Abstract
Hematopoietic stem cell transplantation (HSCT) has been proposed for the treatment of severe multiple sclerosis (MS). In a phase 2 multicenter study we selected 19 non–primary progressive MS patients showing high disease activity on the basis of both brain magnetic resonance imaging (MRI) and sustained clinical deterioration despite conventional treatments. After stem cell mobilization with cyclophosphamide (CY) and filgrastim, patients were conditioned with BCNU (1,3-bis(2-chloroethyl)-1-nitrosourea), cytosine arabinoside, etoposide, and melphalan (BEAM) followed by antithymocyte globulin (ATG). Unmanipulated peripheral blood stem cells (PBSCs) were then infused. No maintenance treatment was administered with a median follow-up of 36 months (range, 12 to 72 months). All patients showed clinical stabilization or improvement; 3 subsequently deteriorated, 1 beyond the baseline. No MRI active lesions were detected after the HSCT except in 1 patient who showed a new lesion at 4.5 years. Infections were limited and restricted to 3 months after HSCT. Health-related quality of life was assessed through the 54-item MS quality of life (MSQOL-54) questionnaire, showing a statistically significant improvement in both composite scores and in most of the individual domains. HSCT is able to induce a prolonged clinical stabilization in severe progressive MS patients, resulting in both sustained treatment-free periods and quality of life improvement.
Introduction
Multiple sclerosis (MS) is the most frequent cause of neurologic disability in young adults in the Western countries.1 Clinical course is widely variable, ranging between isolated episodes without any significant clinical deterioration and extremely aggressive forms resulting in reduction of life expectancy. Etiology of MS is unclear, but a number of clinical and experimental findings indicate some role of autoreactive T-lymphocytic clones entering the central nervous system across small veins in the generation of the immune cascade causing the typical white matter lesions. For this reason MS is conventionally included among the autoimmune diseases.2 Inflammation with loss of myelin, oligodendrocytes, and axonal degeneration are the major components in determining the clinical evolution. Immunosuppressive/immunomodulating treatments are currently the only recognized forms of therapy.3 Interferon-β and glatiramer acetate have been utilized for relapsing forms of MS, but these therapies are only partly effective for most patients.4 Azathioprine, cyclophosphamide, and cladribrine have been employed either as first- or second-line treatment. Recently mitoxantrone has been approved for MS progressive forms not responding to conventional treatments.5,6
Following results in animal models7,8 and clinical observations in patients with malignancies and concomitant MS,9-11 hematopoietic stem cell transplantation (HSCT) was first proposed for the treatment of autoimmune diseases.12,13 Debulking of autoreactive clones followed by restoring of self-tolerance during the immunologic recovery has been postulated.7 Autologous HSCT was first adopted for the therapy of MS in the late 1990s.14-16 Data on the MS cases treated with autologous HSCT have been analyzed and published as single-center studies,17-19 multicenter trials,20,21 and as a collective European Group for Blood and Marrow Transplantation (EBMT) retrospective study.22 It is significant that 74% of 85 MS patients reviewed are progression free at 3 years from transplantation.22 However, due to the different clinical forms of MS treated as well as the multiplicity of the employed immunoablative regimens, these results should be interpreted with caution.
Four different clinical courses of MS have been defined.23 Relapsing-remitting MS (RRMS) is characterized by self-limited attacks of neurologic dysfunction (relapses) evolving over days to weeks. Between relapses most patients experience a recovery of function that is often (but not always) complete. Some RR cases, however, do not improve after relapses and accumulate disability. Primary progressive MS (PPMS) is characterized by a steady decline in function from the beginning without relapses. Secondary progressive MS (SPMS) begins as RRMS, but at some point a steady deterioration in function, with or without superimposed relapses, takes place. Progressive-relapsing MS (PRMS) is characterized by a steady decline in function from the beginning with superimposed clinical relapses. There is some evidence that PPMS is less responsive to HSCT as compared with both SPMS and RRMS.22 A possible explanation of this finding could be the prevalence of degeneration over inflammation in PPMS.
We report the follow-up of a prospective phase 2 multicenter trial started in 1998 and involving 7 Italian centers. The study was promoted by the Italian Group for Bone Marrow Transplantation (GITMO) and focused on clinical and magnetic resonance imaging (MRI) monitoring of poor-prognosis patients, following harmonization of parameters and clinical methodology among the participating centers. The conditioning regimen (BCNU [1,3-bis(2-chloroethyl)-1-nitrosourea], cytosine arabinoside, etoposide, and melphalan [BEAM]; and antithymocyte globulin [ATG]) was adapted from the pioneering work of Fassas et al in Greece.15 The trial was planned to include 20 patients with a 2-year follow-up, which was in fact prolonged whenever possible. A report on the first group of 10 patients with a median follow-up of 15 months has been published.20
This report presents an update and new data on a larger group of 19 patients, with a median follow-up of 36 months. These data concern safety and feasibility of the procedure as well as evaluation of outcome. In addition, the novel but relevant issue of the quality of life in MS patients who have received HSCT has been addressed. Most clinical evaluations in MS patients are based on impairment and functional scales primarily focused on mobility but lack a more global health assessment. This item could be significant in the discussion of the ethical issues associated with the role of HSCT in MS. The evaluation of risks and benefits of HSCT in these patients also should include an assessment of health-related quality of life (HRQOL) expectance based on objective parameters. The impact of HSCT on HRQOL was evaluated in 9 patients utilizing the 54-item MS quality of life (MSQOL-54) questionnaire.
Patients, materials, and methods
Nineteen patients were enrolled in the GITMO study between July 1998 and December 2003. End points were changes in the number of triple-dose gadolinium (Gd)–enhancing lesions on brain MRI, changes in Expanded Disability Status Scale (EDSS), and HSCT toxicity. Changes in HRQOL and in brain MRI volume were assessed in a subgroup of 9 and 10 patients, respectively. The study was approved by the ethics committees of all participating institutions before study initiation. All patients gave written informed consent.
Patient eligibility
The inclusion criteria were the following: age between 18 and 55; clinically and laboratory definite SPMS, RRMS, or PRMS; EDSS score between 5.0 and 6.5; documented rapid progression over the previous year despite conventional therapies (progression is defined as a worsening of 1.0 or more EDSS points between EDSS 5.0 and 6.0 or of 0.5 or more points between 6.0 and 6.5); presence of at least 1 enhancing area on brain MRI using a triple dose (TD) of Gd; absence of cognitive disturbances measured utilizing the Mini-Mental Status Examination and a set of neuropsychological tests; absence of concomitant diseases; and no treatment with interferons in the previous 3 months and immunosuppressive agents within 6 months of enrollment.
Stem cell mobilization and conditioning regimen
Peripheral blood stem cells (PBSCs) were mobilized with cyclophosphamide (CY) 4 g/m2 in 1 day and daily nonglycosylated granulocyte colony-stimulating factor (G-CSF) (filgrastim) 5 μg/kg subcutaneously starting from day +2 from CY until the completion of the harvests. Prednisone (5 mg/kg) was added to prevent cytokine release during CY administration. The target number of harvested CD34+ cells was 3 × 106/kg to 8 × 106/kg. This range was chosen after the first patient received 16.46 × 106/kg. A number exceeding 8 × 106/kg would have resulted in an increase of total lymphocytes infused without improving hematopoietic engraftment. Unmanipulated PBSCs were cryopreserved using standard techniques24 ; when possible, a back-up dose was also stored.
The immunoablative therapy was carried out within 30 to 40 days after mobilization. The conditioning regimen consisted of the combination chemotherapy BEAM: BCNU 300 mg/m2 at day -7; cytosine arabinoside 200 mg/m2 and etoposide 200 mg/m2 from day -6 to day -3; and melphalan 140 mg/m2 at day -2. On day 0 cells were thawed and infused. Rabbit ATG (Thymoglobulin; Genzyme, Cambridge, MA) (5 mg/kg/d) was administered at days +1 and +2 as in vivo T depletion, together with prednisone (5 mg/kg). Intravenous cyclosporin A (1 mg/kg) was also administered during the conditioning regimen to prevent neurologic exacerbation due to cytokine release.25 G-CSF was not administered after transplantation unless the neutrophil count was still below 0.5 × 109/L at day +12, to avoid the risk of neurologic adverse effects due to G-CSF, as previously described.26 Standard guidelines were followed for infection prophylaxis; in particular, acyclovir (250 mg 3 times per day) was given intravenously from day -6 until discharge from the hospital and then orally (400 mg twice a day) for 3 months after transplantation. Trimethoprim-sulfamethoxazole was given for 6 months, and intravenous immunoglobulins were administered 200 mg/kg weekly during hospitalization until hematologic recovery.
Hematologic and immunologic recovery
Engraftment was defined as a polymorphonuclear cell (PMN) count above 0.5 × 109/L and a platelet (Plt) count above 20 × 109/L without transfusion. Lymphocyte subsets were evaluated at baseline, after mobilization, and at 1, 2, 3, and 6 months and 1 and 2 years after transplantation using a 3-color flow cytometric analysis according to the standard techniques. The following combination of mouse monoclonal antibodies were tested: CD3 and CD19, respectively, for T and B cells; CD3 and CD4 for CD4+ T cells; CD3 and CD8 for CD8+ T cells; CD16/CD56 for natural killer (NK) cells; CD4 and CD45RA for naive CD4+ T cells; and CD4 and CD45RO for memory CD4+ T cells. The absolute values of each cell type were calculated from the percentages of total leukocytes, as determined by standard laboratory counter.
Neurologic assessment
Neurologic assessment was scheduled at screening visit, at baseline, 30 days after mobilization, after the conditioning regimen, then monthly for the 6 months following transplantation, and then at +9, +12, +18, and +24 months. Whenever possible the follow-up was longer. EDSS was evaluated at each visit, along with Gd brain MRI. Cerebrospinal fluid (CSF) examination was also scheduled at baseline and at 6 and 12 months. Clinical improvement was defined as a decrease in the EDSS score by at least 0.5 points as compared with baseline confirmed after 6 months; progression was defined as the increase by at least 0.5 points confirmed after 6 months; the time of the first increase of EDSS was taken as the time of disease progression. Clinical relapse was defined as the appearance of new symptoms or worsening of old symptoms of at least 24 hours' duration in the absence of fever in a previously (4 weeks) stable patient.
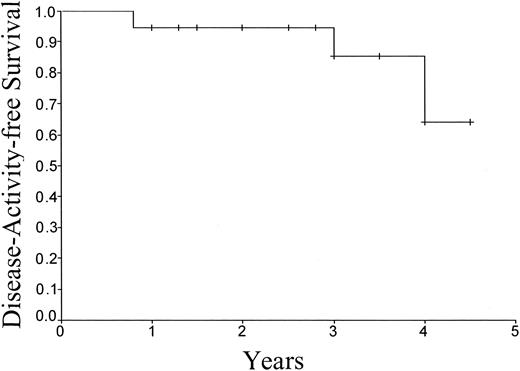
Confirmed progression-free survival was defined as the probability of being alive without clinical progression as compared with baseline measurement. Disease activity-free survival was defined as the probability of being alive without clinical progression of any type, which included any confirmed disease progression on EDSS at last assessment and disease progression events (relapse or exacerbation) even if not associated with deterioration in the EDSS score.22
MRI evaluation
The effect of HSCT was evaluated with serial monthly TD Gd-enhanced brain MRI for a pretreatment period of 3 months and compared with serial monthly TD Gd-enhanced MRI imaging for the following 6 months. Subsequently, MRI scans were obtained every 3 months until month 24 and every 6 months afterward. We used TD Gd (0.3 mmol/kg gadodiamide [Omniscan]; Nycomed Amersham, Princeton, NJ), reported to detect about 70% more lesions than the standard dose (0.1 mmol/kg).27 The MRI procedure was standardized in all participating centers and was performed according to established criteria.28 Images were sent to the Neuroimaging Research Unit, Scientific Institute and University, S. Raffaele Hospital, Milan, Italy, where they were examined and quantified by an experienced observer masked to treatment phase. The number of Gd-enhancing lesions were counted. After the first 10 patients completed the scheduled 24 months of follow-up, MRI scans were locally evaluated.
In 10 patients an analysis of brain volume changes has been performed.29 Based on precontrast T1-weighted images, percentage normalized brain volume change (PBVC) and cross-sectional normalized brain volume (NBV) were estimated. The following metrics were obtained from each patient: the NBV at month 1 and the PBVC between baseline and month 12 and then again between months 12 and 24.
Quality of life assessment
Nine participants in the study completed the 54-item MS quality of life (MSQOL-54) questionnaire at baseline, 6, 12, and 24 months.30,31 These 9 cases were the first patients to be enrolled in the study; they were not selected for any clinical or laboratory reasons and therefore can be considered representative of the entire population of patients examined in the present study.
The MSQOL-54 is a disease-specific measure of HRQOL. It consists of the Short Form 36 (SF-36) along with 18 additional items pertinent to people with MS. The SF-36 is a well-known generic health-related quality of life questionnaire. It consists of 36 items grouped into 8 domains: physical function, social function, physical role limitations, emotional role limitations, pain, energy/fatigue, mental health, and general health. The 18 MS-specific items are grouped into 5 domains: health distress, sexual function, sexual satisfaction, cognitive function, and overall quality of life. As with SF-36, the MSQOL-54 domains can be reduced to 2 composite scores: physical and mental. The “overall quality of life” is 1 of the 12 domains of the MSQOL-54. The overall quality of life scale is made up of 2 items that tap the global subjective assessment of overall QOL. One item is the criterion measure used in a patient preference study,32 which was itself adapted from the “Faces Scale.”33 The other item asks patients to assess their satisfaction with their life in general using a 7-point “delighted-terrible” scale.33,34
Statistical analyses
Outcomes are reported as of April 2004 based on the last follow-up of each patient. Differences in the number of MRI-enhancing lesions before and after transplantation were evaluated with the Mantel-Haenszel test. Time to event curves were estimated using the method of Kaplan-Meier.
HRQOL data were analyzed using Friedman repeated measure analysis of variance on ranks.
Results
Patients enrolled
Patients' characteristics are summarized in Table 1. There were 12 females and 7 males, with a median age of 36 years (range, 26 to 52 years). Disease course was SPMS in 15 cases and RRMS in 4. In SPMS, relapses were superimposed in 5 cases; in 3 of 4 RRMS patients, relapses were not followed by improvement, with an ensuing rapid worsening of disability. The median age at the onset of disease was 24 years (range, 15 to 46 years); the median disease duration was 12 years (range, 4 to 19 years). The median duration of the progressive phase was 5 years (range, 1 to 11 years). Twelve patients had been previously treated with interferon-β 1a or 1b and 7 treated only with azathioprine and/or steroids, all without clinical response. Two patients were treated after interferon-β with cyclophosphamide at the dosage of 1 g intravenously monthly for 4 months and for 6 months, respectively. Another patient, following failure with interferon-β 1b, was treated with mitoxantrone (3 cycles at the dosage of 20 mg intravenously each) without any benefit on the relapse rate and progression.
Characteristics of patients enrolled
No. | 19 |
| Sex, F/M | 12/7 |
| Median age, y (range) | 36 (26-52) |
| Disease course | |
| SPMS | 15 |
| RRMS | 4 |
| Median age at disease onset, y (range) | 24 (15-46) |
| Median disease duration, y (range) | 12 (4-19) |
| Median duration of progressive phase, y (range) | 5 (1-11) |
| Previous treatments | |
| Interferon-β | 12 |
| Steroids, azathioprine | 7 |
| Cyclophosphamide | 2 |
| Mitoxantrone | 1 |
No. | 19 |
| Sex, F/M | 12/7 |
| Median age, y (range) | 36 (26-52) |
| Disease course | |
| SPMS | 15 |
| RRMS | 4 |
| Median age at disease onset, y (range) | 24 (15-46) |
| Median disease duration, y (range) | 12 (4-19) |
| Median duration of progressive phase, y (range) | 5 (1-11) |
| Previous treatments | |
| Interferon-β | 12 |
| Steroids, azathioprine | 7 |
| Cyclophosphamide | 2 |
| Mitoxantrone | 1 |
SPMS indicates secondary progressive MS; RRMS, relapsing-remitting MS.
At the screening visit, the median EDSS was 6.5 (range, 5.0 to 6.5). At baseline, immediately before stem cell mobilization, the neurologic condition had deteriorated in 11 cases (median EDSS, 6.5; range, 5.5 to 8).
Stem cell mobilization and collection
Mobilization was successful in all cases, with a median number of 8.69 × 106/kg (range, 3.51 × 106/kg to 26.02 × 106/kg) collected CD34+ cells. First mobilization failed only in 1 patient, who required 2 further mobilization procedures with G-CSF alone. The median number of harvests was 2 (range, 1 to 5), and the median number of liters of blood processed was 12 (range, 9 to 18). The nadir of PMNs and Plts occurred 8 (range, 7 to 12) and 10 (range, 3 to 15) days after mobilization, respectively, and median days with PMNs below 0.5 × 109/L and Plts below 50 × 109/L were 3 (range, 0 to 4) and 0 (range, 0 to 4), respectively.
No major clinical adverse events were observed during this phase; fever of unknown origin was reported in 4 patients. No clinical relapses occurred. Only 1 patient experienced a severe hemorrhagic cystitis after CY administration, which required a specific treatment for 2 months. Notably, this patient suffered from a severe bladder dysfunction and had been treated in the previous year with monthly CY 1 g intravenously for 6 months. Urinary tract infection occurred in another patient, who showed the highest EDSS score before mobilization (EDSS 8.0) and was routinely under intermittent urinary catheterization. A central venous cathether (CVC)–related phlebitis of the subclavian vein and a transient episode of inappropriate secretion of antidiuretic hormone (ADH) were also reported. All these complications resolved without sequelae after appropriate treatment (Table 2).
Mobilization adverse events
Adverse events . | No. . |
|---|---|
| Fever | 4 |
| Hemorrhagic cystitis | 1 |
| Urinary tract infection | 1 |
| CVC-related phlebitis | 1 |
| Inappropriate secretion of ADH | 1 |
Adverse events . | No. . |
|---|---|
| Fever | 4 |
| Hemorrhagic cystitis | 1 |
| Urinary tract infection | 1 |
| CVC-related phlebitis | 1 |
| Inappropriate secretion of ADH | 1 |
Engraftment and adverse events
Unmanipulated grafts were infused without complications and contained a median number of 6 × 106/kg (range, 3.01 × 106/kg to 16.46 × 106/kg) CD34+ cells. Engraftment was uneventful, and no signs of an engraftment syndrome were reported. Median days with PMNs below 0.5 × 109/L and Plts below 50 × 109/L were 8 (range, 6 to 12) and 10 (range, 6 to 14), respectively; days to reach a complete platelet engraftment (Plts above 100 × 109/L) were 15 (range, 9 to 27). Transfusion support was minimal, with a median number of red blood cell and platelet units transfused of 2 (range, 0 to 6) and 3 (range, 1 to 4), respectively.
Infusion of rabbit ATG (rbATG) was also well tolerated with minor adverse effects; only in one case it was followed by high fever, cutaneous rash, and diffuse myalgia, with complete recovery after steroid therapy.
Infections were common following the immunoablative treatment. Fever during the neutropenic postconditioning phase occurred in 16 of 19 patients (11, fever of unknown origin; 5, documented sepsis) and was successfully treated with intravenous antibiotic therapy, for a median of 12 (range, 5 to 38) days of treatment. Three cases of urinary tract infection and 3 cases of enteritis were reported. In 6 cases a cytomegalovirus (CMV) reactivation was detected within 2 months (range, 19 to 60 days) after transplantation by monitoring p65 antigenemia and/or by polymerase chain reaction (PCR). In 5 of these patients, CMV reactivation was symptomatic with fever, and in 1 case also with arthralgia and diarrhea, requiring specific antiviral treatment (ganciclovir and/or foscarnet). In 1 case, the administration of foscarnet was required due to a particular aggressive course of the infection with a rapid increase of the p65 antigenemia under treatment with ganciclovir; the patient finally achieved the clearance of CMV antigen from the blood. Varicella zoster infection occurred in 2 cases following the cessation of acyclovir prophylaxis, at +3 and +4 months from HSCT, respectively, and responded to retreatment with acyclovir (Table 3). A transient monoclonal gammopathy was reported in 3 patients and a transient increase in aspartate aminotransferase/alanine aminotransferase (AST/ALT) values in 1 patient; finally, another patient suffering from a chronic gastric ulcer experienced a severe esophagitis and bleeding gastric ulcer requiring endoscopic treatment (Table 3). The last patient in the present series suffered a femoral fracture due to an accidental fall. The fracture was surgically treated, and now the patient is on rehabilitation.
Transplantation-related adverse events
Adverse events . | No. . |
|---|---|
| Early: within 2 mo | |
| Fever | 16 |
| FUO (documented sepsis) | 11 (5) |
| CMV reactivation (symptomatic) | 6 (5) |
| Urinary tract infection | 3 |
| Enteritis | 3 |
| Transient increase in AST/ALT levels | 1 |
| Gastric ulcer bleeding | 1 |
| Late: between 2 and 4 mo | |
| HVZ infection | 2 |
| Transient monoclonal gammopathy | 3 |
Adverse events . | No. . |
|---|---|
| Early: within 2 mo | |
| Fever | 16 |
| FUO (documented sepsis) | 11 (5) |
| CMV reactivation (symptomatic) | 6 (5) |
| Urinary tract infection | 3 |
| Enteritis | 3 |
| Transient increase in AST/ALT levels | 1 |
| Gastric ulcer bleeding | 1 |
| Late: between 2 and 4 mo | |
| HVZ infection | 2 |
| Transient monoclonal gammopathy | 3 |
FUO indicates fever of unknown origin; HVZ, herpes varicella zoster.
During and after the conditioning regimen, neither clinical relapses nor transplantation-related neurologic adverse events were reported. Commonly, fever and concomitant infections caused a mild deterioration of neurologic conditions in the first weeks following HSCT, and asthenia was frequent. This clinical worsening was due to fever and infections as suggested by the rapid amelioration upon improvement of the patients' general conditions.
Immunologic recovery
Immunologic recovery following HSCT was analyzed in 17 of 19 patients. While a relatively rapid reconstitution was observed for B and NK populations (Figure 1A-B), a marked decrease of CD4+/CD8+ ratio was still persistent 2 years after transplantation, due both to the rapid increase of CD8+ T lymphocytes and the lack of a complete recovery of CD4+ cells (Figure 1C-D). The evaluation of CD4+CD45RO memory and CD4+CD45RA naive cells' recovery, available for 6 patients, showed a prompt reconstitution of the memory subset and a prolonged suppression of the naive one (Figure 1E-F).
Recovery of lymphocyte subsets after HSCT. Median lymphocyte counts evaluated at baseline, at transplantation, and at 1, 2, 3, and 6 months and 1 and 2 years after transplantation; error bars denote the SEM. Normal values are represented by the solid thick lines indicating the central 95% of the area under the distribution curve of values in healthy adults.35 The numbers of patients analyzed were 17 before transplantation, 15 on day 30, 15 on day 60, 16 on day 90, 16 on day 180, 14 on day 365, and 3 on day 730 for B, T, and NK cells (A-D); for CD45 naive and memory cells (E-F) the analysis was available for 6 patients at all the time points.
Recovery of lymphocyte subsets after HSCT. Median lymphocyte counts evaluated at baseline, at transplantation, and at 1, 2, 3, and 6 months and 1 and 2 years after transplantation; error bars denote the SEM. Normal values are represented by the solid thick lines indicating the central 95% of the area under the distribution curve of values in healthy adults.35 The numbers of patients analyzed were 17 before transplantation, 15 on day 30, 15 on day 60, 16 on day 90, 16 on day 180, 14 on day 365, and 3 on day 730 for B, T, and NK cells (A-D); for CD45 naive and memory cells (E-F) the analysis was available for 6 patients at all the time points.
Clinical outcome
During the 3 months off treatment between enrollment and mobilization, 11 patients worsened in their EDSS score, with 1 patient reaching a score of 8, having been enrolled at 6.5.
Eighteen patients experienced a clinical stabilization or improvement. In particular, 11 patients improved by at least 0.5 points in EDSS score as compared with baseline; 5 remained stable; and 3 patients progressed after an initial improvement. Two patients showed an improvement of 0.5 points lasting, respectively, for 36 and 48 months and then worsened to the baseline EDSS score (6.5). Another patient, after a 9-month improvement, progressed to the baseline EDSS (6.5) and at +30 months to a worse score (7.0). EDSS score changes over the entire study period and the year before the enrollment are reported in Figure 2. After HSCT all the patients received only symptomatic therapy; no one ever received any immunomodulating or immunosuppressive therapy or other drugs that could possibly affect the clinical course of disease or MRI findings. One patient showed a relapse 4.5 years after the transplantation associated with a new Gd-enhancing lesion at MRI scanning. The relapse resolved spontaneously within 3 weeks without any EDSS worsening. Confirmed progression-free survival was 95% ± 5% at 6 years after HSCT. Disease activity-free survival, where all signs of disease activity were considered events, was 64% at 4.5 years since HSCT (Figure 3).
EDSS outcome. Box plot of the changes in EDSS score over the entire study period and in the year before the enrollment. Error bars indicate the highest and lowest values, excluding outliers (○), which are cases with values between 1.5 and 3 box lengths from the upper or lower edge of the box. Extremes (*) are cases with values more than 3 box lengths from the upper or lower edge of the box; the box length is the interquartile range.
EDSS outcome. Box plot of the changes in EDSS score over the entire study period and in the year before the enrollment. Error bars indicate the highest and lowest values, excluding outliers (○), which are cases with values between 1.5 and 3 box lengths from the upper or lower edge of the box. Extremes (*) are cases with values more than 3 box lengths from the upper or lower edge of the box; the box length is the interquartile range.
Disease activity-free survival after HSCT. Estimated disease activity-free survival is 64% at 4.5 years. Tick marks represent censored observations.
Disease activity-free survival after HSCT. Estimated disease activity-free survival is 64% at 4.5 years. Tick marks represent censored observations.
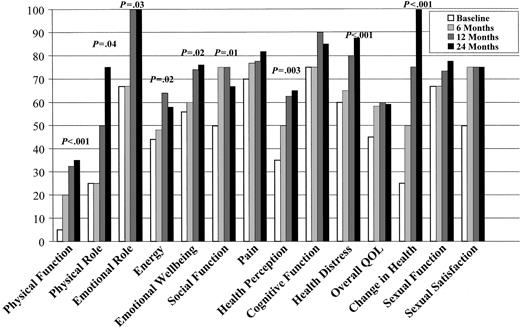
Quality of life outcome evaluation
HRQOL results, assessed in 9 subjects, were also remarkable. We found a significant improvement in both composite scores. Median (interquartile range) physical health composite at baseline was 38.5 (33.1 to 50.3); figures at 6 months were 52.9 (44.2 to 57.6); at 12 months 57.8 (54.8 to 67.8); and at 24 months 62.8 (55.0 to 72.6) (P = .002). Median (interquartile range) mental health composite at baseline was 57.7 (46.1 to 71.3); figures at 6 months were 61.8 (53.8 to 76.6); at 12 months 81.9 (59.0 to 85.6); and at 24 months 78.0 (59.2 to 86.7) (P = .05). When the individual MSQOL-54 domains are considered, improvement was highly statistically significant for physical function, change in health, and health distress (P < .001) (Figure 4).
Quality of life evaluation. Median values in MSQOL-54 domains over time were assessed at baseline and 6, 12, and 24 months after HSCT in 9 patients.
Quality of life evaluation. Median values in MSQOL-54 domains over time were assessed at baseline and 6, 12, and 24 months after HSCT in 9 patients.
MRI results
MRI data, available for 18 of 19 patients, are represented in Figure 5 as mean number of lesions per month per patient. At the enrollment, the mean number of lesions per month per patient was 10.8 (range, 1 to 46), increasing to 11.9 (range, 0 to 66) during the 3 months out of therapy period (Figure 5). An MRI at 30 days after mobilization with CY in 15 of 18 patients showed a dramatic decrease of the enhancing areas (mean, 4.5; range, 0 to 15), with complete disappearance in 6 cases. Except for 1 case that became negative at month 4, all the others dropped to zero during the first 3 months after HSCT. In one patient, a new single lesion appeared at month 4 of follow-up and disappeared at the next evaluation. While in the 3 months before therapy 656 Gd-enhancing lesions were detected, in the months after therapy the number was reduced to 7, with a statistically significant decrease of 99% (P < .0001 using the Mantel-Haenszel test). All the patients currently have negative MRI scans with a median follow-up of 36 months (range, 12 to 72); 1 lesion was detected in the patient who relapsed 4.5 years after the transplantation (see “Clinical outcome”).
MRI results. The mean numbers of lesions per month per patient are reported at baseline during the 3-month period before mobilization (-3-1), after mobilization (Cy), and after transplantation (ASCT) to last follow-up.
MRI results. The mean numbers of lesions per month per patient are reported at baseline during the 3-month period before mobilization (-3-1), after mobilization (Cy), and after transplantation (ASCT) to last follow-up.
In contrast, the analysis of PBVC showed a 1.9% volume reduction at 1 and 2 years after transplantation despite the complete suppression of Gd-enhancing activity. This suggests that in advanced MS a progression of tissue loss occurs independently from the inflammatory events.29 No adverse effects or laboratory abnormalities were observed as a consequence of monthly prolonged use of TD Gd.
Cerebrospinal fluid examination
In 4 evaluable patients, CSF examination before therapy showed oligoclonal bands (OBs) only in the CSF and not in the serum, while in 1 case OBs were present in the CSF and serum with additional bands in the CSF. Mobilizing and conditioning treatment were not able to induce any relevant change on the presence of OBs in the CSF. In fact, in all cases, during the follow-up, OBs were still detected in the CSF 6 or 12 months after transplantation, while in 3 patients a few OBs, not present before therapy, were also detected in the serum.
Discussion
The primary aim of phase 2 trials is to assess the activity of a new treatment in a specific disease while confirming its safety. Starting from 1997 a number of such trials have been reported concerning immunoablative therapy followed by stem cell rescue in autoimmune diseases16-22,36; follow-up of most of those studies has been published. In this paper we analyze the clinical follow-up of 19 MS patients enrolled in a multicenter phase 2 trial, with emphasis on the clinical tolerability of the treatment and the impact of HSCT on HRQOL.
Proper selection of patients is a key issue. Rapidly progressive patients showing high inflammatory activity and without severe disability are the ideal target for such an immunoablative treatment.35 We established an upper cutoff at 6.5 points in the EDSS scale at the time of enrollment, therefore selecting patients still able to walk with bilateral walking aids. EDSS scores increased in these patients during the 3 months off treatment before the transplantation, confirming the rapidly progressing MS form.
Mobilization regimens based on G-CSF administration in steady state have resulted in serious neurologic adverse events,21,26 possibly related to the release of T-lymphocyte active cytokines. Such events were interpreted as disease exacerbations and were apparently prevented by the administration of steroids in association with G-CSF. This sort of neurologic toxicity has not been reported in mobilizing regimens including CY and G-CSF. In our series of patients, CY at 4 g/m2 was effective in decreasing the number of Gd-enhancing lesions with a mild profile of toxicity. Considering the high level of inflammatory activity in these patients and that each new lesion can result in potentially irreversible neurologic impairment, a CY-based mobilizing regimen is preferred. This provides a faster therapeutic approach preventing further deterioration with a low risk of reversible toxic event.
The choice of an appropriate conditioning regimen is challenging. In terms of clinical benefit, the slow clinical evolution of MS requires a follow-up time much longer than hematologic diseases. Transplantation-related toxicity (TRT) can be evaluated in the short term. TRT usually results from both nonhematopoietic tissues damage and immunosuppression, the latter being affected by both the conditioning intensity and graft manipulation. There is some evidence that the association of ATG and CD34+ selection results in a deep and prolonged immunosuppression.37 More than 160 cases of MS treated with HSCT are registered in the EBMT Autoimmune Disease Working Party international database. An extended follow-up report to that first published by Fassas et al22 is underway. Although retrospective and limited by the multiplicity of transplantation protocols and of eligibility criteria, the analysis suggests a very acceptable safety profile for the BEAM plus ATG conditioning regimen without graft manipulation. (R.S., on behalf the EBMT Autoimmune Disease Working Party, in preparation). In our experience, the BEAM conditioning regimen was always well tolerated and extrahematologic toxicity was similar to that usually reported in oncologic patients. CD4+ lymphocyte subpopulation recovery was slow, but no clinically documented infections were observed beyond 3 months from the transplantation. Based on our and others' experience, the mobilization (CY plus G-CSF) and conditioning (BEAM plus rbATG) regimens have therefore been chosen for the transplantation arm of the prospective phase 3 EBMT/ASTIMS (Autologous Stem Cell Transplantation International Multiple Sclerosis) trial (www.astims.org).
MRI lesions are a major marker of inflammatory activity. In our series of patients, clinical deterioration paralleled MRI-evidenced flare. The lack of new lesions after HSCT was associated with a clinical stabilization. These findings are promising when considering the rapid clinical deterioration in the year before the transplantation (Figure 2) although, without a control group, stabilization could be partially accounted for by the regression to the mean. Preliminary analysis of brain volume on the patients with the longest follow-up shows a trend toward atrophy; this parameter does not seem to be halted by the transplantation and might explain the slight worsening of EDSS in 3 of 19 patients at +9, +36 and +48 months, respectively. Progressive brain atrophy is a phenomenon consistently associated with the progressive phase of MS, mostly related to the degeneration of tissues.
MS is a chronic disease requiring life-long treatments that can cause major side effects.38 Assessing the impact of these interventions on HRQOL is important because it gives the patient's perspective on the overall effect of the treatment. Our results, even if obtained on a subset of patients, clearly show that HSCT improves HRQOL in people with severe MS. Physical function, change in health, and health distress were the MSQOL-54 domains more significantly affected by the treatment.
The consistency between our clinical, MRI, and HRQOL results, together with the persistence of the improvement, is in favor of the efficacy and safety of HSCT in patients with severe MS unresponsive to conventional treatments. These promising results need confirmation by means of a randomized controlled trial.
Appendix
The Italian GITMO-Neuro Intergroup that has actively contributed to this study also includes the following scientists: M. G. Marrosu, E. Cocco, and V. Derchi (Cagliari); A. Lugaresi, D. Farina, C. Iarlori, and A. Tartaro (Chieti); L. Massacesi, A. Repice, and G. Pellicanò (Firenze); E. Capello, L. Dogliotti, R. C. Parodi, A. Schenone, M. P. Sormani, and A. Uccelli (Genova); G. Meucci (Livorno); M. Inglese (New York); E. Merelli, F. Casoni, and F. Cavalleri (Modena); A. Bertolotto, M. Capobianco, and S. Duca (Orbassano-Torino); and S. Mosti and A. Abbruzzese (Pisa).
Prepublished online as Blood First Edition Paper, November 16, 2004; DOI 10.1182/blood-2004-08-3205.
A complete list of members of the Italian GITMO-Neuro Intergroup appears in the “Appendix.”
Partially supported by grants from the Fondazione Italiana Sclerosi Multipla (FISM 2001).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
The authors are gratefully indebted to Chiara Tyndall for her critical review of the manuscript.




This feature is available to Subscribers Only
Sign In or Create an Account Close Modal