Abstract
Several studies have reported enhanced oxidative stress in patients with HIV infection. An important pathophysiologic consequence of increased oxidative stress is endogenous DNA damage, and the base excision repair pathway is the most important mechanism to withstand such deleterious effects. To investigate the role of base excision repair in HIV infection, we examined 7,8-dihydro-8-oxoguanine (8-oxoG) levels as a marker of oxidative DNA damage and DNA glycosylase activities in CD4+ and CD8+ T cells of HIV-infected patients and controls. These results showed that the HIV-infected patients, particularly those with advanced disease, had increased levels of 8-oxoG in CD4+ T cells and marked declines in DNA glycosylase activity for the repair of oxidative base lesions in these cells. In contrast, CD8+ T cells from HIV-infected patients, with 8-oxoG levels similar to those in healthy controls, showed enhanced capacity to repair oxidative DNA damage. Finally, highly active antiretroviral therapy induced increased glycosylase activity in CD4+ T cells and normalized 8-oxoG levels. This imbalance between the accumulation of oxidative DNA damage and the capacity to repair such lesions in CD4+ T cells may represent a previously unrecognized mechanism involved in the numerical and functional impairment of CD4+ T cells in patients with HIV infection. (Blood. 2005; 105:4730-4735)
Introduction
Highly reactive oxygen species (ROS) are formed as byproducts during a variety of biochemical reactions, and this steady state formation of pro-oxidants is normally balanced by a similar rate of consumption by antioxidants. Oxidative stress results from an imbalance between the formation and the neutralization of pro-oxidants, resulting in an accumulation of pro-oxidants with potentially harmful consequences.1 Enhanced oxidative stress has been implicated in the pathogenesis of several clinical disorders, such as heart and brain ischemic diseases, neurodegenerative disorders, and various autoimmune diseases, and it seems to be involved in carcinogenesis and aging.1-5 Several lines of evidence suggest that enhanced oxidative stress also plays a pathogenic role in HIV infection. Thus, a number of reports have found impaired antioxidant defense, particularly manifested by disturbed glutathione metabolism in HIV-infected patients.5-9 Moreover, enhanced oxidative stress may be involved in the pathogenesis of impaired T-cell responsiveness and enhanced T-cell apoptosis during HIV infection, and it may also play a role in the development of certain HIV-related clinical disorders, such as malignancies and HIV-related encephalopathy.5,10,11
An important pathophysiologic consequence of increased intracellular oxidative stress is endogenous DNA damage.12 Several types of oxidative DNA lesions have been reported, including strand breaks, baseless sugars (AP-sites), and oxidized base residues, with 7,8-dihydro-8-oxoguanine (8-oxoG) and 5-hydroxycytosine (5-ohC) representing the most frequent mutagenic base lesions.13-15 DNA repair mechanisms have evolved specifically to counteract the biologic effects of DNA damage. Of particular importance for the removal of oxidative damage is the base excision repair pathway, which is initiated by the action of DNA glycosylases removing different types of modified bases by cleavage of the N-glycosylic bond.16,17 Five DNA glycosylases for the removal of oxidative base residues—hNth1, hOgg1, Neil1, Neil2, and Neil3 (hFpg2)—have been cloned and characterized in human cells.18-28 hNth1, Neil1, and Neil2 remove oxidized pyrimidines such as 5-ohC, whereas hOgg1 removes oxidized purines such as 8-oxoG. However, Neil1 appears to be a backup function for hOgg1 for the removal of 8-oxoG. All 5 enzymes have been shown to remove cytotoxic imidazole ring-fragmented formamidopyrimidine (faPy) residues, which represent blocks to replication.
Based on the potential pathogenic role of enhanced oxidative stress in HIV infection, we examined 8-oxoG levels as a marker of oxidative DNA damage in relation to DNA glycosylase activity for the repair of oxidative damage in T-cell subsets from HIV-infected patients and healthy controls. We found increased levels of 8-oxoG in the DNA of CD4+ T cells from HIV-infected patients and reduced capacity for the repair of oxidized base residues in these cells.
Patients, materials, and methods
Patients and controls
Fifteen HIV-infected patients were consecutively recruited for the study (Table 1). They were clinically classified according to the revised criteria from the Centers for Disease Control and Prevention (CDC) in patients with AIDS (CDC group C, n = 7) and patients without AIDS (CDC group A+B, n = 8). Patients with ongoing acute infection or exacerbation of chronic infection at the time of blood collection were not included. Eleven of the patients received antiretroviral therapy with nucleoside analog(s), but, except for one subgroup (see “DNA glycosylase activity during HAART”), none received highly active antiretroviral therapy (HAART). None had initiated or changed therapy during the past 5 months. None had abnormal liver or kidney function, were abusing drugs or alcohol, or were regularly taking medication except for nucleoside analog(s), as described. Controls in the study were 13 healthy HIV-seronegative sex- and age-matched healthy blood donors (Table 1). Approval was obtained from the National Hospital in Oslo institutional review board for these studies. Informed consent was provided according to the Declaration of Helsinki.
Characteristics of the study group
. | HIV-infected patients . | AIDS patients . | Controls . |
|---|---|---|---|
| No. subjects | 8 | 7 | 13 |
| Median age, y (range) | 38 (32-52) | 37 (34-56) | 37 (29-61) |
| No. men/no. women | 6/2 | 5/2 | 9/4 |
| No. CD4+ T cells, × 106/L (range) | 280 (95-430) | 45 (10-110) | 760 (540-980) |
| No. CD8+ T cells, × 106/L (range) | 710 (410-1170) | 280 (110-430) | 400 (210-550) |
| TNF-α, pg/mL (range) | 25 (12-37) | 65 (40-98) | 8 (0-12) |
| HIV RNA copies/mL plasma, × 103 (range) | 44.2 (22.9-108.6) | 510.9 (210.0-1200.0) | NA |
. | HIV-infected patients . | AIDS patients . | Controls . |
|---|---|---|---|
| No. subjects | 8 | 7 | 13 |
| Median age, y (range) | 38 (32-52) | 37 (34-56) | 37 (29-61) |
| No. men/no. women | 6/2 | 5/2 | 9/4 |
| No. CD4+ T cells, × 106/L (range) | 280 (95-430) | 45 (10-110) | 760 (540-980) |
| No. CD8+ T cells, × 106/L (range) | 710 (410-1170) | 280 (110-430) | 400 (210-550) |
| TNF-α, pg/mL (range) | 25 (12-37) | 65 (40-98) | 8 (0-12) |
| HIV RNA copies/mL plasma, × 103 (range) | 44.2 (22.9-108.6) | 510.9 (210.0-1200.0) | NA |
Data are given as medians and as 25th to 75th percentiles if not otherwise stated. T-cell subset counts were analyzed in peripheral blood and TNF-α levels in plasma. NA indicates not applicable.
Isolation of cells
Peripheral blood mononuclear cells (PBMCs) were obtained from heparinized blood by Isopaque-Ficoll (Lymphoprep; Nycomed, Oslo, Norway) gradient centrifugation within 45 minutes, and further positive selection of CD4+ and CD8+ T cells was made at 4°C, as previously described.7 Briefly, PBMCs were mixed with Dynabeads (Dynal, Oslo, Norway) coated with appropriate antibodies (anti-CD4, Dynabeads M-450 CD4; anti-CD8, Dynabeads M-450 CD8) at a cell-to-bead ratio of 1:10. The mixture was incubated in a test tube on a rocking platform for 30 minutes, and rosetting cells were isolated by application of a magnet. After 5 consecutive washes in cold phosphate-buffered saline/bovine serum albumin (Calbiochem, La Jolla, CA), the positively selected cells (cell pellet) were immediately stored in liquid nitrogen. Storage of cells with immunomagnetic beads did not influence glycosylase or 8-oxoG levels. The purity of cell populations was greater than 98%, as assessed by the staining of cytospin preparations of positively selected cells by the alkaline phosphatase-antialkaline phosphatase procedure.7
Preparation of nuclear DNA and analyses of 8-oxoG by HPLC-ECD
Extraction of DNA and hydrolyses to nucleosides by nucleaseP1 and alkaline phosphatase were performed as described elsewhere.29 To reduce oxidation during the preparation of DNA, TEMPO (2,2,6,6-tetramethylpiperidine-N-oxyl) was added to all solutions at 100 μM immediately before use. 8-Hydroxy-2′-deoxyguanosine and 2′-deoxyguanosine were separated by high-performance liquid chromatography (HPLC) and were analyzed by electrochemical detection (ECD) (+300 mV) and ultraviolet (UV) light (290 nm). Results were expressed as the ratio of 8-oxoG/106 bp in each DNA sample.
Preparation of cellular extracts
Cell pellets were resuspended in 25 μL 84% sucrose/10 mM EGTA (ethyleneglycotetraacetic acid). After 10-minute incubation on ice, the cells were frozen and thawed 3 times with subsequent centrifugation (15 000g for 15 minutes) to remove cell debris. Supernatant was stored at -20°C.
Assays for DNA glycosylase activity
All enzyme activities were assayed in a reaction buffer containing 70 mM morpholinopropanesulfonic acid (MOPS), pH 7.5, 1 mM EDTA (ethylenediamine tetraacetic acid), 5% glycerol, and 1 mM dithiothreitol, and the mixture was incubated at 37°C for 30 minutes. For analyzing faPy removal, N-[3H]methyl-N′-nitrosourea (18 Ci/mmol [66.6 Bq/mmol]) was used to prepare poly(dG-dC) DNA containing faPy residues (5000 dpm/μg DNA).30 FaPy DNA glycosylase activity was measured in a total volume of 50 μL containing 0.4 μg faPy-DNA substrate. For analyzing DNA glycosylase activity for the repair of alkylating damage, the cell extracts were mixed with 0.3 μg [methyl 3H] methylated DNA (containing 5-10 pmol of methylated bases) in a total volume of 50 μL.
Assays for cleavage of 8-oxoguanine- and 5-hydroxycytosine-containing DNA
Duplex DNA containing a single 8-oxoG residue at position 10 (5′-ATCACCGGC[8-oxoG]CCACACGAGCTG) opposite C and duplex DNA containing a single 5-ohC residue at position 22 (AATTGCGATCTAGCTCGCCAG[5-ohC]AGCGACCTTA TCTGATGA) were purified by 20% nondenaturing polyacrylamide gel electrophoresis. For all substrates, the 5′ ends were 32P-labeled by T4 polynucleotide kinase and γ-32P]adenosine triphosphate (3000 Ci/mmol [11 100 Bq/mmol]; Amersham, Aylesbury, United Kingdom). Reaction mixtures contained 50 fmol substrates and protein extracts, as indicated in a total volume of 10 μL. After incubation at 37°C for 30 minutes, the reaction products were separated on 20% polyacrylamide/7 M urea denaturing gels (Hydrolink, FMC; AT Biochem, Malvern, PA) with 1 × Tris-Borate-EDTA, and radiolabeled fragments were visualized by PhosphorImaging (model 445 SI; Molecular Dynamics, Sunnyvale, CA).
Miscellaneous
HIV RNA levels were measured in EDTA plasma by quantitative reverse polymerase chain reaction (PCR) (Amplicor HIV Monitor; Roche Diagnostic Systems, Branchburg, NY; detection limit 50 copies/mL). Plasma levels of tumor necrosis factor α (TNF-α) were measured by enzyme immunoassay (BioSource, Camarillo, CA).
Statistical analysis
When comparing 3 groups, the Kruskal-Wallis test was used a priori. If a significant difference was found, the Mann-Whitney U test (2-tailed) was used to determine the differences between each pair of groups. For comparisons within the same persons, the Wilcoxon matched pairs test was used. Coefficients of correlation were calculated using the Spearman rank test. If not otherwise quoted, data are given as medians and 25th to 75th percentiles. P less than .05 was considered significant.
Results
Accumulation of 8-oxoG in the DNA of CD4+ and CD8+ T cells from HIV-infected patients
We have previously reported markedly disturbed intracellular redox balance in CD4+ T cells from HIV-infected patients.7 To examine whether such disturbances were associated with enhanced oxidative DNA damage, we analyzed 8-oxoG levels in the genomic DNA of CD4+ and CD8+ T cells from 5 AIDS patients, 4 HIV-infected patients without AIDS, and 7 healthy controls. As shown in Figure 1, CD4+ T cells from HIV-infected patients were characterized by significantly raised 8-oxoG contents, with particularly high levels in AIDS patients (approximately 6-fold increase). In contrast, 8-oxoG levels were similar in CD8+ T cells from HIV-infected patients and controls (Figure 1). In fact, rather than their being increased, 8-oxoG levels in the CD8 subset tended to decrease in the patients without AIDS compared with healthy controls, though the difference did not reach statistical significance (P = .07; Figure 1). In HIV-infected patients, 8-oxoG levels in CD4+ T cells were positively correlated with numbers of HIV RNA copies (r = 0.77; P < .03) and with TNF-α (r = 0.70; P < .05) levels in plasma.
DNA damage in T-cell subsets during HIV infection. Accumulation of 8-oxoG in (A) CD4+ and (B) CD8+ T cells from HIV-infected patients. Nuclear DNA was isolated from T-cell subsets of AIDS patients (n = 5), HIV-infected patients (n = 4), and healthy controls (n = 7). Levels of 8-oxoG were quantified by HPLC-ECD after enzymatic DNA hydrolysis. *P < .05 compared with healthy controls; #P < .05 compared with patients without AIDS. Data are given as medians and as 25th to 75th percentiles.
DNA damage in T-cell subsets during HIV infection. Accumulation of 8-oxoG in (A) CD4+ and (B) CD8+ T cells from HIV-infected patients. Nuclear DNA was isolated from T-cell subsets of AIDS patients (n = 5), HIV-infected patients (n = 4), and healthy controls (n = 7). Levels of 8-oxoG were quantified by HPLC-ECD after enzymatic DNA hydrolysis. *P < .05 compared with healthy controls; #P < .05 compared with patients without AIDS. Data are given as medians and as 25th to 75th percentiles.
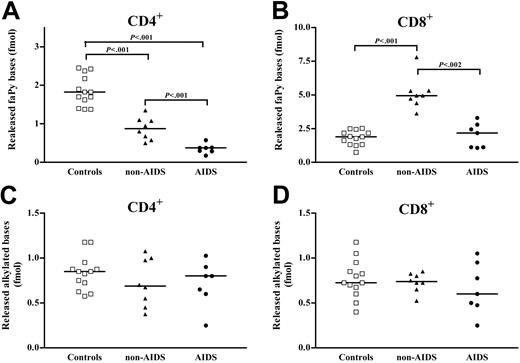
DNA glycosylase activity in CD4+ and CD8+ T cells during HIV infection
We next analyzed whether the accumulation of 8-oxoG in CD4+ T cells was accompanied by alterations in DNA glycosylase activity for the repair of oxidative damage. FaPy is a common substrate for DNA glycosylases involved in the repair of oxidative DNA lesions, and the removal of faPy was measured in CD4+ and CD8+ T cells from 15 HIV-infected patients and 13 healthy controls. Notably, though a slight but significant decrease in the removal of faPy was found in CD4+ T cells from patients without AIDS, CD4+ T cells in AIDS patients had profoundly decreased faPy activity, reaching only approximately 20% of activity in healthy controls (Figure 2). In contrast, faPy excision in CD8+ T cells was markedly increased (approximately 3.5-fold increase, patients without AIDS) or was similar (AIDS patients) to that in healthy controls (Figure 2). In HIV-infected patients, the decrease in faPy activity in CD4+ T cells was inversely correlated with numbers of HIV RNA copies (r =-0.53; P < .05) and with TNF-α (r =-0.61; P < .01) levels in plasma. In contrast to faPy excision, DNA glycosylase activity for the repair of alkylating damage showed no significant differences in these T-cell subsets between HIV-infected patients and controls (Figure 2), suggesting a specific down-regulation of DNA glycosylases repairing oxidative DNA damage in HIV-infected patients.
Repair of oxidative and alkylating DNA damage in T-cell subsets during HIV infection. faPy DNA glycosylase activity (A-B) and alkylated base DNA glycosylase activity (C-D) in extracts of CD4+ and CD8+ T cells from HIV-infected patients and controls. Extracts isolated from AIDS patients (n = 7), HIV-infected patients (n = 8), and healthy controls (n = 13) were incubated with 0.4 μg 3H-labeled faPy-poly(dG-dC) DNA or alkylated calf thymus DNA. Horizontal lines represent median values.
Repair of oxidative and alkylating DNA damage in T-cell subsets during HIV infection. faPy DNA glycosylase activity (A-B) and alkylated base DNA glycosylase activity (C-D) in extracts of CD4+ and CD8+ T cells from HIV-infected patients and controls. Extracts isolated from AIDS patients (n = 7), HIV-infected patients (n = 8), and healthy controls (n = 13) were incubated with 0.4 μg 3H-labeled faPy-poly(dG-dC) DNA or alkylated calf thymus DNA. Horizontal lines represent median values.
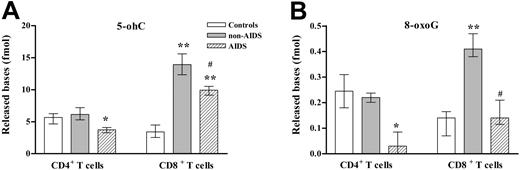
DNA glycosylase activity in T-cell subsets during HIV infection. 5-ohC DNA glycosylase activity (A) and 8-oxoG DNA glycosylase activity (B) in CD4+ and CD8+ T cells from HIV-infected patients. Extracts, isolated from AIDS-patients (n = 7), HIV-infected patients (n = 8), and healthy controls (n = 13), were incubated with 50 fmol duplex oligo containing a single 8-oxoG or 5-ohC residue. The cleavage products were analyzed by 20% denaturing polyacrylamide gel electrophoresis (PAGE) and PhosphorImager scanning. *P < .05; **P < .01 compared with healthy controls. #P < .05 compared with AIDS patients. Data are given as medians and as 25th to 75th percentiles. □ indicates controls;  indicates non-AIDS; ▨ indicates AIDS.
indicates non-AIDS; ▨ indicates AIDS.
DNA glycosylase activity in T-cell subsets during HIV infection. 5-ohC DNA glycosylase activity (A) and 8-oxoG DNA glycosylase activity (B) in CD4+ and CD8+ T cells from HIV-infected patients. Extracts, isolated from AIDS-patients (n = 7), HIV-infected patients (n = 8), and healthy controls (n = 13), were incubated with 50 fmol duplex oligo containing a single 8-oxoG or 5-ohC residue. The cleavage products were analyzed by 20% denaturing polyacrylamide gel electrophoresis (PAGE) and PhosphorImager scanning. *P < .05; **P < .01 compared with healthy controls. #P < .05 compared with AIDS patients. Data are given as medians and as 25th to 75th percentiles. □ indicates controls;  indicates non-AIDS; ▨ indicates AIDS.
indicates non-AIDS; ▨ indicates AIDS.
Levels of DNA glycosylase activity for the repair of 8-oxoG and 5-ohC in T-cell subsets during HIV infection
Although the assay for measuring DNA glycosylase activity for the repair of alkylating damage is specific for the human Aag DNA glycosylase, the faPy assay may detect activity in 5 different DNA glycosylases—hOgg1, hNth1, Neil1, Neil2, and Neil3—for the repair of oxidative damage. Therefore, we examined the removal of 8-oxoG and 5-ohC to further distinguish among these DNA glycosylases. Notably, the removal of 8-oxoG from the CD4+ T cells of AIDS patients showed only approximately 15% of the activity as that from the CD4+ T cells of healthy controls, suggesting a decrease in the major 8-oxoG DNA glycosylase activity (ie, hOgg1) (Figure 3). Excision of 5-ohC in CD4+ T cells was also decreased in AIDS patients (approximately 70% of activity in healthy controls), suggesting a moderate reduction in 1 or more of the 3 glycosylases reported to remove 5-ohC (hNth1, Neil1, and Neil2). Furthermore, and in accordance with our findings for faPy activity, CD8+ T cells from patients without AIDS showed a 3-fold increase in 8-oxoG removal and a 4-fold increase in 5-ohC removal comparing CD8+ T cells from healthy controls, indicating an enhancement of hOgg1 activity and an up-regulation of 1 or several of the DNA glycosylases excising oxidized pyrimidines (hNth1, Neil1, and Neil2). In contrast, although CD8+ T cells from AIDS patients showed no changes in faPy removal, we found a 3-fold increase in 5-ohC excision comparing healthy controls (Figure 3). This could indicate a DNA glycosylase activity with affinity for 5-ohC but not for faPy. The 8-oxoG activity in CD8+ T cells from AIDS patients was not altered (Figure 3).
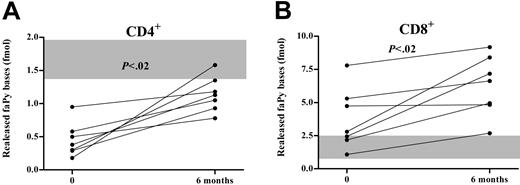
DNA glycosylase activity during HAART. faPy DNA glycosylase activity in CD4+ (A) and CD8+ (B) T cells from HIV-infected patients during HAART. Extracts isolated from 7 HIV-infected patients before and after 6 months of HAART were incubated with 0.4 μg 3H-labeled faPy-poly(dG-dC) DNA. The shaded area indicates ranges in 13 healthy controls.
DNA glycosylase activity during HAART. faPy DNA glycosylase activity in CD4+ (A) and CD8+ (B) T cells from HIV-infected patients during HAART. Extracts isolated from 7 HIV-infected patients before and after 6 months of HAART were incubated with 0.4 μg 3H-labeled faPy-poly(dG-dC) DNA. The shaded area indicates ranges in 13 healthy controls.
Except for 11 patients who were receiving nucleoside analog(s) (see “Patients, materials, and methods”), none of the patients were regularly taking medication. Although these 11 patients did not differ from the other patients with regard to the measured parameters (data not shown), we cannot exclude some influence from the use of these medications.
DNA glycosylase activity during HAART
HAART strongly reduces levels of plasma HIV RNA and produces concomitant increases in T-cell counts and beneficial effects on clinical symptoms and mortality.31 To further examine the relationship between HIV infection, oxidative DNA damage, and DNA glycosylases, we examined DNA glycosylase activity for the removal of faPy and alkylating DNA damage in CD4+ and CD8+ T cells from 7 HIV-infected patients before and 6 months after initiating HAART. Each patient received an HIV protease inhibitor (indinavir 800 mg, 3 times a day) in combination with 2 nucleoside analogs (zidovudine 250 mg and lamivudine 150 mg, twice a day). In response to HAART, there was a marked decrease in HIV RNA copies in plasma (maximal decrease, 3.02 [1.92-3.98] log10; P < .05) and a marked increase in CD4+ (maximal increase, 150 [50-215] × 106/L; P < .05) and CD8+ (maximal increase, 260 [30-415] × 106/L; P < .05) T-cell counts in peripheral blood. Concomitantly, there was a significant increase in faPy activity in CD4+ T cells (Figure 4) that was inversely correlated with the decrease in plasma viral load (r = 0.68; P < .05). However, there was no normalization compared with faPy activity in healthy controls (Figure 4). Moreover, even if faPy activity in CD8+ T cells was increased before therapy was initiated, HAART induced a further increase in activity with particularly enhancing effect in those with the lowest faPy levels at baseline (Figure 4). In comparison, DNA glycosylase activity for the repair of alkylating damage showed no changes during HAART in either CD4+ or CD8+ T cells (data not shown). Finally, we analyzed 8-oxoG levels in T-cell subsets of 4 AIDS patients who had received HAART for 1 year. Notably, though the CD4+ T cells in AIDS patients not receiving HAART showed markedly enhanced levels of 8-oxoG in genomic DNA (Figure 1), CD4+ T cells from AIDS patients on successful HAART showed 8-oxoG levels within the range of those in healthy controls (34.0 [29.5-36.0] 8-oxoG per 106 dG vs 40.5 [27.8-48.0] 8-oxoG per 106 dG, patients and controls, respectively).
Discussion
Several studies report that enhanced oxidative stress in HIV infection may have a pathogenic role in this disorder.10 In the present study, we show that HIV-infected patients, particularly those with advanced disease, have enhanced oxidative DNA damage in CD4+ T cells, as assessed by increased 8-oxoG accumulation. Notably, this increase in oxidative DNA damage was accompanied by a marked decline in DNA glycosylase activity for the repair of oxidative base lesion in CD4+ T cells. In contrast, CD8+ T cells of HIV-infected patients, with 8-oxoG levels that were similar to or lower than those in healthy controls, showed enhanced capacity to repair oxidative damage. Finally, during HAART, there was an increase in glycosylase activity in CD4+ T cells and near normalization of 8-oxoG levels in these cells. Although we cannot totally exclude some influence on our results from an undiagnosed and clinically asymptomatic coinfection, our data suggest that impaired base excision repair of oxidative damage, with subsequent accumulation of oxidative DNA base lesions in CD4+ T cells, may play a pathogenic role in HIV infection.
The mechanisms leading to enhanced oxidative stress in CD4+ T cells during HIV infection are complex. The increased activity of inflammatory cytokines (eg, TNF-α) and the altered intracellular glutathione redox status found in HIV-infected patients9 may promote oxidative DNA damage in CD4+ T cells. However, our findings of an inverse correlation between viral load and glycosylase activity and near normalization of repair capacity during HAART suggest that direct HIV-related mechanisms may be involved in the dysregulation of oxidative DNA damage/repair activity during HIV infection. Thus, TNF-α and ROS can increase the transcription of viral proteins by activating the nuclear factor of transcription-κβ (NF-κβ).32 The HIV proteins Tat and gp120 may again directly enhance oxidative stress in T cells possibly involving TNF-dependent mechanisms,33 representing a pathogenic loop promoting inflammation, enhanced oxidative stress, and HIV replication. Moreover, the HIV protein vpr, which may arrest T cells and may induce subsequent apoptosis, has been found to incorporate catalytically active uracil DNA glycosylase into HIV viron particles, further supporting a link between HIV replication and DNA repair mechanisms.34 In fact, this glycosylase, which initiates base excision repair of deaminated cytosine, is important for the modulation of the virus mutation rate.35 It is, therefore, tempting to hypothesize that the imbalance between glycosylase activity and oxidative DNA damage in CD4+ T cells during HIV infection could reflect potent interactions among viral proteins, enhanced oxidative stress, and increased activity of inflammatory cytokines overwhelming DNA repair mechanisms.
Regulation of the various DNA glycosylases involved in the repair of oxidative damage in humans has not been fully clarified. However, hNth1 transcription was shown to increase during the early and middle S-phases of the cell cycle,36 suggesting that increased 5-ohC DNA glycosylase activity in CD8+ T cells during HIV infection may correlate with the enhanced spontaneous T-cell proliferation observed in these patients.37 In CD4+ T cells, such a stimulus may be counteracted and overshadowed by the enhanced oxidative stress in these cells. In contrast to hNth1, the hOgg1 gene lacks TATA or CAAT boxes, suggesting that Ogg1 is a housekeeping gene with stable expression during cell cycle.38 However, the results are conflicting, possibly reflecting different regulation in different cell types. Thus, increased 8-oxoG levels and ischemia have been reported to enhance Ogg1 activity in human colorectal carcinoma cells and in the mouse brain, respectively.39,40 Moreover, though acute ischemia and oxidative stress may promote the up-regulation of DNA glycosylase activity, persistently enhanced oxidative stress and inflammation, as occur in HIV infection, may potentially down-regulate or “consume” the activity of these enzymes. Nevertheless, the mechanisms for the regulation of DNA glycosylases for the repair of oxidative base lesions in T-cell subsets during HIV infection are unclear.
In the present study, we show that DNA glycosylases for the repair of oxidative base lesions are differently regulated in CD4+ and CD8+ T cells during HIV infection. In fact, rather than decreased activity, CD8+ T cells in patients without AIDS were characterized by enhanced faPy, 5-ohC, and 8-oxoG DNA glycosylase activity and by a nonsignificant decrease in 8-oxoG level in these cells. This phenomenon could possibly reflect that although HIV infection is characterized by a functional and numeric decline in CD4+ T cells, CD8+ T cells are characterized by increased numbers and enhanced activity, at least in patients without AIDS.41
Our findings suggest that CD4+ T cells in HIV-infected patients may lack the ability to sufficiently repair DNA damage induced by oxidative stress that may have several consequences. Mutant forms of hOgg1 have been found in lung and kidney tumors.42 A recent report suggests that reduced Neil1 activity arising from mutations and reduced expression may be involved in the pathogenesis of a subset of gastric cancers.43 It is possible that the imbalance between oxidative DNA damage and repair activity in CD4+ T cells from AIDS patients might contribute to the increased frequency of malignancies in these patients. Moreover, though long-time exposure to moderately increased oxidative DNA damage may result in a predisposition to malignancy, markedly enhanced oxidative DNA damage combined with decreased repair activity, as found in CD4+ T cells from HIV-infected patients, may lead to functional impairment of CD4+ T cells by slowing cell cycle progression on activation and by enhancing apoptosis, possibly contributing to the pathogenesis of T-cell deficiency in HIV-infected patients. Finally, the HIV genome is characterized by a high frequency of mutation that at least partly can be attributed to the high rate of HIV replication and the low fidelity of the reverse transcriptase gene. These mutations, which involve a high frequency of base misincorporations, may lead to a several-fold decrease in sensitivity to 1 or more antiretroviral drugs and are at present an increasing challenge in HAART.44 Several oxidative base lesions are strongly premutagenic if they remain in DNA during replication. For instance, 5-ohC and 8-oxoG are stable oxidation products with strong miscoding properties, which produce G>T transversions45 and C>T transitions/C>A transversions,46 respectively. Therefore, it is possible that the accumulation of mutagenic base lesions as a result of enhanced oxidative stress and impaired capacity for repair of oxidative DNA damage in CD4+ T cells in HIV-infected patients may predispose them to elevated mutation frequency in the HIV genome of these cells.
In conclusion, the present study further supports a role for oxidative stress in the pathogenesis of HIV infection by demonstrating a marked imbalance between the accumulation of oxidative DNA damage and the capacity to repair such lesions in CD4+ T cells (favoring enhanced DNA damage). These findings may represent a previously unrecognized mechanism involved in the numeric and functional impairment of CD4+ T cells during HIV infection.
Prepublished online as Blood First Edition Paper, February 10, 2005; DOI 10.1182/blood-2004-11-4272.
Supported by the Norwegian Cancer Society and the Research Council of Norway, Anders Jahre's Foundation, Medinnova Foundation, and Odd Kåre Rabben's Memorial Fund for AIDS Research.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal