Abstract
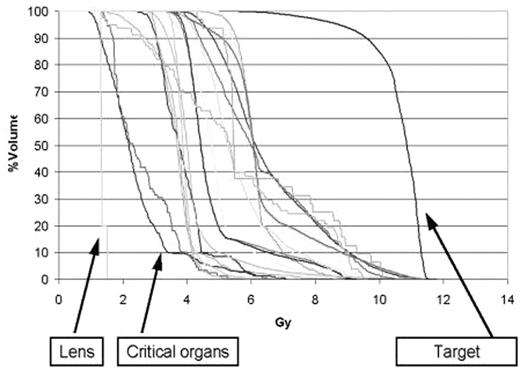
Tandem high-dose therapy (HDT) followed by peripheral blood progenitor cell reinfusion (PBPC) improves survival for patients with MM, but 80% of patients relapse within 7 years after HDCT. Attempts to treat all areas of skeletal involvement by combining total body irradiation (TBI) with high-dose melphalan (Mel) resulted in substantial organ toxicities and precluded optimal dosing of Mel. Helical tomotherapy allows for 3D CT image guided intensity modulated radiation therapy to large target regions. Radiation beams can be shaped and directed at disease sites from multiple directions. This technology may allow delivery of total marrow irradiation (TMI) at high doses in order to treat MM, while avoiding collateral toxicities. We had performed pre-clinical simulation studies for an adult female patient generating dose volume histograms (DVH) which demonstrated a 2–7 fold reduction in median dose to critical organs and which predicted for the ability to deliver up to 2.0 Gy to the marrow compartment with comparable or reduced risks of mucositis, espohagitis, enteritis, pneumonitis, nephropathy, and cardiomyopathy as it would be expected with TBI of 1.2 Gy. We then designed a phase I/II study for patients with responding or stable stage I-III MM who undergo PBPC mobilization with cyclophosphamide 1.5 gm/kg and G-CSF 10 microgram/kg, and than receive tandem HDT first with melphalan 200 mg/m2 and PBPC, and a minimum of 6 weeks later they are treated with escalating doses of TMI (starting dose: 200 cGy daily x 5, to be escalated up to 200 cGy twice daily x 5 days), and PBPC. Subsequent maintenance therapy consists of dexamethasone 40 mg/day x 4 days every 28 days and thalidomide 50-200 mg/day. The first patient treated with 1 Gy of TMI was a 53 year old woman with stage I IgGκ MM in complete remission after thalidomide and dexamethasone induction. Neutrophil (ANC) and platelet nadirs were observed on days 5 and 9 after melphalan and PBPC; ANC recovery to > 500/uL occured by day 13 and the patient became platelet transfusion independent by day 9. TMI and PBPC were administered 12 weeks later. ANC and platelet nadirs occurred on days 3 and 5; ANC recovered in 10 days and platelet transfusion independence was accomplished by day 11. The patient experienced partial alopecia, grade 2 nausea and grade 1 emesis on the second day of TMI, but she was completely devoid of erythema, mucositis, or diarrhea. The actual DVHs were comparable to those seen in the preclinical studies/simulations and reflected an estimated 2.5 fold median decrease in the amount of radiation delivered to non-target organs in comparison to the target: bone marrow.
Accrual to the first dose level is completed. Details of toxicities and DVH curves from additional patients/cohorts who will have completed their TMI cycles will be presented.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal