Abstract
Background: Acquired SAA is a potentially life-threatening bone marrow failure disorder that is usually immune-mediated. SAA can be effectively treated with bone marrow transplantation (BMT), immunosuppressive therapy (IST), or CY. BMT can cure the disease but ideally requires a matched sibling donor. IST has a high response rate, but up to 50% of patients relapse, become dependent on cyclosporine, or develop secondary clonal disease such as paroxysmal nocturnal hemoglobinuria (PNH) or myelodysplastic syndromes (MDS). We previously showed that CY induces durable remissions in the majority of SAA patients, but concern has been raised about the safety of this approach.
Methods: Since 1996, we treated 38 previously untreated, and 17 IST failed, SAA patients with CY (50 mg/kg/d x 4) followed by daily G-CSF (5 ug/kg/day) until the neutrophil count (ANC) reached 1000/dl. Response was defined as ANC > 1000/dl and transfusion independence without growth factor support for > 3 months. Relapse was defined as no longer meeting criteria for response. PNH was monitored by flow cytometry.
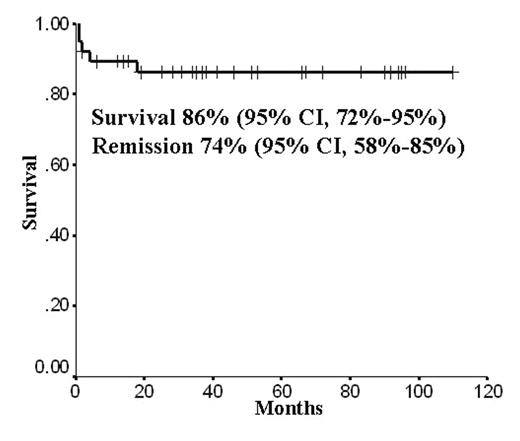
Results: The median age of the newly diagnosed patients was 40 (range 2–68) years. With a median follow-up of 41 (range, 6 – 111) months, 33/38 patients survive (actuarial survival of 86%, 95% CI 72–95%) with 28 (74%, 95% CI 58–85%) achieving remission, most being complete. Median time to ANC of 500, last platelet and red cell transfusion was 50, 99, and 181 days, respectively. Before treatment, 15 patients met criteria for very (v) SAA (ANC < 200). Mortality within 6 months after CY occurred in 4 (10.5%) patients, all with vSAA; 1 additional patient died from bacterial sepsis 18 months after CY. 22/23 (96%) SAA patients survive (20 in remission) compared to 11/15 (73%) with vSAA (10 in remission). Eight patients had a severe infection at the time of beginning treatment and 5 survive in remission. PNH screening revealed a PNH population ranging from 0.5–40% of granulocytes in 12 patients, and all 12 achieved a durable remission (p = 0.039). No patient in this series has progressed to PNH or MDS, and the PNH clone is regressing in all 12 patients. Two patients have relapsed. One patient, whose first remission lasted 5 years, was retreated with CY into a persisting second complete remission 3 years ago; another patient recently relapsed 3 years after achieving remission. Ten of the 17 patients who failed IST (median age of 31, range 6–58) are alive and nine are in remission.
Conclusions: Cy is safe and highly effective therapy for both untreated and relapsed SAA. Relapses after CY are rare and progression to PNH or MDS in previously untreated patients has not been observed in this series with now 15 patients out beyond 5 years. The presence of a PNH population may be a favorable risk factor, perhaps by excluding non-immune mediated forms of SAA.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal