skin transplantation.92 Alternatively, the initial inoculum of regulatory T cells could persist and themselves act early and late. In addition, donor CD4+CD25- T cells could exert effects early in T-cell activation that only become evident at later times; for example, they may not affect priming of early effector cells but could alter the generation of memory-type cells. That some recipients of additional CD4+CD25+ cells heal initial lesions, but later develop recurrent disease, suggests that there is active ongoing regulation that perhaps wanes over time (Figure 5). The observation that donor T cells can promote healing of late-stage lesions holds out the promise that regulatory T cells could be useful as therapy for established cGVHD. It will therefore be interesting to determine if late infusions of donor-type CD4+CD25+ T cells or in vivo depletion of these cells will modulate ongoing cGVHD in mice.
Clinically, our observations are directly relevant to the effects that various conditioning regimens have on the incidence and type of GVHD. Nonmyeloablative stem cell transplantation uses a relatively nontoxic preparative strategy focused on immunosuppression using lymphocyte-depleting agents. This approach minimizes the presumed “cytokine storm” associated with the inflammation that follows massive cell death and compromise of mucosal barriers, which was predicted to reduce GVHD. However, GVHD, and especially cGVHD, has occurred in a surprisingly high fraction of nonmyeloablative stem cell transplant recipients.4,93-97 A mechanism suggested by our results is that the lymphocyte depletion caused by the preparative regimen ablates the endogenous regulatory T-cell response. Further investigation could reveal whether this novel mechanism should impact the design of preparative regimens.
Taken together, the data reported here show for the first time that host CD4+ T cells that persist after lethal radiation control the incidence and severity of cGVHD. In addition, repletion of either host- or donor-type CD4+CD25+ T cells restored the defect in lymphocyte-deficient recipients. These data have implications for our understanding of the function of regulatory T cells, suggesting that CD4+CD25+ T cells can act at late time points and even after irradiation. The results also suggest a mechanism for increased cGVHD after nonmyeloablative alloSCT and could guide the design of preparative regimens that would maintain residual host regulatory T-cell activity.
Prepublished online as Blood First Edition Paper, May 18, 2004; DOI 10.1182/blood-2004-01-0328.
Supported by National Institutes of Health (NIH) grants R01 HL66279 (M.J.S.), K08 HL03979 (W.D.S.), and T32 AI 071019-23-25 (B.E.A.).
M.J.S. and W.D.S. contributed equally to this study.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Bob Tigelaar, Fadi Lakkis, and Dan Kaplan for critical reading of the manuscript. We thank the Yale Animal Resources Center staff for superb animal care.




This feature is available to Subscribers Only
Sign In or Create an Account Close Modal