Two articles in this issue provide further hope for the future of novel hemophilia therapies. In one of these articles, long-term therapeutic expression of factor IX has followed lentiviral-mediated prenatal transgene delivery, while the second article describes studies of factor IX expression and immunogenicity in hemophilia B mice rendered transgenic for several human factor IX mutations.
While current hemophilia treatments with both plasma-derived and recombinant clotting factor concentrates are safe and effective, there continues to be progress toward the development of novel therapies that might ultimately result in long-term cure of this disease. In this issue, 2 articles describe important preclinical advances for the treatment of hemophilia B.
Waddington and colleagues report their results of using lentiviral-mediated delivery of a human factor IX (FIX) transgene to immuno-competent mice at 16 weeks gestation by injection into the yolk sac vessels, a route of delivery corresponding to umbilical vein injection in humans. This mode of administration targets the liver, and in this study, in which 50% of the fetal liver cells were found to be in a proliferative state, up to 5% of hepatocytes were transduced with the therapeutic lentivector.
In 3 hemophilic and 6 normal outbred mice, these single-transgene administrations resulted in therapeutic plasma levels of human FIX out to more than 400 days after injection. In the hemophilic animals, the human FIX antigen levels ranged from 0.11 to 0.18 U/mL at around 300 days after treatment. Throughout the study, the levels of functional human FIX:C showed a significant correlation with the FIX:Ag levels but were consistently and inexplicably approximately 5-fold higher than the antigen levels. In contrast, mice treated prenatally with an adenoviral FIX construct showed only low-level and transient human FIX expression.
In addition to documenting the long-term therapeutic expression of FIX, this study has also shown a number of other promising details. There was no evidence of hepatoxicity, no apparent germ line transmission of the lentivector, and none of the mice developed anti-human FIX antibodies, even after being challenged with human FIX coadministered with adjuvants.
The results of this study provide very encouraging news for the hemophilia gene therapy community. However, ongoing concerns about the potential adverse outcomes from insertional mutagenesis and the extent to which studies in fetal mice can be extrapolated to humans will require further work to corroborate this study.
In the related work of Sabatino and colleagues, another important advance in developing mouse models for preclinical testing of hemophilia gene therapy is reported. To date, 3 mouse models of hemophilia B exist.1-3 In each of these models, the resulting gene disruption has produced a null phenotype for murine FIX with the consequence that any FIX produced by these animals is likely to be immunogenic. These investigators have addressed this limitation of the murine hemophilia B model by introducing a wild-type and several different mutant human FIX transgenes into the gene-disrupted hemophilia B mouse. These FIX mutations represent a small sample of the several hundred genetic alterations now documented to produce this phenotype in humans. Mice transgenic for the various human FIX constructs (wild-type, 5′ and 3′ nonsense mutations, and 2 missense mutations) were generated by a standard microinjection technique and transgene-positive males were crossed with hemophilia B females to obtain animals transgenic for the human FIX sequences on a mouse FIX null background.
The biosynthetic characteristics and functional activity of the human FIX constructs were studied in cell culture and in the transgenic mice, and, most importantly, the host immune response to an adeno-associated virus (AAV)-mediated intramuscular delivery of a human FIX transgene was evaluated in the mice. These latter studies showed results that would be predicted from our knowledge of FIX immunogenicity in human hemophiliacs, with the appearance of anti-FIX antibodies only in the original FIX null mice and in the 2 transgenic strains with nonsense mutations.
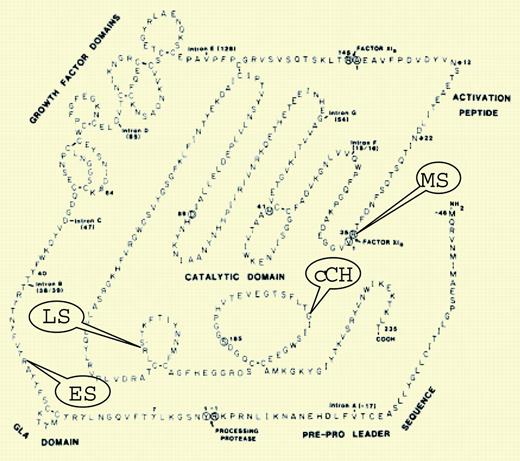
As preclinical studies of hemophilia gene therapy continue, the development of animal models that best reflect the likely efficacy and safety of this therapeutic approach in humans is critical. This is particularly important for the assessment of the host immune response to the transgene product. The report of Sabatino and colleagues represents an important advance toward the attainment of such a model for hemophilia B.FIG1
Human FIX transgenes expressed in mice. See the complete figure in the article beginning on page 2767.
Human FIX transgenes expressed in mice. See the complete figure in the article beginning on page 2767.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal