Abstract
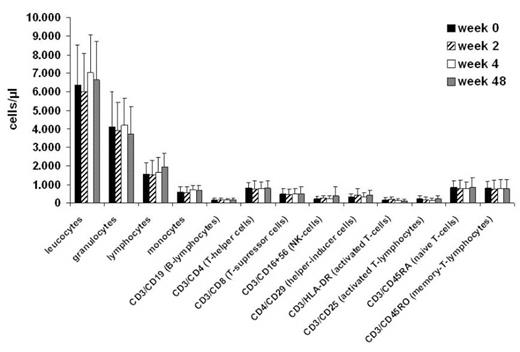
Intravenous infusion of bisphosphonates can cause acute phase reactions which may be caused by changes in the cellular immune system, particularly in lymphocyte subtypes. These immune changes and an acute phase reaction both normally disappear after 48 hours. Previous studies have shown that kidney transplant recipients treated with immunosuppressive therapy and ibandronate for bone protection have a lower rejection rate than those treated with immunosuppressive therapy and placebo.1 This suggests that there may be long-term changes in the immune system occurring with ibandronate treatment. We investigated the long term changes in the cellular immune system during ibandronate treatment in dialysis patients. As these patients are not normally treated with immunosuppressive or cytotoxic agents, which can cause changes in the cellular immune system, they are an eligible population for such a study. In this open-label trial, 16 patients with end-stage renal disease receiving regular hemodialysis were recruited. All patients were treated with ibandronate 2mg every 4 weeks for renal osteopathy; a dose that provides similar AUC and bone exposure as a 6mg dose in patients with normal renal function. The cellular immune system was investigated before first ibandronate application and the measurement was repeated at weeks 2, 4 and 48. The following parameters were measured by blood count differentiation: leucocytes, granulocytes lymphocytes, monocytes. Lymphocyte subtypes were measured by flow cytometry: B-lymphocytes (CD3+/CD19+), T-helper cells (CD3+/CD4+), T-suppressor cells (CD3+/CD8+), natural killer (NK)-cells (CD3+/CD16+56+), helper-inducer cells (CD4+/CD29+), activated T-cells (CD3+/HLA-DR+), activated T-lymphocytes (CD3+/CD25+), naive T-cells (CD3+/CD45RA+) and memory-T-lymphocytes (CD3+/CD45RO+). Twelve patients completed the study and were evaluated. One patient dropped out because of flu-like symptoms with muscle pain after the first ibandronate infusion; however this was well controlled with paracetamol. Three patients died due to concomitant diseases (diabetes and cardiovascular events). There were no statistically significant differences in cellular immunity over time as measured in weeks 0, 2, 4 and 48 (see Figure). In this small-pilot study of dialysis patients receiving ibandronate, no changes in the cellular immune system were observed over time. Changes in different lymphocyte subtypes, which occur in the acute phase reaction after first infusion, were not seen. Reduced rejection rate in transplant recipients after ibandronate infusion cannot be explained by changes in the cellular immune system, and must therefore occur by another mechanism.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal