Comment on Cooling et al, page 3356
The expression of ABH antigens by red cells and platelets has been thought to be similar but this is not true. Platelets from group A2 donors lack A antigen and are compatible with all blood groups.
Group O red blood cells (RBCs) are universal blood components since they can be transfused to patients of all blood groups. Similarly, group AB plasma can be transfused to patients of any blood group. Until now there has not been a universal platelet type. Neither group O or AB platelets can be used universally since the transfusion of group AB to patients with anti-A or anti-B results in decreased platelet recovery and survival,1,2 and group O platelets contain 200 to 400 mL of plasma with anti-A and -B, which may hemolyse group A and B RBCs. In this issue of Blood, Cooling and colleagues describe a nearly universal platelet component: platelets from group A2 individuals.
Cooling et al discovered that the conventional belief that platelet expression of ABH antigens was similar to the expression of these antigens by RBCs is incorrect. Among group A individuals, approximately 80% are A1 and 20% are A2. The A antigen on A1 and A2 RBCs is the same but the antigen density differs: it's lower on A2 RBCs. Cooling et al confirmed that A antigen is expressed on platelets from most group A1 individuals but A2 platelets lacked or expressed only very low levels of A antigen. Group A2 platelets also lack the precursor on which A and B antigens are built, H antigen, suggesting that ABH antigen expression on platelets may be determined primarily by the activity of H-glycosyltransferase activity. In contrast, on RBCs ABH antigen levels are determined primarily by A- and B-glycosyltransferase activity.
Since platelet components for group A2 donors contain anti-B, they are not truly universal platelets but they can be transfused to both group A and O patients. Approximately 45% of US blood donors are group O and 40% are group A, so A2 platelet components are compatible with approximately 85% of patients.FIG1
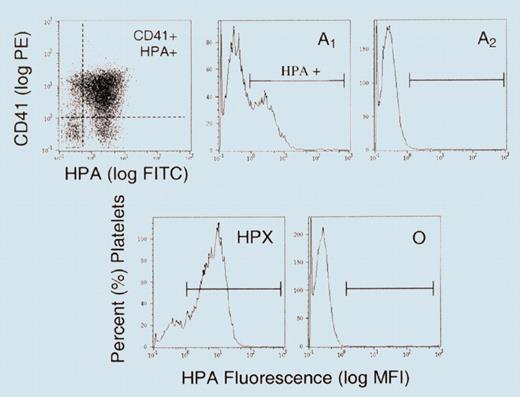
Flow cytometry analysis of platelets with fluorescein-labeled Helix pomatia, a lectin specific for A antigen, shows that group A1 platelets express A antigen but not group A2. See the complete figure in the article beginning on page 3356.
Flow cytometry analysis of platelets with fluorescein-labeled Helix pomatia, a lectin specific for A antigen, shows that group A1 platelets express A antigen but not group A2. See the complete figure in the article beginning on page 3356.
The absence of A antigen on A2 platelets has important clinical implications since the transfusion of ABH incompatible platelets results in reduced platelet recovery and survival in all patients. The clinical responses to platelet transfusions are variable and differences in platelet A antigen expression may explain some of this variability. Group O patients are often given group A platelets of unknown subgroup. Since group A2 platelets do not express A antigen, group O patients likely respond better to A2 platelets than A1 platelets.
These finding are especially important for hematopoietic stem cell transplantations involving donors and recipients with mismatched A and O blood groups. It is best to transfuse these patients with platelets that do not express A antigen and that lack anti-A. Since only group A2 platelets meet both criteria, for these patients A2 platelets are ideal.
While platelets are currently labeled A, B, O, or AB, it is easy to identify A2 platelets. Group A1 and A2 donors can be distinguished by an RBC agglutination assay. The lectin Dolichos biflorus agglutinates A1 RBCs but not A2 cells. ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal