Abstract
Germ-line heterozygous mutations in the hematopoietic transcription factor AML1 (RUNX1) have been identified in patients with familial platelet disorder with predisposition to acute myelogenous leukemia (FPD/AML), which is characterized by thrombocytopenia, abnormal platelet function, and propensity to myeloid malignancies. We identified a novel mutation in the AML1 gene in an FPD/AML pedigree characterized by a single nucleotide deletion that generates a frameshift and premature chain termination (Pro218fs-Ter225). Both wild-type and mutant transcripts were expressed in affected individuals by allele-specific reverse transcriptase-polymerase chain reaction (RT-PCR). Thrombopoietin (TPO) binds to the Mpl receptor and is the major regulator of megakaryopoiesis. To explore the mechanisms underlying thrombocytopenia, we studied the TPO/Mpl pathway in this newly identified pedigree. TPO levels were mildly to moderately elevated. On flow cytometry and immunoblotting, Mpl receptor expression was decreased and TPO-induced signaling was impaired. While no mutations were identified in the MPL gene by sequence analysis, low MPL mRNA levels were found, suggesting decreased gene expression. Of particular interest, several AML1-binding motifs are present in the MPL promoter, suggesting MPL is an AML1 target. In conclusion, we identified a C-terminal AML1 mutation that leads to a decrease in Mpl receptor expression, providing a potential explanation for thrombocytopenia in this FPD/AML pedigree. (Blood. 2005;105:4664-4670)
Introduction
Familial platelet disorder with predisposition to acute myelogenous leukemia (FPD/AML) is an autosomal dominant disorder characterized by moderate thrombocytopenia, a defect in platelet function, and propensity to develop myeloid malignancy.1 Germ-line heterozygous mutations in the hematopoietic transcription factor AML1, also known as RUNX1 and CBFA2, have been identified in 12 pedigrees reported so far, including missense, frameshift, and nonsense mutations and a large intragenic deletion.2-6 AML1 is the DNA-binding subunit of the core binding factor (CBF) transcription complex. Heterodimerization with the non-DNA-binding subunit, CBFβ, increases the affinity of AML1 to DNA and protects it from proteolytic degradation.7,8 AML1 includes a runt homology domain (RHD), which mediates DNA binding and heterodimerization with CBFβ, and a carboxy (C)-terminal domain responsible for transcriptional activation.9 The AML1/CBFβ complex regulates the expression of genes specific to hematopoiesis, including several cytokines and their receptors, such as granulocyte macrophage colony-stimulating factor, interleukin-3, and macrophage colony-stimulating factor receptor.7 This transcription factor is essential for the establishment of definitive hematopoiesis, as demonstrated in AML1-/- mice, which show a complete absence of fetal liver hematopoiesis and die during embryonic development, precluding analysis of the effects of AML1 in later stages of blood-cell development.10 The role of this transcription factor in platelet production and function was first revealed by the phenotype of patients with FPD/AML. Moreover, although early studies failed to show platelet defects in AML1+/- mice, recently a 15% reduction in platelet counts has been found, mimicking the human platelet disorder.11 However, the mechanisms by which AML1 facilitates platelet production remain to be clarified. Patients with FPD/AML show a decrease in megakaryocyte colony number and size, reflecting impaired megakaryopoiesis.2 Recent data show that AML1 expression is up-regulated in cells induced to differentiate along the megakaryocytic lineage and down-regulated in erythroid progenitors, suggesting it participates in megakaryocyte lineage commitment and divergence from the erythroid pathway.12 In addition, biallelic conditional deletion of AML1 in hematopoietic cells of adult mice leads to a partial arrest in megakaryocyte differentiation.13 FPD/AML is a rare disorder. Analysis of human samples provides a unique opportunity to investigate the mechanisms by which AML1 influences platelet production.
Thrombopoietin (TPO) is the major regulator of megakaryopoiesis. It stimulates the proliferation of progenitors committed to the megakaryocyte lineage and the maturation and endomitosis of megakaryocytes through binding to the Mpl receptor.14 Signaling events triggered by TPO include tyrosine phosphorylation and activation of several substrates, including the Janus kinase/signal transducer and activator of transcription (JAK/STAT), mitogen-activated protein kinase (MAPK), and phosphatidylinositol-3 kinase (PI3K) pathways.15,16 Analysis of Baf3 cells shows that the biologic response to TPO is dependent on the cell surface density of Mpl receptors, suggesting there is a threshold effect for the activation of downstream signaling pathways.17 Considering the key role of TPO and its receptor in megakaryopoiesis, we sought to determine whether abnormalities in the TPO/Mpl pathway contribute to the pathogenesis of thrombocytopenia and impaired megakaryopoiesis found in FPD/AML. In the present study, we describe a novel mutation in the AML1 gene that leads to a decrease in Mpl receptor expression in a pedigree with this platelet disorder. This defect provides a potential explanation for thrombocytopenia in affected family members. In addition, the mechanisms underlying low Mpl levels are explored.
Patients, materials, and methods
Patients
Members of a family with inherited thrombocytopenia were included as study subjects. The study was approved by the Instituto de Investigaciones Médicas Alfredo Lanari (IDIM A. Lanari) Institutional Review Board, and written informed consent was obtained from patients, in accordance with the Declaration of Helsinki.
Laboratory studies
Platelet counts were determined by optical microscopy in a Neubauer chamber. White and red blood-cell counts and mean platelet volume (MPV) were measured in an automated cell counter (Beckman Coulter, Miami, FL). Platelet-rich plasma (PRP) was prepared by centrifugation at 200g for 10 minutes, and platelet aggregation with adenosine diphosphate (ADP), 2 μM; epinephrine, 1 μM; collagen, 4 μg/mL; and arachidonic acid, 1 mM (Biopool, Ventura, CA) was evaluated by the turbidimetric method of Born18 using a lumiaggregometer (Chrono-log, Havertown, PA). Platelet membrane glycoproteins were analyzed on a FACScan flow cytometer (Becton Dickinson, San Jose, CA) after incubation of PRP with monoclonal antibodies to glycoproteins IIIa (CD61), IX (CD42a) (Becton Dickinson), and Ib (CD42b) (Beckman Coulter) for 30 minutes at 4°C.
Sequence analysis of AML1 and MPL genes
DNA was extracted from peripheral blood leukocytes by standard procedures. The entire coding regions of hAML1/CBFA2 and hMPL were amplified from gDNA using the primer pairs detailed in Table 1 at a concentration of 20 pmol/μL. Primers were designed to include the entire exons plus flanking exon/intron splice junction boundaries. The amplified fragments were separated in a 1.0% TAE (40 mM Tris [tris(hydroxymethyl) aminomethane]-acetate, 1 mM EDTA [ethylenediaminetetraacetic acid]) agarose gel and purified using the QIAquick Gel Extraction Kit from QIAgen Sciences (Valencia, CA) and were sequenced using the respective forward (F) or reverse (R) primer at a concentration of 2 pmol/μL for fluorescent labeling and analysis on an ABI 3100 Genetic Analyzer (Applied Biosystems, Foster City, CA). Sequencing results were compared with the National Center for Biotechnology Information (NCBI) nucleotide database. For AML1: locus NM_001754 (exons 1-6, 7b, and 8) and locus D43967 (exon 7a). For MPL: locus NM_005373.1. Any heterozygous mutations were confirmed by repeat sequencing.
Primers for AML1 and MPL sequence analysis
Exon . | Sequence . |
|---|---|
| hAML1/CBFA2 primers | |
| 1F | TGACATCACTTAAGTCACATGATTG |
| 1R | CGAGGCATCTCTGCACCGAGGTGA |
| 2F | TGACAGATATTCAGTATTAGCTAG |
| 2R | CAAGTTATACATAGAGATACATAG |
| 3F | CTGAACGTGTATGTTGGTCTCC |
| 3R | TGGCCGCTGCCCTCGCGGATCTC |
| 4F | CATTGCTATTCCTCTGCAACCTA |
| 4R | AAGAATGTTAAGACAGACCGAGTT |
| 5F | ACAGATATGTTCAGGCCACCAAC |
| 5R | GGTTCTAACATATGATTCAGTCAGC |
| 6F | GGCATATCTCTAGCGAGTCTATGTT |
| 6R | CAGAGCTCCTCGTATCCTCTGTA |
| 7aF | GGAATGCATTCGCGGCTCTATA |
| 7aR | TGTGTGACTTGGAGAGGACCGATG |
| 7bF | CAACAGAGGCAGATACTTGGACT |
| 7bR | CTTCATGCACCTCTAGTCTCCTG |
| 8F | CCTGACCTACAGCGAGATCCTG |
| 8R | AGCAGTAGCATCCTGGGTGGCTTC |
| hMPL primers | |
| 1F | CTCTTCCTGGGCATAGGTGA |
| 1R | GGGGCTGTATCTGACAGGAA |
| 2F | GGACTCAGCTAAGTGCAGGG |
| 2R | CCCCTTCCACATAAACATGC |
| 3F | GGAGCTGGACTAGGGGCAG |
| 3R | AGGTCTGGGTCCTCAGGG |
| 4F | TGGGGCAAGATTGAAGGTAG |
| 4R | CCAGAGGCTGAGCCATAGAC |
| 5F | TAGCCCAGGCTTCCCTAA |
| 5R | TCAGCTGACAGGCAGACCTA |
| 6F | TTTTTCTGCAAGATTGTGGC |
| 6R | TGAACACCCTATACAGTAGGGGC |
| 7F | ACAGGGTCAGATTCAGTGGG |
| 7R | TTGGGATTAGTCTCTGAGGCA |
| 8F | GGATCCCCTGCGTAGTGAG |
| 8R | GCCTTGTGCACAGAAGGACT |
| 9F | TCTTTGTGGGAATCTCCGAC |
| 9R | AGGCGCTGTGCGGCTTGGT |
| 10F | GACGGAGATCTGGGGTCAC |
| 10R | CCGAACTCTGACCCTTTTTG |
| 11F | ATCCAGTACCAGGCAGGGTT |
| 11R | GCCCAACTTTATTGCCTTGA |
| 12F | AGGGAACTGGGAGTGAGGAG |
| 12R | AGGCACTACCCCAGCACTAC |
Exon . | Sequence . |
|---|---|
| hAML1/CBFA2 primers | |
| 1F | TGACATCACTTAAGTCACATGATTG |
| 1R | CGAGGCATCTCTGCACCGAGGTGA |
| 2F | TGACAGATATTCAGTATTAGCTAG |
| 2R | CAAGTTATACATAGAGATACATAG |
| 3F | CTGAACGTGTATGTTGGTCTCC |
| 3R | TGGCCGCTGCCCTCGCGGATCTC |
| 4F | CATTGCTATTCCTCTGCAACCTA |
| 4R | AAGAATGTTAAGACAGACCGAGTT |
| 5F | ACAGATATGTTCAGGCCACCAAC |
| 5R | GGTTCTAACATATGATTCAGTCAGC |
| 6F | GGCATATCTCTAGCGAGTCTATGTT |
| 6R | CAGAGCTCCTCGTATCCTCTGTA |
| 7aF | GGAATGCATTCGCGGCTCTATA |
| 7aR | TGTGTGACTTGGAGAGGACCGATG |
| 7bF | CAACAGAGGCAGATACTTGGACT |
| 7bR | CTTCATGCACCTCTAGTCTCCTG |
| 8F | CCTGACCTACAGCGAGATCCTG |
| 8R | AGCAGTAGCATCCTGGGTGGCTTC |
| hMPL primers | |
| 1F | CTCTTCCTGGGCATAGGTGA |
| 1R | GGGGCTGTATCTGACAGGAA |
| 2F | GGACTCAGCTAAGTGCAGGG |
| 2R | CCCCTTCCACATAAACATGC |
| 3F | GGAGCTGGACTAGGGGCAG |
| 3R | AGGTCTGGGTCCTCAGGG |
| 4F | TGGGGCAAGATTGAAGGTAG |
| 4R | CCAGAGGCTGAGCCATAGAC |
| 5F | TAGCCCAGGCTTCCCTAA |
| 5R | TCAGCTGACAGGCAGACCTA |
| 6F | TTTTTCTGCAAGATTGTGGC |
| 6R | TGAACACCCTATACAGTAGGGGC |
| 7F | ACAGGGTCAGATTCAGTGGG |
| 7R | TTGGGATTAGTCTCTGAGGCA |
| 8F | GGATCCCCTGCGTAGTGAG |
| 8R | GCCTTGTGCACAGAAGGACT |
| 9F | TCTTTGTGGGAATCTCCGAC |
| 9R | AGGCGCTGTGCGGCTTGGT |
| 10F | GACGGAGATCTGGGGTCAC |
| 10R | CCGAACTCTGACCCTTTTTG |
| 11F | ATCCAGTACCAGGCAGGGTT |
| 11R | GCCCAACTTTATTGCCTTGA |
| 12F | AGGGAACTGGGAGTGAGGAG |
| 12R | AGGCACTACCCCAGCACTAC |
Reverse transcriptase-polymerase chain reaction (RT-PCR) amplification of AML1 with allele-specific primers
We designed 2 reverse AML1 primers in exon 6, spanning the mutation, with variation in their 3′ end such that each was complementary to the wild-type (WT), 5′-AGGGTTGGGCGTGGGGGC-3′ (nt 2244 to 2227, GenBank accession no. D43968), or the mutant (M), 5′-GAGGGTTGGGCGTGGGGC-3′ (nt 2245 to 2227), allele and a third F primer in exon 3 common to both alleles, 5′-GCTGGTGCGCACCGACAG-3′ (nt 1761 to 1778). The polymerase chain reaction (PCR) protocol was as follows: 1 μL platelet cDNA was mixed in 2 tubes with 1 μM of each WT and F primer in the first tube and 1 μM of each M and F primer in the second one in a total volume of 25 μL PCR buffer containing 0.2 mM deoxyribonucleoside triphosphate (dNTP), 1 unit Taq DNA polymerase (Life Technologies, Bethesda, MD), and 1.5 mM MgCl2. The reaction was performed in a thermal cycler (Biometra UNO-Thermoblock; BIOTRON, Göttingen, Germany) for 30 cycles (94°C for 1 minute, 75°C for 1 minute, 72°C for 30 seconds, each), preceded by denaturation at 94°C for 3 minutes and followed by incubation at 72°C for 5 minutes. The amplified product was analyzed by 2% agarose gel electrophoresis and ethidium bromide staining.
Analysis of platelet surface Mpl expression by flow cytometry
Platelets were pelleted from PRP, washed twice with phosphate-buffered saline (PBS), bovine serum albumin (BSA) 0.5%, and sodium citrate 0.6% and resuspended in a modified HEPES (N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid)-Tyrode buffer (137 mM NaCl, 2.7 mM KCl, 11.9 mM NaHCO3, 0.42 mM NaH2PO4, 1 mM MgCl2, 556 mM glucose, 5 mM HEPES, 1 mM CaCl2, pH 7.35). A total of 2 × 106 platelets were incubated with 10 μg/mL recombinant anti-human Mpl polyclonal rabbit immunoglobulin G (IgG) (kindly provided by Kirin Brewery, Tokyo, Japan) or normal rabbit IgG as isotype control (Santa Cruz Biotechnology, Santa Cruz, CA) during 30 minutes at 4°C. Platelets were washed and incubated with antirabbit fluorescein isothiocyanate (FITC)-conjugated F(ab′)2 fragment (Dako, Carpinteria, CA), 1:5 dilution, and CD41 phycoerythrin (PE)-conjugated antibody (Beckman Coulter) during 30 minutes at 4°C. Then, CD41+ events were collected and analyzed on a flow cytometer.
Western blot analysis of platelet Mpl expression
Platelet-rich plasma was filtered through a leukocyte reduction filter (Purecell PL; Pall Biomedical Products, East Hills, NY), and red blood cells were lysed by incubation with 8.6 g/L NH4Cl. Platelets were pelleted, washed twice with PBS containing EDTA 2 mM, and 2 × 106 platelets per microliter were lysed in lysis buffer (20 mM HEPES, 5 mM KCl, 5 mM MgCl2, 10% glycerol, 1 mM EDTA, 1% Nonidet P-40 [NP-40], 1% sodium dodecyl sulfate [SDS]) supplemented with 1 mM phenylmethylsulfonyl fluoride (PMSF), 5 μg/mL trypsin inhibitor, and 500 μg/mL aprotinin. After centrifugation at 14 000g for 10 minutes at 4°C, the supernatant was collected and 20 μg protein was loaded per lane, resolved by SDS-polyacrylamide gel electrophoresis (SDS-PAGE) on an 8% gel and electrophoretically transferred to nitrocellulose membranes (Amersham Pharmacia Biotech, Buckinghamshire, United Kingdom) at 15 V for 30 minutes. After blocking of nonspecific binding sites with TBST (10 mM Tris, 150 mM sodium chloride, 1% Tween 20) and 1% BSA, membranes were incubated with 1 μg/mL recombinant anti-human Mpl polyclonal rabbit IgG (Kirin Brewery) in TBST supplemented with 0.5% BSA at room temperature for 1 hour, washed, and incubated with horseradish peroxidase (HRP)-linked anti-rabbit IgG (Amersham Pharmacia Biotech), at a dilution of 1:5000, in TBST with 0.5% BSA at room temperature for 1 hour. After washing, detection was performed by enhanced chemiluminescence (ECL; Amersham Pharmacia Biotech). To assess protein loading, membranes were reprobed with an anti-β3 integrin murine monoclonal antibody (kindly provided by Dr T. Kunicki, The Scripps Research Institute, La Jolla, CA) and HRP-linked antimouse antibody (Sigma, St Louis, MO). After scanning and densitometric analysis, a ratio between Mpl and β3 integrin was calculated and expressed as percentage of healthy controls.
TPO-induced tyrosine phosphorylation of platelet proteins
Indomethacin, 0.042 M, (Sigma) was added to PRP, and washed platelets were prepared as for flow cytometry at a concentration of 106/μL. Half the sample remained unstimulated while half was stimulated with recombinant human TPO (R&D Systems, Minneapolis, MN), 100 ng/mL at 37°C for 10 minutes, and lysed in lysis buffer (20 mM Tris, 137 mM NaCl, 5 mM MgCl2, 10% glycerol, 1 mM EDTA, 1% NP-40, 10% SDS, pH 7.5) supplemented with 50 mM sodium fluoride, 2 mM sodium vanadate, 1 mM PMSF, 2 μg/mL aprotinin, and 2 μg/mL leupeptin. After centrifugation at 14 000g for 10 minutes at 4°C, supernatants were collected and 35 μg of platelet lysates per lane were separated by SDS-PAGE (7.5% polyacrylamide gel) and transferred to nitrocellulose membranes. After blocking with TBST and 1% blocking reagent (Amersham Pharmacia Biotech), membranes were incubated with antiphosphotyrosine HRP-conjugated antibody (Amersham Pharmacia Biotech), 1:1000 dilution, in TBST with 1% blocking reagent at room temperature for 1 hour. Detection was performed by ECL.
Semiquantitative RT-PCR analysis of platelet MPL transcripts
Platelet-rich plasma was filtered through a leukocyte reduction filter, 5 × 109 platelets were lysed in Trizol (Life Technologies) after addition of 0.042 M indomethacin, and RNA was isolated. First-strand cDNA synthesis was carried out using 1 μg RNA and random primers with the SuperScript preamplification system (Life Technologies). Amplified MPL transcripts were normalized by comparison with glyceraldehyde 3-phosphate dehydrogenase (GAPDH) amplified under identical conditions. The reaction mixture contained 1 μL sequential dilutions of cDNA, 0.2 mM dNTP, 1 unit Taq DNA polymerase, 1.5 mM MgCl2, 0.80 ηM primers for MPL (F 5′-GCACACTACAGGAGACTGAGGCAT-3′ [nt 1555 to 1578, GenBank accession no. M90102] and reverse 5′-TCAAGGCTGCTGCCAATAGCTTAGTGGT-3′ [nt 1881 to 1908]), 1.2 μM primers for GAPDH (F 5′-TGCACCACCAACTGCTT-3′ and R 5′-TACTCCTTGGAGGCCAT-3′), and PCR buffer in a final volume of 25 μL. Amplification was carried out in a thermal cycler for 29 cycles (94°C for 30 seconds, 60°C for 30 seconds, 72°C for 1 minute, each), preceded by denaturation at 94°C for 3 minutes and followed by extension at 72°C for 5 minutes. The PCR products were electrophoresed in 2% agarose gel, ethidium bromide stained, and a ratio between MPL and GAPDH calculated by densitometry. Products were analyzed in the linear range of amplification.
Plasma thrombopoietin levels
Thrombopoietin was measured by enzyme-linked immunosorbent assay (Human TPO Quantikine kit; R&D Systems) in plasma, which was prepared by sequential centrifugation at 2000g for 30 minutes and 10 000g for 10 minutes at 4°C.
Statistical analysis
Comparison between patients and controls was performed using the Mann-Whitney rank sum test. For statistical analysis, TPO values ranging from 0 to 50 pg/mL, 51 to 100 pg/mL, 101 to 150 pg/mL, and 151 to 200 pg/mL were given a rank of 1, 2, 3, and 4, respectively.
Results
Medical history and platelet features
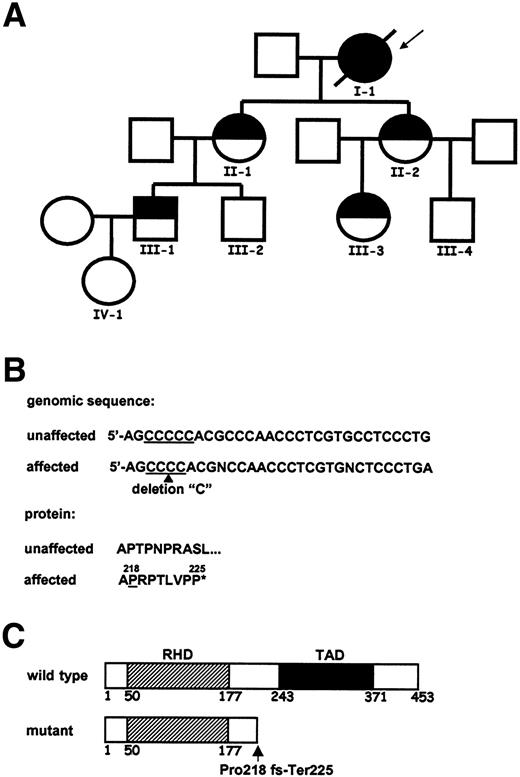
The family pedigree is shown in Figure 1A. The proband (I-1), who had a 7-year history of presumed immune thrombocytopenic purpura, developed chronic myelomonocytic leukemia (CMMoL) at age 54 and died of central nervous system bleeding. A cytogenetic study showed a normal karyotype while 3 signals were detected in 50% of metaphases by fluorescence in situ hybridization (FISH) with a whole chromosome 5 probe. Four of 9 family members in 4 generations were found to have mild to moderate thrombocytopenia, consistent with an autosomal dominant pattern of inheritance. Clinical and laboratory features of affected family members are shown in Table 2. Red and white blood-cell counts were normal, except for mild iron deficiency anemia in patient II-1. Expression of platelet membrane glycoproteins IIIa, Ib, and IX was normal. Affected individuals suffer from a mild to moderate bleeding diathesis consisting of easy bruising, menorrhagia, gingival bleeding, and prolonged bleeding after surgery and childbirth. Patients II-2 and III-3 underwent bone marrow examination that revealed an increased fraction of immature, hypolobulated megakaryocytes. Cytogenetic analysis showed 46,XX,del(11)(q21)[3]/46,XX[9] in patient II-2 while no abnormalities were found in patient III-3.
Clinical and laboratory features of patients with FPD/AML
. | . | Platelet count, × 109/L . | . | Aggregation, %† . | . | . | . | Bone marrow morphology . | . | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient . | Age, y . | . | MPV, fL* . | ADP . | Epi . | AA . | Col . | . | Cytogenetics . | |||
| I-1 | 56‡ | 2 | ND | ND | ND | ND | ND | CMMoL | 46,XX§ | |||
| II-1 | 39 | 145 | 7.4 | 42 | 18 | 57 | 20 | ND | ND | |||
| II-2 | 38 | 50 | 8.1 | 23 | 0 | 26 | 0 | Immature MK | 46,XX,del(11)(q21)[3]/46,XX[9] | |||
| III-1 | 19 | 140 | 6.3 | 30 | 15 | 0 | 13 | ND | ND | |||
| III-3 | 15 | 90 | 7.7 | 27 | 19 | 22 | 21 | Immature MK | 46,XX | |||
. | . | Platelet count, × 109/L . | . | Aggregation, %† . | . | . | . | Bone marrow morphology . | . | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient . | Age, y . | . | MPV, fL* . | ADP . | Epi . | AA . | Col . | . | Cytogenetics . | |||
| I-1 | 56‡ | 2 | ND | ND | ND | ND | ND | CMMoL | 46,XX§ | |||
| II-1 | 39 | 145 | 7.4 | 42 | 18 | 57 | 20 | ND | ND | |||
| II-2 | 38 | 50 | 8.1 | 23 | 0 | 26 | 0 | Immature MK | 46,XX,del(11)(q21)[3]/46,XX[9] | |||
| III-1 | 19 | 140 | 6.3 | 30 | 15 | 0 | 13 | ND | ND | |||
| III-3 | 15 | 90 | 7.7 | 27 | 19 | 22 | 21 | Immature MK | 46,XX | |||
MPV indicates mean platelet volume; Epi, epinephrine; AA, arachidonic acid; Col, collagen; ND, not done; MK, megakaryocytes.
Mean ± SD MPV in healthy controls (n = 33) was 8.32 ± 1.02 fL.
Mean ± SD platelet aggregation in response to 2 μM ADP, 1 μM Epi, 1 mM AA, and 4 μg/mL Col in healthy controls (n = 60) was 66% ± 6%, 75% ± 3%, 66% ± 5%, and 70% ± 5%, respectively.
Age at death.
FISH analysis with a whole chromosome 5 probe revealed 3 signals in 50% of metaphases.
Sequence analysis of the AML1 and MPL genes
Sequence analysis of the AML1 gene revealed a heterozygous single nucleotide (C) deletion located in exon 6, corresponding to position 2232 of AML1b cDNA (GenBank accession no. D43968), that creates a frameshift after amino acid Pro218 and results in a premature termination codon 22 nucleotides downstream (Figure 1B-C). This mutation was present in genomic DNA from 5 affected individuals but not in unaffected family members. In contrast, no mutations were found in the MPL gene in 2 affected individuals.
Family pedigree and sequence analysis of the AML1 gene. (A) The family pedigree is shown. Half-filled symbols indicate thrombocytopenia; the closed symbol, the individual who developed CMMoL; and open figures, unaffected family members. The index patient is indicated by the arrow. (B) Genomic and protein AML1 sequence in healthy and affected individuals. A single nucleotide deletion (arrowhead) within 5 consecutive C's generates a frameshift at amino acid position 218 (underlined) and premature chain termination (*). (C) Schematic representation of the wild-type and mutant truncated AML1 protein. The predicted protein includes an intact runt homology domain (RHD) (amino acids 50 to 177) but lacks a transactivation domain (TAD) (amino acids 243 to 371). The position of the Pro218fs-Ter225 mutation is indicated by the arrow.
Family pedigree and sequence analysis of the AML1 gene. (A) The family pedigree is shown. Half-filled symbols indicate thrombocytopenia; the closed symbol, the individual who developed CMMoL; and open figures, unaffected family members. The index patient is indicated by the arrow. (B) Genomic and protein AML1 sequence in healthy and affected individuals. A single nucleotide deletion (arrowhead) within 5 consecutive C's generates a frameshift at amino acid position 218 (underlined) and premature chain termination (*). (C) Schematic representation of the wild-type and mutant truncated AML1 protein. The predicted protein includes an intact runt homology domain (RHD) (amino acids 50 to 177) but lacks a transactivation domain (TAD) (amino acids 243 to 371). The position of the Pro218fs-Ter225 mutation is indicated by the arrow.
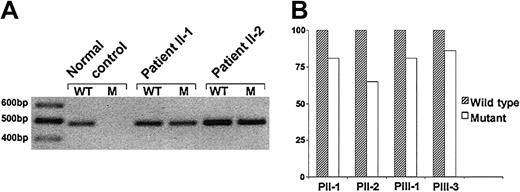
Both wild-type and mutant AML1 transcripts are expressed in patients
To distinguish between WT and M AML1 transcripts, we performed RT-PCR amplification with allele-specific primers. While only the WT mRNA was detected in controls (n = 6), both WT and M transcripts were expressed in platelets from affected individuals (Figure 2A). To determine the relative levels of WT and M mRNA, serial cDNA dilutions were amplified and the intensity of each band was quantitated by densitometry under nonlimiting PCR conditions. Mutant transcript levels were slightly lower compared with WT expression, as follows: patient II-1, 81%; II-2, 65%; III-1, 81%; and III-3, 86% (Figure 2B).
Platelet Mpl expression is reduced by flow cytometry and immunoblotting
Flow cytometry analysis with an anti-Mpl antibody of platelets from healthy subjects revealed weak but clearly detectable staining, as previously reported.19 In contrast, Mpl expression on the platelet surface was significantly reduced or scarcely detectable in the 4 patients studied, as shown in Figure 3. The ratio between mean fluorescence intensity obtained with the Mpl antibody and the isotype control was 1.04 plus or minus 0.16 in patients compared with 1.70 plus or minus 0.27 in controls (n = 10) (P = .004). To explore whether the decrease in Mpl surface levels correlated with a decrease in total Mpl protein, we performed immunoblotting of platelet lysates with an anti-Mpl antibody and normalized its expression with respect to β3 integrin, which was expressed at normal levels by flow cytometry. Reduced Mpl receptor was found in patients, as follows: II-1, 50%; II-2, 17%; III-1, 10%; and III-3, 18%; with a mean of 23.75% (P = .01) (Figure 4).
RT-PCR amplification of AML1 with allele-specific primers. Platelet cDNA was amplified in 2 tubes with an R primer complementary to either the WT (in the first tube) or the M (in the second) AML1 allele and a common F primer yielding a 484-base pair (bp) product, which was analyzed by ethidium bromide-stained 2% agarose gel electrophoresis. (A) Representative RT-PCR analysis. Both WT and M transcripts are expressed in patients while only the normal allele is detected in the control. A 100-bp DNA ladder is shown on the left lane. (B) Comparison of WT and M mRNA levels. Expression of M relative to WT mRNA, set as 100%, is indicated by the bars. Results represent the average of 2 PCR assays performed using serial cDNA dilutions.
RT-PCR amplification of AML1 with allele-specific primers. Platelet cDNA was amplified in 2 tubes with an R primer complementary to either the WT (in the first tube) or the M (in the second) AML1 allele and a common F primer yielding a 484-base pair (bp) product, which was analyzed by ethidium bromide-stained 2% agarose gel electrophoresis. (A) Representative RT-PCR analysis. Both WT and M transcripts are expressed in patients while only the normal allele is detected in the control. A 100-bp DNA ladder is shown on the left lane. (B) Comparison of WT and M mRNA levels. Expression of M relative to WT mRNA, set as 100%, is indicated by the bars. Results represent the average of 2 PCR assays performed using serial cDNA dilutions.
TPO-induced tyrosine phosphorylation of platelet proteins is impaired
After stimulation of normal platelets with TPO, we found a prominent increase in tyrosine phosphorylation of proteins of relative molecular weight 95 kDa. In contrast, stimulation of platelets from patients II-2 and III-3 failed to induce phosphorylation of proteins, as shown in Figure 5, while a faint response was found in patient III-1. On the other hand, phosphorylation was only slightly diminished in patient II-1, who showed a milder reduction in Mpl levels by flow cytometry and immunoblotting.
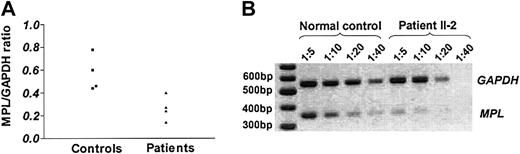
Expression of MPL transcripts is decreased in platelets
To investigate the mechanisms underlying low Mpl expression, we studied platelet MPL mRNA levels by semiquantitative RT-PCR with primers specific to the Mpl-P isoform, which is the predominant full-length RNA species. As illustrated in Figure 6, reduced MPL transcripts were found in affected individuals. The mean MPL/GAPDH ratio in patients was 0.26 plus or minus 0.1 (II-1, 0.40; II-2, 0.14; III-1, 0.24; and III-3, 0.27) compared with 0.57 plus or minus 0.15 in controls (P = .02).
Analysis of platelet surface Mpl expression by flow cytometry. Washed platelets were incubated with anti-human Mpl rabbit IgG or normal rabbit IgG as isotype control. Binding was detected by labeling with FITC-conjugated anti-rabbit F(ab′)2 fragment and fluorescence-activated cell sorter (FACS) analysis of CD41-gated cells. Gray-shaded histograms represent staining with the isotype control whereas solid black lines indicate staining with the Mpl antibody. Shown are the results obtained in healthy subjects (A,D) and patients with FPD/AML, who reveal reduced (B) or barely detectable (C,E,F) Mpl surface expression. Samples were analyzed in duplicate with similar findings.
Analysis of platelet surface Mpl expression by flow cytometry. Washed platelets were incubated with anti-human Mpl rabbit IgG or normal rabbit IgG as isotype control. Binding was detected by labeling with FITC-conjugated anti-rabbit F(ab′)2 fragment and fluorescence-activated cell sorter (FACS) analysis of CD41-gated cells. Gray-shaded histograms represent staining with the isotype control whereas solid black lines indicate staining with the Mpl antibody. Shown are the results obtained in healthy subjects (A,D) and patients with FPD/AML, who reveal reduced (B) or barely detectable (C,E,F) Mpl surface expression. Samples were analyzed in duplicate with similar findings.
TPO levels in affected individuals
Plasma TPO is cleared by binding to the Mpl receptor followed by internalization and degradation.20 TPO levels were nondetectable in 12 of 17 control subjects (detection limit of the assay, 7.45 pg/mL) and ranged from 12.9 to 32.1 pg/mL in the remaining 5. TPO values in patients were mildly to moderately elevated, as follows: patient II-1, 55.7 pg/mL; II-2, 200 pg/mL; III-1, 158 pg/mL; and III-3, 99.7 pg/mL (P = .002).
Analysis of platelet Mpl levels by Western blot. Platelet lysates (20 μg per lane) were separated by 8% SDS-PAGE and immunoblotted with an anti-human Mpl antibody and an HRP-conjugated second antibody. Detection was carried out by chemiluminescence. To control for protein loading, membranes were reprobed with an anti-β3 integrin antibody. (A) Representative Western blot experiment shows the results of a healthy control (C) and patients (P), who reveal decreased Mpl levels. (B) Expression of Mpl relative to that of β3 integrin. Bars represent the ratio of Mpl to β3 integrin, which was calculated by densitometry and expressed as percentage of healthy controls (n = 6), set as 100%. Data represent the mean of 3 separate experiments.
Analysis of platelet Mpl levels by Western blot. Platelet lysates (20 μg per lane) were separated by 8% SDS-PAGE and immunoblotted with an anti-human Mpl antibody and an HRP-conjugated second antibody. Detection was carried out by chemiluminescence. To control for protein loading, membranes were reprobed with an anti-β3 integrin antibody. (A) Representative Western blot experiment shows the results of a healthy control (C) and patients (P), who reveal decreased Mpl levels. (B) Expression of Mpl relative to that of β3 integrin. Bars represent the ratio of Mpl to β3 integrin, which was calculated by densitometry and expressed as percentage of healthy controls (n = 6), set as 100%. Data represent the mean of 3 separate experiments.
Discussion
In this study we describe a novel mutation in the AML1 gene that leads to decreased Mpl receptor expression in a pedigree with FPD/AML. Affected individuals have mild to moderate thrombocytopenia and marked abnormalities in first- and second-wave platelet aggregation, as described for other FPD/AML patients.21 Propensity to develop acute myeloid leukemia and myelodysplastic syndrome is another feature of this platelet disorder, with a leukemic rate of approximately 35%.22 One individual in this newly identified pedigree developed CMMoL, which has not been previously described in FPD/AML. Several additional chromosomal abnormalities have been reported in FPD/AML patients who develop leukemia, including -7, +8, +21, 20q-, 5q-, and 11q-.1,2,4,5 FISH analysis with a chromosome 5 probe in our patient with CMMoL revealed an abnormal pattern although the underlying abnormality could not be further characterized. The finding of a cytogenetic del(11)(q21) without myelodysplastic features in another family member warrants close follow-up.
Induction of tyrosine phosphorylation of platelet proteins after stimulation with TPO. Platelets were unstimulated (-) or stimulated (+) with TPO, 100 ng/mL, followed by lysis and immunoblotting. Platelet proteins (35 μg) were loaded and separated on a 7.5% polyacrylamide gel. After protein transfer, membranes were incubated with an HRP-conjugated antiphosphotyrosine antibody followed by ECL detection. Stimulation of normal platelets (left lanes) with TPO led to phosphorylation of proteins of apparent molecular weight 95 kDa (arrow). Shown are the results of 2 affected family members (middle and right lanes) who fail to reveal TPO-mediated signaling. This experiment was performed in duplicate with similar results.
Induction of tyrosine phosphorylation of platelet proteins after stimulation with TPO. Platelets were unstimulated (-) or stimulated (+) with TPO, 100 ng/mL, followed by lysis and immunoblotting. Platelet proteins (35 μg) were loaded and separated on a 7.5% polyacrylamide gel. After protein transfer, membranes were incubated with an HRP-conjugated antiphosphotyrosine antibody followed by ECL detection. Stimulation of normal platelets (left lanes) with TPO led to phosphorylation of proteins of apparent molecular weight 95 kDa (arrow). Shown are the results of 2 affected family members (middle and right lanes) who fail to reveal TPO-mediated signaling. This experiment was performed in duplicate with similar results.
MPL transcript levels in platelets by semiquantitative RT-PCR.MPL mRNA was amplified from leukocyte-depleted platelets after reverse transcription with primers specific to the P isoform. Amplification of GAPDH was used as internal control. A ratio between them was calculated by densitometry after electrophoresis in 2% agarose gel and staining with ethidium bromide. (A) ▪ represents MPL/GAPDH ratio in healthy controls while ▴ indicates MPL/GAPDH ratio in patients. Results represent the average of 2 experiments. (B) Representative RT-PCR assay. MPL and GAPDH were amplified from sequential 1:5, 1:10, 1:20, and 1:40 cDNA dilutions from a healthy control and patient II-2, yielding 354-bp and 554-bp products, respectively. MPL transcripts are expressed at lower levels in the patient's sample. A 100-bp DNA ladder is shown on the left lane.
MPL transcript levels in platelets by semiquantitative RT-PCR.MPL mRNA was amplified from leukocyte-depleted platelets after reverse transcription with primers specific to the P isoform. Amplification of GAPDH was used as internal control. A ratio between them was calculated by densitometry after electrophoresis in 2% agarose gel and staining with ethidium bromide. (A) ▪ represents MPL/GAPDH ratio in healthy controls while ▴ indicates MPL/GAPDH ratio in patients. Results represent the average of 2 experiments. (B) Representative RT-PCR assay. MPL and GAPDH were amplified from sequential 1:5, 1:10, 1:20, and 1:40 cDNA dilutions from a healthy control and patient II-2, yielding 354-bp and 554-bp products, respectively. MPL transcripts are expressed at lower levels in the patient's sample. A 100-bp DNA ladder is shown on the left lane.
A novel heterozygous single base deletion in exon 6 of the AML1 gene, which results in a frameshift and premature chain termination, was found in 5 affected individuals. The predicted protein contains an intact RHD, which mediates DNAbinding and heterodimerization with CBFβ but lacks the C-terminal region responsible for transactivation. Most mutations identified in FPD/AML are clustered within the RHD.2-6 Besides the one described in this paper, so far only one familial C-terminal mutation has been reported.3 In addition, acquired RHD and C-terminal AML1 point mutations have been found in sporadic leukemia and myelodysplastic syndrome.23-25 Runt domain mutants show reduced DNA binding and transactivation potential in functional assays and, according to their ability to bind CBFβ, may cause transdominant inhibition of wild-type AML1 or act through haploinsufficiency.3,24,25 On the other hand, C-terminalAML1 mutants show normal or enhanced DNA binding and strongly repress wild-type AML1.25,26 FPD/AML pedigrees harboring AML1 dominant-negative mutations seem to carry a higher risk of leukemia than those acting via haploinsufficiency.3 Although the functional effects of this novel mutation were not explored, it would be expected to act as a dominant-negative inhibitor, in a similar fashion as other C-terminal mutants.
Most transcripts harboring premature termination codons are subjected to degradation by nonsense-mediated decay.27 Nonsense mutations might therefore act in vivo predominantly via haploinsufficiency rather than in a dominant-negative manner. By means of RT-PCR with allele-specific primers, we found that both mutant and wild-type alleles were expressed in platelets, with mutant mRNA levels slightly lower than that of wild-type. This finding suggests that a significant amount of the mutant transcript escapes nonsense-mediated decay, as recently reported for several nonsense mutations,27,28 and may result in the synthesis of truncated AML1 protein with potential dominant-negative activity.
To explore the mechanisms underlying thrombocytopenia, we studied the TPO/Mpl pathway and found a reduction in Mpl levels by both flow cytometry and immunoblotting. The decrease in Mpl levels was variable but was quite marked in 3 affected individuals (II-2, III-1, and III-3), who showed faint or absent TPO-induced phosphorylation of platelet proteins. However, for similar degrees of Mpl reduction, the severity of thrombocytopenia differed in these 3 patients. In contrast, the other patient (II-1) had a milder reduction in Mpl levels, slightly diminished response to TPO, and platelet counts at the lower limit of normal. It remains, at present, unclear what level of Mpl expression is required to maintain steady state megakaryopoiesis. Mpl knock-out mice (mpl-/-) display platelet counts 6% to 15% of normal and low numbers of megakaryocytes.29 Likewise, patients with congenital amegakaryocytic thrombocytopenia, which is caused by homozygous or compound heterozygous mutations in the MPL gene, are characterized by lack of functional Mpl, severe thombocytopenia, and progression to pancytopenia.30 On the other hand, mpl+/- mice do not develop thrombocytopenia although they do have a reduction in megakaryocyte colony formation in response to TPO. However, the binding of 125I-TPO to hematopoietic cells is not consistently decreased in mpl+/- mice, suggesting this model might not be useful to assess the effect of a 50% reduction in Mpl levels.29 Low Mpl expression found in this study may contribute to the pathogenesis of thrombocytopenia in this FPD/AML pedigree. However, other factors involved in platelet production may be reduced secondary to the AML1 defect. In this regard, decreased protein kinase C-θ (PKC-θ), which has been implicated in megakaryocyte differentiation,31 has been found in FPD/AML,6 providing another explanation for impaired platelet production.
To investigate the mechanisms underlying low Mpl expression, we sequenced the MPL gene and found no abnormalities, indicating that the reduction in Mpl levels was unlikely to be caused by a mutation in the MPL gene. Alternatively, we considered the possibility that TPO concentrations 1000- to 5000-fold above normal may lead to low Mpl levels due to increased receptor internalization.32,33 However, this mechanism may not explain the observed reduction in Mpl expression, because TPO levels were only mildly to moderately elevated in our patients. By means of semiquantitative RT-PCR, we found a decrease in MPL transcripts, suggesting decreased gene expression. The MPL gene is transcriptionally regulated by GATA-1 and Ets family members,34 both of which have been shown to directly interact with AML1.12,35 Furthermore, AML1 cooperates with GATA-1 in the activation of the megakaryocyte promoter αIIb integrin, which provides evidence for its role as a megakaryocytic transcription factor.12 We searched the MPL promoter (including a fragment extending to -905 relative to the transcriptional start, GenBank accession no. AH003655) for the presence of AML1-binding sites using the TRANSFAC database (web program TESS [Transcription Element Search System]36 ) and found 2 consensus (TGTGGT) and 1 variant (TGGGGT) motifs at positions -101, -688, and -756, respectively. The presence of AML1-binding sites in the upstream region of the MPL gene suggests that AML1 is likely to regulate MPL transcription, possibly through interaction with GATA-1 and Ets proteins. However, further studies assessing the functional relevance of these consensus motifs should be performed to definitively establish a role for AML1 in the regulation of MPL expression. In this setting, decreased MPL gene transcription secondary to AML1 loss of function represents a plausible explanation for low Mpl levels. Studying the response of the MPL promoter to wild-type and mutant AML1 by means of a reporter transactivation assay would be useful to test this hypothesis. In addition, analysis of other potential AML1 targets involved in platelet production and function may identify additional pathways dysregulated in FPD/AML.
Prepublished online as Blood First Edition Paper, March 1, 2005; DOI 10.1182/blood-2005-01-0050.
Supported by grants from the University of Buenos Aires (MO37, MO53), Agencia Nacional de Promoción Científica y Tecnológica (PICT 05-11229), and Fundación Pedro F. Mosoteguy.
An Inside Blood analysis of this article appears in the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Susana Laguna for participation in early stages of this study, Silvia García for helpful assistance with PCR analysis, and Irene Larripa for performing cytogenetic studies.




This feature is available to Subscribers Only
Sign In or Create an Account Close Modal