Comment on Li et al, page 3465
When bone marrow progenitor cells from Fanconi anemia knockout (Fancc-/-) mice are cultured ex vivo in a growth-factor cocktail, they exhibit apparent stem cell exhaustion and clonal evolution to apoptosis-resistant leukemia.
Fanconi anemia (FA) is a genetic disorder that predisposes to bone marrow failure, birth defects, and cancer. Links to breast cancer susceptibility gene 1 (BRCA1) and BRCA2 have suggested a role for the FA proteins in DNA damage repair. Unfortunately, advances in our understanding of FA have not yet been translated into successful treatment strategies. One elusive goal has been the development of effective hematopoietic stem cell gene therapy. In many respects, FA seems a particularly good candidate for gene therapy1 : (1) the hematopoietic defect likely involves a primitive stem or progenitor cell so that reconstitution with corrected cells could lead to multilineage recovery, even if only a small number of stem cells were corrected; (2) there should be strong selective pressure favoring the growth of gene-corrected cells; (3) there might be little or no need to precondition patients with myeloablative therapy since they are already aplastic. With these considerations in mind we completed a pilot study of gene therapy in 4 FA patients in which we documented engraftment of hematopoietic progenitor cells repeatedly transduced with a Moloney retroviral vector expressing FANCC.2 Although this trial did not lead to clinically significant benefits, we believe this may have been due to inability to target long-term reconstituting stem cells with the vector used. Subsequent experiments in mice have lent further credence to the idea that gene therapy could restore the repopulating ability of mutant FA stem cells to near wild-type levels.3 Some mice, however, that were reconstituted with uncorrected Fancc-/- mutant cells (lacking the wild-type Fancc transgene) developed bone marrow failure and myelodysplasia (MDS). As gene therapy is still an inefficient process, the question was asked: what is the fate of these uncorrected mutant cells?
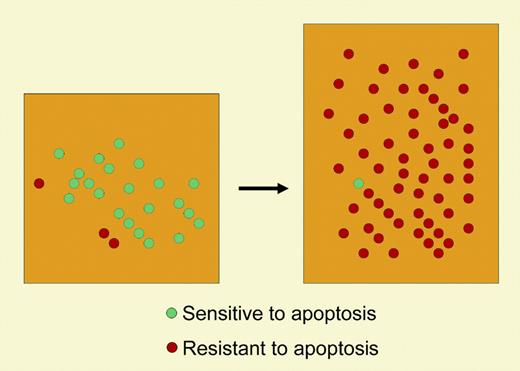
In this issue of Blood, Li and colleagues provide some answers as to the pathologic consequences of ex vivo culture of Fancc-/- stem cells that are not gene corrected. They demonstrate that the culture process (needed to promote cell proliferation for transduction with Moloney retroviruses) is associated with increased apoptosis of a primitive population of Fancc-/- cells. When irradiated mouse recipients were reconstituted with Fancc-/- bone marrow cells cultured for either 2 or 4 days, many mice developed MDS, myeloproliferative disease, or acute myeloid leukemia (AML). Whereas progenitors cultured from the bone marrow of unaffected Fancc-/- recipients are hypersensitive to various inhibitory cytokines, cells from mice with AML or MDS were found to be resistant to tumor necrosis factor-α–mediated apoptosis.
Several questions raised by the present study remain unanswered. First, why haven't most or all of the 8 (4 FA-C2 and 4 FA-A4 ) patients who received ex vivo–cultured and –transduced cells developed AML or MDS? The authors themselves suggest that the difference may lie in the relative efficiency of engraftment of cultured cells in the lethally irradiated mouse recipients compared with the inefficient engraftment in the human recipients (who received no irradiation). If true, then dealing with the consequences of clonal escape may be necessary once gene therapists become more adept at stem cell engraftment (see figure). One potential solution to this problem may be to limit ex vivo manipulation of the cells, perhaps by using lentiviral vectors. Alternatively, it may be possible to enrich for only gene-corrected cells using a selectable marker. Since the mouse experiments suggest that gene-corrected cells are less susceptible to clonal evolution,3 there may yet be hope for gene therapy. ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal