Abstract
Background. Management of patients with suspected Pulmonary Embolism (PE) is problematic if diagnostic imaging is not available. Pretest Clinical Probability (PCP) and D-dimer (D-d) assessment were shown to be useful to identify those high risk patients for whom empirical, protective anticoagulation is indicated (
Objective of the study. In consecutive patients with suspected PE, we evaluated whether PCP and D-d assessment, together with the use of low molecular weight heparins (LMWHs), allow objective appraisal of PE to be deferred for up to 72 hours.
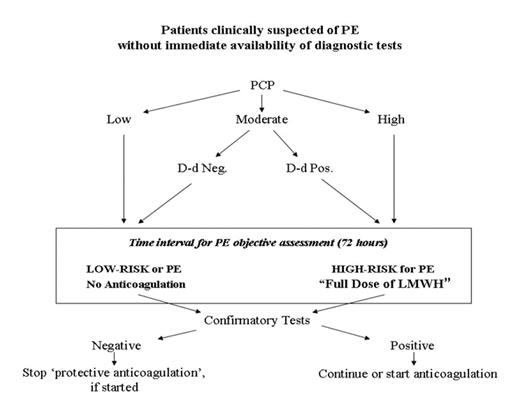
Methods. In case of deferment of diagnostic imaging for PE, patients identified at high-risk (those with high PCP and those with moderate PCP and a positive D-d), received a protective full-dose treatment of LMWH; the remaining patients were discharged without anticoagulants. All patients were scheduled to undergo objective tests for PE (ventilation/perfusion lung scanning or computed tomography lung scan) within 72 hours from the index visit (figure). Standard antithrombotic therapy was then administered when diagnostic tests confirmed Venous ThromboEmbolism (VTE).
Results. 336 patients with suspected PE were included in this study. The prevalence of VTE was 6.1% (95% CI 2.7–9.3) in the “low-risk group” and 50.4% (95% CI 41.7–59.1) in the “high-risk group”. In total, VTE was confirmed in 76 (22.6%) of 336 patients (95% CI 18.2–27). Patients’ characteristics, median time for deferral test and for LMWH administration are listed in table 1. Events at the short-term (72 hours) and long-term follow-up are listed in table 2. None of the patients had major bleeding events during the follow-ups.
Conclusions. When objective diagnostic assessment of PE is not immediately available, management of symptomatic PE patients can prove highly unsatisfactory. This study demonstrates that a simple and reproducible approach allows a safe deferral of diagnostic imaging for PE for up to 72 hours.
patients’ characteristics
| Baseline features . | Low risk group (n. 211) . | High-risk group (n. 125) . | p value . |
|---|---|---|---|
| n.s.: not significant | |||
| Age in years (range) | 59.3 (22–91) | 60.3 (23–91) | n.s. |
| Sex (F/M) | 98/113 | 59/66 | n.s. |
| Time since onset of symptoms (days) | 1.7 | 1.5 | n.s. |
| Co-morbidity and | 16 (7.5) | 25 (19.2) | 0.03 |
| Median time of deferral test (hours) | 49.5 | 42.5 | n.s. |
| Median time of protective anticoagulation (hours) | not applicable | 35.5 | not applicable |
| Baseline features . | Low risk group (n. 211) . | High-risk group (n. 125) . | p value . |
|---|---|---|---|
| n.s.: not significant | |||
| Age in years (range) | 59.3 (22–91) | 60.3 (23–91) | n.s. |
| Sex (F/M) | 98/113 | 59/66 | n.s. |
| Time since onset of symptoms (days) | 1.7 | 1.5 | n.s. |
| Co-morbidity and | 16 (7.5) | 25 (19.2) | 0.03 |
| Median time of deferral test (hours) | 49.5 | 42.5 | n.s. |
| Median time of protective anticoagulation (hours) | not applicable | 35.5 | not applicable |
Outcome of Short- and Long-term FU
| Categories of patients (n) . | Events at the short-term FU . | Events at the long -term FU* . |
|---|---|---|
| FU indicates follow-up; CI indicates Confidence Intervals. *This refers to patients in whom Pulmonary Embolism has been previously ruled out (n. 260). | ||
| “Low-risk group” (211) | 0 (0%) [95% CI 1.4] | 0 (0%) [95% CI 1.4] |
| “High-risk group” (125) | 1 (0.8%) [95% CI 2.3] | 3 (2.4%) [95% CI 3.2] |
| Categories of patients (n) . | Events at the short-term FU . | Events at the long -term FU* . |
|---|---|---|
| FU indicates follow-up; CI indicates Confidence Intervals. *This refers to patients in whom Pulmonary Embolism has been previously ruled out (n. 260). | ||
| “Low-risk group” (211) | 0 (0%) [95% CI 1.4] | 0 (0%) [95% CI 1.4] |
| “High-risk group” (125) | 1 (0.8%) [95% CI 2.3] | 3 (2.4%) [95% CI 3.2] |
Patients clinically suspected of PE without immediate availability of diagnostic tests
Patients clinically suspected of PE without immediate availability of diagnostic tests
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal