Comment on Krishnan et al, page 874
High-dose chemotherapy and autologous stem cell transplantation in HIV-infected patients with relapsed lymphomas led to a durable remission with an 85% progression-free survival.
The introduction of highly active antiretroviral therapy (HAART) has reduced the morbidity and mortality of HIV/AIDS with malignancies being the first cause of death. However, HIV-positive patients with relapsed lymphomas have very limited therapeutic options. Autologous stem cell transplantation (ASCT) is the first-choice treatment for HIV-negative patients with relapsed chemosensitive lymphomas. American and European groups, such as ours, have recently explored this approach in HIV patients, and it has been demonstrated that the treatment is feasible and active also in this setting. Previous studies have already shown that it is usually possible to mobilize a sufficient number of stem cells, that HAART can be administrated with high-dose chemotherapy (HDC), and that the rates of infectious complications are similar to the ones occurring in HIV-negative patients when the appropriate prophylaxes are used.1-3
But, up to now, we have little information about the long-term follow-up in these patients, and little is known about the dynamics of immune reconstitution and HIV replication after the ASCT.FIG1
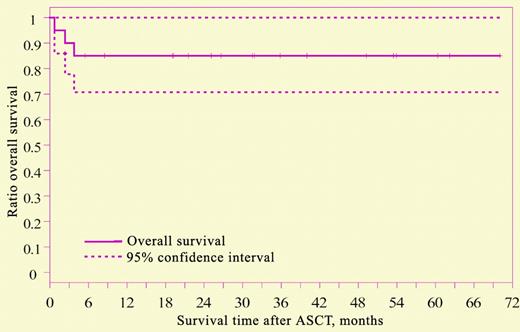
Overall survival after ASCT, N = 20. See the complete figure in the article beginning on page 874.
Overall survival after ASCT, N = 20. See the complete figure in the article beginning on page 874.
In this issue of Blood, Krishnan and colleagues reported the results of the longest follow-up performed in HIV patients with lymphomas who underwent ASCT. In this series of 20 patients, 17 are still alive and in remission after a median period of observation of 31.8 months. The progression-free survival is 85% and the overall survival (OS) is 85% for the entire group (Figure 1). These results are very impressive and the best reported in literature, but they are affected by a favorable patient selection: 4 patients were in first complete remission (CR). Moreover, the study is not an intention-to-treat analysis as reported by Re et al.3 Therefore, the paper does not completely clarify how many patients with HIV-related lymphomas may really benefit from ASCT.
The authors also demonstrated that the underlying HIV infection did not worsen as a result of the transplantation, and CD4 count returned to baseline within 1 year. This observation is not a surprise; in fact, we have observed that HIV patients with relapsed lymphomas treated with HDC and ASCT with the same program offered to the general population had the same dynamics of immune reconstitution.4 In the Krishnan et al series, the long-term follow-up showed that 10 of 17 patients experienced viral failure and needed HAART changes, nevertheless the CD4 count overcame the baseline level at the second year. All of these observations demonstrated that the iatrogenic immunodepression following ASCT not only does not significantly differ from HIV-negative patients, but it might not enhance HIV progression, if particular attention is taken in the management of HAART and antiretroviral options are still available.
This paper not only confirms the feasibility and the favorable long-term survival of ASCT in HIV patients, but clearly points out that this therapeutic strategy should be offered as a salvage therapy in HIV-related relapsed chemosensitive lymphomas, while it should be considered still experimental for patients in first CR. ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal