Abstract
The impact of estrogens on the cardiovascular system and their ability to regulate platelet function are matters of controversy. The recent finding that estrogen receptors are expressed in human platelets renders these cells an excellent model for studying the nongenomic effects of these hormones. In this work, we investigated 17β-estradiol–dependent signaling in platelets from adult healthy men. 17β-estradiol caused the rapid phosphorylation of the tyrosine kinases Src and Pyk2 and the formation of a signaling complex, which included Src, Pyk2, and the phosphatidylinositol 3-kinase. Both these events were dependent on estrogen receptor β engagement. We found that estrogen receptor β was membrane-associated in platelets. On treatment with 17β-estradiol, Src and Pyk2 activation occurred in the membrane fraction but not in the cytosol. In contrast, no significant activation of phosphatidylinositol 3-kinase was detected in estrogen-treated platelets. 17β-estradiol did not induce any platelet response directly, but it strongly potentiated the activation of integrin αIIbβ3 and the platelet aggregation induced by subthreshold concentrations of thrombin. These effects were dependent on estrogen receptor β recruitment and were associated with a strong synergistic effect with thrombin on Src activation. Taken together, these results indicate that 17β-estradiol can modulate platelet function by exercising a proaggregating role.
Introduction
Steroid hormones bind to nuclear receptors and regulate a number of biologic processes, including morphogenesis, cell proliferation, differentiation, and apoptosis.1,2 Recently, it has been reported that, in addition to these classical actions, steroid hormones can also induce rapid, nongenomic effects in different cell types.3 These effects include regulation of adenylyl cyclase, stimulation of p21ras and mitogen-activated protein kinases, activation of phosphatidylinositol 3-kinase (PI3-K), and mobilization of Ca2+ from intracellular stores.4-11 Estrogens have also been reported to affect the cardiovascular system. For instance, engagement of membrane-associated estrogen receptors causes the rapid stimulation of endothelial nitric oxide synthase, leading to the production of nitric oxide in endothelial cells.12,13 Moreover, estrogen has been found to alter the metabolism of plasma lipoproteins, promoting a decrease in low-density lipoprotein levels and a concomitant increase in high-density lipoprotein levels.14
The role of sex steroid hormones in the regulation of platelet function has been investigated for years, but conflicting results have been reported.15-21 Many of the discrepancies can be ascribed to the different experimental models analyzed. In fact, though some studies have been performed on washed platelets exposed to high concentrations of hormones, others have analyzed the functional responses of platelets isolated from donors being treated with estrogens. Moreover, for many years, the rationale for the investigation of the effects of estrogens on human platelets has been questioned because of the supposed absence of estrogen receptors in these anucleated cells. Recently, however, estrogen receptor α (ERα) and estrogen receptor β (ERβ) have been found to be expressed in circulating platelets.22,23 Although this finding suggests that estrogens can actually exert a nongenomic effect in these anucleated cells, the signal transduction pathways and the physiologic consequences of ERα and ERβ engagement in platelets have not been investigated.
In a number of cell lines, including Cos-7 and MCF-7 cells, 17β-estradiol (17β-E2) induces the activation of Src kinase and its association with the engaged estrogen receptor.8,24,25 It is well known that activated Src initiates an intracellular signaling transduction cascade that involves different effectors, including mitogen-activated kinases, Pyk2, and PI3-K. For instance, the expression of specific genes is mediated by the Src-dependent activation of mitogen-activated kinases.26-28 Moreover, activated Src was found to bind and to phosphorylate the tyrosine kinase Pyk2.26-28 All these elements involved in estrogen-mediated cell activation are present in human platelets. In particular, these cells express high levels of different tyrosine kinases, including Src and Pyk2, which are rapidly tyrosine-phosphorylated during an early phase of platelet activation.29,30 In addition, PI3-K, a versatile enzyme that catalyzes the production of 3-phosphoinositides and controls a number of cellular events, 31-34 has been found to coimmunoprecipitate with Pyk2 in resting and in stimulated platelets35 and is required for agonist-dependent tyrosine phosphorylation of Pyk2.36
Although platelets contain high levels of different Src kinases, 37 in particular Src, Fyn, Lyn, and Yes, their roles are not completely known. Evidence suggests that platelet Src kinase may be tightly correlated with the regulation of the adhesive functions of integrin αIIbβ3. In fact, Src kinase has been found to physically interact with integrin αIIbβ3 and to be activated upon integrin αIIbβ3–dependent platelet adhesion.38 Moreover, a role for Src kinase in the agonist-induced stimulation of the affinity of integrin αIIbβ3 for fibrinogen, through a process indicated as inside-out signaling, has been proposed.39,40
In this work, we have investigated the effect of the treatment with acute doses of estrogens on the function of human platelets from healthy men, and we have characterized the signal transduction pathways activated upon engagement of ERβ, which is the predominant estrogen receptor expressed in these cells. We have found that 17β-E2 caused the rapid and transient tyrosine phosphorylation of Src and the formation of a membrane-associated, Src-dependent signaling complex, which includes ERβ, Src, Pyk2, and PI3-K. Moreover, we have found that, in platelets stimulated with low concentrations of thrombin, 17β-E2 caused a strong potentiation of integrin αIIbβ3 activation and platelet aggregation through a mechanism dependent on ERβ engagement and Src kinase activation. These results indicate that estrogen may have proaggregatory effects on human platelets, and they identify critical events in the signal transduction pathways mediating nongenomic effects of 17β-E2.
Materials and methods
Materials
Polyclonal antibodies against ERβ and Pyk2, monoclonal antibody against Src, and horseradish-peroxidase–conjugated antigoat antibody were from Santa Cruz Biotechnology (Santa Cruz, CA). Polyclonal anti–p85/PI3-K, monoclonal anti–caspase-9, and antiphosphotyrosine antibodies were from Upstate Biotechnology (Lake Placid, NY). Monoclonal antibody anti-Akt, phosphospecific polyclonal antibodies anti-Src kinases (Tyr416), and anti-Akt (Ser473 and Thr308) were from Cell Signaling Technology (Beverly, MA). Goat anti–mouse immunoglobulin G (IgG) horseradish-peroxidase–labeled antibodies and enhanced chemiluminescence (ECL) reagents were from Perkin Elmer Life Science (Boston, MA), and goat anti–rabbit IgG horseradish-peroxidase–labeled antibody was from NEN Life Science Products (Brussels, Belgium). Fluorescein isothiocyanate (FITC)–conjugated PAC-1 antibody was from Becton Dickinson (San Jose, CA). Thrombin, 17β-E2, wortmannin, protein A–and protein G–Sepharose 4B Fast Flow, protease inhibitor cocktail, bovine serum albumin, digitonin, Triton X-100, leupeptin, phenylmethylsulfonyl fluoride (PMSF), aprotinin, and orthovanadate were purchased from Sigma-Aldrich (St Louis, MO). BCA protein assay kit was from Pierce (Rockford, IL). Electrophoresis reagents were from Bio-Rad Laboratories (Hercules, CA). Hybond-P polyvinylidene difluoride (PVDF) transfer membranes, Hyperfilm-ECL, and cyclic adenosine monophosphate (cAMP) assay kit were from Amersham Pharmacia Biotech (Uppsala, Sweden). U46619 and PP1 were from Alexis Biochemicals (Lausen, Switzerland). FURA-2/am was from Calbiochem (San Diego, CA). ICI 182,780 was from Tocris (Bristol, United Kingdom). All other reagents were of analytical grade.
Platelet preparation and aggregation studies
Blood was withdrawn from 20- to 40-year-old healthy male volunteers who had not taken any drugs for at least 2 weeks before venipuncture; ACD (130 mM citric acid, 152 mM sodium citrate, 112 mM glucose) was used as the anticoagulant. Platelets, obtained by gel filtration on Sepharose CL-2B as previously described, 41 were adjusted to 3 × 108 cells/mL in HEPES (N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid) buffer containing 2 mM CaCl2, 2 mM MgCl2, and 2 mM glucose. Platelet samples (0.4 mL) were preconditioned at 37°C in a lumiaggregometer before 17β-E2 (100 nM) or thrombin (0.02 or 1 U/mL) was added. Preincubation of platelets with 100 nM 17β-E2 before thrombin stimulation was performed for 30 seconds. Platelets were preincubated with the SRC kinase inhibitor PP1 (10 μM) for 15 minutes before stimulation, and the ER competitive inhibitor ICI 182 780 (10 μM) was added together with 17β-E2 before stimulation. Platelet aggregation was monitored continuously as light transmission increment.
Subcellular localization of ERβ and signaling proteins in 17β-E2–treated platelets
Gel-filtered platelets were treated with buffer or with 100 nM 17β-E2 for increasing times, and membranes and cytosol were prepared on lysis with digitonin, essentially as described by Barry and Gibbins.42 Aliquots of cytosol and membrane-rich fractions, containing the same amounts of protein, were separated by sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) on 8% polyacrylamide gels, transferred to PVDF membrane, and probed with anti-ERβ or anti–caspase-9 antibodies. Membrane fractions were also probed with specific antibodies against Src, Src phospho-Tyr416 (pSrc-Tyr416), Pyk2, and p85/PI3-K. Immunoreactive bands were detected by an ECL reaction.
Analysis of thrombin- and 17β-E2–induced tyrosine phosphorylation of Src
Samples of gel-filtered platelets were incubated with increasing concentrations of 17β-E2 (1 nM-1 μM), with 0.02 U/mL thrombin, or with 100 nM 17β-E2 and 0.02 U/mL thrombin for 15 to 180 seconds, as indicated in the figures. In some experiments, 10 μM ICI 182 780 was added to platelet samples together with 17β-E2. Aliquots of each sample containing the same amounts of protein were simultaneously analyzed by immunoblotting using anti-pSrc-Tyr416 and anti-Src antibodies.
Immunoprecipitation
Gel-filtered platelets, resting or treated with 100 nM 17β-E2 (0.4 × 109 cells/mL) and eventually preincubated at 37°C with 10 μM PP1 or 50 nM wortmannin for 15 minutes, were lysed with immunoprecipitation buffer 2 × (100 mM Tris/HCl, pH 7.4, 200 mM NaCl, 2 mM ethyleneglycotetraacetic acid (EGTA), 2% Nonidet P40, 0.5% sodium deoxycholate, 20% glycerol, 20 μg/mL leupeptin, 20 μg/mL aprotinin, 2 mM PMSF, 2 mM Na3VO4, 2 mM NaF). Protein A–Sepharose-precleared supernatants were incubated with anti-p85/PI3-K or anti-Pyk2 antibodies (1 μg) for 2 hours at 4°C, immunoprecipitated with 50 μL protein A–Sepharose for 45 minutes, and washed 3 times with immunoprecipitation buffer 1 ×. Immunoprecipitated proteins were separated by SDS-PAGE, transferred to PVDF membrane, and probed with antiphosphotyrosine antibodies. In some experiments, membranes were stripped and reprobed with anti-p85/PI3-K or anti-Pyk2 antibodies. For coimmunoprecipitation experiments, cells were lysed with 1% NP-40 lysis buffer (1% NP-40, 150 mM NaCl, 50 mM Tris-HCl (pH 8.0), 5 mM EDTA, 10 mM NaF, 10 mM Na4P2O7, 0.4 mM Na3VO4, 10 μg/mL leupeptin, 4 μg/mL pepstatin, and 0.1 U/mL aprotinin). Samples containing the same amount of proteins (typically 2 mg) were immunoprecipitated with antibodies against ERβ for 1 hour at 4°C in the presence of 50 μL protein A–Sepharose beads. Immunoprecipitated proteins were analyzed by immunoblotting with specific antibodies, as described.
Analysis of PI3-K activation in 17β-E2–treated platelets
Platelet samples were incubated with buffer or 100 nM 17β-E2 for 1 minute, or they were stimulated with 1 U/mL thrombin or 2 μM U46619 for 3 minutes. Aliquots of each sample containing the same amounts of proteins were separated by SDS-PAGE on 10% polyacrylamide gels, transferred to PVDF membranes, and probed with anti–phospho-Akt-Ser473 or anti–phospho-Akt-Thr308 antibody. In parallel, corresponding aliquots of the samples were analyzed by immunoblotting with anti-Akt antibody.
Evaluation of platelet cytosolic Ca2+ and cAMP concentration
Platelet-rich plasma (PRP) was incubated with 3 μM FURA-2/am at 37°C for 40 minutes before gel-filtration on Sepharose CL-2B. Platelet samples preconditioned at 37°C were stimulated with 100 nM 17β-E2. Cytosolic Ca2+ concentration was measured in a spectrofluorimeter, as previously described.43 To measure intracellular cAMP concentration, samples containing 1 × 108 cells/mL were incubated at 37°C with 100 nM 17β-E2 for 30 seconds. Platelets were lysed, and cAMP content was evaluated using a commercial assay kit, according to the manufacturer's instruction.
Measurement of PAC-1 binding by flow cytometry
PAC-1 binding to gel-filtered platelets was measured basically as described by Shattil et al, 44 with some modifications. Aliquots of platelet suspension (3 × 108 cells/mL) were stimulated with buffer, 0.02 U/mL or 1 U/mL thrombin, 100 nM 17β-E2, or 100 nM 17β-E2 for 30 seconds before the addition of 0.02 U/mL or 1 U/mL thrombin. Stimulation was performed for 10 minutes at 37°C in the presence of FITC-labeled PAC-1 antibody (2.5 μg/mL) and was then stopped by the addition of 4 volumes of a freshly prepared 0.5% paraformaldehyde solution. In some experiments, cells were preincubated at 37°C with 10 μM PP1 for 15 minutes before stimulation or with 10 μM ICI 182 780. Flow cytometry analysis was carried out on a Becton-Dickinson FACScalibur, acquiring data of 5000 particles per sample. The significance of the differences between 2 series of data was evaluated by Student t test.
Results
Src kinase activation in 17β-E2–treated platelets
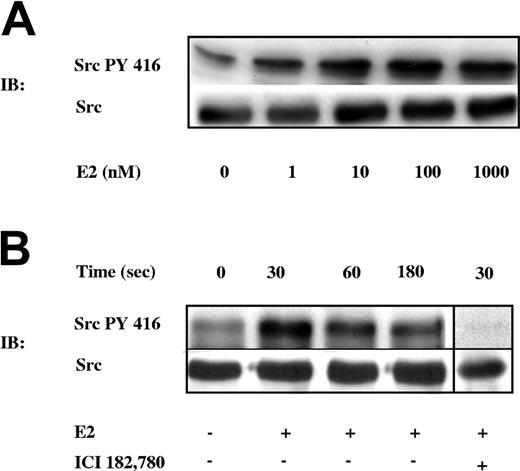
The tyrosine kinase Src is involved in signal transduction pathways activated by 17β-E2 in different cell types.8,24,25 To investigate the possible effects of 17β-E2 on platelet signaling, we examined whether the hormone was able to trigger the activation of the tyrosine kinase Src in these cells. Gel-filtered platelets were incubated with increasing concentrations of 17β-E2 for 30 seconds. Identical aliquots from each sample were analyzed by immunoblotting with a phosphospecific antibody recognizing the activated, Tyr416-phosphorylated form of Src (pSrc-Tyr416). In parallel, identical aliquots from the same samples were analyzed by immunoblotting with an anti-Src antibody to verify that the same amount of protein was present in each sample. Figure 1A shows that 17β-E2 triggered Src phosphorylation on Tyr416 in a dose-dependent manner. Because maximal activation of Src was achieved by 100 nM 17β-E2, this concentration was used in all subsequent experiments.
17β-E2–dependent Src kinase activation. (A) Gel-filtered platelets were incubated with buffer or with increasing concentrations of 17β-E2 (E2: 1, 10, 100, and 1000 nM) for 30 seconds. (B) Gel-filtered platelets were incubated with buffer or with 100 nM 17β-E2 (E2) for increasing times (0, 30, 60, and 180 seconds.) Platelets were lysed, and identical aliquots from each sample were simultaneously analyzed by immunoblotting with specific antibodies against pSrc-Tyr416 (Src PY 416) or against Src. Platelet stimulation with 100 nM 17β-E2 for 30 seconds was performed in the presence of 10 μM ICI 182 780, an ER antagonist. Results are representative of those of several different experiments.
17β-E2–dependent Src kinase activation. (A) Gel-filtered platelets were incubated with buffer or with increasing concentrations of 17β-E2 (E2: 1, 10, 100, and 1000 nM) for 30 seconds. (B) Gel-filtered platelets were incubated with buffer or with 100 nM 17β-E2 (E2) for increasing times (0, 30, 60, and 180 seconds.) Platelets were lysed, and identical aliquots from each sample were simultaneously analyzed by immunoblotting with specific antibodies against pSrc-Tyr416 (Src PY 416) or against Src. Platelet stimulation with 100 nM 17β-E2 for 30 seconds was performed in the presence of 10 μM ICI 182 780, an ER antagonist. Results are representative of those of several different experiments.
We next analyzed the kinetics of Src phosphorylation induced by 17β-E2. Figure 1B shows that 17β-E2–promoted Src phosphorylation on Tyr416 was rapid and transient, because it reached a maximum at 30 seconds and rapidly decreased afterward. 17β-E2–induced Src phosphorylation was totally abolished by preincubation of platelets with the ER antagonist ICI 182 780 (Figure 1B), demonstrating that this effect was mediated by engagement of an ER expressed in platelets.
ERβ coordinates the assembly of an Src-dependent signaling complex in 17β-E2–treated platelets
Although ERα and ERβ have been detected in human platelets, ERβ appears to be the predominant isoform expressed in these cells.22,23 We investigated the possible physical association between ERβ and Src in 17β-E2–treated platelets. ERβ was immunoprecipitated from resting or 17β-E2–treated platelets and then was analyzed by immunoblotting with antibodies against Src or ERβ. Figure 2A shows that Src was actually coimmunoprecipitated with ERβ in estrogen-treated, but not resting, platelets. The amount of Src associated with ERβ was maximal after 60 seconds of stimulation with 17β-E2 and then decreased close to the basal level. The lower panel of Figure 2A shows that comparable amounts of ERβ were immunoprecipitated from each sample.
Formation of an ERβ-associated signaling complex in estrogen-treated platelets. (A) Platelets were treated with buffer or 100 nM 17β-E2 for the indicated times, and ERβ was immunoprecipitated with specific antibodies. Immunoprecipitated proteins were analyzed by immunoblotting with anti-Src antibody and were reprobed with anti-ERβ antibody. (B) Immunoprecipitates obtained with anti-ERβ antibodies from resting platelets or platelets incubated with 100 nM 17β-E2 for 60 and 180 seconds, together with aliquots of whole platelet lysates (WCL), were analyzed by immunoblotting with antibodies against pSrc-Tyr416, Pyk2, p85/PI3-K, FAK, Syk, and ERβ, as indicated on the left. (C) ERβ was immunoprecipitated from resting or 17β-E2–stimulated platelets (E2; 100 nM, 60 seconds) preincubated for 15 minutes in the absence or presence of 10 μM PP1 or 50 nM wortmannin. Immunoprecipitated proteins were analyzed by immunoblotting with antibodies against Pyk2, p85/PI3-K, Src, and ERβ. Results are representative of those of at least 3 different experiments.
Formation of an ERβ-associated signaling complex in estrogen-treated platelets. (A) Platelets were treated with buffer or 100 nM 17β-E2 for the indicated times, and ERβ was immunoprecipitated with specific antibodies. Immunoprecipitated proteins were analyzed by immunoblotting with anti-Src antibody and were reprobed with anti-ERβ antibody. (B) Immunoprecipitates obtained with anti-ERβ antibodies from resting platelets or platelets incubated with 100 nM 17β-E2 for 60 and 180 seconds, together with aliquots of whole platelet lysates (WCL), were analyzed by immunoblotting with antibodies against pSrc-Tyr416, Pyk2, p85/PI3-K, FAK, Syk, and ERβ, as indicated on the left. (C) ERβ was immunoprecipitated from resting or 17β-E2–stimulated platelets (E2; 100 nM, 60 seconds) preincubated for 15 minutes in the absence or presence of 10 μM PP1 or 50 nM wortmannin. Immunoprecipitated proteins were analyzed by immunoblotting with antibodies against Pyk2, p85/PI3-K, Src, and ERβ. Results are representative of those of at least 3 different experiments.
Given that 17β-E2 was found to induce the activation of Src, we next investigated whether the ERβ-associated Src in 17β-E2–treated platelets was actually phosphorylated on Tyr416. Moreover, the possibility was analyzed that other signaling proteins involved in estrogen-mediated signaling and platelet activation—such as Syk, Pyk2, FAK, and p85/PI3-K27,28,31,33,45 —associated with ERβ in 17β-E2–treated platelets. As shown in Figure 2B, in addition to pSrc-Tyr416, Pyk2 and p85/PI3-K coimmunoprecipitated with ERβ on platelet stimulation with 17β-E2 for 60 seconds. In contrast, neither FAK nor Syk was detected in the ERβ immunoprecipitates. The formation of this signaling complex was rapid and transient—it underwent complete disassembly after 180 seconds of stimulation. Preincubation of platelets with the Src kinase inhibitor PP1 before stimulation with 17β-E2 completely prevented the association of Src, Pyk2, and p85/PI3-K with ERβ (Figure 2C), indicating that the formation of this signaling complex requires Src activity. However, the association of Src, Pyk2, and p85/PI3-K with ERβ was not affected by the PI3-K inhibitor wortmannin (Figure 2C).
Role of 17β-E2 on the subcellular localization of ERβ, Src, p85/PI3-K, and Pyk2
The subcellular localization of ERβ in human platelets treated with 17β-E2 was investigated by immunoblotting on the fractionation of platelets into membrane-rich (MR) and cytosolic (CYT) fractions. As shown in Figure 3A, ERβ was exclusively detected in the membrane fractions but not in the cytosol, both in resting and in 17β-E2–treated platelets. Caspase-9 was detected only in the cytosolic fractions, as expected. Therefore, ERβ was membrane localized in human platelets and did not relocate upon treatment of these cells with 17β-E2.
Subcellular localization of ERβ, Src, p85/PI3-K, and Pyk2 in 17β-E2–treated platelets. Cytosol (CYT) and membrane-rich (MR) fractions were prepared from platelets incubated with buffer or with 100 nM 17β-E2 for 30, 60, and 180 seconds, as described in “Materials and methods.” (A) Identical amounts of protein from each fraction were analyzed by immunoblotting with anti-ERβ and anti–caspase-9 antibodies. (B) Aliquots containing the same amount of proteins from each MR fraction obtained from platelets, treated as described for panel A, were analyzed by immunoblotting with antibodies against Src, pSrc-Tyr416, Pyk2, and p85/PI3-K, as indicated on the left. Results are representative of those of at least 4 different experiments.
Subcellular localization of ERβ, Src, p85/PI3-K, and Pyk2 in 17β-E2–treated platelets. Cytosol (CYT) and membrane-rich (MR) fractions were prepared from platelets incubated with buffer or with 100 nM 17β-E2 for 30, 60, and 180 seconds, as described in “Materials and methods.” (A) Identical amounts of protein from each fraction were analyzed by immunoblotting with anti-ERβ and anti–caspase-9 antibodies. (B) Aliquots containing the same amount of proteins from each MR fraction obtained from platelets, treated as described for panel A, were analyzed by immunoblotting with antibodies against Src, pSrc-Tyr416, Pyk2, and p85/PI3-K, as indicated on the left. Results are representative of those of at least 4 different experiments.
Platelet membrane fractions were then analyzed to investigate the subcellular localization and possible relocation of the signaling proteins recruited by ERβ upon treatment of platelets with 17β-E2. Figure 3B shows that identical amounts of Src were present in the membranes of resting and 17β-E2–treated platelets. Membrane-associated active Tyr416-phosphorylated Src, however, rapidly and transiently increased upon platelet treatment with 17β-E2. In addition, Figure 3B shows that, upon stimulation of platelets with 17β-E2, a significant but transient translocation of Pyk2 to the platelet membranes also occurred. Identical amounts of p85/PI3-K were detected in all the membrane fractions analyzed, indicating that p85/PI3-K and Pyk2 undergo different types of relocation in estrogen-treated human platelets.
Pyk2, but not p85/PI3-K, is tyrosine-phosphorylated in 17β-E2–treated platelets by a Src-dependent mechanism
To further characterize the involvement of Pyk2 and p85/PI3-K in ERβ-dependent signaling in human platelets, we investigated the tyrosine phosphorylation of these proteins in 17β-E2–treated platelets. Both Pyk2 and p85/PI3-K were immunoprecipitated from platelet lysates, analyzed by immunoblotting with antiphosphotyrosine antibodies, and subsequently reprobed with anti-Pyk2 or anti–p85/PI3-K antibodies. Figure 4A shows that 17β-E2 caused a sustained tyrosine phosphorylation of Pyk2 that persisted up to 180 seconds of stimulation. Preincubation of platelets with the Src kinase inhibitor PP1 completely prevented 17β-E2–induced tyrosine phosphorylation of Pyk2. By contrast, no tyrosine-phosphorylated proteins with a molecular mass of 85 kDa, corresponding to the regulatory subunit of p85/PI3-K, were detected in immunoprecipitates with anti-p85/PI3-K antibodies (Figure 4B). To analyze whether PI3-K was activated in 17β-E2–treated platelets, despite the lack of tyrosine phosphorylation of the regulatory subunit p85, we investigated the estrogen-induced phosphorylation of Akt, a known PI3-K downstream effector, 46 by immunoblotting with phosphospecific antibodies against Akt (phospho-Ser473 or phospho-Thr308). Figure 4C shows that, as expected, Akt was robustly phosphorylated in response to thrombin or to the thromboxane A2 analog U46619. In platelets stimulated with 17β-E2, faint, almost negligible, phosphorylation of Akt was detected, indicating that estrogens do not significantly signal through PI3-K in platelets.
Analysis of Pyk2 and PI3-K activation in estrogen-treated platelets. (A) Pyk2 and (B) p85/PI3-K were immunoprecipitated from gel-filtered platelets treated with 100 nM 17β-E2 (E2) for 60 or 180 seconds. Pyk2 was also immunoprecipitated from platelets preincubated with 10 μM PP1 for 15 minutes before treatment with 100 nM 17β-E2 for 60 seconds. Immunoprecipitated proteins were analyzed by immunoblotting with antiphosphotyrosine antibodies and then were reprobed with the same antibody used for immunoprecipitation (anti-Pyk2 or anti-p85/PI3-K, as indicated). Analysis of Akt phosphorylation was performed in resting platelets or in platelets treated with 100 nM 17β-E2 for 60 seconds or stimulated with 1 U/mL thrombin (Thr) or 2 μM U46619 for 180 seconds. Identical amounts of whole platelet proteins were analyzed by immunoblotting with anti–phospho-Akt-Ser473 or anti–phospho-Akt-Thr308 antibodies. (C) In parallel, corresponding aliquots of the samples were analyzed by immunoblotting with anti-Akt antibody. Results are representative of those of at least 3 separate experiments.
Analysis of Pyk2 and PI3-K activation in estrogen-treated platelets. (A) Pyk2 and (B) p85/PI3-K were immunoprecipitated from gel-filtered platelets treated with 100 nM 17β-E2 (E2) for 60 or 180 seconds. Pyk2 was also immunoprecipitated from platelets preincubated with 10 μM PP1 for 15 minutes before treatment with 100 nM 17β-E2 for 60 seconds. Immunoprecipitated proteins were analyzed by immunoblotting with antiphosphotyrosine antibodies and then were reprobed with the same antibody used for immunoprecipitation (anti-Pyk2 or anti-p85/PI3-K, as indicated). Analysis of Akt phosphorylation was performed in resting platelets or in platelets treated with 100 nM 17β-E2 for 60 seconds or stimulated with 1 U/mL thrombin (Thr) or 2 μM U46619 for 180 seconds. Identical amounts of whole platelet proteins were analyzed by immunoblotting with anti–phospho-Akt-Ser473 or anti–phospho-Akt-Thr308 antibodies. (C) In parallel, corresponding aliquots of the samples were analyzed by immunoblotting with anti-Akt antibody. Results are representative of those of at least 3 separate experiments.
17β-E2 potentiates thrombin-induced platelet aggregation and integrin αIIbβ3 inside-out signaling
We next investigated whether 17β-E2–induced activation of Src and formation of the signaling complex could result in a platelet functional response. We found that treating gel-filtered platelets with 17β-E2 did not result in any detectable aggregation and did not alter the intracellular levels of second messengers such as Ca2+ or cAMP (data not shown).
Therefore, we considered the possibility that 17β-E2 could influence platelet aggregation induced by classic physiologic agonists such as thrombin. Samples of gel-filtered platelets were treated with 17β-E2 for 30 seconds and were then stimulated with high (1 U/mL) or low (0.02 U/mL) doses of thrombin. Upon platelet stimulation with a high concentration of thrombin able to trigger maximal platelet aggregation, preincubation with 17β-E2 did not produce any detectable effect (data not shown). Priming platelets with 17β-E2, however, resulted in a strong potentiation of platelet aggregation induced by a low concentration of thrombin. In fact, as shown by the representative traces reported in Figure 5A, stimulation of platelets with 0.02 U/mL thrombin induced 31.2% ± 10.8% aggregation (n = 4). However, upon preincubation of platelets with 17β-E2, thrombin-induced aggregation increased to 55.3% ± 10.6% (n = 4). Thus, 17β-E2 potentiated the aggregation induced by low doses of thrombin by 73.7% (P = .008; n = 4). Potentiation of platelet aggregation by 17β-E2 was blocked by ICI 182 780, suggesting that it was mediated by ER engagement (Figure 5A). Moreover, preincubation with PP1 totally prevented thrombin-induced aggregation in the absence and in the presence of 17β-E2, indicating an essential role for Src kinase in platelet response to thrombin.
Effect of 17β-E2 on thrombin-dependent platelet aggregation and integrin αIIbβ3 activation. (A) Aggregation traces of gel-filtered platelets treated with 100 nM 17β-E2 (E2), 0.02 U/mL thrombin (Thr), 100 nM 17β-E2 for 30 seconds and then 0.02 U/mL thrombin (E2+Thr), 100 nM 17β-E2, and 10 μM ICI 182 780 for 30 seconds and then 0.02 U/mL thrombin (ICI+E2+Thr), 10 μM PP1 for 15 minutes, 100 nM 17β-E2 for 30 seconds and then 0.02 U/mL thrombin (PP1+E2+Thr). Identical results were obtained from 4 similar experiments performed with platelets from different donors. (B) Binding of FITC-labeled PAC-1, a fibrinogen mimetic antibody that recognizes the active form of integrin αIIbβ3 to resting platelets (Bas), and platelets treated as indicated in panel A. Incubation with PAC-1 was for 10 minutes at 37°C before fixation. Data are mean ± SEM of 7 independent experiments performed with platelets from different donors. * indicates that the difference in PAC-1 binding between the samples stimulated with thrombin in the presence or absence of 17β-E2 is statistically significant (P < .005).
Effect of 17β-E2 on thrombin-dependent platelet aggregation and integrin αIIbβ3 activation. (A) Aggregation traces of gel-filtered platelets treated with 100 nM 17β-E2 (E2), 0.02 U/mL thrombin (Thr), 100 nM 17β-E2 for 30 seconds and then 0.02 U/mL thrombin (E2+Thr), 100 nM 17β-E2, and 10 μM ICI 182 780 for 30 seconds and then 0.02 U/mL thrombin (ICI+E2+Thr), 10 μM PP1 for 15 minutes, 100 nM 17β-E2 for 30 seconds and then 0.02 U/mL thrombin (PP1+E2+Thr). Identical results were obtained from 4 similar experiments performed with platelets from different donors. (B) Binding of FITC-labeled PAC-1, a fibrinogen mimetic antibody that recognizes the active form of integrin αIIbβ3 to resting platelets (Bas), and platelets treated as indicated in panel A. Incubation with PAC-1 was for 10 minutes at 37°C before fixation. Data are mean ± SEM of 7 independent experiments performed with platelets from different donors. * indicates that the difference in PAC-1 binding between the samples stimulated with thrombin in the presence or absence of 17β-E2 is statistically significant (P < .005).
Platelet aggregation is supported by the agonist-induced activation of integrin αIIbβ3 and the subsequent fibrinogen binding.44 To investigate the mechanism by which 17β-E2 potentiated platelet aggregation induced by thrombin, we investigated the inside-out signaling process leading to affinity regulation of integrin αIIbβ3. The activation of integrin αIIbβ3 on stimulated platelets was measured by flow cytometry using FITC-PAC-1, a fibrinogen-mimetic monoclonal antibody. Results from 7 different experiments are reported in Figure 5B. Consistent with its inability to promote platelet aggregation, we found that 17β-E2 alone did not induce the activation of integrin αIIbβ3. Stimulation of platelets with 0.02 U/mL thrombin induced a small increase in PAC-1 binding over nonstimulated platelets, but this increase was clearly able to support a partial platelet aggregation. However, preincubation with 17β-E2 induced a strong and significant increase in PAC-1 binding of platelets stimulated with 0.02 U/mL thrombin. When compared with the response elicited by thrombin alone, priming with 17β-E2 caused a 2.3-fold increase of the fluorescence signal bound to platelets (P < .005; n = 7). The potentiation effect of 17β-E2 on integrin αIIbβ3 inside-out signaling was found to be mediated by recruitment of an ER and to involve the activation of a Src kinase because it was completely reverted by the preincubation of platelets with ICI 182 780 or PP1.
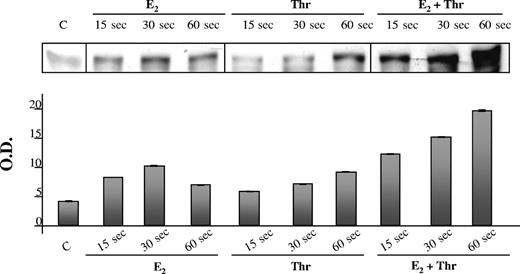
17β-E2 and thrombin induce synergistic activation of Src
To further correlate the ability of 17β-E2 to activate Src through phosphorylation on Tyr416 and to potentiate thrombin-induced platelet aggregation, we analyzed the effect of the combined treatment of platelets with 17β-E2 and a low concentration of thrombin on the phosphorylation of Src on Tyr416. Figure 6 compares the kinetics of Src activation induced by 100 nM 17β-E2 and 0.02 U/mL thrombin. In agreement with the results reported in Figure 1B, 17β-E2 induced rapid and transient tyrosine phosphorylation of Src, which peaked after 30 seconds. Src tyrosine phosphorylation was hardly detectable after 30 seconds in thrombin-stimulated platelets, but it was clearly evident at 60 seconds (Figure 6). When platelets were treated with 17β-E2 and thrombin, much stronger phosphorylation of Src on Tyr416 occurred within 15 seconds, and it further increased for at least 60 seconds. This evidence indicates that 17β-E2 and thrombin exert a synergistic effect on Src phosphorylation, resulting in more rapid and stronger activation of this kinase.
Effect of 17β-E2 on thrombin-dependent Src activation. Platelet samples were treated with 100 nM 17β-E2 (E2), 0.02 U/mL thrombin (Thr), or 100 nM 17β-E2 plus 0.02 U/mL thrombin (E2+Thr) for increasing times (15, 30, and 60 seconds). Identical amounts of total platelet proteins from each sample were analyzed by immunoblotting with anti–pSrc-Tyr416 antibody. Relative amounts of phosphorylated Src detected in each sample were evaluated by densitometric imaging of the immunoblots, and results are reported in the histogram in the bottom part of the figure. Data are mean ± SEM (n = 3). O.D. indicates optical density.
Effect of 17β-E2 on thrombin-dependent Src activation. Platelet samples were treated with 100 nM 17β-E2 (E2), 0.02 U/mL thrombin (Thr), or 100 nM 17β-E2 plus 0.02 U/mL thrombin (E2+Thr) for increasing times (15, 30, and 60 seconds). Identical amounts of total platelet proteins from each sample were analyzed by immunoblotting with anti–pSrc-Tyr416 antibody. Relative amounts of phosphorylated Src detected in each sample were evaluated by densitometric imaging of the immunoblots, and results are reported in the histogram in the bottom part of the figure. Data are mean ± SEM (n = 3). O.D. indicates optical density.
Discussion
In this work, we have described a new intracellular signaling pathway activated by estrogens in human platelets that involves ERβ and the tyrosine kinase Src. Exposure of gel-filtered platelets to 17β-E2 resulted in the rapid and dose-dependent phosphorylation of Src on Tyr416 and induced the transient formation of a signaling complex containing ERβ, Src, Pyk2, and p85/PI3-K. Activation of Src was found to occur at the platelet membrane and was required for the formation of the signaling complex. Although treating platelets with 17β-E2 did not elicit any functional response in the platelets, it primed aggregation induced by thrombin. This process was found to be a consequence of the estrogen-dependent potentiation of thrombin-induced activation of integrin αIIbβ3 and fibrinogen binding through activated Src kinase.
These results document, in a well-defined experimental model, an active role for estrogens in the regulation of platelet function. Although the action of estrogens on human platelets has been investigated for years, contrasting results have been presented, and stimulatory and inhibitory effects have been reported in different studies.15-21 These discrepancies may be attributed to the different methodologies adopted by different investigators, including type of platelet preparation analyzed (washed platelets or PRP), sex and age of blood donors, concentration of estrogens used, and length of platelet exposure to estrogens. In this work, we have exclusively used gel-filtered platelets prepared from male donors exposed to high concentrations of 17β-E2 for a relatively short time. Therefore, the observed events are to be considered consequences of acute platelet treatment with estrogens. It should be noted that cellular response to high nanomolar concentrations of estrogens, such as those used in the present study, has been reported to have physiologic relevance.47
The fact that platelets are anucleated cells, whereas estrogens have long been believed to exert biologic effects exclusively through the regulation of transcriptional processes, has generated serious concern in past years about the physiologic relevance of platelet exposure to these hormones. Recent findings, however, have clearly demonstrated that estrogens can also elicit rapid, nongenomic effects on target cells.48 In addition, the estrogen receptors ERα and ERβ, have been found to be expressed in human platelets.22,23 Therefore, these anucleated cells came to represent an excellent and unique model to selectively investigate the signaling pathways mediating the nongenomic effect of estrogens.
We have demonstrated that the activation of Src and the potentiation of thrombin-induced aggregation in 17β-E2–treated platelets were dependent on the engagement of an estrogen receptor. Moreover, we found that ERβ associated with Src, Pyk2, and p85/PI3-K in a 17β-E2–dependent manner. Therefore, ERβ appeared to be the estrogen receptor mediating the effects of 17β-E2 in human platelets. This conclusion is supported by the evidence that ERβ is actually the main estrogen receptor expressed in these cells. In fact, recently reported23 immunologic evidence for the expression of ERα in platelets has not been confirmed in other studies that failed to detect the protein and the messenger.22 In the present work, we clearly revealed a significant amount of ERβ in the membranous fraction of human platelets, but we failed, under the same conditions, to detect ERα in membranous or cytosolic fractions (data not shown). It is well documented that ERα and ERβ have different patterns of tissue distribution.49 Although both ERα and ERβ mediate genomic and nongenomic effects of estrogens, they may display peculiar features and fulfill different functions. In this regard, mechanistic differences in the activation of ERα- and ERβ-dependent gene expression have been reported.50 Moreover, ERα, but not ERβ, has been found to associate with PI3-K in endothelial cells6 and in human sperm51 as part of the signaling pathway for nongenomic action of estrogens. We found that in human platelets, ERβ associates with PI3-K in a 17β-E2–dependent manner. This interaction however, results in a modest activation of the kinase, as judged by the faint phosphorylation of Akt in estrogen-treated platelets. This may suggest that estrogen-induced activation of PI3-K is more efficiently promoted by the recruitment of ERα than of ERβ. However, the lack of a massive activation of PI3-K does not preclude the possibility for this kinase to play an important role in the estrogen-initiated signaling pathway because it is known that this enzyme may also act as a docking protein. In this regard, a similar role for PI3-K as a docking protein in the formation of a macromolecular signaling complex has been described in von Willebrand factor–stimulated platelets.52
We have also found that, in addition to Src, recruitment of ERβ by 17β-E2 stimulated the tyrosine phosphorylation of Pyk2. Although estrogen-induced Src phosphorylation was rapid and transient, Pyk2 phosphorylation was more sustained and persisted up to 3 minutes. Although Pyk2 has been found to be activated during an early phase of platelet stimulation by different agonists, its exact role in platelet function is still unknown.30 Based on experiments with specific inhibitors, here we have placed Pyk2 downstream of Src in the 17β-E2–mediated signaling pathway for the potentiation of platelet aggregation. However, in the absence of specific inhibitors of Pyk2, its contribution to the estrogen effect remains to be established.
We have also demonstrated that the 17β-E2–mediated potentiation of platelet aggregation, induced by low concentrations of thrombin, resulted from a robust increase of integrin αIIbβ3 affinity for fibrinogen. We observed that albumin-bound estrogen, which does not permeate the cell membrane, was as effective as 17β-E2 in potentiating platelet aggregation induced by thrombin (data not shown), consistent with the membrane localization of ERβ reported in this study.
Our results represent the first evidence that estrogen-mediated signaling can modulate integrin function. Regulation of platelet integrin αIIbβ3 by 17β-E2 involved estrogen receptor–mediated activation of Src kinase. Moreover, we found that platelet treatment with thrombin in the presence of 17β-E2 resulted in a synergistic activation of Src. Thus, our results point to a significant role for Src in the inside-out signaling for integrin αIIbβ3 activation.
The effects of estrogen in priming platelet aggregation have been documented in this study using platelets from male donors. Although platelets from men and from women express similar levels of estrogen receptors, 22 estrogens are present in the plasma of men at a lower concentration than in women, and this concentration is supposed to remain constant. For this reason, we considered platelets from men a more suitable and reliable model to investigate estrogen-mediated signaling and function because they clearly have been more protected from any possible desensitization caused by prolonged exposure to circulating estrogens. Whether platelet response to estrogens is dependent on sex is under investigation.
Evidence that estrogens have pro-aggregatory effects is physiologically relevant because it may confirm previously reported evidence, and it may have clinical implications. For instance, it has been reported that, although there are no differences in the total number of integrin αIIbβ3 expressed on platelets from men and from women, agonist stimulation of platelets from women leads to conversion of a greater proportion of available receptors into the active conformation.53 Our results suggest that this observation may be related to the higher, and variable, concentration of estrogens in the plasma of women. As a consequence, the direct action of estrogens on circulating platelets, in addition to other factors, should be taken into account when programming the acute use of estrogens to improve blood vessel viability and when using low doses of the hormone as a contraceptive or for menopausal symptoms.
In conclusion, our results identify a possible new mechanism by which estrogens may affect the cardiovascular system: in addition to the genomic effects on endothelial cells and smooth muscle cells of the vessel wall, estrogens can directly sensitize platelets to physiologic agonists by strictly nongenomic action on the regulation of integrin αIIbβ3 through ERβ and Src kinase.
Prepublished online as Blood First Edition Paper, June 15, 2004; DOI 10.1182/blood-2003-11-3840.
Supported by grants from Consorzio Interuniversitario Biotecnologie (CIB), MIUR (PRIN 2002), Regione Piemonte, and University “A. Avogadro,” Novara, Italy.
L.M. and S.R. contributed equally to this work.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.





This feature is available to Subscribers Only
Sign In or Create an Account Close Modal