Abstract
Introduction: Assessment of bleeding in ITP is difficult. There is no agreed upon methodology; the WHO bleeding score does not seem useful for ITP. We report an ITP bleeding score including the relationship between site-specific bleeding severity (BLS), platelet count (plt ct), and plt size.
Methods: A bleeding score was created which has 11 sites, 9 by history (Hx) of the previous week: skin, oral, epistaxis, GI, GU, GYN, hemoptysis, subconjunctival (SC), and intracranial hemorrhage (ICH); and 2 by Exam (PE): skin and oral. The BLS grades (gr) pts for each site on a defined scale from no bleeding (0) to “major” bleeding (2). Plt cts and large plts (LP) were measured on the Bayer Advia 120. No pt had > 2 study visits.
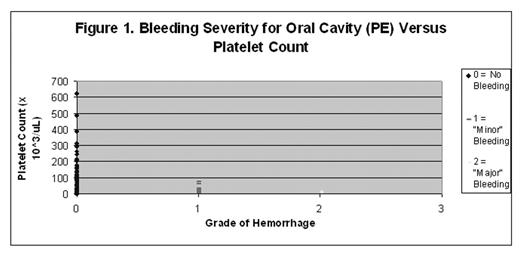
Results: The 65 ITP pts on 100 visits over 6 months had a median (mdn) plt ct of 41,500/uL (41.5k). The mdn age was 31.5 yrs; 20 pts were children. 56 pts had chronic ITP, 26 s/p splenectomy, with a mdn duration of ITP of 6 yrs. There were no GU, SC hemorrhage (hem), or ICH. 72% of all gr 1 hem’s were skin whereas 46% of gr 2 hem’s were oral. There was 1 GI hem and 3 hemoptysis visits that were gr 2. 42 women on 63 visits had 5 visits each with GYN BLS gr 1 and gr 2. X2 testing correlated plt ct and BLS for 6 sites: both oral and both skin sites, epistaxis, and GYN (p’s < 0.05). Oral PE correlated best with the plt ct (fig 1). For oral PE, BLS of gr 2 did not occur at plt cts > 20k.
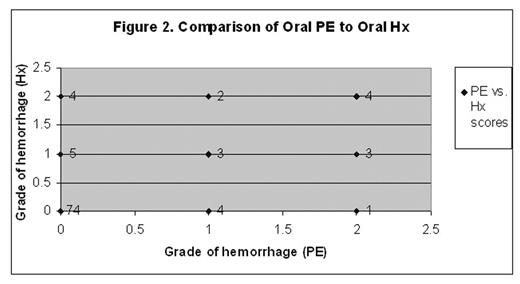
When the BLS was scored independently by two observers (LKP & JB) on 63 of the100 visits, 92% of individual BLS grs were identical (PearsonR=0.75). Skin PE and epistaxis each had 11/63 discrepancies. In addition, 16 BLS for oral (15 for skin) were different comparing Hx and PE (fig 2).
LP did not correlate well with site-specific BLS when only plt cts ≤ 30k were included, suggesting that large, young platelets may not primarily determine bleeding severity in ITP. However for Skin Hx, if the BLS was gr 0, 4/6 had LP ≥ 2 whereas only 7/28 LP were ≥ 2 when the BLS was gr 1.
Conclusions: The Bleeding Score reported here was validated by: a) the relationship of bleeding severity at multiple sites to plt ct including the absence of gr 2 bleeding at plt cts >20k; and b) the high degree of interobserver reliability despite a low but irreducible error rate based on variability in pt recall. It takes ≤ 3–5 minutes to complete. The significance of LP remains unclear. Studies of the BLS in larger numbers of patients will further determine its usefulness.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal